Abstract
Aims/hypothesis
On cross-sectional assessment, a delayed timing of the peak blood glucose level at ≥60 min post-challenge on an OGTT is associated with beta cell dysfunction. In this context, we hypothesised that longitudinal changes in the timing of this peak might predict changes in glucose metabolism. We thus sought to evaluate the longitudinal associations of changes in the timing of the peak glucose level with changes over time in insulin sensitivity, beta cell function and glucose tolerance.
Methods
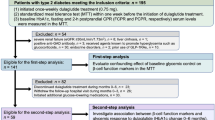
A total of 532 women underwent an OGTT at both 3 months and 12 months postpartum. The participants were stratified into four groups according to the change in timing of their glucose peak between the two visits: women with no change in timing of the glucose peak at 30 min (n = 217), those whose glucose peak shifted to an earlier time point (n = 120), those whose peak shifted to a later time point (n = 87) and women with an unchanged glucose peak at ≥60 min (n = 108). Beta cell function was measured using the Insulin Secretion-Sensitivity Index-2 (ISSI-2).
Results
Compared with an unchanged glucose peak at 30 min, both the shift of the glucose peak to a later time point and a peak that was unchanged at ≥60 min were independently associated with declining ISSI-2 scores (β = −127.5, p < 0.001 and β = −98.8, p = 0.006, respectively) and increased 2 h post-challenge glucose levels (β = 1.28, p < 0.001 and β = 0.91, p < 0.001, respectively) between the two visits. Furthermore, both these patterns of change in peak were independently associated with worsening glucose tolerance (from normal to prediabetes [defined as impaired fasting glucose or impaired glucose tolerance]/diabetes or from prediabetes to diabetes) (OR 8.1, 95% CI 3.0, 22.1 and OR 3.7, 95% CI 1.2, 11.7, respectively).
Conclusions/interpretation
A delayed timing of the post-challenge peak glucose level is associated with declining beta cell function and worsening glucose tolerance over time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The OGTT has long been used for the classification of glucose tolerance status through the measurement of fasting blood glucose and 2 h post-challenge blood glucose levels [1, 2]. In recent years, other features of the glucose and insulin response during the OGTT have been studied as potential indicators of metabolic function, including the shapes of the glucose and insulin curves [3–6], the times to their respective peak levels [7], the 1 h plasma glucose level [8] and the relationship between fasting glucose level and the nadir of the post-challenge glucose response [9]. Of these measures, the time point after the oral glucose challenge at which the peak blood glucose concentration occurs has recently emerged as a reliably reproducible variable on the OGTT, with 76% agreement on the triplicate testing of individuals assessed on three different days [10]. Furthermore, the presence of a delayed glucose peak (defined as a peak blood glucose level occurring at ≥60 min after the oral challenge) has been associated with beta cell dysfunction, suggesting that this variable may hold a biological meaning [10].
In this context, we hypothesised that longitudinal changes in the timing of this peak might predict changes in glucose metabolism. Specifically, we hypothesised that a shift of the glucose peak to a later time point in response to the OGTT might predict worsening glucose metabolism. Our objective in this study was therefore to evaluate the longitudinal associations between changes in the timing of the peak glucose on the OGTT and changes over time in insulin sensitivity, beta cell function and glucose tolerance in the first year postpartum in a cohort of women with varying degrees of glucose intolerance in pregnancy, reflecting a broad range of diabetic risk, as described in the next section.
Methods
Study participants
This study was performed in the setting of a prospective observational cohort consisting of women representing the full spectrum of glucose tolerance in a recent pregnancy (from normal glucose tolerance [NGT] to gestational diabetes mellitus [GDM]), who thereby have a broad range of risk of the future development of prediabetes (impaired fasting glucose/impaired glucose tolerance—see the following section) and type 2 diabetes in the years after delivery [11]. This cohort provided a model for studying the longitudinal relationship between changes in the timing of the peak glucose level and glucose metabolism because the range of future diabetic risk within this cohort has been shown to manifest as changes in beta cell function, insulin sensitivity and glycaemia between 3 and 12 months postpartum [11].
As previously described [11], the women comprising this cohort are recruited at the time of antepartum screening for GDM in the late second trimester and undergo metabolic characterisation at recruitment and at both 3 months and 12 months postpartum. At our institution, pregnant women are screened for GDM using a 50 g glucose challenge test (GCT) late in the second trimester, and this is followed by referral for a diagnostic OGTT if the GCT is abnormal. In this cohort study, women are recruited either before or after the GCT, and all participants undergo a 3 h 100 g OGTT for determination of GDM status (even if the GCT result is normal). The resultant cohort thus reflects the full spectrum of glucose tolerance in pregnancy from NGT to GDM, which translates to a gradient of future risk for postpartum progression to prediabetes and diabetes. For this cohort study, participants return to the clinical investigation unit at both 3 and 12 months postpartum to undergo repeat metabolic characterisation, including an evaluation of glucose tolerance using a 2 h 75 g OGTT on both occasions. The protocol has been approved by the Mount Sinai Hospital Research Ethics Board and all women have provided written informed consent for their participation.
The current study was performed in the first 532 women to have completed the 12 month visit, thereby enabling an assessment of the longitudinal relationship between changes in the timing of the peak glucose level on the OGTT and changes in glucose metabolism between 3 and 12 months.
Participant assessments at 3 and 12 months postpartum
Participants returned to the clinical investigation unit for a 2 h 75 g OGTT at both 3 and 12 months postpartum. All the OGTTs were performed in the morning after an overnight fast, and venous blood samples were drawn to measure both glucose and insulin at fasting and at 30, 60 and 120 min after ingestion of the glucose load, as previously described [12]. At both visits, the OGTT enabled a classification of glucose tolerance into one of three categories, as per the current clinical practice guidelines from the Canadian Diabetes Association [13]: (1) NGT, defined by a fasting glucose level <6.1 mmol/l and a 2 h glucose <7.8 mmol/l, (2) prediabetes, defined as fasting glucose level between 6.1 and 6.9 mmol/l inclusive or a 2 h glucose between 7.8 and 11.0 mmol/l inclusive, and (3) diabetes, defined by a fasting glucose ≥7.0 mmol/l or a 2 h glucose ≥11.1 mmol/l.
Physiological indices
The AUCs for insulin (AUCins) and for glucose (AUCgluc) during the OGTT were calculated using the trapezoidal rule. Insulin sensitivity was measured using the Matsuda Index, an established measure of whole-body insulin sensitivity that has been validated against the euglycaemic–hyperinsulinaemic clamp [14]. Beta cell function was assessed for each OGTT using the Insulin Secretion-Sensitivity Index-2 (ISSI-2), a validated measure of beta cell function that is analogous to the disposition index obtained from the IVGTT [15, 16]. ISSI-2 has been directly validated against the disposition index from the IVGTT, with which it exhibits a stronger correlation than do other OGTT-derived measures of beta cell function [16], and it has been used to measure beta cell function in several previous studies, including both clinical trials [17, 18] and observational studies [11, 19–21]. ISSI-2 is defined as the product of (1) insulin secretion measured by the ratio of AUCins to AUCgluc, and (2) insulin sensitivity measured by the Matsuda Index [15, 16].
Glucose response on the OGTT (time to peak glucose)
The time to peak glucose was defined as the time point during the OGTT at which the blood glucose level was highest (either 30, 60 or 120 min). For each participant, the peak was determined on OGTTs at both 3 and 12 months postpartum. Based on the relationship between the time to peak glucose at 3 months and that at 12 months, participants were stratified into four groups: (1) those with a time to peak glucose that was unchanged at 30 min between the two visits; (2) those with a peak glucose that was shifted to an earlier time point during the OGTT at the 12 month postpartum visit compared with 3 months postpartum, (3) those with a peak glucose that was shifted to a later time point during the OGTT at 12 months compared with 3 months, and (4) women with a time to peak glucose peak that was unchanged at ≥60 min at both visits.
Statistical analysis
All analyses were conducted using SAS9.2 (SAS Institute, Cary, NC, USA). Continuous variables were tested for normality of distribution, and natural log transformations of skewed variables were used, where necessary, in subsequent analyses. Variables with normal distribution are presented as mean ± SD, and those with non-normal distribution are presented as median (25th–75th percentiles).
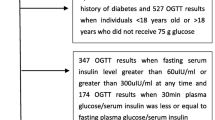
Univariate differences between the four groups that were defined according to change in time to peak glucose were assessed at 3 and 12 months postpartum using one-way ANOVA for continuous variables and the χ 2 test for categorical variables (Table 1). The changes in each group of insulin sensitivity (Matsuda index), beta cell function (ISSI-2), fasting glucose and 2 h glucose between 3 and 12 months postpartum were compared using ANOVA (Fig. 1a–d) to determine whether there were differential changes between the groups in these measures over time. In addition, the baseline-adjusted changes in ISSI-2 and 2 h post-challenge glucose were compared between the groups by analysis of covariance (Fig. 1e, f).
Comparison of the change between 3 and 12 months postpartum in (a) Matsuda Index, (b) ISSI-2, (c) fasting glucose, and (d) 2 h post-challenge blood glucose between groups defined by the change in timing of the peak glucose level. Circles, women with no change in peak glucose at 30 min; triangles, women with a shift to an earlier peak; inverse triangles, women with a shift to a later peak; squares, women with no change at ≥60 min. Comparison of baseline-adjusted changes in (e) ISSI-2 and (f) 2 h post-challenge blood glucose between these groups (*p < 0.05 compared with the reference group [no change in glucose peak at 30 min])
Multiple linear regression models were constructed to determine whether the change in the time to peak glucose on the OGTT was independently associated with the change in beta cell function (ISSI-2) and 2 h post-challenge glucose (Table 2). The reference group in these analyses was those with a glucose peak that was unchanged at 30 min for the two visits. The covariates included in these models consisted of (1) conventional risk factors for diabetes (age, ethnicity, family history of diabetes, BMI and previous GDM), (2) a potential confounder that could affect the association of peak glucose with the outcomes (AUCgluc), and (3) baseline measure of the outcome (ISSI-2 or 2 h glucose at 3 months postpartum). The covariates were tested for multicollinearity using the variance inflation factor. To evaluate the robustness of these findings, sensitivity analyses were performed that were restricted to only those women with NGT at 3 months postpartum (see electronic supplementary material [ESM] Table 1).
Finally, logistic regression analyses were performed to identify independent determinants of worsening glucose tolerance between the OGTT at 3 months postpartum and the OGTT at 12 months. Worsening glucose tolerance was defined as (1) a progression from NGT at 3 months to either prediabetes or diabetes at 12 months postpartum, or (2) a progression from prediabetes at 3 months to diabetes at 12 months. Covariates were chosen based on clinical relevance and univariate analysis (i.e. those that differed between the groups on unadjusted analysis) (Fig. 2). In the same way as for the linear regression models, sensitivity analyses were performed including only women with NGT at 3 months postpartum (ESM Fig. 1).
Logistic regression model of (as a dependent variable) worsening of glucose tolerance status between 3 and 12 months postpartum (from normal to prediabetes/diabetes or from prediabetes to diabetes). ORs for changes in the timing of the peak glucose are presented compared with no change in peak glucose at 30 min (the reference group) (log scale)
A sample size of 500 women would provide >90% power to detect an R 2 of 0.015 in the change in ISSI-2 attributed to a single independent variable (the shift of glucose peak to a later time point) at a significance level of 0.05, with adjustment for an additional eight independent variables (age, Asian ethnicity, other non-white ethnicity, family history of diabetes, previous GDM, baseline BMI, AUCgluc at 3 months and baseline ISSI-2 at 3 months) with an R 2 of 0.32 (R 2 taken from previous data [11]).
Results
Characteristics of the study population at 3 and 12 months postpartum
The 532 study participants were stratified into the following four groups according to the change in timing of their glucose peak from their OGTT at 3 months postpartum to their repeat OGTT at 12 months postpartum: (1) 217 women (40.8%) had a glucose peak that was unchanged at 30 min between the two visits, (2) 120 (22.6%) had a glucose peak that was shifted to an earlier time point at 12 months compared with 3 months, (3) 87 (16.4%) had a glucose peak that was shifted to a later time point, and (4) 108 (20.3%) had no change in glucose peak at ≥60 min between the two visits. Table 1 shows a comparison of the characteristics of these four groups at 3 and 12 months postpartum. The groups differed in systolic and diastolic BP at 3 months postpartum (both p < 0.01) and BMI at 12 months (p = 0.03). More strikingly, they differed significantly in AUCgluc and glucose tolerance at both 3 and 12 months postpartum (all p < 0.0001). At both visits, the women with no change in peak glucose at 30 min had the lowest AUCgluc and best glucose tolerance, while those with no change in peak at ≥60 min had the worst metabolic profile. Interestingly, the two intermediate groups showed a marked change in metabolic profile between the two visits. Specifically, the women in whom there was a shift to an earlier peak showed an improvement in the prevalence of NGT from 75% at 3 months to 94.2% at 12 months. Conversely, the group in which there was a shift to a later peak exhibited a worsening of glucose tolerance, with the prevalence of NGT decreasing from 89.7% to 74.7%. As such, at 12 months postpartum, the prevalence of dysglycaemia progressively increased from the group with a peak that was unchanged at 30 min (4.1%) to the women with a shift to an earlier peak (5.8%) to those with a shift to a later peak (25.3%) to the group with an unchanged peak at ≥60 min (41.6%) (p < 0.0001).
Figure 1 shows the change in insulin sensitivity (Matsuda Index), beta cell function (ISSI-2), fasting glucose and 2 h glucose level between the 3 and 12 month postpartum visits in each of the four groups. The groups did not differ in their pattern of change in the Matsuda Index (p = 0.53, Fig. 1a) and fasting glucose level (p = 0.23, Fig. 1c). In contrast, there were differential changes between the groups in ISSI-2 (p = 0.01, Fig. 1b) and 2 h glucose (p < 0.0001, Fig. 1d). To further evaluate these differential changes while accounting for the impact of baseline differences in the respective measures, we next compared the baseline-adjusted change in ISSI-2 and post-challenge glucose between the groups. Compared with the reference group (i.e. women with a peak that was unchanged at 30 min), the baseline-adjusted ISSI-2 decreased significantly in both the women with a shift to a later peak and those with a peak unchanged at ≥60 min (Fig. 1e). Similarly, the latter two groups also showed a significant increase in baseline-adjusted 2 h blood glucose (Fig. 1f).
Adjusted analyses
In light of the univariate associations between the change in glucose peak and the changes in beta cell function and post-challenge glucose values, we performed multiple linear regression analyses of the dependent variables (1) change in ISSI-2 and (2) change in 2 h glucose level between 3 and 12 months postpartum. On these analyses (Table 2), both a shift to a later peak and no change in glucose peak at ≥60 min were associated with both a decline in ISSI-2 (fully adjusted model: β = −127.5, p < 0.001, and β = −98.8, p = 0.006, respectively) and an increase in 2 h glucose (fully adjusted model: β = 1.28, p < 0.001, and β = 0.91, p < 0.001, respectively). These findings were unchanged in sensitivity analyses that were limited to only those women with NGT at 3 months postpartum (ESM Table 1).
To evaluate the longitudinal association between the change in timing of the glucose peak on OGTT and glucose tolerance after adjustment for covariates, we performed logistic regression analyses with an outcome of worsening of glucose tolerance status (from normal to prediabetes/diabetes at 12 months postpartum or from prediabetes to diabetes at 12 months postpartum) (Fig. 2). As expected, BMI at 3 months was associated with glycaemic progression (OR = 1.09, 95% CI 1.03, 1.16). More interestingly, however, both a shift to a later glucose peak and an unchanged peak at ≥60 min were independently associated with worsening glucose tolerance (OR = 8.1, 95% CI 3.0, 22.1 and OR = 3.7, 95% CI 1.2, 11.7, respectively). These findings were unchanged on sensitivity analysis limited to women with NGT at 3 months postpartum (ESM Fig. 1).
Discussion
In this report, we demonstrate that both a shift of the glucose peak to a later time point and a consistently delayed glucose peak (≥60 min) are independently associated with (1) declining beta cell function, (2) an increased 2 h post-challenge blood glucose level, and (3) worsening of glucose tolerance status over a 9 month period. Moreover, these findings apply even to participants with NGT at baseline. Conversely, a shift of the glucose peak to an earlier time point is associated with improved glucose metabolism. It thus emerges that the dynamic of the time to peak glucose in response to an OGTT is a simple measure that may provide an insight into early changes in beta cell function and glucose tolerance over time.
Several previous studies have demonstrated that the shape of the glucose curve on the OGTT, of which the peak is a central feature, is associated with glucose homeostasis [3–5, 9, 22–27]. Indeed, a delayed peak has been associated with dysglycaemia and with beta cell dysfunction measured in a variety of advanced ways, including by hyperglycaemic clamp [3–5, 9, 22, 23]. Furthermore, the presence of a delayed peak on an otherwise clinically normal OGTT at 3 months postpartum identifies normoglycaemic women who are at risk of subsequent progression to prediabetes [7]. Most importantly, in a study of 1,282 participants with initial NGT, Abdul-Ghani et al [9] demonstrated that those whose baseline OGTT showed a quicker return of the postload glucose concentration to their fasting level (i.e. those with an earlier peak) had a lower risk of developing type 2 diabetes over 8 years of follow-up than individuals whose postload glucose fell more slowly (i.e. those with a delayed peak).
While these studies have established the importance of a delayed peak at baseline, the current study now evaluates the implications of changes in the timing of the glucose peak when assessed longitudinally over time with successive OGTTs. Of note, it has previously been shown that, in patients who are early in the course of type 2 diabetes, the improvement in beta cell function induced by short-term intensive insulin therapy is associated with a shift of the glucose peak to an earlier time point [10]. The current study now extends this literature by showing that spontaneous changes in the timing of the post-challenge peak glucose over time are associated with longitudinal changes in beta cell function and glucose tolerance in an otherwise young healthy patient population. These data thus demonstrate that the time to peak glucose is a dynamic variable that tracks with early changes in glucose metabolism.
These data are supported by several strengths in the design of the current study. First, the study population consisted of a large cohort of young women reflecting a broad range of future diabetic risk, who were evaluated by OGTT at two points in time (3 and 12 months postpartum). Second, the range of future diabetic risk within this cohort has previously been shown to manifest in differential changes in beta cell function, insulin sensitivity and glycaemia within this period of observation [20], leading to differential rates of prediabetes and diabetes in the years thereafter [21]. Third, the women comprising this cohort experienced the full range of changes in peak glucose during this time, from an unchanged peak at either 30 min or ≥60 min, to shifts to either an earlier or later time point. Accordingly, it was possible to show that (1) an unchanged peak at 30 min was associated with the best metabolic profile, (2) an unchanged peak at ≥60 min was present in those with the poorest metabolic profile, (3) a shift of the peak to a later time point was accompanied by a worsening metabolic function, and (4) a shift of the peak to an earlier time point was associated with an improvement in glucose homeostasis.
A limitation of this study is that its observational nature precludes any commentary on cause and effect in the observed longitudinal relationships. Nevertheless, the biological relevance of the current findings is supported by the mutual consistency of the inverse metabolic changes observed with a shift of the glucose peak to later and earlier time points, respectively. Furthermore, it is noteworthy that a delay in the glucose peak (both a chronic and an incident delay) was an independent predictor of worsening glucose tolerance status after adjustment for established diabetic risk factors (Fig. 2). Indeed, among the latter risk factors, only BMI accompanied a delayed peak glucose as a significant independent predictor of this outcome.
Another limitation of this study is that sampling during the OGTTs was only performed at four time points, as measurement at more time points may provide a greater resolution of the timing of the glucose peak. In addition, beta cell function and insulin sensitivity were assessed with surrogate indices rather than more direct measures such as clamp studies. However, owing to their time-consuming nature, clamp studies would have been difficult to complete on two occasions in the first year postpartum in 532 new mothers. Moreover, it should be noted that ISSI-2 and the Matsuda Index are validated measures that have been widely used in previous studies [11, 14–21]. Finally, the clinical application of the time to peak glucose is limited by the requirement for a multisample OGTT. It is also possible that time to peak glucose may shift in either direction over time, as occurs with glucose tolerance categories [28]. Further longitudinal studies will thus be needed to evaluate the natural history of the time to peak glucose and its determinants.
The current data demonstrate that a delayed glucose peak is independently associated with worsening beta cell function after adjustment for covariates and even when limited to women with NGT (Table 2 and ESM Table 1). Coupled with the previous demonstration that the improvement in beta cell function induced by short-term intensive insulin therapy in early type 2 diabetes is associated with an earlier shift of the glucose peak [10], these data potentially implicate beta cell function as a pathophysiological basis for the link between peak glucose and dysglycaemia.
However, it should also be recognised that the timing of the glucose peak on the OGTT probably reflects the complex interaction of several physiological factors that are triggered by the oral glucose challenge. Besides early-phase insulin secretion, these physiological factors include intestinal glucose absorption, glucagon suppression, secretion of incretins and glucose disposal [29–32]. The relative contributions of each of these factors are difficult to determine. In this context, it seems prudent to conclude that the current data suggest that the timing of peak glucose may provide an integrated measure of multiple physiological processes involved in glucose regulation, one that is sensitive to the subclinical metabolic changes associated with the progression of dysglycaemia early in the natural history of prediabetes/diabetes.
In conclusion, both a shift of the glucose peak to a later time point and an unchanged glucose peak at ≥60 min are independently associated with declining beta cell function, increased 2 h blood glucose and worsening glucose tolerance status. These relationships of incident and chronically delayed peak glucose are present even in women with NGT at baseline. Thus, the time to peak glucose in response to an OGTT emerges as a dynamic measure that may provide insight into early changes over time in beta cell function and glucose tolerance.
Abbreviations
- AUCgluc :
-
AUC for glucose
- AUCins :
-
AUC for insulin
- GCT:
-
Glucose challenge test
- GDM:
-
Gestational diabetes mellitus
- ISSI-2:
-
Insulin Secretion-Sensitivity Index-2
- NGT:
-
Normal glucose tolerance
References
Standards of medical care in diabetes—2014 (2014) Diabetes Care 37(Suppl 1):S14–S80
Barrett-Connor E (2002) The oral glucose tolerance test, revisited. Eur Heart J 23:1229–1231
Kim JY, Coletta DK, Mandarino LJ, Shaibi GQ (2012) Glucose response curve and type 2 diabetes risk in Latino adolescents. Diabetes Care 35:1925–1930
Nolfe G, Spreghini MR, Sforza RW, Morino G, Manco M (2012) Beyond the morphology of the glucose curve following an oral glucose tolerance test in obese youth. Eur J Endocrinol 166:107–114
Tschritter O, Fritsche A, Shirkavand F, Machicao F, Haring H, Stumvoll M (2003) Assessing the shape of the glucose curve during an oral glucose tolerance test. Diabetes Care 26:1026–1033
Hayashi T, Boyko EJ, Sato KK et al (2013) Patterns of insulin concentration during the OGTT predict the risk of type 2 diabetes in Japanese Americans. Diabetes Care 36:1229–1235
Retnakaran R, Qi Y, Connelly PW, Sermer M, Hanley AJ, Zinman B (2010) Risk of early progression to prediabetes or diabetes in women with recent gestational dysglycaemia but normal glucose tolerance at 3-month postpartum. Clin Endocrinol 73:476–483
Alyass A, Almgren P, Akerlund M et al (2015) Modelling of OGTT curve identifies 1 h plasma glucose level as a strong predictor of incident type 2 diabetes: results from two prospective cohorts. Diabetologia 58:87–97
Abdul-Ghani MA, Williams K, DeFronzo R, Stern M (2006) Risk of progression to type 2 diabetes based on relationship between postload plasma glucose and fasting plasma glucose. Diabetes Care 29:1613–1618
Kramer CK, Vuksan V, Choi H, Zinman B, Retnakaran R (2014) Emerging parameters of the insulin and glucose response on the oral glucose tolerance test: reproducibility and implications for glucose homeostasis in individuals with and without diabetes. Diabetes Res Clin Pract 105:88–95
Kramer CK, Swaminathan B, Hanley AJ et al (2014) Prospective associations of vitamin D status with beta-cell function, insulin sensitivity and glycemia: the impact of parathyroid hormone status. Diabetes 63:3868–3879
Retnakaran R, Qi Y, Sermer M, Connelly PW, Hanley AJ, Zinman B (2008) Glucose intolerance in pregnancy and future risk of pre-diabetes or diabetes. Diabetes Care 31:2026–2031
Canadian Diabetes Association Clinical Practice Guidelines Expert Committee (2013) Canadian Diabetes Association 2013 clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes 37(Suppl 1):S8–S11
Matsuda M, DeFronzo RA (1999) Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care 22:1462–1470
Retnakaran R, Shen S, Hanley AJ, Vuksan V, Hamilton JK, Zinman B (2008) Hyperbolic relationship between insulin secretion and sensitivity on oral glucose tolerance test. Obesity 16:1901–1907
Retnakaran R, Qi Y, Goran MI, Hamilton JK (2009) Evaluation of proposed oral disposition index measures in relation to the actual disposition index. Diabet Med 26:1198–1203
Zinman B, Harris SB, Neuman J et al (2010) Low-dose combination therapy with rosiglitazone and metformin to prevent type 2 diabetes mellitus (CANOE trial): a double-blind randomised controlled study. Lancet 376:103–111
Retnakaran R, Kramer CK, Choi H, Swaminathan B, Zinman B (2014) Liraglutide and the preservation of pancreatic beta-cell function in early type 2 diabetes: the LIBRA Trial. Diabetes Care 37:3270–3278
Kayaniyil S, Retnakaran R, Harris SB et al (2011) Prospective associations of vitamin D with beta-cell function and glycemia: the PROspective Metabolism and ISlet cell Evaluation (PROMISE) cohort study. Diabetes 60:2947–2953
Retnakaran R, Qi Y, Sermer M, Connelly PW, Hanley AJ, Zinman B (2010) Beta-cell function declines within the first year postpartum in women with recent glucose intolerance in pregnancy. Diabetes Care 33:1798–1804
Kramer CK, Swaminathan B, Hanley AJ et al (2014) Each degree of glucose intolerance in pregnancy predicts distinct trajectories of β-cell function, insulin sensitivity, and glycemia in the first 3 years postpartum. Diabetes Care 37:3262–3269
Kanauchi M, Kimura K, Kanauchi K, Saito Y (2005) Beta-cell function and insulin sensitivity contribute to the shape of plasma glucose curve during an oral glucose tolerance test in non-diabetic individuals. Int J Clin Pract 59:427–432
Zhou W, Gu Y, Li H, Luo M (2006) Assessing 1-h plasma glucose and shape of the glucose curve during oral glucose tolerance test. Eur J Endocrinol 155:191–197
Abdul-Ghani MA, Lyssenko V, Tuomi T, Defronzo RA, Groop L (2010) The shape of plasma glucose concentration curve during OGTT predicts future risk of type 2 diabetes. Diabetes Metab Res Rev 26:280–286
Tura A, Morbiducci U, Sbrignadello S, Winhofer Y, Pacini G, Kautzky-Willer A (2011) Shape of glucose, insulin, C-peptide curves during a 3-h oral glucose tolerance test: any relationship with the degree of glucose tolerance? Am J Physiol Regul Integr Comp Physiol 300:R941–R948
Frøslie KF, Røislien J, Qvigstad E et al (2013) Shape information from glucose curves: functional data analysis compared with traditional summary measures. BMC Med Res Methodol 13:6
Frøslie KF, Røislien J, Qvigstad E et al (2014) Shape information in repeated glucose curves during pregnancy provided significant physiological information for neonatal outcomes. PLoS One 9:e90798
Ferrannini E, Natali A, Muscelli E et al (2011) Natural history and physiological determinants of changes in glucose tolerance in a non-diabetic population: the RISC Study. Diabetologia 54:1507–1516
Mitrakou A, Kelley D, Mokan M et al (1992) Role of reduced suppression of glucose production and diminished early insulin release in impaired glucose tolerance. N Engl J Med 326:22–29
Caumo A, Luzi L (2004) First-phase insulin secretion: does it exist in real life? Considerations on shape and function. Am J Physiol Endocrinol Metab 287:E371–E385
Baggio LL, Drucker DJ (2007) Biology of incretins: GLP-1 and GIP. Gastroenterology 132:2131–2157
Woerle HJ, Carneiro L, Derani A, Goke B, Schirra J (2012) The role of endogenous incretin secretion as amplifier of glucose-stimulated insulin secretion in healthy subjects and patients with type 2 diabetes. Diabetes 61:2349–2358
Funding
This study was supported by operating grants from the Canadian Institutes of Health Research (CIHR) (MOP-84206) and the Canadian Diabetes Association (CDA) (OG-3-11-3300-RR). AJGH holds a Tier-II Canada Research Chair in Diabetes Epidemiology. BZ holds the Sam and Judy Pencer Family Chair in Diabetes Research at Mount Sinai Hospital and University of Toronto. RR is supported by a Heart and Stroke Foundation of Ontario Mid-Career Investigator Award and his research programme is supported by an Ontario Ministry of Research and Innovation Early Researcher Award.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
CKK planned the analysis, researched the data and wrote the first draft of the manuscript. CY performed the statistical analyses. AJGH, PWC, MS, BZ and RR were involved in the design and implementation of the overall study. All authors contributed to interpretation of the data and critical revision of the manuscript. All authors approved the manuscript. RR is the guarantor, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Table 1
(PDF 64 kb)
ESM Fig. 1
(PDF 12 kb)
Rights and permissions
About this article
Cite this article
Kramer, C.K., Ye, C., Hanley, A.J.G. et al. Delayed timing of post-challenge peak blood glucose predicts declining beta cell function and worsening glucose tolerance over time: insight from the first year postpartum. Diabetologia 58, 1354–1362 (2015). https://doi.org/10.1007/s00125-015-3551-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-015-3551-6