Abstract
Purpose
Adolescent depression is associated with a range of interpersonal adversities. We hypothesized that depressed adolescents are at subsequent increased risk of problems related to intimate relationships and childbearing in adulthood, and used longitudinal data to examine this.
Method
A population-based investigation of depression in 16 to 17 year olds was followed up after 15 years, at around the age of 30 years. Comparisons were made between adolescents with depression (n = 361, 78% females) and non-depressed peers (n = 248, 77% females). Data from both national registers and personal interviews were used.
Results
At follow-up, the former depressed and non-depressed adolescents had become parents to a similar extent. The former depressed females were more likely than the non-depressed females to report abortion, miscarriage, intimate partner violence and sexually transmitted disease. They also reported a higher number of intimate relationships and were more likely to have divorced and to be registered as single mothers. Depressed females with a comorbid disruptive disorder had a particularly poor outcome. In the depressed females without a disruptive disorder, only those who subsequently had recurrent depressions in adulthood were at increased risk of poor outcome. There was no indication that the formerly depressed males were at increased risk of subsequent problems related to intimate relationships.
Conclusion
Females with adolescent depression subsequently have problems related to intimate relationships and childbearing. Disruptive disorders and recurrence of depression appear to be instrumental in this association. Attention should be given to intimate relationship problems and sexual and reproductive health issues in young women with depression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescent depression is related to a range of interpersonal adversities. The research to date suggests that depressed adolescents have a less supportive family environment and more conflicts within the family, compared with non-depressed adolescents of the same age [48, 51]. Depressed adolescents are also less content with their social network and have difficulties with their peer affiliations and social skills [5, 41, 43], and these difficulties appear to persist in adulthood [4, 10, 18, 42, 58]. Further, adolescent depression has been shown to be associated with sexual risk behaviour, multiple sexual partners and early pregnancies [16, 18, 32, 33, 47]. This raises questions on how depressed adolescents subsequently cope with intimate relationships, pregnancy and the process of starting a family of their own, issues that might be further complicated throughout the lifespan by recurrent depressions, psychiatric comorbidity and social disadvantages [28, 34].
Previous studies suggest that depression in adulthood is associated with abortion [15, 19], marital dissatisfaction and divorce [1, 31, 57], intimate partner violence [9, 49] and single parenthood [12, 13]. Depression has been investigated both as a precursor [31] and as a consequence [29, 30] of such adversities. Since a substantial proportion of adult cases of depression have an onset already in adolescence [44], longitudinal studies spanning from adolescence to adulthood are well suited to investigate the temporal order further. The few longitudinal population-based studies studying this indicate that formerly depressed females get married earlier and are at increased risk of early motherhood [18, 25]. Gotlib et al. [25] discuss that this might be due to interpersonal dependency or conflicts with parents, motivating them to leave their parental home early. Gotlib et al. [25] also report that adolescent depression in females predicts subsequent marital dissatisfaction at age 23–24 years. Although divorce was a low frequency outcome at this age [34], marital dissatisfaction indicates that these young adults might be heading for future marital disruption.
Given these results, there is reason to investigate this further with a broad range of outcomes and a longer follow-up period. This is further motivated by concerns that family disruption and associated social adversities could have long-lasting negative implications for both parents and their children [8, 12, 21, 56]. This seems especially of concern in adolescents and young adults with depression, since the stress and strain of disrupted relationships and adverse pregnancy outcomes might trigger recurrent depressive episodes.
Multiple factors can be expected to contribute to the psychosocial outcome after adolescent depression [18, 34]. Early adversities, such as maltreatment of poor family environment, might set the stage for future problems. Further, the course and patterns of the psychopathology might have a decisive influence on the outcome; adolescents with depression may have had symptoms of depression, anxiety and disruptive behaviour from an early age [37] and a substantial proportion experience recurrent depression in adulthood [20]. Closer inspection of these aspects might shed new light on the pathways leading to a poor outcome.
Aim
The general aim of the present study was to investigate how adolescents with depression subsequently adapt to intimate relationships, childbearing and family life. We therefore set out to follow up depressed adolescents and non-depressed peers at an age when marriage and childbearing, as well as family breakdown and adverse pregnancy outcomes, have become frequent outcomes [55]. A broad range of outcomes was used, to give as complete a picture as possible of how depressed adolescents adapt to these aspects of adulthood. Three main research questions were addressed:
-
1.
Is adolescent depression associated with subsequent problems related to intimate relationships, childbearing and family life?
-
2.
To what extent does problems in childhood and adolescence related to adolescent depression, such as family adversities and disruptive disorders, contribute to the outcome?
-
3.
Is poor outcome in this domain associated with recurrence of depression in adulthood in adolescents with depression?
Method
Study population and procedure
The present study followed up a population-based investigation of adolescent depression, carried out in 1991–1993 in the Swedish University town of Uppsala. In the original investigation [40], all first year students in upper-secondary school (16–17 years old) were asked to participate. Dropouts from school of the same age group were also invited; out of the 183 dropouts, 97 participated. Out of a total of 2,465 adolescents in the age group, 2,300 participated in a screening with two self-evaluations of depression, the Beck Depression Inventory (BDI) [3] and the Centre for Epidemiological Studies-Depression Scale for Children (CES-DC) [50]. Those with positive screening (BDI ≥ 16; CES-DC ≥ 30 + BDI ≥ 11; or a reported suicide attempt) were assessed with the diagnostic interview for children and adolescents in the revised form according to DSM-III-R for adolescents (DICA-R-A) [46]. For each student who either had high scores or reported a suicide attempt, a same-sex classmate with negative screening was selected as a control and was interviewed in the same manner. In all, 631 adolescents (314 with positive and 317 with negative screening) were interviewed and asked for consent to be contacted for a future follow-up.
The 609 participants who consented to a new contact (307 with positive and 302 with negative screening) were included in the present follow-up study. In accordance with previous research showing that subthreshold depression in adolescents is similar to major depression with respect to psychosocial functioning and psychosocial outcome [23, 24], a broad definition of depression was used. Subjects meeting the DICA-R-A criteria for lifetime major depression amongst both those with positive and negative screening (n = 260, 82% female) or reporting subthreshold symptoms (dysthymic disorder and/or positive screening, n = 101, 68% females) were defined as depressed adolescents (n = 361 in total, 78% females). Subjects who did not meet any of these criteria were classified as non-depressed and constituted a comparison group (n = 248, 77% females).
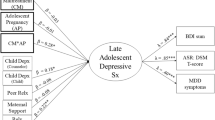
At age 30–33 years, these two groups were anonymously followed up in registers held by Statistic Sweden. In addition, the participants were contacted for a follow-up interview. Out of those with adolescent depression, 65% (n = 236, 80% females) took part in the interview; out of the non-depressed peers, 69% (n = 170, 79% females) participated. The register data were obtained in a way so that no participant could be identified, and thus the register data and the interview data could not be linked. The procedure is outlined in Fig. 1.
Chart outlining the procedure, both in adolescence and at follow-up in adulthood. Asterisk indicates the Beck Depression Inventory (BDI) and the Center for Epidemiological Studies. Depression Scale for Children (CES-DC) were used. Positive screening was defined as BDI ≥ 16; or CES-DC ≥ 30 and BDI ≥ 11; or attempted suicide
Our comparison group of non-depressed peers might not have been representative of non-depressed adolescents in general. As a complement, we therefore obtained register data on the total corresponding birth cohort registered as residents in Uppsala County (the approximate uptake area of the original investigation) at the time of the original investigation. As the original investigation spanned over 2 years, with about half of the schools in Uppsala investigated in the first year and the other half the next, we obtained data on both these age groups (born in 1975 and 1976, respectively; n = 6,968).
Interpersonal and family related adversities and disruptive disorders reported in adolescence
Socioeconomic group of the household was identified in the Swedish Population and Housing Consensus of 1990 and was defined according to a classification used by the Statistics Sweden [54]. This classification is based on occupation and considers the required level of qualification, type of production and position of work of the head of the household. The classification was divided into two ordinal categories: low (manual workers and grade I white-collar workers or no information available on social group) and high (white-collar workers grade II and III).
At the time of the original investigation, the participants completed the DICA-R-A and the Children’s Life Event Inventory [11]. Information on child or adolescent disruptive disorder according to DICA-R-A was included partly due to the social and interpersonal importance of these symptoms, partly due to their continuity in adulthood [17, 53]. Subjects meeting the DICA-R-A lifetime criteria for ADHD (23 females, 22 males), conduct disorder (60 females, 33 males) or oppositional defiant disorder (28 females, 6 males) were classified as having a disruptive disorder. Information on physical or sexual abuse in childhood and adolescence, as well as whether the participants lived with both parents in adolescence, was also derived from DICA-R-A. From the children’s life event inventory, information on parental divorce, conflicts between the parents, conflicts with the parents, breakup with boyfriend/girlfriend, pregnancy and induced abortion was included. A socioeconomic measure was created from the interview data by combining a question from the DICA-R-A about economic hardships in the family with an item from the children’s life event inventory about parental unemployment.
Outcome data retrieved from registers
Register data were retrieved from the register of the total population (held by Statistics Sweden) when the participants were between 30 and 33 years old. The data were obtained separately for males and females, with the participants divided into those with and those without adolescent depression. All childbirths and marriages were registered until the age of 30 years. Data on single parenthood by age 30 years, divorce and whether the participants resided in the same household as their biological parents at follow-up were also retrieved.
The register of the total population is continuously updated (with 1 month delay) with births and deaths, as well as changes of address, civil status and citizenship, recorded by the Swedish tax agency. The quality of data in general is reported to be good. Emigrations that have not been registered are reported to be the major source of error.
Personal follow-up interview in adulthood
An interview for demographic data and information on life events, specifically crated for this study, was used at follow-up. For the present study, we included questions about occurrences of induced abortion (“Have you ever had an abortion?” “When?”), miscarriage (including both spontaneous abortion and stillbirth) (“Have you ever miscarried/lost a child near birth?” “When?”), intimate partner violence (“Have you ever been physically abused/threatened to your life?” “By whom?” “When?”), number of permanent intimate relationships (“How many times have you been married/lived in consensual union/had other permanent intimate relationships since age 16?”), and sexually transmitted diseases (“Have you ever had a sexually transmitted disease?”). Incidents known to have taken place before the interview in adolescence (e.g. adolescent abortions) were excluded.
Major depressive episodes in adulthood (from age 19 to follow-up at age 30–33 years) were investigated with the Mini International Neuropsychiatric Interview Plus [52]. From these interviews, we categorized the participants as either having had substantial problems with depression in adulthood (at least two episodes or >6 month duration) or not.
Attrition
Participants not included in the national registers at age 30 years (mostly due to emigration) were excluded from the analyses unless previous information on the investigated outcome was available. On these grounds, 17 depressed (11 females) and 7 non-depressed (6 females) participants were excluded.
Out of the 609 eligible participants, 406 (67%; 65% of the depressed and 69% of the non-depressed) took part in the follow-up interview. The attrition was not significantly associated with sex, depression in adolescence or any of the investigated background variables. As illustrated by Table 1, the background variables did not seem to have a substantial effect on attrition.
Statistical analysis
As the timing of family-related outcomes such as marriage and childbearing differ substantially between the sexes in the general Swedish population [55], all analyses were conducted separately for females and males. Univariate comparisons were performed by means of the χ2 test. For small samples, Fisher’s exact probability test was used. The Mann–Whitney U test was used to compare data on an ordinal scale. To investigate the timing of marriage and childbearing, the Kaplan–Meier method was used, and log-rank statistics were used to test the equivalence of the survival curves.
The association between adolescent depression and the outcome of females was further investigated by means of logistic regression. Parental socioeconomic group was the only background variable that was linked to the register data, and was therefore the only variable included as a covariate in models with register data as dependent variable. In models with outcome measures from the follow-up interview as dependent variable, four background variables were included as covariates: economic hardship/parental unemployment; conflicts with parents; physical/sexual abuse at home; and disruptive disorder. These variables were selected on the grounds that they covered a wide range of child and adolescent adversities. No collinearity was detected. Due to the small group sizes and the low frequent outcomes, similar analyses were not possible for the males.
As the data on recurrent depression in adulthood were not linked to the register data, comparisons between the depressed females with and without recurrence were only conducted regarding the interview-based outcomes.
Overall, P values below 0.05 in two-tailed tests were considered to be statistically significant. SPSS 15.0 for Windows was used for all statistical analyses.
Ethics
To guarantee the integrity of the subjects, register data were obtained anonymously and arranged into larger groups. The study was approved by the local ethical vetting board of Uppsala University, Sweden.
Results
Interpersonal and family-related adversities reported in adolescence
A substantially larger proportion of the depressed adolescents, both males and females, reported adversities such as violence at home, family conflicts, economic hardships or parental unemployment, and disruptive disorder, as compared to their non-depressed peers. Notably, a larger proportion of the female adolescents with depression reported that they had been pregnant (Table 1).
Outcome data retrieved from registers
The depressed and non-depressed adolescents had become parents to a similar extent, and the proportion that got married did not differ significantly between the groups. Whilst survival curves did not suggest that there was a difference in timing of childbearing between the depressed and non-depressed adolescents, there was a tendency for the females with adolescent depression to get married earlier than their non-depressed peers (χ2 = 2.94, P < 0.086).
The whole range of investigated adverse outcomes was more common in the depressed females, as compared to the non-depressed females, whereas there were no statistically significant differences between the depressed and non-depressed males (Table 2).
As illustrated in Table 3, the estimates regarding the females’ outcome changed little or not at all by adjustment for parental socioeconomic group, although low parental socioeconomic group was a significant predictor of becoming a parent or divorcing.
The outcome of the larger reference group from the normal population was almost identical to that of the non-depressed peers, both regarding females and males. On the other hand, the females of the reference group differed significantly from the depressed females on the same measures as the non-depressed females did. In addition, there was a significant difference between the female reference group and the depressed females regarding the proportion who had married at the age of 30 years (30.1 vs. 37.1%, χ2 = 5.91, P < 0.05).
Comparisons between the subgroup with subthreshold symptoms of depression and those with major depression revealed few meaningful differences. Females with subthreshold symptoms were more likely than females with major depression to still be living with their parents at the follow-up (16.2 vs. 7.8%, χ2 = 3.96, P < 0.05), and males with subthreshold symptoms were less likely than males with major depression to be married at the age of 30 years (6.5 vs. 30.0%, χ2 = 6.12, P < 0.05).
Outcome measures from the follow-up interview in adulthood
A larger proportion of the formerly depressed females reported that they had experienced an induced abortion or miscarriage, as compared to the non-depressed peers (Table 2). The pregnancy per woman ratio was 1.77 in the formerly depressed females and 1.38 in the non-depressed peers, indicating that the depressed females in this study were more exposed to the risk of adversities related to pregnancy. As much as 14.1% of the pregnancies in the depressed females ended in miscarriage and 28.2% in induced abortion. The corresponding figures in the non-depressed females were 9.2 and 16.8%, respectively. Depressed females reported a higher number of intimate relationships than their peers (z = 2.68, P < 0.01) and were also more likely to report intimate partner violence and sexually transmitted disease (Table 2). No group differences between the formerly depressed males and their non-depressed peers could be discerned (Table 2).
Among the depressed adolescents, there were no significant differences between those with subthreshold symptoms and those with major depression.
The associations between adolescent depression in females and subsequent induced abortion and sexually transmitted disease were attenuated by adjustment for background variables, whilst this was not the case for miscarriage. Adolescent depression was still a significant predictor of intimate partner violence after adjustment. Disruptive disorder turned out to be a powerful predictor of subsequent abortion and intimate partner violence, whilst physical/sexual abuse at home was a predictor of future partner violence (Table 3).
The role of disruptive disorder in females with adolescent depression
Further analyses of females with adolescent depression revealed that those with comorbid disruptive disorder were more likely to subsequently have an induced abortion (48.9 vs. 25.5%; χ2 = 8.97, P < 0.01), get a sexually transmitted disease (40.4 vs. 23.4%; χ2 = 5.10, P < 0.05) and be exposed to partner violence (27.7 vs. 9.2%; χ2 = 10.06, P < 0.01), as compared to depressed females without this comorbidity. The same pattern was not evident for miscarriage (14.9 vs. 22.7%; χ2 = 1.50, NS).
The role of recurrent depressions in adulthood in females with adolescent depression
Given the evident impact of disruptive disorder, the association between the outcomes and adult recurrent depression in females with adolescent depression was analysed separately for those with and without comorbid disruptive disorder. Recurrent major depression in adulthood (defined as at least two episodes or >6 month duration) was reported by 57.1% of the females with comorbid disruptive disorder and 45.8% of those without this comorbidity. Among those with the comorbid condition, the ones with recurrent depression were not more likely than the ones without to report abortion (46.4 vs. 52.6%; χ2 = 0.17, NS), miscarriage (7.1 vs. 26.3%; χ2 = 3.28, NS), partner violence (28.6 vs. 26.3%; χ2 = 0.03, NS) or sexually transmitted disease (39.3 vs. 42.1%; χ2 = 0.04, NS). Within those who did not have comorbid disruptive disorder, on the other hand, the ones with recurrent depression were more likely than those without recurrent depression to report abortion (35.4 vs. 17.1%; χ2 = 6.16, P < 0.05), partner violence (18.5 vs. 1.3%; χ2 = 12.31, NS), and sexually transmitted disease (32.3 vs. 15.8%; χ2 = 5.33, P < 0.05), but not miscarriage (24.6 vs. 21.1%; χ2 = 0.25, NS).
Discussion
In this population-based follow-up study, we have used data spanning from adolescence to around the age of 30 years to investigate the link between adolescent depression and subsequent outcomes related to childbearing and intimate relationships. The results suggest that females with adolescent depression are at increased risk of abortion and miscarriage and a diversity of other problems related to intimate relationships, such as divorce, single parenthood, intimate partner violence and sexually transmitted disease. In addition, depressed females lived with their parents at follow-up to a larger extent than their peers, indicating that they might have problems entering adult roles. Our data align well with previous longitudinal studies of adolescent depression [18, 25], as well as cross-sectional investigations of depression in adults [31]. The most original feature of this contribution is the combination of a long follow-up period, extensive background data and a broad range of outcome measures from both registers and personal interviews. This allows us to conclude that adolescent depression in females can predict poor outcome in this domain.
As illustrated in previous studies [18, 34] psychosocial outcomes after adolescent depression could have multiple explanations. In line with previous research [5, 48], our data clearly show that the depressed adolescents were exposed to a wide range of adverse conditions already in adolescence. Closer inspection of our data revealed that especially disruptive disorder seems to be at the root of the investigated outcomes. About one-fourth of the depressed females had a comorbid disruptive disorder, and this subgroup was substantially more likely than the other depressed females to report abortion, partner violence and sexually transmitted disease. Recurrence of depression in adulthood did not further increase the likelihood of poor outcome in this subgroup, indicating that disruptive disorder in itself might constitute a risk for these outcomes. One might speculate that this risk is mediated by factors such as impulsive sexual risk behaviour, alcohol and substance use, and affiliation with peers and intimate partners with antisocial behaviour [7, 35, 38].
The majority of the depressed females did not have a disruptive disorder, though, and in these women recurrence of depression in adulthood seemed to be decisive. Those who did not have recurrent depression in adulthood (slightly more than half) reported abortion, partner violence and sexually transmitted diseases to an extent similar to that of non-depressed females. Those with recurrent depressions, on the other hand, reported these outcomes to an extent more reminiscent of that of the depressed females with disruptive disorder. Recurrence of depressions thus seems to reflect another pathway connecting adolescent depression and poor outcome. However, it is not clear from the present study whether recurrent depressions increase the risk of these adverse outcomes, whether these outcomes kindle recurrent depressions in vulnerable females, or if both recurrent depressions and the investigated outcomes are caused by other unmeasured variables. In line with that previously argued by Hammen [26], it is probable that all these alternatives interact in a “vicious circle” in depressed females. First, underlying interpersonal problems and cognitive difficulties might imply vulnerability for both recurrent depression and the investigated outcomes. Second, depression in itself might interfere with the rapid development of social and sexual behaviour in adolescence and young adulthood and hinder formation of social networks and stable intimate relationships, setting the stage for future problems. Recurrence of depression throughout the lifespan is also likely to be demanding both for the depressed females and their partners [45]. Further, social adversities in the wake of adolescent depression, such as low educational attainment and unemployment [4, 28], could also impair intimate relationships. Third, the stress and strain of disrupted intimate relationships, single motherhood and adversities related to pregnancy might kindle recurrent episodes of depression; incidentally, this could be a partial explanation for the increased risk of depression after divorce and in single mothers observed in previous research [1, 12, 13]. Fourth, it has also been reported that depressed females select unsupportive or depressed partners through assortative mating [14, 36], which could increase the risk of relationship discord further. For instance, our results on intimate partner violence indicate that partner choice adds to the burden of depressed females. Finally, ending up with an abusive partner or as a single mother could result in children growing up in an unfavourable environment. Thereby, the vulnerability to poor mental health might be transferred to the next generation [27].
The association between miscarriage and adolescent depression deserves further discussion. Unlike the other outcomes, miscarriage was not associated with disruptive disorder, recurrent depressions or any of the background variables. Further, miscarriage did not seem to be related to the other outcomes. This suggests that we have to look for an explanation elsewhere. First, it should be noted that the depressed females in our study had a higher pregnancy/woman ratio than their non-depressed peers and were thereby more exposed to the risk of miscarriage. However, the possible direction of causality is unclear; miscarriage might motivate women to try having a child once more, resulting in more pregnancies. Other factors that could have an impact are alcohol, smoking, medication, poor nutrition and infections [6, 22]. In addition, a recent study has proposed that emotional abuse by the partner increases the risk of miscarriage [2], which suggests that psychological distress might increase the risk of foetal loss. However, such explanations seem unlikely since the outcome was unrelated to disruptive disorders and recurrence of depression. More research on the association between miscarriage and depression is needed before any conclusions can be drawn.
Although both the females and males with adolescent depression reported more adversities in adolescence than their peers, our data did not suggest that the former depressed males had more troubled intimate relationships in young adulthood. This seems somewhat counterintuitive, especially since half of the depressed males had a disruptive disorder. It should be noted that there were few males in the present study, reflecting the lower prevalence of adolescent depression in males. In addition, most outcomes were less frequent in the male group, presumably explained by the fact that Swedish males marry and have children later than Swedish females [55]. Therefore, there could be a delay in the occurrence of such events as divorce, for instance. These caveats notwithstanding, it should be considered that the association between adolescent depression and subsequent intimate relationship problems might be specific to females. More research on the outcome of males with adolescent depression is needed.
Overall, the results suggest that interventions aimed at intimate relationship problems and sexual risk behaviour might be helpful for young females with depression, regardless of whether the recurrence of depression was a cause or consequence of adversities related to intimate relationships. It is now important to evaluate whether such interventions can have an effect on the recurrence of depression and the quality of life of these women. In addition, future research efforts should further elucidate the pathways from early depression to problems related to intimate relationships; apart from disruptive disorders, a range of other factors associated with early onset depression (such as cognitive competence, interpersonal skills, attachment, personality disorders and bipolar spectrum disorders) could prove to be decisive.
Limitations
Some characteristics of the data should be noted. First, the information on induced abortion, miscarriage and sexually transmitted disease was based on self-reports. The participants’ definitions of these concepts might not always have coincided with the medical terms. Second, the timing of the follow-up might have had relevance for the results. For instance, depressed adolescents can be expected to terminate their education earlier than their peers [4, 28]. As those who complete higher education or pursue a career might enter family life later, outcome at the age of 35 or 40 years could show a different pattern. Third, about one-third of the original participants did not take part in the follow-up interview, which might have biased the interview-based results somewhat. However, the attrition did not appear to be related to any of the background variables we investigated. Finally, although disruptive disorder and recurrence of depression might be expected to also be associated with register data (e.g. divorce and single parenthood), this could not be analysed.
Some characteristics of our depression group and comparison group should also be considered. Subgroups of our broadly defined depression group (e.g. with different duration and severity of depression) might differ regarding the outcomes. Further, the representativeness of our comparison group might be called into question. Whilst the original screening procedure identified a group of adolescents that was arguably representative of depressed adolescents in general, non-depressed peers (selected form the same educational programmes as the depressed adolescents) might not have been representative of non-depressed adolescents in general. However, register data obtained for a larger reference group from the normal population turned out to be almost identical to the non-depressed peers regarding all register outcomes. Finally, when generalizing from our results, one should reflect on the characteristics of the Swedish society. For instance, legislations on abortion differ fundamentally between countries. According to Swedish law, the woman herself can decide about abortion up until the 18th week. Of the Nordic countries, Sweden has the highest number of abortions per known pregnancy (25.3 per 100 known pregnancies in 2006) [39]. However, unwanted pregnancies in depressed females might be just as common in countries with less liberal abortion laws.
Conclusion
The broad range of investigated outcomes paints a bleak overall picture of how females with adolescent depression subsequently adjust to family-related aspects of adulthood. Both comorbid disruptive disorders and subsequent recurrence of depression appear to be important factors in this association. Attention should be brought to intimate relationship problems and sexual and reproductive health issues in young women with depression.
References
Afifi TO, Cox BJ, Enns MW (2006) Mental health profiles among married, never-married, and separated/divorced mothers in a nationally representative sample. Soc Psychiatry Psychiatr Epidemiol 41:122–129
Alio AP, Nana PN, Salihu HM (2009) Spousal violence and potentially preventable single and recurrent spontaneous fetal loss in an African setting: cross-sectional study. Lancet 373:318–324
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (1961) An inventory for measuring depression. Arch Gen Psychiatry 4:561–571
Berndt ER, Koran LM, Finkelstein SN, Gelenberg AJ, Kornstein SG, Miller IM, Thase ME, Trapp GA, Keller MB (2000) Lost human capital from early-onset chronic depression. Am J Psychiatry 157:940–947
Bond L, Toumbourou JW, Thomas L, Catalano RF, Patton G (2005) Individual, family, school, and community risk and protective factors for depressive symptoms in adolescents: a comparison of risk profiles for substance use and depressive symptoms. Prev Sci 6:73–88
Broy P, Berard A (2009) Gestational exposure to antidepressants and the risk of spontaneous abortion: a review. Curr Drug Deliv 7:76–92
Burke JD, Loeber R, Birmaher B (2002) Oppositional defiant disorder and conduct disorder: a review of the past 10 years, part II. J Am Acad Child Adolesc Psychiatry 41:1275–1293
Cairney J, Wade TJ (2002) Single parent mothers and mental health care service use. Soc Psychiatry Psychiatr Epidemiol 37:236–242
Campbell JC (2002) Health consequences of intimate partner violence. Lancet 359:1331–1336
Chen H, Cohen P, Johnson JG, Kasen S (2009) Psychiatric disorders during adolescence and relationships with peers from age 17 to age 27. Soc Psychiatry Psychiatr Epidemiol 44:223–230
Coddington RD (1972) The significance of life events as etiologic factors in disease of children. I. A survey of professional workers. J Psychosom Res 16:7–18
Cooper C, Bebbington PE, Meltzer H, Bhugra D, Brugha T, Jenkins R, Farrell M, King M (2008) Depression and common mental disorders in lone parents: results of the 2000 National Psychiatric Morbidity Survey. Psychol Med 38:335–342
Crosier T, Butterworth P, Rodgers B (2007) Mental health problems among single and partnered mothers. The role of financial hardship and social support. Soc Psychiatry Psychiatr Epidemiol 42:6–13
Daley SE, Hammen C (2002) Depressive symptoms and close relationships during the transition to adulthood: perspectives from dysphoric women, their best friends, and their romantic partners. J Consult Clin Psychol 70:129–141
Dingle K, Alati R, Clavarino A, Najman JM, Williams GM (2008) Pregnancy loss and psychiatric disorders in young women: an Australian birth cohort study. Br J Psychiatry 193:455–460
Ethier KA, Kershaw TS, Lewis JB, Milan S, Niccolai LM, Ickovics JR (2006) Self-esteem, emotional distress and sexual behavior among adolescent females: inter-relationships and temporal effects. J Adolesc Health 38:268–274
Fergusson DM (1998) Stability and change in externalising behaviours. Eur Arch Psychiatry Clin Neurosci 248:4–13
Fergusson DM, Woodward LJ (2002) Mental health, educational, and social role outcomes of adolescents with depression. Arch Gen Psychiatry 59:225–231
Fergusson DM, Horwood LJ, Ridder EM (2006) Abortion in young women and subsequent mental health. J Child Psychol Psychiatry 47:16–24
Fergusson DM, Boden JM, Horwood LJ (2007) Recurrence of major depression in adolescence and early adulthood, and later mental health, educational and economic outcomes. Br J Psychiatry 191:335–342
Fergusson DM, Boden JM, Horwood LJ (2007) Exposure to single parenthood in childhood and later mental health, educational, economic, and criminal behavior outcomes. Arch Gen Psychiatry 64:1089–1095
Gentile S (2008) Pregnancy exposure to serotonin reuptake inhibitors and the risk of spontaneous abortions. CNS Spectr 13:960–966
Gonzalez-Tejera G, Canino G, Ramirez R, Chavez L, Shrout P, Bird H, Bravo M, Martinez-Taboas A, Ribera J, Bauermeister J (2005) Examining minor and major depression in adolescents. J Child Psychol Psychiatry 46:888–899
Gotlib IH, Lewinsohn PM, Seeley JR (1995) Symptoms versus a diagnosis of depression: differences in psychosocial functioning. J Consult Clin Psychol 63:90–100
Gotlib IH, Lewinsohn PM, Seeley JR (1998) Consequences of depression during adolescence: marital status and marital functioning in early adulthood. J Abnorm Psychol 107:686–690
Hammen C (2003) Interpersonal stress and depression in women. J Affect Disord 74:49–57
Jenkins R, Meltzer H, Bebbington P, Brugha T, Farrell M, McManus S, Singleton N (2009) The British Mental Health Survey Programme: achievements and latest findings. Soc Psychiatry Psychiatr Epidemiol 44:899–904
Jonsson U, Bohman H, Hjern A, von Knorring L, Olsson G, von Knorring AL (2010) Subsequent higher education after adolescent depression: a 15-year follow-up register study. Eur Psychiatry, (in press)
Kendler KS, Gardner CO, Prescott CA (2002) Toward a comprehensive developmental model for major depression in women. Am J Psychiatry 159:1133–1145
Kendler KS, Gardner CO, Prescott CA (2006) Toward a comprehensive developmental model for major depression in men. Am J Psychiatry 163:115–124
Kessler RC, Walters EE, Forthofer MS (1998) The social consequences of psychiatric disorders, III: probability of marital stability. Am J Psychiatry 155:1092–1096
Kessler RC, Berglund PA, Foster CL, Saunders WB, Stang PE, Walters EE (1997) Social consequences of psychiatric disorders, II: Teenage parenthood. Am J Psychiatry 154:1405–1411
Lehrer JA, Shrier LA, Gortmaker S, Buka S (2006) Depressive symptoms as a longitudinal predictor of sexual risk behaviors among US middle and high school students. Pediatrics 118:189–200
Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH (2003) Psychosocial functioning of young adults who have experienced and recovered from major depressive disorder during adolescence. J Abnorm Psychol 112:353–363
Loeber R, Burke JD, Lahey BB, Winters A, Zera M (2000) Oppositional defiant and conduct disorder: a review of the past 10 years, part I. J Am Acad Child Adolesc Psychiatry 39:1468–1484
Mathews CA, Reus VI (2001) Assortative mating in the affective disorders: a systematic review and meta-analysis. Compr Psychiatry 42:257–262
Mazza JJ, Abbott RD, Fleming CB, Harachi TW, Cortes RC, Park J, Haggerty KP, Catalano RF (2009) Early predictors of adolescent depression: a 7 year longitudinal study. J Early Adolesc 29:664–692
O’Donnell L, Agronick G, Duran R, Myint UA, Stueve A (2009) Intimate partner violence among economically disadvantaged young adult women: associations with adolescent risk-taking and pregnancy experiences. Perspect Sex Reprod Health 41:84–91
Official Statistics of Sweden (2009) Induced abortion 2008. http://www.socialstyrelsen.se/Lists/Artikelkatalog/Attachments/8301/2009-125-10_200912510_rev3.pdf. Accessed 12 May 2010
Olsson GI, von Knorring AL (1999) Adolescent depression: prevalence in Swedish high-school students. Acta Psychiatr Scand 99:324–331
Olsson GI, Nordstrom ML, Arinell H, von Knorring AL (1999) Adolescent depression: social network and family climate—a case-control study. J Child Psychol Psychiatry 40:227–237
Paradis AD, Reinherz HZ, Giaconia RM, Fitzmaurice G (2006) Major depression in the transition to adulthood: the impact of active and past depression on young adult functioning. J Nerv Ment Dis 194:318–323
Puig-Antich J, Kaufman J, Ryan ND, Williamson DE, Dahl RE, Lukens E, Todak G, Ambrosini P, Rabinovich H, Nelson B (1993) The psychosocial functioning and family environment of depressed adolescents. J Am Acad Child Adolesc Psychiatry 32:244–253
Rao U, Chen LA (2009) Characteristics, correlates, and outcomes of childhood and adolescent depressive disorders. Dialogues Clin Neurosci 11:45–62
Rehman US, Gollan J, Mortimer AR (2008) The marital context of depression: research, limitations, and new directions. Clin Psychol Rev 28:179–198
Reich W, Herjanic B, Welner Z, Gandhy PR (1982) Development of a structured psychiatric interview for children: agreement on diagnosis comparing child and parent interviews. J Abnorm Child Psychol 10:325–336
Rubin AG, Gold MA, Primack BA (2009) Associations between depressive symptoms and sexual risk behavior in a diverse sample of female adolescents. J Pediatr Adolesc Gynecol 22:306–312
Sander JB, McCarty CA (2005) Youth depression in the family context: familial risk factors and models of treatment. Clin Child Fam Psychol Rev 8:203–219
Sarkar NN (2008) The impact of intimate partner violence on women’s reproductive health and pregnancy outcome. J Obstet Gynaecol 28:266–271
Schoenbach VJ, Kaplan BH, Grimson RC, Wagner EH (1982) Use of a symptom scale to study the prevalence of a depressive syndrome in young adolescents. Am J Epidemiol 116:791–800
Sheeber L, Hops H, Davis B (2001) Family processes in adolescent depression. Clin Child Fam Psychol Rev 4:19–35
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC (1998) The Mini-International Neuropsychiatric Interview M.I.N.I.: the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 59(suppl 20):22–33 quiz 34–57
Simonoff E, Elander J, Holmshaw J, Pickles A, Murray R, Rutter M (2004) Predictors of antisocial personality. Continuities from childhood to adult life. Br J Psychiatry 184:118–127
Statistics Sweden (1982) http://www.scb.se/Grupp/Hitta_statistik/Forsta_Statistik/Klassifikationer/_Dokument/SEI-AGG_Eng.pdf. Accessed 12 May 2010
Statistics Sweden (2008) Tables on the population in Sweden 2007. http://www.scb.se/statistik/_publikationer/BE0101_2007A01_BR_00_BE0108TAB.pdf. Accessed 12 May 2010
Weitoft GR, Hjern A, Haglund B, Rosen M (2003) Mortality, severe morbidity, and injury in children living with single parents in Sweden: a population-based study. Lancet 361:289–295
Whisman MA (2007) Marital distress and DSM-IV psychiatric disorders in a population-based national survey. J Abnorm Psychol 116:638–643
Zisook S, Lesser I, Stewart JW, Wisniewski SR, Balasubramani GK, Fava M, Gilmer WS, Dresselhaus TR, Thase ME, Nierenberg AA, Trivedi MH, Rush AJ (2007) Effect of age at onset on the course of major depressive disorder. Am J Psychiatry 164:1539–1546
Acknowledgments
We thank H. Arinell, B.Sc. for his support regarding statistics and data files. The study was supported by the Swedish Council for Working Life and Social Research (FAS), the Märta and Nicke Nasvell Foundation and the foundation in memory of Professor Bror Gadelius.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jonsson, U., Bohman, H., Hjern, A. et al. Intimate relationships and childbearing after adolescent depression: a population-based 15 year follow-up study. Soc Psychiatry Psychiatr Epidemiol 46, 711–721 (2011). https://doi.org/10.1007/s00127-010-0238-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-010-0238-7