Abstract
Aims/hypothesis
Obesity causes an imbalance in fat mass distribution between visceral and subcutaneous adipose tissue (AT) depots. We tested the hypothesis that this relates to increased NEFA uptake between these depots in obese compared with healthy participants. Second, we hypothesised that a diet very low in energy (very low calorie diet [VLCD]) decreases fat mass in obese participants and that this is associated with the decline in NEFA uptake.
Methods
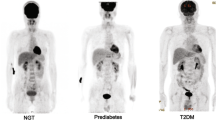
NEFA uptake in AT depots was measured with [18F]-fluoro-6-thia-heptadecanoic acid (18F-FTHA) and positron emission tomography (PET) in 18 obese participants with the metabolic syndrome before and after a 6 week VLCD. Whole body fat oxidation was measured using indirect calorimetry and [U-13C]palmitate. Sixteen non-obese participants were controls.
Results
Obese participants had >100% higher (p < 0.0001) NEFA uptake in the visceral and subcutaneous abdominal AT depots than controls. VLCD decreased AT mass in all regions (12% to 21%), but NEFA uptake was decreased significantly (18%; p < 0.006) only in the femoral AT. Whole body carbohydrate oxidation decreased, while fat oxidation increased.
Conclusions/interpretation
The data demonstrate that weight loss caused by VLCD does not affect abdominal fasting NEFA uptake rates. We found that visceral fat takes up more NEFAs than subcutaneous AT depots, even after weight loss.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Visceral and subcutaneous fat depots differ in their biological and physiological properties [1]. Femoral subcutaneous fat plays a protective role against diabetes [2] because it positively associates with favourable lipid and glucose levels [3], and coronary artery disease risk factors [4]. A low amount of femoral fat is a metabolic risk factor, independent of the amount of abdominal fat [3]. Visceral fat associates with reduced insulin sensitivity, hypertension, impaired glucose tolerance, type 2 diabetes, coronary heart disease [5], and accumulation of liver [6] and intramuscular fat [7]. Visceral fat, compared with abdominal subcutaneous fat, is metabolically more active in the fasting state in terms of NEFA uptake per unit of fat mass in young, healthy, non-obese men [8], and in obese otherwise healthy people [9]. Although the net storage of lipids in adipose tissue (AT) occurs primarily from lipoprotein-derived fatty acid (FA) uptake in the postprandial period [10–12], recently, Shadid et al found that, during the post-absorptive period, circulating NEFAs are stored in subcutaneous AT [13]. During a diet very low in energy (very low calorie diet [VLCD]) when a very low amount of fat is introduced by diet, lipoprotein-derived uptake of NEFAs into AT may play a less significant role than direct NEFA uptake. Compared with other weight loss methods, VLCDs tend to reduce more visceral than subcutaneous AT [14]. The changes, in visceral and subcutaneous AT FA metabolism, after a VLCD, are currently unclear.
The objective of this study was to determine whether VLCD produces a more pronounced decline in fasting NEFA uptake in visceral than subcutaneous AT in proportion with the reduction of the respective masses. Additionally, the effect of VLCD on skeletal muscle NEFA uptake and intra-myocellular lipid accumulation was tested.
Methods
Study design
The study was designed to investigate the effects of a 6-week VLCD regimen on: (1) energy expenditure; (2) whole body and regional fat metabolism using [18F]-fluoro-6-thia-heptadecanoic acid (18F-FTHA) and positron emission tomography (PET), uniformly labelled [U-13C]palmitate and indirect calorimetry; and (3) fat masses, skeletal muscle mass and lipid content using computerised tomography (CT, femoral masses), MRI (abdominal masses) and magnetic resonance spectroscopy (1H-MRS) in obese participants. All daily meals were replaced by diet products (2.3 MJ, 4.5 g fat, 59 g protein and 72 g carbohydrate per day; Nutrifast, Leiras, Finland). After the diet, there was a 1 week recovery period with an isocaloric diet (Electronic Supplementary Material [ESM] Materials and Methods) to avoid the catabolic state.
Participants
Eighteen participants with the metabolic syndrome, as defined by the current International Diabetes Federation (IDF) criteria [15], were recruited through a local newspaper advertisement. Control participants were non-obese. Participants with an eating disorder, known cardiovascular disease, hypertension (blood pressure >160/100 mmHg) or medication for hypertension, previous or present abnormal hepatic or renal function, or oral corticosteroid treatments, were excluded. Participants were instructed not to use any alcohol during the study period. Smoking was an exclusion criterion. The protocol was approved by the Ethics Committee of the Hospital District of Southwest Finland and all participants gave their written informed consent. At the time when the study was approved, in Finland it was not compulsory to register clinical trials internationally, and for this reason this study has not been registered with a clinical trials database.
Study day protocol
The study day started with measurements of anthropometric values (ESM Materials and Methods) and a collection of baseline samples. Then, the infusion of [U-13C]palmitate was started in a subgroup of ten obese participants (nine women and one man) together with indirect calorimetry. PET imaging was started with an injection of 18F-FTHA: the abdominal region was acquired first for 25 min (dynamic scanning), and after 65 to 70 min from the injection, the femoral region was acquired for 10 min (static scanning). In PET images, regions of interest were manually drawn in visceral and subcutaneous (abdominal and femoral) fat and in femoral skeletal muscle to obtain time-activity curves. Together with plasma activity levels, tissue curves were used to calculate fractional NEFA uptake rates (Ki, net influx constant) from dynamic images, and fractional uptake rates (from static images), which were multiplied by serum NEFA levels and divided by the tissue density to obtain NEFA uptake values.
The rate of appearance (Ra) of palmitate was calculated for each sample point using the single-pool non-steady state Steele equations adapted for stable isotope methodology [16]. The adipose insulin resistance index (AIRI) was calculated as described in ESM Materials and Methods. Indirect calorimetry was used to measure whole body carbohydrate and fat oxidation. In the obese participants, resting energy expenditure (REE) was obtained by the calorimetry monitor. Additional details about the study day are reported in the ESM Materials and Methods.
1H-MRS studies
Triacylglycerol content in skeletal muscle was measured from the tibialis anterior muscle, using a 1.5 T MR imager (Gyroscan Intera CV Nova Dual, Philips Medical Systems, the Netherlands) with a flexible surface coil and internal body coil. 1H-MRS spectra were analysed using the LCModel software package (version 2.6-1, www.s-provencher.com/pages/lcmodel.shtml) [9].
OGTT
The OGTT (75 g) was done on a separate day, both before and after, the VLCD in the obese group, and once before imaging studies, in the control group. Blood samples were drawn at 0, 60 and 120 min for determination of plasma glucose, insulin, and C-peptide. Glucose tolerance status was defined according to the 2006 WHO recommendations [17]. The oral glucose insulin sensitivity (OGIS) and HOMA indices were calculated as described in ESM Materials and Methods.
Statistical analysis
Statistical analysis was performed using SPSS/Win statistical program (version 15.0 for Windows; SPSS, Chicago, IL, USA). Data are reported as mean ± SD. The normality of variables was assessed by Shapiro–Wilk test. The Student’s paired t test was used for normally distributed variables to compare results before and after VLCD. Group comparisons between control participants and obese participants before and after VLCD were performed using parametric and nonparametric ANOVA tests. For parametric analysis, a Bonferroni post hoc test was performed and for nonparametric analysis, a Bonferroni-corrected Mann–Whitney U test was used. Correlations were calculated using either Pearson or Spearman tests according to the normality of the variable.
Results
Changes in fat depots and skeletal muscle mass
Obese participants lost 11.2 ± 2.5 kg during the 6 week VLCD period (p < 0.0001) in which loss of fat mass accounted for 7.5 ± 1.3 kg (74%) and fat-free mass (FFM) accounted for 2.9 ± 2.2 kg (26%). All the AT depots decreased significantly (Table 1). Men had initially more visceral AT than women (2.8 ± 0.6 vs 2.0 ± 0.6 kg, p = 0.02) and women showed a tendency for more abdominal subcutaneous AT than men (6.4 ± 1.5 vs 4.9 ± 1.6 kg, p = 0.07). Sex did not have an impact on the loss of fat from these depots. Weight loss decreased intramyocellular lipid content in skeletal muscle from 0.65 ± 0.37% to 0.37 ± 0.24% (p < 0.05). There was no difference in baseline femoral muscle masses between the obese and the non-obese groups, with the former group having more femoral AT than the latter (p < 0.03). Weight loss decreased both femoral adipose (p < 0.0003) and skeletal muscle masses (p < 0.02).
Changes in glucose tolerance status and insulin resistance indices
Before weight loss, one participant had type 2 diabetes mellitus, two had impaired glucose tolerance, five had impaired fasting glucose levels and ten were classified as normoglycaemic. After weight loss, only four participants had impaired fasting glucose and 13 were normoglycaemic. Weight loss improved OGIS (p < 0.01) and AIRI (p < 0.03; Table 1).
Changes in laboratory values
Weight loss did not change serum NEFA levels (Table 1). Women had higher levels than men both before and after weight loss (0.70 ± 0.13 vs 0.47 ± 0.16, p < 0.007; 0.67 ± 0.17 vs 0.41 ± 0.65, p < 0.003 mmol/l, respectively). Weight loss decreased fasting glucose, total cholesterol, LDL-cholesterol and triacylglycerol levels.
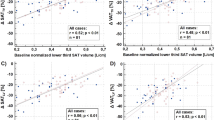
Results from PET data
Group comparisons are shown in Table 1 and Fig. 1. The obese vs the non-obese participants had significantly higher NEFA uptake in visceral AT and this difference persisted after weight loss. NEFA uptake in abdominal subcutaneous AT did not differ among the groups when measured per 100 g of tissue, but it was higher in the whole depot in the obese patients. NEFA uptake in femoral muscle was similar among the groups.
NEFA uptake rates in abdominal AT (a, b) and femoral SAT and muscle (c, d). Uptake rates obtained by dynamic imaging are shown in (a) ([100 g]−1) and (b) (whole depot), whereas relative uptake rates obtained by static imaging are given in (c) ([100 g]−1) and (d) (whole depot). White bars, non-obese participants; dark grey bars, obese group participants before VLCD; light grey bars, obese group participants after weight loss. NEFA uptake (μmol min−1) of both visceral and subcutaneous AT (b) were log10 transformed to perform statistical tests. *p < 0.05, **p < 0.01, ***p < 0.001 vs abdominal subcutaneous AT (same group, paired t test). ††† p < 0.001 vs obese group after diet, ‡‡‡ p < 0.001 vs obese group at baseline. SAT, subcutaneous AT; VAT, visceral AT
In obese individuals, visceral AT was metabolically more active than subcutaneous AT (Fig. 1). Visceral AT took up to four times more NEFAs than abdominal subcutaneous AT per 100 g. The whole visceral AT depot extracted 1.5 times more NEFAs than the abdominal subcutaneous AT depot at baseline and after weight loss. VLCD did not change NEFA uptake in visceral AT, abdominal subcutaneous AT, or femoral skeletal muscle, but decreased the uptake in femoral subcutaneous AT, both per 100 g of tissue (p < 0.006) and in the whole depot (p < 0.002).
Sex effects are reported in Table 2 and Fig. 2. The above comparisons were repeated while accounting for sex as a covariate in the statistical analyses, and the differences between obese and non-obese groups persisted.
Abdominal visceral and subcutaneous AT NEFA uptake rates stratified by sex and group. The variables are subgrouped into non-obese men (white bars) and women (light grey bars); and obese men (dark grey bars) and women (black bars). ***p ≤ 0.001 vs obese women; ††† p ≤ 0.001 vs obese men. ‡ p ≤ 0.05, ‡‡ p ≤ 0.01, ‡‡‡ p ≤ 0.001 vs abdominal subcutaneous AT (same group). SAT, subcutaneous AT; VAT, visceral AT
Visceral AT NEFA uptake was correlated with the HOMA-IR index in controls (r = 0.57, p < 0.03), and in post-VLCD participants, and in the latter group, visceral AT NEFA uptake was associated with fasting glucose levels (r = 0.65, p < 0.002) and the OGIS index (r = −0.76, p < 0.03). No other correlations were found.
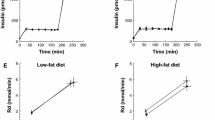
Indirect calorimetry
The 24 h energy expenditure decreased (Table 1). Weight loss increased FFM-adjusted total fat oxidation (p = 0.002), while carbohydrate oxidation decreased (p < 0.0001; Table 3, Fig. 3).
Discussion
Our principal findings were, first, that NEFA uptake in visceral AT in the obese group with the metabolic syndrome, was significantly higher than in any other AT depot, and remained higher after weight loss. Our data are in line with our previous studies in healthy participants and in obese otherwise healthy participants [8, 9], and extend these observations to obese patients with the metabolic syndrome. Dietary NEFA uptake is reported to be higher in visceral than subcutaneous AT in healthy, lean [11] and obese participants [12], although this difference was blunted in extremely obese individuals. We found the same trend in fasting NEFA uptake rates in our obese participants, and the participant with the highest BMI was the only outlier in the relationship between visceral NEFA uptake and BMI (r = 0.78, p = 0.002). Instead, dietary NEFA uptake was reduced in participants with impaired glucose tolerance [10], whereas we did not observe any group difference in our study. Differences in the characteristics (impaired glucose tolerance vs obesity+metabolic syndrome) of the study participants, and the route of tracer administration may explain this discrepancy. More likely, group differences observed during the postprandial period, when AT NEFA uptake and substrate storage are high, may not occur in the fasting state because of lower net uptake and higher lipolysis. We tested if the heterogeneous oral glucose tolerance status at baseline would have influenced the effects of VLCD, and no influence was found. Nonetheless, VLCD diet improved the glucose tolerance status as well as the OGIS of the participants; HOMA-IR did not reach significance, although it improved in 12 out of 17 cases, which is likely because of the large variability observed in fasting insulin levels, especially after VLCD.
Second, obese participants, compared with non-obese controls, had higher total FA uptake in both visceral and abdominal subcutaneous adipose depots, but the difference remained only in the visceral AT after accounting for fat mass.
Third, while weight loss had no effect on either visceral or abdominal subcutaneous AT FA uptake, the uptake in femoral subcutaneous AT decreased. FA uptake in skeletal muscle did not change after weight loss and did not differ between the obese and the non-obese groups. After weight loss, whole body carbohydrate oxidation decreased, while fat oxidation increased. No changes existed in systemic lipolysis.
The evidence that weight loss neither reversed the quantity nor the partitioning of NEFA uptake between abdominal masses, suggests that this trait is independent of changes in metabolic status and insulin resistance indices. In line with our findings, fat metabolism is different in obese compared with non-obese participants, and this impairment remains after weight loss [18, 19]. Although weight loss is associated with a beneficial reduction in adipocyte size [20, 21], and our data showed an improvement of the AIRI, this change is not sufficient to modify the efficiency of AT fatty uptake in obese participants.
Although Shadid et al demonstrated the physiological impact of direct NEFA uptake during the fasting state [13], postprandial NEFA uptake is more relevant under normal conditions [10–12]. However, our VLCD includes a very low content of fats (4.5 g in the study diet), and therefore we presumed that fasting NEFA uptake would gain relative importance, and decline in proportion with the tissue mass. Against our hypothesis, the uptake process, during fasting, did not play a significant role in the pathophysiology of weight loss, and the −20 ± 15% visceral fat mass change was not caused by a change in AT NEFA uptake.
Subcutaneous NEFA uptake per depot and per 100 g of tissue was lower than that in visceral AT, at baseline, with the difference even more pronounced after weight loss. Femoral subcutaneous AT NEFA uptake was reduced by weight loss. Lower body adiposity is considered to be protective against ectopic fat accumulation and metabolic disorders [2]. Our findings may indicate that lower body adiposity is associated with greater metabolic flexibility and adaptability. A reduction in NEFA uptake may be associated with a less pronounced tendency to re-accumulate fat mass in this region. On the one hand, this may confer the advantage of a long-term buffering capacity. On the other hand, the low uptake of FAs in this tissue and their further reduction after dieting may reflect a weak buffering capacity.
We found a significant reduction in intramyocellular lipid droplets (IMCL) content. Our data indicate that weight loss has an impact on intramyocellular lipid stores, enhancing their consumption in skeletal muscle, while leaving the metabolism of plasma NEFA unaltered.
Limitations of this study are noted. Due to the radiation exposure and the demands of the study for the participants, we would have included a placebo group only if a change in the main interest variables occurred. For the same reason, it has not been possible to study also the postprandial metabolic condition that would have been useful in comprehensively elucidating the effect of the diet. In fact, our data suggest that the study of AT NEFA uptake in the fasting state may be insufficient to understand the metabolic mechanisms of weight loss by VLCD in full. The participants were selected according to the IDF metabolic syndrome definition, and therefore they were heterogeneous in terms of glucose tolerance status. Thus, our conclusions are limited to the specific entry criteria chosen in this study, although we tested the confounding effect of heterogeneous glucose tolerance and did not find it to be significant.
Some of our measurements (whole body fat mass in some participants, visceral adipose mass), have been obtained with estimations via formulae, which are validated but still less optimal than direct measurements. A baseline assessment of caloric balance was not performed, nor was the monitoring of dietary intake, and physical activity was assessed by questionnaires only. Therefore, adherence to the diet programme is assumed based on confirmation from the participants and remarkable weight loss.
In conclusion, fasting NEFA uptake does not explain the reduction in abdominal fat masses caused by very low calorie dieting in obese participants with the metabolic syndrome. We found that visceral fat took up quantitatively more NEFAs than subcutaneous fat, even after weight loss.
Abbreviations
- AIRI:
-
Adipose insulin resistance index
- AT:
-
Adipose tissue
- FA:
-
Fatty acid
- FFM:
-
Fat-free mass
- 18F-FTHA:
-
[18F]-Fluoro-6-thia-heptadecanoic acid
- HOMA-βCFI:
-
HOMA-β-cell function index
- IDF:
-
International Diabetes Federation
- MRS:
-
Magnetic resonance spectroscopy
- OGIS:
-
Oral glucose insulin sensitivity index
- Ra:
-
Rate of appearance
- VLCD:
-
Very low calorie diet
References
Ibrahim MM (2010) Subcutaneous and visceral adipose tissue: structural and functional differences. Obes Rev 11:11–18
Manolopoulos KN, Karpe F, Frayn KN (2010) Gluteofemoral body fat as a determinant of metabolic health. Int J Obes (Lond) 34:949–959
Snijder MB, Visser M, Dekker JM et al (2005) Low subcutaneous thigh fat is a risk factor for unfavourable glucose and lipid levels, independently of high abdominal fat. Health ABC Study Diabetol 48:301–308
Okura T, Nakata Y, Yamabuki K, Tanaka K (2004) Regional body composition changes exhibit opposing effects on coronary heart disease risk factors. Arterioscler Thromb Vasc Biol 24:923–929
Westphal SA (2008) Obesity, abdominal obesity, and insulin resistance. Clin Cornerstone 9:23–29
Jakobsen MU, Berentzen T, Sorensen TI, Overvad K (2007) Abdominal obesity and fatty liver. Epidemiol Rev 29:77–87
Sinha R, Dufour S, Petersen KF et al (2002) Assessment of skeletal muscle triglyceride content by (1)H nuclear magnetic resonance spectroscopy in lean and obese adolescents: relationships to insulin sensitivity, total body fat, and central adiposity. Diabetes 51:1022–1027
Hannukainen JC, Kalliokoski KK, Borra RJ et al (2010) Higher free fatty acid uptake in visceral than in abdominal subcutaneous fat tissue in men. Obesity (Silver Spring) 18:261–265
Bucci M, Borra R, Nagren K et al (2011) Human obesity is characterized by defective fat storage and enhanced muscle fatty acid oxidation, and trimetazidine gradually counteracts these abnormalities. Am J Physiol Endocrinol Metab 301:E105–E112
Labbe SM, Grenier-Larouche T, Noll C et al (2012) Increased myocardial uptake of dietary fatty acids linked to cardiac dysfunction in glucose-intolerant humans. Diabetes 61:2701–2710
Labbe SM, Grenier-Larouche T, Croteau E et al (2011) Organ-specific dietary fatty acid uptake in humans using positron emission tomography coupled to computed tomography. Am J Physiol Endocrinol Metab 300:E445–E453
Votruba SB, Mattison RS, Dumesic DA, Koutsari C, Jensen MD (2007) Meal fatty acid uptake in visceral fat in women. Diabetes 56:2589–2597
Shadid S, Koutsari C, Jensen MD (2007) Direct free fatty acid uptake into human adipocytes in vivo: relation to body fat distribution. Diabetes 56:1369–1375
Chaston TB, Dixon JB (2008) Factors associated with percent change in visceral versus subcutaneous abdominal fat during weight loss: findings from a systematic review. Int J Obes (Lond) 32:619–628
International Diabetes Federation (2006) The IDF consensus worldwide definition of the metabolic syndrome. http://www.idf.org/metabolic-syndrome
van Loon LJ, Manders RJ, Koopman R et al (2005) Inhibition of adipose tissue lipolysis increases intramuscular lipid use in type 2 diabetic patients. Diabetologia 48:2097–2107
World Health Organization (2006) Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia. http://whqlibdoc.who.int/publications/2006/9241594934_eng.pdf
Thyfault JP, Kraus RM, Hickner RC, Howell AW, Wolfe RR, Dohm GL (2004) Impaired plasma fatty acid oxidation in extremely obese women. Am J Physiol Endocrinol Metab 287:E1076–E1081
Berggren JR, Boyle KE, Chapman WH, Houmard JA (2008) Skeletal muscle lipid oxidation and obesity: influence of weight loss and exercise. Am J Physiol Endocrinol Metab 294:E726–E732
Pasarica M, Tchoukalova YD, Heilbronn LK et al (2009) Differential effect of weight loss on adipocyte size subfractions in patients with type 2 diabetes. Obesity (Silver Spring) 17:1976–1978
Bjorntorp P, Carlgren G, Isaksson B, Krotkiewski M, Larsson B, Sjostrom L (1975) Effect of an energy-reduced dietary regimen in relation to adipose tissue cellularity in obese women. Am J Clin Nutr 28:445–452
Acknowledgements
The authors thank the staff of the Turku PET Centre for their excellent technical assistance.
Funding
The study was conducted within the Centre of Excellence in Molecular Imaging in Cardiovascular and Metabolic Research, supported by the Academy of Finland, the University of Turku, Turku University Hospital and Åbo Academy. HEPADIP EU FP6 program, the Academy of Finland, the Novo Nordisk foundation, the Finnish Cultural Foundation, the South Western Finland Cultural Foundation, Juho Vainio Foundation, the Turku University Foundation, the Finnish Sports Institute Foundation and the Finnish Sports Research Foundation supported this study.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
MB and ACK analysed and interpreted the data, and drafted the article. BAF, RMB, AV, RB, VS, TP, MH-S, TV and RP analysed data and revised the manuscript; AV and ACK were involved in the acquisition of the data. PN was responsible for the conception of the study and drafting the article. PI, KNF, JCH and KK made substantial contributions to the conception and design of the study, and interpretation of data, and revised the article critically for important intellectual content. All authors approved the final version. MB is the guarantor of this work.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Materials and Methods
(PDF 169 kb)
ESM Fig. 1
(PDF 144 kb)
Rights and permissions
About this article
Cite this article
Bucci, M., Karmi, A.C., Iozzo, P. et al. Enhanced fatty acid uptake in visceral adipose tissue is not reversed by weight loss in obese individuals with the metabolic syndrome. Diabetologia 58, 158–164 (2015). https://doi.org/10.1007/s00125-014-3402-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-014-3402-x