Abstract
Background
Previous studies have reported a very high incidence of schizophrenia for immigrant ethnic groups in Western Europe. The explanation of these findings is unknown, but is likely to involve social stress inherent to the migrant condition. A previous study reported that the incidence of schizophrenia in ethnic groups was higher when these groups perceived more discrimination. We conducted a case-control study of first-episode schizophrenia, and investigated whether perceived discrimination at the individual level is a risk factor for schizophrenia.
Methods
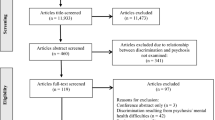
Cases included all non-western immigrants who made first contact with a physician for a psychotic disorder in The Hague, the Netherlands, between October 2000 and July 2005, and received a diagnosis of a schizophrenia spectrum disorder (DSM IV: schizophrenia, schizophreniform disorder, schizoaffective disorder) (N = 100). Two matched control groups were recruited, one among immigrants who made contact with non-psychiatric secondary health care services (N = 100), and one among siblings of the cases (N = 63). Perceived discrimination in the year before illness onset was measured with structured interviews, assessing experiences of prejudice, racist insults or attacks, and perception of discrimination against one’s ethnic group. Conditional logistic regression analyses were used to predict schizophrenia as a function of perceived discrimination.
Results
Cases reported somewhat higher rates of perceived discrimination in the year prior to illness onset than their siblings and the general-hospital controls, but these differences were not statistically significant; 52% of the cases and 42% of both control groups had perceived any discrimination. Perceived discrimination at the individual level was not a risk factor for schizophrenia in these data. Perceived discrimination was positively correlated with cultural distance and cannabis use, and negatively with ethnic identity, self-esteem, and mastery.
Conclusions
The relationship between racial discrimination and psychosis may vary with the aspect of discrimination that is studied, and may also depend upon the social context in which discrimination takes place.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of schizophrenia and other psychotic disorders is very high among ethnic minority groups in western Europe [15, 37]. Racial discrimination has been suggested as a possible explanation for this increased incidence [4, 29], but although many studies have shown that discrimination has a pervasive, adverse influence on health of ethnic minority populations [39], the relationship between discrimination and mental health is poorly understood [5] and research of the association between discrimination and psychosis is scarce [40]. Two cross-sectional studies found an association between perceived discrimination and the prevalence of psychotic symptoms [18, 19], and a prospective study in the Netherlands suggested that perceived discrimination (albeit not only racial, but any discrimination) may induce the onset of delusional ideations [16]. We have previously reported that the incidence of psychotic disorders in The Hague, the Netherlands, varied across ethnic minority groups by degree of perceived discrimination: the incidence was higher when groups perceived more discrimination [36]. Within an ethnic group, however, individual perceptions of discrimination vary, and may influence disease risk. These individual variations may depend upon many factors, including gender, educational level, generation, cultural distance, ethnic density, social support, self- esteem and ethnic identity [26, 38, 39].
There is hardly any published research on discrimination as risk factor for schizophrenia at the individual level. Results from one recent study suggested that the higher incidence of schizophrenia and other psychotic disorders in Black people in the UK is partly mediated by individual perceptions of disadvantage [7]. The present case-control study of first episode schizophrenia among ethnic minorities in The Hague aimed to investigate the association between perceived discrimination and schizophrenia and to explore factors that influence degree of perceived discrimination at the individual level.
Method
Classification of ethnicity
We used the classification of ethnicity as defined by the Netherlands’ Bureau of Statistics. If a citizen, or (one of) his or her parents, was born abroad, he or she is assigned to the group of people born in the same country. If the parents were born in different foreign countries, the country of birth of the mother determines the assignment to a particular group.
Participants
Cases
All first or second generation immigrants from non-western countries (of which 85% from Surinam, Morocco, Turkey, or Netherlands-Antilles), aged 18–54 years, who made first contact with a physician in The Hague for a psychotic disorder and received a diagnosis of a schizophrenia spectrum disorder (DSM IV: schizophrenia, schizophreniform disorder, schizoaffective disorder) between October 1, 2000 and July 1, 2005, were eligible for the study. Case-finding procedures and diagnostic protocol of the study have been described elsewhere [37]. If the patient had been adopted as a child, he or she was excluded (N = 4).
Controls
For each patient, two control subjects were recruited, matched for 5-year age-group, sex, and ethnicity (including generation). They were screened for psychotic symptoms (see “Measures”), and were excluded if these were present (N = 5).
The first control group was recruited among the general ethnic minority population of The Hague. To minimize selection bias as a result of pathways to care, the controls were selected from immigrants who made contact with non-psychiatric secondary health care services. Controls were recruited from the outpatient departments of internal medicine and surgery of a general hospital. The reasons for making contact with these departments differed widely, and included: lipoma or naevus (N = 15), fracture (N = 8), contusion (N = 11), haemorrhoids (N = 8), sinus pilonidalis (N = 5), anal fissure (N = 5), inflammatory bowel disease (N = 5), diabetes mellitus (N = 5), and other, less frequent diagnoses (N = 38).
The second control group consisted of siblings of the patients, in order to (partially) control for genetic factors and to control implicitly for unmeasured shared socio-environmental confounding factors.
All participants gave written informed consent for the study. The study was approved by the local ethics committee. Structured interviews were conducted by a resident in psychiatry (WV) and four trained research assistants. If participants did not speak Dutch sufficiently (N = 9), trained research assistants (N = 3) who were native speakers in Turkish, Kurdish, Urdu, Arabic or Berber, conducted the interviews. Because we expected this in advance to concern only a small minority of the sample, we neither developed nor maintained a protocol for translation and back-translation of the questionnaires.
Participants were instructed to answer according to their experiences in the year before illness onset. When prodromal symptoms could be identified, the occurrence of these was chosen as moment of illness onset; for the minority of the patients that did not recognize any prodromal symptoms, illness onset was defined as the date of first psychotic symptoms.
Measures
Psychotic symptoms
In control subjects, the psychosis section of the composite International Diagnostic Interview (CIDI), Version 2.1 [30], was administered.
Perceived discrimination
This scale was developed by the International Comparative Study of Ethnocultural Youth (ICSEY) [1], a study among more than 10,000 adolescents from 30 ethnic groups in 13 countries, which included Surinamese, Turkish and Antillean immigrants in the Netherlands. The scale is an ordinal measure; response options range from “strongly disagree” (1) to “strongly agree” (5). The scale consists of five items:
-
(1)
I think that others have behaved in an unfair or negative way towards my ethnic group;
-
(2)
I do not feel accepted by Dutch people;
-
(3)
I feel Dutch people have something against me;
-
(4)
I have been teased or insulted because of my ethnic background;
-
(5)
I have been threatened or attacked because of my ethnic background.
We used the total scale score as a measure of perceived discrimination. For further exploration, we also used item (1) as a separate measure of perceived discrimination against one’s own group, and items (2), (3), (4) and (5) as perceived individual discrimination. Finally, for the total and for the exploratory measures, dichotomous variables were created. Responses of “Somewhat agree” or “Strongly agree” on any of the items were classified as “Yes”, all other scores as “No”.
Other measures
We assessed several socio-demographic and social factors that previously have been associated with perceived discrimination or schizophrenia, and may be considered as potential confounding or mediating factors in their relationship. Socio-economic status was assessed with level of education (no or primary, secondary, or higher education) and employment status (unemployed or else). Information was noted on marital status (single or else) and on lifetime cannabis use (use defined as more than five times). Cultural distance, defined as differences with the mainstream host culture in attitudes towards and opinions about social relationships, religion and society, was measured with 25 statements involving emancipation, autonomy and authority, secularization, and moral values (adapted from [8]). Ethnic density was calculated as the proportion of members of one’s own ethnic group living in the neighbourhood. The required population data were provided by the municipal authorities [38]. Measures of ethnic identity and mastery were adapted from the International Comparative Study of Ethnocultural Youth (ICSEY) [1]. The scale of Ethnic identity assesses ethnic affirmation and feelings about being a group member and the Mastery scale assesses the extent to which one experiences to be in control of his or her own life [1]. We also used the 15-item Rosenberg self-esteem scale [27], and the 12-item shortened social support scale [33]. In this paper, we address the associations of these measures with perceived discrimination; the separate results will be reported elsewhere.
Validity and reliability
For each ICSEY scale it has been shown that it measures the same psychological construct in all ethnic groups, as all Tucker’s phis, a measure of agreement [32], were 0.90 or higher [1]. The measures have shown good to excellent internal reliability as well (Cronbach’s alphas > 0.70) [1]. Cronbach’s alphas in our sample were good to excellent for mastery (0.70), Ethnic identity (0.81), perceived discrimination (0.81), self-esteem (0.83), and perceived social support (0.85). Factor analyses of the cultural distance subscales showed that these could be combined into one factor (loadings 0.49–0.79, eigenvalue 1.9, explained variance 47%). In two sub-samples we investigated inter-rater reliability (N = 23) and test–retest reliability after 1 week (N = 24) of the scales. Intra-class coefficients were 0.85–0.99 and 0.63–0.96, respectively.
Key informants
For all participants, key informants were asked to complete a short version of the structured interview for their relatives, which included items (4) and (5) of the perceived discrimination scale.
Statistical analyses
Stata Version 9.2 was used for all statistical analyses. The matched case-control design required conditional (fixed-effects) logistic regression techniques. First, the total scale score, as well the exploratory and the dichotomous measures, were entered separately in the regression models. Comparisons were made between cases and general-hospital controls (100 pairs), and between cases and sibling controls (63 pairs). If there were significant differences between groups, the other variables were added to the regression model to adjust for confounding.
Second, in the total sample, we calculated bivariate Pearson’s correlations between total perceived discrimination and the other scale scores. Associations between perceived discrimination and dichotomous variables were tested with χ2 tests.
Additional analyses addressed the issue of information bias. The scores of participants on items (4) and (5) were compared to the scores provided by their key informants with use of conditional logistic regression. We only used dichotomized scores, because many key informants answered (3) “I do not know”. Responses of “Somewhat agree” or “Strongly agree” on any of the items were classified as “Yes”, all other scores as “No”.
Results
Of the 146 patients who were eligible for the study, two patients had deceased before the present study was conducted. Twenty-six patients could not be interviewed, because they had remigrated to their home country (N = 5), they were too ill during the entire study period (N = 8) or because there was no current address available (N = 13). Of the 118 patients who were contacted, 18 refused to participate. Thus, 100 patients were interviewed. Of the 168 subjects in the general-hospital control group who were matched to the schizophrenia patients, four subjects were physically too ill to be interviewed, one was mentally handicapped, three were excluded because they had a psychotic disorder, and 60 refused to participate. For 15 patients there was no sibling available, because all siblings were too young or lived abroad, patients had no sibling, or patients did not know their current address. Nine patients refused permission to contact their siblings, two patients only had a sibling who had psychotic symptoms. For 11 of the remaining 74 patients, the siblings refused to participate. Thus, siblings of 63 patients could be interviewed. Socio-demographic characteristics of the study sample are shown in Table 1.
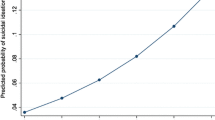
Fifty two percent of the cases and 42% of both control groups reported experiences of discrimination (Tables 2, 3), but this difference was not statistically significant. The other measures of perceived discrimination did not yield statistically significant differences between cases and controls either, except that cases reported more personal experiences of discrimination than general-hospital controls (OR per unit increase of the scale = 1.08 [95% CI, 1.01–1.17], Table 2).
After adjustment for unemployment, level of education, marital status, cultural distance, mastery, ethnic identity, self-esteem, social support, and cannabis use, there were no statistically significant differences in perceived discrimination between cases and controls (results not shown for comparisons between cases and siblings).
In the total sample, perceived discrimination was reported more often by males than by females (50 vs. 37%, χ2 = 3.98, df = 1, P = 0.046), and by those with a history of cannabis use (55 vs. 41% in non-users, χ2 = 4.69, df = 1, P = 0.03). There were no significant differences in prevalence of discrimination with regard to generation, unemployment, level of education, and marital status. Table 4 shows correlations between perceived discrimination and ethnic density, ethnic identity, cultural distance, social support, mastery, and self-esteem. Perceived discrimination was positively correlated with cultural distance, and negatively correlated with ethnic identity, mastery and self-esteem.
Information from key informants was available for 43 cases, 37 siblings and 45 general-hospital controls. As was found with the self-report measure, cases were reported to have perceived discrimination somewhat more often than controls (Table 5). In all groups, the proportions of self-reported perceived discrimination were higher than those reported by their key informants, but these differences were not statistically significant.
Discussion
Racial discrimination has been suggested to explain the consistent finding of an increased incidence of schizophrenia in ethnic minority groups in western Europe [4], but to date, the association between discrimination and schizophrenia has hardly been studied [7, 36]. In this case-control study of first-episode schizophrenia among non-western immigrants, individuals who developed schizophrenia reported somewhat higher rates of perceived discrimination in the year prior to illness onset than their siblings and matched general-hospital controls, but the differences were not statistically significant. A considerable proportion of all groups (52% of the cases and 42% of both control groups) had perceived discrimination.
These results suggest that there may be no direct and strong relationship between perceived discrimination at the individual level and the development of schizophrenia. A previous study showed that the incidence of psychotic disorders in The Hague was higher when ethnic minority groups experienced more discrimination [36], and other studies reported associations between perceived discrimination and the prevalence or the onset of psychosis [16, 18, 19]. The heterogeneity of these findings may depend upon the aspect of discrimination that is studied and the way it is measured [39], but also upon social and psychological factors that have been shown to influence the perception and impact of discrimination [5, 6, 40].
Measure of discrimination
Racial discrimination adversely affects mental health in at least three different ways [40]. Interpersonal experiences of racist insults or violence have been related to psychological distress, depression, low self-esteem [39], and, as noted earlier, psychosis [18, 19]. Structural discrimination by institutions, as in employment policies or access to education or housing facilities, also has a deleterious influence on health [23, 40], not only because it leads to lower socio-economic status, which has been linked to the increased incidence of schizophrenia among ethnic minorities [14], but also because the gap between aspirations and achievements may give rise to feelings of humiliation and social defeat, factors that may be involved in the aetiology of schizophrenia [22, 28]. Finally, awareness of prevailing negative cultural stereotypes has been associated with poor mental health and academic underachievement, independent of personal experiences of racist insults or violence [6, 17, 31]. Our measure of discrimination assessed the individual’s perceptions of discrimination with five statements that may not have captured all aspects of racial discrimination. Particularly, experiences of institutional racism and negative stereotyping may have been missed. The previous finding of a relationship between the incidence of psychotic disorders and ethnic groups’ experience of discrimination [36] suggests that these aspects of discrimination may be relevant for schizophrenia.
Cases may have underreported experiences of discrimination. Recall bias may have occurred because of cognitive impairments due to the illness, or because the recent experience of first psychosis was so overwhelming that memories of negative experiences before onset of illness have faded. This is unlikely to account for the results, however, as the reports of key informants showed a similar pattern to the self-report data (it should be noted that this information was available only for 43 cases) (Table 5). Also, a study from the UK found that, although ethnic minority schizophrenia patients experienced similar numbers of life events to white British patients, they attributed these more often to discrimination [11]. Thus, there is no evidence that ethnic minority patients would underreport racial discrimination.
Context of discrimination
Given the relatively high prevalence of perceived discrimination in these data, another explanation for the results may be that the experience of discrimination itself is not sufficient, but that the development of schizophrenia depends upon other factors, such as the social context in which discrimination takes place. Recent studies have shown that neighbourhood-level socioenvironmental factors influence the incidence of schizophrenia [20]. Among ethnic minorities, the incidence is lower when they live in neighbourhoods with a high percentage of members of their own ethnic group [2, 38], or where ethnic fragmentation is low [21]. A mechanism possibly underlying these findings is that pathogenic effects of discrimination are buffered or prevented in high ethnic density neighbourhoods, by social support [25], social capital [21] and strong ethnic identity [10], factors that may be greater in high ethnic density neighbourhoods [12]. Thus, while the degree of perceived discrimination may be similar among cases and controls, social support and ethnic identity may eventually determine the risk of schizophrenia. If such resources are scarce, the social stress resulting from these difficulties may exceed the coping ability of individuals with a genetic vulnerability to schizophrenia, who often have impaired executive function [3]. When subjected to such a severe challenge, they may be more likely to develop the disorder [9].
This hypothesis is consistent with the directions of the correlations that we found in our data. Perceived discrimination was negatively correlated with ethnic density, ethnic identity, mastery and self-esteem, and positively with cultural distance; ethnic density was positively correlated with ethnic identity and social support; and ethnic identity was positively correlated with social support, cultural distance, mastery, and self-esteem (Table 4).
Cannabis is frequently used by patients with early psychosis [34]. It has been related to psychotic symptoms [24] and is likely to increase the risk of developing schizophrenia [13]. In our data, cannabis use was not only strongly associated with schizophrenia [35], but was also correlated with perceived discrimination. It is conceivable that perceived discrimination leads to cannabis use, for instance because individuals may use it to alleviate the stress that is brought about by experiences of discrimination.
Other methodological considerations
The power of study was too low to detect small effects. It was designed to investigate potential explanations for the substantially increased incidence rates of schizophrenia among ethnic minorities (for instance, the incidence rate ratio for first- and second-generation Moroccans in The Hague was 4.0 [95% CI, 2.5–6.3] and 5.8 [2.9–11.4], respectively, compared to the indigenous Dutch population [37]). To explain an increase of this magnitude requires a causal factor with a strong effect. Thus, even if perceived discrimination at the individual level would be associated with schizophrenia, it is unlikely that it is a strong risk factor in itself.
All consecutive first-episode schizophrenia cases between 2000 and 2005 were eligible for the study, but not all patients participated. It is conceivable that those individuals who believed to be discriminated against more often refused to participate. However, the same selection bias would occur in the control groups.
The general-hospital controls may not have been representative for the general immigrant population, but the choice for a control group selected from immigrants who made contact with non-psychiatric secondary health care services minimized selection bias as a result of pathways to care, as the schizophrenia cases were also recruited from secondary psychiatric services. In addition, the very diverse complaints for which the controls made contact makes it very unlikely that their somatic illness would be related to perceived discrimination.
Conclusion
Perceived discrimination at the individual level was not a strong risk factor for schizophrenia in these data. The relationship between racial discrimination and psychosis may vary with the aspect of discrimination that is studied, and may also depend upon the social context in which discrimination takes place.
References
Berry JW, Phinney JS, Sam DL, Vedder PE (2006) Immigrant youth in cultural transition. Acculturation, identity, and adaptation across national contexts. Lawrence Erlbaum Associates, Mahwah
Boydell J, van Os J, McKenzie K, Allardyce J, Goel R, McCreadie RG, Murray RM (2001) Incidence of schizophrenia in ethnic minorities in London: ecological study into interactions with environment. Br Med J 323:1336–1338
Cannon TD, Zorrilla LE, Shtasel D, Gur RE, Gur RC, Marco EJ, Moberg P, Price RA (1994) Neuropsychological functioning in siblings discordant for schizophrenia and healthy volunteers. Arch Gen Psychiatry 51:651–661
Cantor-Graae E, Selten JP (2005) Schizophrenia and migration: a meta-analysis and review. Am J Psychiatry 162:12–24
Chakraborty A, McKenzie K (2002) Does racial discrimination cause mental illness? Br J Psychiatry 180:475–477
Clark R, Anderson NB, Clark VR, Williams DR (1999) Racism as a stressor for African Americans. Am Psychol 54:805–816
Cooper C, Morgan C, Byrne M, Dazzan P, Morgan K, Hutchinson G, Doody GA, Harrison G, Leff J, Jones P, Ismail K, Murray R, Bebbington PE, Fearon P (2008) Perceptions of disadvantage, ethnicity and psychosis. Br J Psychiatry 192:185–190
Dagevos J (2001) Perspective on integration. The socio-cultural and structural integration of ethnic minorities in the Netherlands. The Netherlands Scientific Council for Government Policy, WRR, The Hague
Eaton W, Harrison G (2001) Life chances, life planning, and schizophrenia. A review and interpretation of research on social deprivation. Int J Mental Health 30:58–81
Fischer AR, Shaw CM (1999) African Americans’ mental health and perceptions of racist discrimination: the moderating effects of racial socioalization experiences and self-esteem. J Couns Psychol 46:395–407
Gilvarry CM, Walsh E, Samele C, Hutchinson G, Mallett R, Rabe-Hesketh S, Fahy T, van Os J, Murray RM (1999) Life events, ethnicity and perceptions of discrimination in patients with severe mental illness. Soc Psychiatry Psychiatr Epidemiol 34:600–608
Halpern D (1993) Minorities and mental health. Soc Sci Med 36:597–607
Henquet C, Krabbendam L, Spauwen J, Kaplan C, Lieb R, Wittchen HU, van Os J (2005) Prospective cohort study of cannabis use, predisposition for psychosis, and psychotic symptoms in young people. Br Med J 330:11
Hjern A, Wicks S, Dalman C (2004) Social adversity contributes to high morbidity in psychoses in immigrants—a national cohort study in two generations of Swedish residents. Psychol Med 34:1025–1033
Hutchinson G, Haasen C (2004) Migration and schizophrenia; the challenges for European psychiatry and implications for the future. Soc Psychiatry Psychiatr Epidemiol 39:350–357
Janssen I, Hanssen M, Bak M, Bijl RV, de Graaf R, Vollebergh W, McKenzie K, van Os J (2003) Discrimination and delusional ideation. Br J Psychiatry 182:71–76
Karlsen S, Nazroo JY (2004) Fear of racism and health. J Epidemiol Commun Health 58:1017–1018
Karlsen S, Nazroo JY (2002) Relation between racial discrimination, social class, and health among ethnic minority groups. Am J Public Health 92:624–631
Karlsen S, Nazroo JY, McKenzie K, Bhui K, Weich S (2005) Racism, psychosis and common mental disorder among ethnic minority groups in England. Psychol Med 35:1–9
Kirkbride JB, Fearon P, Morgan C, Dazzan P, Morgan K, Murray RM, Jones PB (2007) Neighbourhood variation in the incidence of psychotic disorders in Southeast London. Soc Psychiatry Psychiatr Epidemiol 42:438–445
Kirkbride JB, Morgan C, Fearon P, Dazzan P, Murray RM, Jones PB (2007) Neighbourhood-level effects on psychoses: re-examining the role of context. Psychol Med 37:1413–1425
Kleiner RJ, Parker S (1963) Goal-striving, social status, and mental disorder: a research review. Am Sociol Rev 28:189–203
Meyer IH (2003) Prejudice and stress: conceptual and measurement problems. Am J Public Health 93:262–265
Miller P, Lawrie SM, Hodges A, Clafferty R, Cosway R, Johnstone EC (2001) Genetic liability, illicit drug use, life stress and psychotic symptoms: preliminary findings from the Edinburgh study of people at high risk for schizophrenia. Soc Psychiatry Psychiatr Epidemiol 36:338–342
Noh S, Kaspar V (2003) Perceived discrimination and depression: moderating effects of coping, acculturation, and ethnic support. Am J Public Health 93:232–238
Phinney JS (2003) Ethnic identity and acculturation. In: Chun KM, Balls Organista P, Marin G (eds) Acculturation: advances in theory, measurement and applied research. American Psychological Association, Washington, DC, pp 63–82
Rosenberg M (1965) Society and the adolescent self-image. Princeton University Press, Princeton
Selten JP, Cantor-Graae E (2005) Social defeat: risk factor for schizophrenia? Br J Psychiatry 187:101–102
Sharpley MS, Hutchinson G, Murray RM, McKenzie K (2001) Understanding the excess of psychosis among the African–Caribbean population in England: review of current hypotheses. Br J Psychiatry 178:S60–68
Smitten MH, Smeets RMW, Van den Brink W (1998) Composite international diagnostic interview (CIDI), Version 2.1. World Health Organization, Amsterdam
Steele CM (1997) A threat in the air. How stereotypes shape intellectual identity and performance. Am Psychol 52:613–629
Van de Vijver FJR, Leung K (1997) Methods and data analysis for cross-cultural research. Sage, Thousand Oaks
Van Eijk LM, van Kempen GIJM, van Sonderen FLP (1994) A short scale for measuring social support in the elderly: the SSL12-I. Tijdschr Gerontol Geriatr 25:192–196
Van Mastrigt S, Addington J, Addington D (2004) Substance misuse at presentation to an early psychosis program. Soc Psychiatry Psychiatr Epidemiol 39:69–72
Veling W, Mackenbach JP, Van Os J, Hoek HW (2008) Cannabis use and genetic predisposition for schizophrenia: a case-control study. Psychol Med. doi:10.1017/s00332g1708003474
Veling W, Selten JP, Susser E, Laan W, Mackenbach JP, Hoek HW (2007) Discrimination and the incidence of psychotic disorders among ethnic minorities in the Netherlands. Int J Epidemiol 36:761–768
Veling W, Selten JP, Veen N, Laan W, Blom JD, Hoek HW (2006) Incidence of schizophrenia among ethnic minorities in the Netherlands: a 4-year first-contact study. Schizophr Res 86:189–193
Veling W, Susser E, Van Os J, Mackenbach JP, Selten JP, Hoek HW (2008) Ethnic density of neighborhoods and incidence of psychotic disorders among immigrants. Am J Psychiatry 165:66–73
Williams DR, Neighbors HW, Jackson JS (2003) Racial/ethnic discrimination and health: findings from community studies. Am J Public Health 93:200–208
Williams DR, Williams-Morris R (2000) Racism and mental health: the African American experience. Ethn Health 5:243–268
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Veling, W., Hoek, H.W. & Mackenbach, J.P. Perceived discrimination and the risk of schizophrenia in ethnic minorities. Soc Psychiat Epidemiol 43, 953–959 (2008). https://doi.org/10.1007/s00127-008-0381-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-008-0381-6