Abstract
Aims/hypothesis
We aimed to investigate the genetic evidence that supports the repurposing of drugs already licensed or in clinical phases of development for prevention of type 1 diabetes.
Methods
We obtained genome-wide association study summary statistics for the risk of type 1 diabetes, whole-blood gene expression and serum protein levels and investigated genetic polymorphisms near seven potential drug target genes. We used co-localisation to examine whether the same genetic variants that are associated with type 1 diabetes risk were also associated with the relevant drug target genetic proxies and used Mendelian randomisation to evaluate the direction and magnitude of the associations. Furthermore, we performed Mendelian randomisation analysis restricted to functional variants within the drug target genes.
Results
Co-localisation revealed that the blood expression levels of IL2RA (encoding IL-2 receptor subunit α [IL2RA]), IL6R (encoding IL-6 receptor [IL6R]) and IL6ST (encoding IL-6 cytokine family signal transducer [IL6ST]) shared the same causal variant with type 1 diabetes liability near the corresponding genes (posterior probabilities 100%, 96.5% and 97.0%, respectively). The OR (95% CI) of type 1 diabetes per 1-SD increase in the genetically proxied gene expression of IL2RA, IL6R and IL6ST were 0.22 (0.17, 0.27), 1.98 (1.48, 2.65) and 1.90 (1.45, 2.48), respectively. Using missense variants, genetically proxied TYK2 (encoding tyrosine kinase 2) expression levels were associated with type 1 diabetes risk (OR 0.61 [95% CI 0.54, 0.69]).
Conclusions/interpretation
Our findings support the targeting of IL-2, IL-6 and TYK2 signalling in prevention of type 1 diabetes.
Data availability
The analysis code is available at https://github.com/jkoskenniemi/T1DSCREEN, which also includes instructions on how to download the original GWAS summary statistics.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Type 1 diabetes is an autoimmune disease characterised by the loss of beta cell function. Despite advances in continuous glucose monitoring and insulin administration, managing type 1 diabetes remains a significant burden and few individuals reach glycaemic targets [1]. Several drugs have shown potential in delaying the loss in beta cell function in newly diagnosed diabetes [2] and teplizumab, a monoclonal anti-CD3 antibody, even delayed the onset of the clinical disease by a median of 2 years [3]. However, no current therapy can completely halt the disease progression and therefore it is crucial to identify new efficacious drug targets.
Drug targets backed by genetic evidence have higher success rates in clinical development [4]. Genome-wide association studies (GWAS) enable the discovery of genomic regions strongly associated with the disease of interest. These associations can be considered as evidence for the involvement of the corresponding proteins in the disease pathogenesis, implying that these proteins are potential drug targets for the disease. The evidence for a likely drug target can be further investigated via co-localisation and Mendelian randomisation. Co-localisation can be used to study whether the same causal variant is shared between the drug target and the disease liability or whether the loci of the risk allele and an allele influencing the drug target are distinct [5]. Furthermore, Mendelian randomisation can be used to assess how much the genetic variability in drug target levels affects the risk of a disease in the population [6].
To inform the prioritisation of targets for prevention of type 1 diabetes, we aimed to investigate the genetic evidence for the efficacy of 12 drug targets in prevention of type 1 diabetes. These targets were selected because a prior GWAS reported that they are associated with the risk of type 1 diabetes and drugs that target them are already licensed for indications other than type 1 diabetes or have progressed to clinical development (see electronic supplementary material [ESM] Table 1).
Methods
Study design
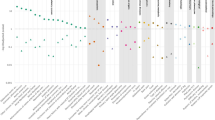
We selected the drug targets based on a previous GWAS of type 1 diabetes by Robertson et al [7] (Table 1 and ESM Fig. 1). Using a priority index, we ranked the drugs based on the following four factors: (1) existence of genetic variant(s) close to the potential target; (2) chromatin accessibility; (3) gene expression data in relevant cell types; and (4) protein–protein interactions [8]. We focused on 12 proteins (IL-2 receptor subunit α [IL2RA], IL-2 receptor subunit β [IL2RB], IL-2 receptor subunit γ [IL2RG], IL-6 receptor [IL6R], IL-6 cytokine family signal transducer [IL6ST], IL-12 subunit β [IL12B], IL-23 subunit α [IL23A], IFN-α and -β receptor subunit 2 [IFNAR2], Janus kinase 1 [JAK1], Janus kinase 2 [JAK2], Janus kinase 3 [JAK3] and tyrosine kinase 2 [TYK2]) that have already been targeted in clinical trials for autoimmune diseases and some of which have been licensed for indications other than type 1 diabetes (ESM Table 1) [7]. Among these targets, eight target genes (IL2RA, IL2RB, IL6R, IL6ST, IL23A, JAK2, JAK3, TYK2) had a locus associated with the risk of type 1 diabetes (p<1 × 10−5) within a distance of 1 million base pairs from the target gene (see ESM Fig. 2). IL23A was excluded from the analyses because data on its circulating levels were unavailable, leaving seven targets for the subsequent analyses. Genomic regions under investigation are listed in Table 1.
All primary studies that generated the GWAS summary statistics used in our analysis have undergone institutional board review, have received ethical approval and were conducted according to declaration of Helsinki [9,10,11].
Participants
We obtained the GWAS summary statistics for type 1 diabetes, whole-blood gene expression (expression quantitative trait loci [eQTL]) and serum protein levels (protein quantitative trait loci [pQTL]) (ESM Table 2). eQTL data were used for loci near the drug target genes since they encode intracellular or membrane-bound proteins. However, pQTL data were also analysed for loci in the vicinity of IL6ST and IL6R genes, since soluble forms of their proteins (gp130 and IL-6 receptor [IL-6R], respectively) may also modulate IL-6 signalling (see ESM Fig. 3) [12]. We included loci within 1 million base pairs of the seven potential drug target genes (Table 1). We obtained the data on type 1 diabetes risk variants from a subsequent GWAS of 18,942 cases and 501,638 controls of European ancestry from nine cohorts [9]. We obtained pQTL data for IL6ST from a GWAS of 35,559 Icelanders and eQTL data from GWAS of 31,684 individuals from 37 eQTLGen Consortium cohorts, most individuals being European [10, 11]. We summarise the study population details of the utilised GWAS, as well as methods of ascertainment of cases of type 1 diabetes, measurement of whole-blood gene expression and serum protein levels, in ESM Methods.
Co-localisation
We conducted co-localisation analysis to assess whether the genetic associations for type 1 diabetes risk near the seven drug target genes align with those for the whole-blood gene expression or serum protein levels of these targets. We performed a co-localisation analysis using a ‘coloc’ package in R [5]. This method uses Bayesian principles to assess the relationship between two traits. It considers all variants within a specific genetic locus and evaluates the following hypotheses (H0–H4), assuming a maximum of one causal variant per trait:
-
H0: there is no association with either trait, implying no specific causal variants
-
H1: there is an association with the exposure trait only
-
H2: there is an association with the outcome trait only
-
H3: there are associations with both exposure and outcome traits, two independent SNPs (i.e. distinct casual variants)
-
H4: there are associations with both exposure and outcome traits, one shared causal variant
A high posterior probability for H4 implies a shared causal variant for the two traits. A substantial posterior probability for H3 suggests the two traits are influenced by distinct causal variants linked to each trait. We used the default prior probabilities of 1 × 10−4, 1 × 10−4 and 1 × 10−5 for a variant being associated with the exposure trait, the outcome trait and both traits, respectively.
Mendelian randomisation
To evaluate the direction and magnitude of the causal effects, we performed Mendelian randomisation for those variants that co-localised between drug target levels and the risk of type 1 diabetes (posterior probability for H4 >0.8). Mendelian randomisation uses genetic variants to investigate the relationship between an exposure (e.g. drug target levels) and an outcome (e.g. type 1 diabetes risk) for causality. Under Mendel’s law of assortment, genetic variants are accepted to be independent of other genetic alleles and can be used as valid instrumental variables to estimate the causal effect of the exposure on the outcome if the following three assumptions are fulfilled [6].
-
1:
the genetic variant is associated with the exposure
-
2:
the genetic variant is associated with the outcome only through the exposure
-
3:
the genetic variant is not associated with any confounders
Advantages of Mendelian randomisation include limited susceptibility to reverse causation and confounding by external factors that influence both exposure and the outcome. Linkage disequilibrium (LD) may confound Mendelian randomisation if genetic variants are not shared between the exposure and outcome but they reside in the same genomic area. However, we investigated this possibility in the prior co-localisation step.
Examination of functional variants near drug target genes
To further examine the potential causality of the putative drug targets on type 1 diabetes risk, we searched for functional missense variants in the coding area of these seven drug target genes from PhenoScanner [13] that were associated with the protein/expression levels of the target at p<1 × 10−5. We sought for missense variants only within the gene region for each gene. We used a more lenient threshold than the genome-wide significance of p<5 × 10−8 since we only focused on cis-variants, and the threshold used can be interpreted as a Bonferroni-corrected threshold for 5000 independent variants. These variants were then individually used as instruments in Mendelian randomisation to test for causality of the targets on the risk of type 1 diabetes.
Tissue-specific gene expression analyses using bulk tissue and single-cell eQTL data
To further assess the tissue specificity of the regions that showed evidence for association in Mendelian randomisation, we conducted co-localisation with tissue-specific gene expression and type 1 diabetes liability. We obtained data for IL2RA, IL6R, IL6ST and TYK2 single-cell eQTL of data for immune cell subsets from a GWAS of 982 individuals from the OneK1K cohort, and spleen and pancreas eQTL data from the Genotype Tissue Expression (GTEx) project (v8) [14, 15].
Statistical analysis
All analyses were done with R version 4.2 (R Foundation for Statistical Computing, Vienna, Austria) using the ‘coloc’ and ‘TwoSampleMR’ packages [5, 16]. Effect size for change in the risk of type 1 diabetes is reported per change in SD of serum protein or mRNA levels, and the genetic variants were not weighted in any of the analyses. β and SE values for whole-blood RNA levels were calculated using formulae \(\beta ={z\left(\sqrt{2p\left(1-p\right)\left(n+{z}^{2}\right)}\right)}^{-1}\) and \(SE={2p\left(1-p\right)\left(n+{z}^{2}\right)}^{-1}\), where p = minor allele frequency, n = sample size, and z = z score. Mendelian randomisation estimates are reported as Wald estimates. To assess the instrument strength and potential weak instrument bias, we calculated the F statistics for the instruments using formula F = (β/SE)2.
We only used variants that were available in the GWAS summary statistics for both exposure and outcome traits within each genomic locus. All the LD r2 values reported in this study were obtained from the European population of the 1000 Genomes project using the package ‘ieugwasr’. The study protocol was not preregistered for this study. The code used to generate our results is available at https://github.com/jkoskenniemi/T1DSCREEN.
Results
The same genetic variants affect type 1 diabetes risk and whole-blood IL2RA, IL6R and IL6ST gene expression
We found evidence for a shared causal variant between the risk of type 1 diabetes and whole-blood IL2RA (rs61839660, posterior probability 100%, Fig. 1), IL6R (rs10908839, posterior probability 96.5%, Fig. 2) and IL6ST gene expression (rs7731626, posterior probability 97.0%, Table 2 and ESM Fig. 4). The variant rs10908839 is in strong LD (r2=0.76) with the previously identified lead SNP rs2229238 associated with the risk of type 1 diabetes in the study by Robertson et al [7]. No evidence for co-localisation was observed between drug target levels and the risk of type 1 diabetes near the other target genes (Table 2 and ESM Figs 5–10).
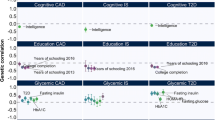
Genetically proxied variability in IL2RA, IL6R and IL6ST expression is associated with the risk of type 1 diabetes
We investigated, using Mendelian randomisation, the direction and magnitude of the expected change in the risk of type 1 diabetes if IL2RA, IL6R and IL6ST were targeted, using variants identified as the most likely shared causal variant in co-localisation (rs61839660 for IL2RA gene expression, F=248; variant rs10908839 for IL6R gene expression, F=148; and variant rs7731626 for IL6ST expression, F=159). The results revealed an OR of 0.22 (95% CI 0.17, 0.27) for type 1 diabetes risk (p=5.3 × 10−43) per SD increase in genetically proxied IL2RA expression, an OR of 1.98 (95% CI 1.48, 2.65) per SD increase in genetically proxied IL6R expression (p=5.2 × 10−6) and an OR of 1.90 (95% CI 1.45, 2.48) per SD increase in genetically proxied IL6ST expression (p=2.6 × 10−6; Table 3).
Functional variant in coding area of TYK2 is associated with the risk of type 1 diabetes
We found 22 missense mutations in the examined drug target genes with GWAS summary data on type 1 diabetes risk (ESM Table 3). Most of the mutations had an allele frequency of <0.01 with the notable exceptions of rs2228145 (minor allele frequency [MAF] =0.39) in IL6R as well as rs12720356 (MAF=0.09) and rs2304256 (MAF=0.28) in TYK2. Summary statistics for both drug target level and type 1 diabetes risk were available for nine variants. One independent variant at LD r2<0.2 within each locus (rs41316003 in JAK2, rs2304256 in TYK2 and rs141500365 IL6ST) was associated with the relevant drug target (protein or gene expression levels at p<1 × 10−5). When using these variants as instruments in Mendelian randomisation, the genetically proxied TYK2 expression was associated with the risk of type 1 diabetes (rs2304256: OR 0.61 [95% CI 0.54, 0.69]) whereas we found no clear evidence for association when using missense variants in IL6ST (OR 0.98 [95% CI 0.78, 1.20]) or JAK2 (OR 0.74 [95% CI 0.46, 1.20]; Table 3). ESM Table 4 shows the LD matrix between the functional variants in the coding area of TYK2 as well as the lead SNPs associated with TYK2 expression and the risk of type 1 diabetes in the vicinity of the TYK2 gene.
Type 1 diabetes and IL2RA co-localise in CD8+ effector memory T cells and type 1 diabetes and IL6ST in CD4+ and CD8+ naive and central memory T cells
To study which specific blood immune cells or tissues mediate the association between IL2RA, IL6R, IL6ST and TYK2 expression and type 1 diabetes risk, we analysed their pairwise co-localisation with type 1 diabetes risk in spleen, pancreas and subsets of blood immune cells. IL2RA expression in CD8+ effector memory T cells co-localised (posterior probability 99.4%, ESM Table 5) with type 1 diabetes risk, with the lead causal variant rs61839660 being the same as for whole-blood IL2RA mRNA expression. Neither IL6R nor TYK2 expression co-localised in any of available immune cells. However, IL6ST expression co-localised in CD4+ and CD8+ naive and central memory T cells (lead causal variant rs7731626; posterior probabilities 97.0% and 92.4%, respectively, ESM Table 5). We did not observe such robust evidence for co-localisation between IL2RA, IL6R, IL6ST or TYK2 eQTL and the risk of type 1 diabetes in other cell types (ESM Table 5) or in spleen or pancreas (ESM Table 6).
Discussion
Leveraging data from large-scale GWAS and multiple quantitative trait locus datasets, we investigated the genetic evidence for the efficacy of seven candidate drugs in prevention of type 1 diabetes. Using co-localisation and Mendelian randomisation, we found genetic evidence to support the role of IL-2 and IL-6 signalling in the pathogenesis of type 1 diabetes. In addition, the investigation of functional missense variants suggested that TYK2 signalling is involved in the aetiology of type 1 diabetes.
While the original GWAS of immune cell subsets did not report the eQTL of IL2RA in regulatory T cells (Tregs), our evidence for the protective effect of blood IL2RA expression on the risk of type 1 diabetes could be interpreted as supporting the role of Tregs as a natural protection against type 1 diabetes. A low but sufficient level of IL-2 is crucial for the survival and function of Tregs, which constitutively express IL2RA, IL2RB and IL2RG to produce α-, β- and γ-chains, respectively, required for trimeric high-affinity IL-2 receptors [17]. Naive T cells express IL2RB and IL2RG, required for the intermediate-affinity IL-2-receptors, but they express IL2RA only transiently when stimulated by antigen-presenting cells and are thus less stimulated by IL-2 when not activated. Thus, higher blood IL2RA expression could be a sign of increased quantity and function of Tregs, which maintain a level of tolerance towards self-peptides and decrease the risk of type 1 diabetes [18]. A previous small study showed that rs12722495, which is in strong LD (r2=0.89) with our lead IL2RA eQTL and type 1 diabetes risk locus rs61839660 near IL2RA, decreased IL2RA expression in Tregs as well as their sensitivity to IL-2 [19].
Alternatively, as IL-2 signalling increases the proliferation of the conventional T cells and Tregs alike, IL-2 signalling might not decrease the risk of type 1 diabetes only by increasing tolerance but also by promoting appropriate responses to pathogens. This is supported by our single-cell-level results, in which we observed evidence for co-localisation between IL2RA expression and the risk of type 1 diabetes only in CD8+ central memory T cells (eQTL of Tregs were not available as they were not distinguished from other T cells). In a birth cohort study of children at high genetic risk of type 1 diabetes (TEDDY study), presence of enteroviral DNA in stool was associated with the risk of islet autoimmunity and the association was stronger in persistent infections indicated by prolonged shedding of enteroviral DNA [20]. Likewise, children who developed islet autoimmunity presented longitudinal transcriptional signatures consistent with a less-robust immune response against enteroviral infections compared with matched control children [21]. Since the increased IL-2 signalling in CD8+ T cells during viral infections prioritises robust immune response against production of long-lived memory cells, this explanation might also explain why rs61839660 near IL2RA strongly co-localised between the risk of type 1 diabetes and the eQTL of IL2RA in effector memory T cells and CD8+ naive/central memory T cells.
The co-localisation of IL2RA expression in CD8+ effector memory T cells with type 1 diabetes risk is further supported by the previous reports of IL-2 impairment leading to CD8+ T cell exhaustion, potentially driven by both acute and chronic viral infections [22, 23]. Interestingly, our lead rs61839660 near IL2RA, which was associated with increased IL2RA expression and decreased risk of type 1 diabetes, was previously shown to be associated with higher risk of Crohn’s disease [24] and lower risk of type 1 diabetes [25]. This suggests that the optimal balance between effector and regulatory T cell function may vary between autoimmune diseases [17]. Regardless of the possible mechanism, our findings support the rationale of conducting type 1 diabetes prevention trials with low-dose IL-2.
Consistent with our finding of the protective effect of IL-2 signalling, we found that IL-6 signalling increased the risk of type 1 diabetes. The secretion of IL-6 from macrophages rapidly in response to infections and tissue damage promotes various acute phase responses [26]. IL-6 signalling occurs as classic signalling through a cell-membrane-bound IL-6R, trans-signalling through soluble circulating IL6R and membrane-bound gp130 (encoded by IL6ST) and trans-presentation by dendritic cells, in which IL-6 is presented to membrane-bound gp130 in T cells via dendritic cell-membrane-bound IL-6R (ESM Fig. 3) [27]. IL-6 inhibits the development and function Tregs and promotes the development of pathogenic T helper 17 (Th17) cells [28], which is inhibited by IL-2. Pronounced IL-6 signalling may alter the balance of Treg/Th17, a proposed causative factor in autoimmune diseases such as rheumatoid arthritis [28] and possibly also type 1 diabetes [29].
While, IL-6 trans-signalling and trans-presentation may be a more potent inducer of autoimmunity than classic signalling [12], our finding that blood IL6R and IL6ST expression are associated with increased risk of type 1 diabetes may be explained by any of the three signalling modalities. However, since IL6ST expression in CD4+ and CD8+ naive or central memory T cells co-localised with type 1 diabetes and IL6R expression did not, it is tempting to speculate that trans-signalling might be more important than classic IL-6 signalling in the pathogenesis of type 1 diabetes.
In contrast to our findings, tocilizumab (a monoclonal antibody against IL6R), which blocks all three IL-6 signalling modalities, did not significantly affect the decline in residual beta cell function in individuals with newly diagnosed type 1 diabetes in a randomised, placebo-controlled, double-blind clinical trial [30]. However, this discrepancy may be partially explained by the timing of the intervention. Genetic polymorphisms typically exert life-long influence on risk of diseases, including every stage of type 1 diabetes, whereas the intervention in the study by Greenbaum et al [30] took place after the diagnosis of type 1 diabetes, at which stage a sharp fall in beta cell function has already taken place [31].
Whole-blood TYK2 expression and the risk of type 1 diabetes did not co-localise, whereas when using the missense mutation rs2304256 in TYK2 as an instrument in Mendelian randomisation, TYK2 expression was associated with type 1 diabetes risk. The absence of evidence for co-localisation may reflect violations of the one-causal-variant assumption. Indeed, the missense mutation rs2304256 is in very high LD (r2=1.00) with the lead TYK2 eQTL rs34725611. Moreover, rs2304256 is only in moderate LD (r2=0.10) with rs144309607, the lead variant on type 1 diabetes liability in co-localisation, suggesting two independent signals. Of note, a known missense variant rs34536443 is not available in the eQTL data and therefore could not be used in co-localisation. Despite the one-causal-variant assumption, ‘coloc’ is relatively robust to multiple causal variants, and co-localisation methods allowing for multiple causal variants are highly sensitive to LD misspecifications in the reference panel [6]. Therefore, in the absence of an accurate LD reference, we proceeded with the ‘coloc’ method for our co-localisation while acknowledging its limitations.
Overall, our TYK2 findings are consistent with previous studies suggesting that TYK2 signalling is associated with the risk of type 1 diabetes [32]. Promising results have been found in clinical trials targeting TYK2 in autoimmune diseases, supporting the potential of drug repurposing in type 1 diabetes [33]. Other reasons for the co-localisation discordance could be that TYK2 is not activated until IFN-α binding to IFNAR1 and TYK2 RNA expressions are known to have low tissue and cell type specificity [34, 35].
It is important to note that Mendelian randomisation estimates are only valid if the instrumental variable associations (relevance, independence, exclusion restriction) are met. The strong associations between the assessed genetic polymorphisms and the studied exposures suggested that the genetic instruments studied were relevant for the studied exposures. The strategy of selecting instruments from within the cis-region of the exposure of interest is an established approach for investigating drug effects [36]. cis-Mendelian randomisation studies are by design less prone to horizontal pleiotropy and exposure misspecification (which may lead to violations of independence and exclusion restriction assumptions), as genetic variants typically exert the strongest influence on nearby genes and therefore most effects are secondary to reading of the nearby genes. However, restricting the instruments to cis-variants comes at the expense of potentially missing strong trans-variants that associate with the exposure. Furthermore, our co-localisation results suggest that associations between whole-blood IL2RA and IL6R expression and the risk of type 1 diabetes are unlikely to be caused by LD with a genetic variant that primarily influences the reading of other genes in the vicinity of IL2RA or IL6R loci.
Some aspects of generalisability of our results are also worth mentioning. While our study did not explicitly exclude individuals from non-European ancestries, the original GWAS studies primarily included individuals of European descent, which limits the spectrum of rare variants and the generalisability of our findings to other ancestries. Furthermore, our Mendelian randomisation estimates represent the influence of small changes in IL2RA, IL6R and TYK2 expression during the entire life course before the diagnosis of type 1 diabetes. Therefore, these effect sizes cannot be directly extrapolated to clinical trials in which the doses are larger and exposures shorter, and possibly outside a key sensitive window for disease development. Thus, natural history studies and clinical prevention trials should pinpoint the optimal stage of pathogenesis at which to interfere with IL-2, IL-6 or TYK2 signalling to prevent type 1 diabetes. Finally, even if up to 50% of variability in genetic risk of type 1 diabetes is attributable to HLA-II locus [37], we could not analyse the interactions between SNPs reported here and the HLA genotype or genetic risk scores on risk of type 1 diabetes, or any sex-specific effects, as we did not have access to individual-level data.
In conclusion, our results provide genetic evidence that IL-2, IL-6 and TYK2 signalling are associated with type 1 diabetes risk. Our findings suggest that clinical trials investigating the efficacy of drugs such as tocilizumab (IL-6R antagonist that targets all IL-6 signalling modalities), olamkicept (soluble gp130Fc that blocks IL-6 trans-signalling) and low-dose aldesleukin (IL-2 analogue) may be promising candidates for the prevention of type 1 diabetes.
Abbreviations
- eQTL:
-
Expression quantitative trait locus / loci
- GWAS:
-
Genome-wide association study
- IL2RA:
-
IL-2 receptor subunit α
- IL2RB:
-
IL-2 receptor subunit β
- IL2RG:
-
IL-2 receptor subunit γ
- IL-6R:
-
IL-6 receptor
- IL6ST:
-
IL-6 cytokine family signal transducer
- JAK1:
-
Janus kinase 1
- JAK2:
-
Janus kinase 2
- JAK3:
-
Janus kinase 3
- LD:
-
Linkage disequilibrium
- MAF:
-
Minor allele frequency
- NK:
-
Natural killers
- pQTL:
-
Protein quantitative trait locus / loci
- Th17:
-
T helper 17
- Treg:
-
Regulatory T cell
- TYK2:
-
Tyrosine kinase 2
References
Foster NC, Beck RW, Miller KM et al (2019) State of type 1 diabetes management and outcomes from the T1D exchange in 2016–2018. Diabetes Technol Ther 21(2):66–72. https://doi.org/10.1089/dia.2018.0384
Dayan CM, Besser REJ, Oram RA et al (2021) Preventing type 1 diabetes in childhood. Science 373(6554):506–510. https://doi.org/10.1126/science.abi4742
Herold KC, Bundy BN, Long SA et al (2019) An anti-CD3 antibody, teplizumab, in relatives at risk for type 1 diabetes. N Engl J Med 381(7):603–613. https://doi.org/10.1056/NEJMoa1902226
King EA, Wade Davis J, Degner JF (2019) Are drug targets with genetic support twice as likely to be approved? Revised estimates of the impact of genetic support for drug mechanisms on the probability of drug approval. PLoS Genet 15(12):1–20. https://doi.org/10.1371/journal.pgen.1008489
Giambartolomei C, Vukcevic D, Schadt EE et al (2014) Bayesian test for colocalisation between pairs of genetic association studies using summary statistics. PLoS Genet 10(5):e1004383. https://doi.org/10.1371/JOURNAL.PGEN.1004383
Zuber V, Grinberg NF, Gill D et al (2022) Combining evidence from Mendelian randomization and colocalization: Review and comparison of approaches. Am J Hum Genet 109(5):767–782. https://doi.org/10.1016/j.ajhg.2022.04.001
Robertson CC, Inshaw JRJ, Onengut-Gumuscu S et al (2021) Fine-mapping, trans-ancestral and genomic analyses identify causal variants, cells, genes and drug targets for type 1 diabetes. Nat Genet 53(7):962–971. https://doi.org/10.1038/s41588-021-00880-5
The ULTRA-DD Consortium, Fang H, De Wolf H et al (2019) A genetics-led approach defines the drug target landscape of 30 immune-related traits. Nat Genet 51(7):1082–1091. https://doi.org/10.1038/s41588-019-0456-1
Chiou J, Geusz RJ, Okino ML et al (2021) Interpreting type 1 diabetes risk with genetics and single-cell epigenomics. Nature 594(7863):398–402. https://doi.org/10.1038/s41586-021-03552-w
Ferkingstad E, Sulem P, Atlason BA et al (2021) Large-scale integration of the plasma proteome with genetics and disease. Nat Genet 53(12):1712–1721. https://doi.org/10.1038/s41588-021-00978-w
Võsa U, Claringbould A, Westra H-J et al (2021) Large-scale cis- and trans-eQTL analyses identify thousands of genetic loci and polygenic scores that regulate blood gene expression. Nat Genet 53(9):1300–1310. https://doi.org/10.1038/s41588-021-00913-z
Rose-John S, Jenkins BJ, Garbers C, Moll JM, Scheller J (2023) Targeting IL-6 trans-signalling: past, present and future prospects. Nat Rev Immunol 23(10):666–681. https://doi.org/10.1038/s41577-023-00856-y
Kamat MA, Blackshaw JA, Young R et al (2019) PhenoScanner V2: an expanded tool for searching human genotype-phenotype associations. Bioinforma Oxf Engl 35(22):4851–4853. https://doi.org/10.1093/bioinformatics/btz469
Yazar S, Alquicira-Hernandez J, Wing K et al (2022) Single-cell eQTL mapping identifies cell type–specific genetic control of autoimmune disease. Science 376(6589):eabf3041. https://doi.org/10.1126/science.abf3041
The GTEx Consortium (2020) The GTEx consortium atlas of genetic regulatory effects across human tissues. Science 369(6509):1318. https://doi.org/10.1126/science.aaz1776
Hemani G, Zheng J, Elsworth B et al (2018) The MR-Base platform supports systematic causal inference across the human phenome. eLife 7:e34408. https://doi.org/10.7554/eLife.34408
Abbas AK, Trotta E, Simeonov DR, Marson A, Bluestone JA (2018) Revisiting IL-2: biology and therapeutic prospects. Sci Immunol 3(25):eaat1482. https://doi.org/10.1126/sciimmunol.aat1482
Mitra S, Leonard WJ (2018) Biology of IL-2 and its therapeutic modulation: Mechanisms and strategies. J Leukoc Biol 103(4):643–655. https://doi.org/10.1002/JLB.2RI0717-278R
Garg G, Tyler JR, Yang JHM et al (2012) Type 1 diabetes-associated IL2RA variation lowers IL-2 signaling and contributes to diminished CD4+CD25+ regulatory T cell function. J Immunol 188(9):4644–4653. https://doi.org/10.4049/jimmunol.1100272
the TEDDY Study Group, Vehik K, Lynch KF et al (2019) Prospective virome analyses in young children at increased genetic risk for type 1 diabetes. Nat Med 25(12):1865–1872. https://doi.org/10.1038/s41591-019-0667-0
Lin J, Moradi E, Salenius K et al (2023) Distinct transcriptomic profiles in children prior to the appearance of type 1 diabetes-linked islet autoantibodies and following enterovirus infection. Nat Commun 14(1):7630. https://doi.org/10.1038/s41467-023-42763-9
Shouse AN, LaPorte KM, Malek TR (2024) Interleukin-2 signaling in the regulation of T cell biology in autoimmunity and cancer. Immunity 57(3):414–428. https://doi.org/10.1016/j.immuni.2024.02.001
Bachmann MF, Wolint P, Walton S, Schwarz K, Oxenius A (2007) Differential role of IL-2R signaling for CD8 + T cell responses in acute and chronic viral infections. Eur J Immunol 37(6):1502–1512. https://doi.org/10.1002/eji.200637023
International Inflammatory Bowel Disease Genetics Consortium, Huang H, Fang M et al (2017) Fine-mapping inflammatory bowel disease loci to single-variant resolution. Nature 547(7662):173–178. https://doi.org/10.1038/nature22969
Type 1 Diabetes Genetics Consortium, Onengut-Gumuscu S, Chen W-M et al (2015) Fine mapping of type 1 diabetes susceptibility loci and evidence for colocalization of causal variants with lymphoid gene enhancers. Nat Genet 47(4):381–386. https://doi.org/10.1038/ng.3245
Tanaka T, Narazaki M, Kishimoto T (2014) IL-6 in inflammation, immunity, and disease. Cold Spring Harb Perspect Biol 6(10):a016295. https://doi.org/10.1101/cshperspect.a016295
Garbers C, Heink S, Korn T, Rose-John S (2018) Interleukin-6: designing specific therapeutics for a complex cytokine. Nat Rev Drug Discov 17(6):395–412. https://doi.org/10.1038/nrd.2018.45
Kimura A, Kishimoto T (2010) IL-6: regulator of Treg/Th17 balance. Eur J Immunol 40(7):1830–1835. https://doi.org/10.1002/eji.201040391
Spence A, Tang Q (2016) Restoring regulatory T cells in type 1 diabetes. Curr Diab Rep 16(11):110. https://doi.org/10.1007/s11892-016-0807-6
Greenbaum CJ, Serti E, Lambert K et al (2021) IL-6 receptor blockade does not slow β cell loss in new-onset type 1 diabetes. JCI Insight 6(21):e150074. https://doi.org/10.1172/jci.insight.150074
Sosenko JM, Skyler JS, Beam CA et al (2013) Acceleration of the loss of the first-phase insulin response during the progression to type 1 diabetes in diabetes prevention trial-type 1 participants. Diabetes 62(12):4179–4183. https://doi.org/10.2337/db13-0656
Pellenz FM, Dieter C, Duarte GCK, Canani LH, de Souza BM, Crispim D (2021) The rs2304256 polymorphism in TYK2 gene is associated with protection for type 1 diabetes mellitus. Diabetes Metab J 45(6):899–908. https://doi.org/10.4093/dmj.2020.0194
Yuan S, Wang L, Zhang H et al (2023) Mendelian randomization and clinical trial evidence supports TYK2 inhibition as a therapeutic target for autoimmune diseases. eBioMedicine 89:104488. https://doi.org/10.1016/j.ebiom.2023.104488
Kalvakolanu DV, Nallar SC, Kalakonda S (2016) Interferons: Cellular and Molecular Biology of Their Actions. In: Reference Module in Biomedical Sciences. Elsevier, Amsterdam, the Netherlands, p B9780128012383961166. https://doi.org/10.1016/B978-0-12-801238-3.96116-6
Uhlén M, Fagerberg L, Hallström BM et al (2015) Proteomics. Tissue-based map of the human proteome. Science 347(6220):1260419. https://doi.org/10.1126/science.1260419
Gill D, Georgakis M, Walker V et al (2021) Mendelian randomization for studying the effects of perturbing drug targets [version 2; peer review: 3 approved, 1 approved with reservations]. Wellcome Open Res 6(16):eCollection 2021. https://doi.org/10.12688/wellcomeopenres.16544.2
Pociot F, Lernmark Å (2016) Genetic risk factors for type 1 diabetes. Lancet 387(10035):2331–2339. https://doi.org/10.1016/S0140-6736(16)30582-7
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Acknowledgements
The authors wish to acknowledge CSC – IT Center for Science, Finland, for computational resources, the authors of original studies for summary statistics, T. Kinnunen (University of Eastern Finland) for helpful discussions, and two anonymous reviewers for insightful comments.
During the preparation of this work the authors used ChatGPT version 4.0 to proofread and to improve the readability of the manuscript. After using this tool/service, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
Data availability
Analysis code can be accessed at https://github.com/jkoskenniemi/T1DSCREEN, which also includes instructions on how to download the original GWAS summary statistics.
Funding
This study was funded by Kyllikki ja Uolevi Lehikoisen säätiö, Foundation for Paediatric Research, Finnish Cultural Foundation, JDRF International (JJK); The University of Oulu & The Research Council of Finland Profi 326291 (VK); European Union’s Horizon 2020 research and innovation programme under grant agreement no. 848158 (EarlyCause) (VK); Wellcome Trust (225790/Z/22/Z) and the UK Research and Innovation Medical Research Council (MC_UU_00040/01) (VK). The study funders were not involved in the design of the study; the collection, analysis, and interpretation of data; writing the report; and did not impose any restrictions regarding the publication of the report.
Authors’ relationships and activities
The authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Contribution statement
JJK, VK and DG designed the study. JJK, VK and JL curated data. TEH and EKK analysed and visualised the data under supervision of JL, JJK and VK. TEH, EKK and JJK wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version to be published. All authors had access to data, and JJK, VK, JL, TEH and EKK accessed and verified the data. JJK, VK, TEH and EKK are guarantors for this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Tea E. Heikkilä and Emilia K. Kaiser contributed equally to the manuscript and are joint first authors.
Jaakko J. Koskenniemi and Ville Karhunen contributed equally to the manuscript and share senior authorship.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Heikkilä, T.E., Kaiser, E.K., Lin, J. et al. Genetic evidence for efficacy of targeting IL-2, IL-6 and TYK2 signalling in the prevention of type 1 diabetes: a Mendelian randomisation study. Diabetologia (2024). https://doi.org/10.1007/s00125-024-06267-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00125-024-06267-5