Abstract
Aims/hypothesis
This study examined the efficacy of supplemental l-carnitine as an adjunctive diabetes therapy in mouse models of metabolic disease. We hypothesised that carnitine would facilitate fatty acid export from tissues in the form of acyl-carnitines, thereby alleviating lipid-induced insulin resistance.
Materials and methods
Obese mice with genetic or diet-induced forms of insulin resistance were fed rodent chow ± 0.5% l-carnitine for a period of 1–8 weeks. Metabolic outcomes included insulin tolerance tests, indirect calorimetry and mass spectrometry-based profiling of acyl-carnitine esters in tissues and plasma.
Results
Carnitine supplementation improved insulin-stimulated glucose disposal in genetically diabetic mice and wild-type mice fed a high-fat diet, without altering body weight or food intake. In severely diabetic mice, carnitine supplementation increased average daily respiratory exchange ratio from 0.886 ± 0.01 to 0.914 ± 0.01 (p < 0.01), reflecting a marked increase in systemic carbohydrate oxidation. Similarly, under insulin-stimulated conditions, carbohydrate oxidation was higher and total energy expenditure increased from 172 ± 10 to 210 ± 9 kJ kg fat-free mass−1 h−1 in the carnitine-supplemented compared with control animals. These metabolic improvements corresponded with a 2.3-fold rise in circulating levels of acetyl-carnitine, which accounts for 86 and 88% of the total acyl-carnitine pool in plasma and skeletal muscle, respectively. Carnitine supplementation also increased several medium- and long-chain acyl-carnitine species in both plasma and tissues.
Conclusions/interpretation
These findings suggest that carnitine supplementation relieves lipid overload and glucose intolerance in obese rodents by enhancing mitochondrial efflux of excess acyl groups from insulin-responsive tissues. Carefully controlled clinical trials should be considered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In mammals, l-carnitine is a conditionally essential nutrient that can be synthesised endogenously from lysine and methionine or obtained from the diet, primarily from red meat [1]. Carnitine serves as essential substrate for carnitine palmitoyltransferase 1, the enzyme that catalyses the initial step in the transport of long-chain fatty acids into the mitochondrial matrix. This well-known essential role of carnitine in fatty acid oxidation has led to 20 years of weight loss and exercise enhancement experiments. Yet, convincing evidence to show that carnitine supplementation has favourable metabolic effects in healthy people is still lacking. In contrast, carnitine has proven beneficial in circumstances of disease. As early as 1986 dietary carnitine supplementation was shown to reduce concentrations of total lipids and triacylglycerols in a variety of experimental rat models of hepatic steatosis [2–5]. Moreover, the foregoing changes in the plasma and hepatic concentrations of various classes of lipids were found to be inversely related to the carnitine supplementation level, up to a daily dose of 0.5% l-carnitine [2, 3, 5].
Despite its potential to improve insulin sensitivity, almost all studies on carnitine supplementation have focused on the role of carnitine in regulating fatty acid oxidation and lipid metabolism, whereas only a few have examined changes in glucose oxidation. Although sparse, positive outcomes have been reported in humans. For example, carnitine infusion during a hyperinsulinaemic–euglycaemic clamp has been shown to improve glucose disposal [6–10]. Additionally, a study from China [11] and another from Italy [12] found that carnitine lowered circulating lipids but did not improve fasting glucose levels. A recent study conducted in Iran [13] reported that dietary carnitine lowered fasting glucose levels, but increased triacylglycerol levels.
To our knowledge, only two mouse studies have investigated carnitine treatment of diabetes, both of which reported positive outcomes. One reported that oral administration of a zinc–carnitine complex lowered the high blood glucose levels and improved glucose tolerance in KK-Ay mice with type 2 diabetes [14]. A more recent study [15] examined the effects of carnitine in liver-specific carcinoembryonic antigen-related cell adhesion molecule 1 (CEACAM1)-deficient mice. CEACAM1 regulates insulin action by promoting insulin receptor-mediated insulin uptake and degradation in a phosphorylation-dependent manner. In the same study, treatment of liver-specific S503A CEACAM1-deficient mice with carnitine reduced plasma NEFA and improved insulin resistance.
The current investigation was undertaken to test our hypothesis that carnitine supplementation might improve insulin action in obese diabetic mice by facilitating tissue formation and export of acyl-carnitines. Our findings indicate that carnitine supplementation increased the actions of insulin in rodent models of metabolic dysfunction. The level of dietary supplementation used in our study was equivalent to an intake of 2 g l-carnitine/day for humans, costing less than US$1.00 per day. Should these findings be replicated in humans, l-carnitine may be a relatively inexpensive adjunctive treatment for type 2 diabetes and related metabolic disorders.
Materials and methods
Animals and diets
All mice were from breeding colonies maintained at Pennington Biomedical Research Center. Experimental procedures involving mice were approved by the Pennington Biomedical Research Center Institutional Animal Care and Use Committee. All mice were fed Purina Rodent Chow no. 5015 (Purina Mills, St Louis, MO, USA) prior to being fed the semi-purified diets with or without 0.5% l-carnitine. Free access to food and water were provided.
In experiment 1 we used beta actin promoter agouti mice (BAP-agouti), an obese diabetic mouse model, generated and maintained on the FVB/N background and carrying a transgene with the beta actin promoter driving the expression of agouti, resulting in agouti expression in all tissues [16]. The widespread ectopic expression of agouti in these transgenic mice recapitulates the dominant mutations at the Agouti locus collectively known as the yellow obese syndrome [16]. Two weeks prior to the first insulin sensitivity test, 8-month-old mice were switched from the Purina chow diet to a semi-purified diet (D12450B; Research Diets, New Brunswick, NJ, USA) consisting of: 10% of energy from fat, 20% of energy from protein, 70% of energy from carbohydrate. After baseline values were established, the experiment was carried out as outlined in Table 1.
The mice used in experiment 2 were on a mixed Black Swiss/129 background. Approximately 40 male mice between 4 and 5 months of age were fed a semi-purified diet (10% of energy from fat, 20% of energy from protein, 70% of energy from carbohydrate; Research Diets) for 2 weeks and screened for impaired glucose tolerance (i.e. blood glucose values greater than 20 mmol/l 60 min after i.p. glucose [2 mg/kg body weight]). Eight mice were identified as glucose-intolerant and baseline insulin sensitivity and glucose tolerance tests were performed in them. The mice were then placed on the carnitine-supplemented diet for 1 week.
In a third model of insulin resistance, 6-week-old male C57BL/6J mice were fed a high-fat diet (45% of energy from fat, 20% of energy from protein, 35% of energy from carbohydrate; Research Diets) ±0.5% l-carnitine for 8 weeks.
Insulin sensitivity
The mouse models used in experiments 1 and 2 are affected by severe insulin resistance, which is evidenced by their failure to reduce blood glucose levels even when challenged with extremely high insulin doses. Based on preliminary experiments to optimise insulin tolerance tests in these mice, a high dose of 1 U per mouse was chosen for evaluation of the glucose-lowering properties of l-carnitine supplementation. In contrast, the high fat-fed mice exhibited a more moderate form of insulin resistance and insulin tolerance tests were performed with a lower dose of 1 U/kg body weight.
Indirect calorimetry
Obese diabetic BAP-agouti mice were fed the semi-purified diet ±0.5% l-carnitine (see above) for 4 weeks prior to indirect calorimetry. During this time, food intake and body weight were measured every other day and body composition was measured weekly. Indirect calorimetry was then performed as previously described [17] using a 16-chamber Oxymax system (Columbus Instruments, Columbus, OH, USA). Mice were acclimatised to the system for 3 days prior to measurement. After 2 days of measurements, the mice were given an i.p. bolus of insulin (1 U per mouse) at 07.00 h for the final day of measurements. Periodic movements were measured by a motion detector in the system to estimate physical activity throughout the indirect calorimetry study. Energy expenditure (kJ kg fat-free mass [FFM]−1 h−1) was calculated using oxygen consumption (VO2) and the following equation: \( {\text{EE}} = {{\left( {VO_{2} \times {\left[ {3.815 + {\left\{ {1.232 \times {\text{RER}}} \right\}}} \right]} \times 4.1868} \right)}} \mathord{\left/ {\vphantom {{{\left( {VO_{2} \times {\left[ {3.815 + {\left\{ {1.232 \times {\text{RER}}} \right\}}} \right]} \times 4.1868} \right)}} {{\text{kg}}\,{\text{FFM}}}}} \right. \kern-\nulldelimiterspace} {{\text{kg}}\,{\text{FFM}}} \), where EE is energy expenditure and RER is respiratory exchange ratio. RER, VO2 and energy expenditure data were analysed as 2-h blocks.
Whole homogenate preparation
Mice were killed by cervical dislocation and tissues were either used immediately or frozen in liquid nitrogen for storage at −80°C. Approximately 50 mg fresh red and white gastrocnemius muscle and liver were immediately placed into ice-cold modified sucrose EDTA medium (SET) on ice containing 250 mmol/l sucrose, 1 mmol/l EDTA and 10 mmol/l Tris–HCl, pH 7.4. Tissue samples were minced thoroughly with scissors and then additional SET buffer was added to achieve a 20-fold diluted (weight/volume) suspension. The minced samples were homogenised in a Potter-Elvehjem glass homogeniser (Fisher Scientific, Waltham, MA, USA) at ten passes across 30 s at 1,200 rev/min with a motor-driven Teflon pestle.
Pyruvate dehydrogenase activity
Pyruvate dehydrogenase (PDH) activity was determined in the fresh red and white gastrocnemius muscle and liver homogenates by measuring 14CO2 produced from [1] pyruvic acid. We preincubated 40 μl of 20-fold diluted tissue homogenates in an atmosphere of 95% O2 and 5% CO2 at 30°C for 15 min. Next 160 μl of reaction mixture (pH 7.4) was added to the preincubated muscle homogenates. Final concentrations of the incubation mixture were (in mmol/l): sucrose, 100; Tris–HCl, 10; potassium phosphate, 5; potassium chloride, 80; magnesium chloride, 1; malate, 0.1; ATP, 2; coenzyme A (CoA), 0.05; dithiothreitol, 1; EDTA, 0.2; and bovine serum albumin, 0.3%. The substrate used was 10 mmol/l [1] pyruvic acid (1,800 Bq). After 60 min of incubation at 30°C, 100 μl of sulphuric acid (4 mmol/l) was injected to stop the reaction and evolve CO2 from the incubation media. CO2 produced during the 60-min incubation was trapped with 200 μl of 2 mol/l sodium hydroxide. Trapped 14CO2 was determined by liquid scintillation counting by use of 5 ml liquid scintillation cocktail.
Acyl-carnitine measurement
Soleus muscle, liver, adipose tissue and plasma samples were removed from obese diabetic BAP-agouti mice in the fed state. Acyl-carnitines were measured at the Metabolomics and Biomarker Core Facility at Duke University. Briefly, plasma and tissue extracts were processed as previously described [18, 19] and analysed by direct-injection electrospray tandem mass spectrometry, using a Quattro Micro LC-MS system (Waters-Micromass, Milford, MA, USA) equipped with an HTS-PAL autosampler (Leap Technologies, Carrboro, NC, USA), an 1,100 HPLC solvent delivery system (Agilent Technologies, Santa Clara, CA, USA) and a data system running MassLynx software (Waters-Micromass).
Measurement of NEFA, β-hydroxybutyrate, lactate and glycerol
Plasma levels of NEFA and β-hydroxybutyrate were measured using kits (Wako Chemicals, Richmond, VA, USA). Plasma levels of lactate were measured using a kit (Instruchemie, Delfzijl, the Netherlands). Glycerol was measured in deproteinised, neutralised medium extracts [20] according to the enzymatic method of Laurell and Tibbling [21].
Statistical analysis
All data presented are mean±SEM. Statistical analysis of studies comparing genotype and diet used a two-way ANOVA, followed by all pair-wise multiple comparison procedures (Student–Newman–Keuls test). Statistical analysis used SigmaStat for Windows version 2.03 (SPSS, Chicago, IL, USA). For studies comparing two groups, statistical analysis used the Student’s t test.
Results
Effects of carnitine supplementation on insulin sensitivity
The efficacy of carnitine supplementation as an adjunctive diabetes therapy was tested in three different models of insulin resistance: (1) an obese diabetic transgenic mouse model, (BAP-agouti) [16]; (2) out-bred mice on a mixed Black Swiss/129 background fed a rodent diet with moderate fat content (10% energy as fat); (3) C57BL/6J fed a high-fat diet (45% energy as fat) for 8 weeks, representing diet-induced obesity.
The BAP-agouti mice are obese (50 g body weight and 30% body fat) (Table 1) and become severely diabetic, with blood glucose levels rising above 30 mmol/l following a glucose tolerance test. These mice are remarkably unresponsive to insulin administration (i.e. no significant change in blood glucose following 1 U insulin per mouse) (Fig. 1a). After 3 weeks of 0.5% l-carnitine supplementation insulin-stimulated glucose disposal improved, with glucose values dropping to near 5 mmol/l (Fig. 1a). Following carnitine supplementation, the mice were then placed back on the non-supplemented diet for 3 weeks and insulin-stimulated glucose disposal reverted to an intermediate level. After 6 weeks without supplementation, insulin sensitivity reverted to a diabetic state. Notably, however, one additional week of carnitine supplementation restored insulin sensitivity. This second round of supplementation reduced basal glucose levels, suggesting that prolonged carnitine therapy might attenuate diabetes-associated increases in hepatic glucose production. Body weight and composition did not change during the 12-week study (Table 1), suggesting that carnitine did not alter food intake.
Effects of dietary carnitine supplementation on blood glucose levels following insulin administration. a Transgenic, BAP-agouti obese diabetic mice (n = 15) were fed a semi-purified diet and given an insulin sensitivity test as described in Materials and methods section. The mice were then placed on the same diet containing 0.5% l-carnitine for 3 weeks and the insulin sensitivity test was repeated. The mice were returned to the unsupplemented diet for 6 weeks and insulin sensitivity was measured at 3 weeks (3-week wash-out) and 6 weeks (6-week wash-out). The mice were then placed back on the l-carnitine-supplemented diet for 1 week until final insulin sensitivity test. Closed diamond, beginning; closed square, first carnitine supplementation; open square, second carnitine supplementation; closed triangle, 3-week washout; open triangle, 6-week wash-out. b Wild-type mice on a mixed Black Swiss/129 background (n = 8) were fed a semi-purified diet and given an insulin sensitivity test as described in Materials and methods. The mice were then placed on the same diet containing 0.5% l-carnitine for 1 week and the insulin sensitivity test was repeated. Values are mean±SEM. * p < 0.05 for difference from non-supplemented mice. Closed diamond, non-supplemented diet; closed square, diet supplemented with 0.5% l-carnitine
This first experiment clearly demonstrated that dietary carnitine improved insulin-stimulated glucose disposal in an obese diabetic mouse model. We next tested the ability of carnitine to improve glucose disposal in out-bred mice. Approximately 40 male mice between 4 and 5 months of age were screened for impaired glucose tolerance as described in Materials and methods. In eight mice that were identified as glucose intolerant, carnitine supplementation improved glucose disposal, consistent with the outcome in the obese transgenic mice (Fig. 1b). In this second cohort of mice carnitine supplementation decreased basal glucose levels, again implying that hepatic insulin sensitivity may have improved with the intervention. Body weight was unchanged by carnitine supplementation (data not shown). Importantly, these results demonstrate that the salutary actions of l-carnitine were not limited to the transgenic mice.
The effects of dietary carnitine supplementation were next tested in inbred C57BL/6J mice that are susceptible to obesity and diabetes when fed a high-fat diet. Six-week-old male C57BL/6J mice were fed a high-fat diet ±0.5% l-carnitine for 8 weeks. Final body weight was not different between the non-supplemented group (34.7 ± 0.7 g) and the l-carnitine-supplemented group (32.9 ± 1.0 g). Daily food intake, measured in the final week of the experiment, was similar between the non-supplemented group (4.7 ± 0.3 g/day) and the l-carnitine-supplemented group (4.9 ± 0.4 g/day). C57BL/6J mice receiving carnitine supplementation were partially protected against the development of diet-induced insulin resistance (Fig. 2). Plasma levels of NEFA, β-hydroxybutyrate, glycerol and lactate were similar between the non-supplemented and carnitine-supplemented mice after 8 weeks on the high-fat diet (data not shown). In aggregate, results from these initial experiments demonstrated that carnitine supplementation effectively improved insulin-stimulated glucose disposal in three distinct rodent models of insulin resistance.
Effects of dietary carnitine supplementation on the development of insulin resistance in mice fed high-fat diets. a Six-week-old C57BL/6 male mice were fed a diet containing 10% of energy from fat for 1 week before baseline insulin sensitivity was assessed. b The mice were then switched to a high-fat diet (45% energy) −0.5% l-carnitine for 8 weeks and insulin sensitivity was re-assessed. Values are mean±SEM, n = 8 per group. * p < 0.05 for difference from non-supplemented mice. Closed diamonds, non-supplemented diet; closed squares, diet supplemented with 0.5% l-carnitine
Effects of carnitine supplementation on substrate utilisation
In a fourth study, obese diabetic BAP-agouti mice were fed a semi-purified diet—0.5% l-carnitine for 4 weeks and indirect calorimetry was used to determine the effects of carnitine supplementation on substrate utilisation and energy expenditure as described in Materials and methods. Basal carbohydrate oxidation was higher in the carnitine-supplemented group (average daily RER 0.886 ± 0.01 in control group, 0.914 ± 0.01 in carnitine-supplemented group; p < 0.01) (Fig. 3b). Immediately upon insulin administration, the RER rose quickly to values near 1.0 in the carnitine-supplemented group, but remained below 0.9 in the non-supplemented group. However, during the later post-insulin phase RER dropped to similarly low levels in both groups, suggesting increased fat oxidation due to rebound hypoglycaemia.
Effects of carnitine supplementation on substrate utilisation, measured in terms of energy expenditure (EE) (a), RER (b) and activity (c). Transgenic, BAP-agouti obese diabetic mice were fed a semi-purified −0.5% l-carnitine diet for 4 weeks as described. The mice were then placed in the Oxymax CLAMS system for a 3-day acclimatisation period, before measurements began. After 2 days of measurements the mice were given an i.p. bolus of insulin (1 U per mouse) at 07.00 hours for the final day of data collection. Values are mean±SEM. Filled squares, control group, n = 7; filled circles, carnitine group, n = 8
Total energy expenditure over 24 h tended to be higher in the carnitine-supplemented mice, although the difference between groups did not reach statistical significance. However, in the period following insulin administration, total body energy expenditure increased in the carnitine-supplemented compared with control mice (172 ± 10 vs 210 ± 9 kJ kg FFM−1 h−1; p < 0.01). Physical activity was unchanged in the carnitine-supplemented group compared with the control group. The increased energy expenditure in the carnitine-treated animals in response to insulin was probably caused by increased insulin sensitivity and subsequent glucose oxidation. Taken together, these data clearly demonstrate that in obese diabetic mice supplemental carnitine improves insulin-stimulated glucose utilisation and the abnormalities of fuel metabolism that are typical of type 2 diabetes.
Effects of carnitine supplementation on acyl-carnitine concentrations
Our hypothesis predicted that increased carnitine in the diet might improve glucose metabolism by sequestering excess acyl moieties. Tandem mass spectrometry was used to analyse 36 independent acyl-carnitine species ranging in size from two to 22 carbons in extracts from plasma, liver, skeletal muscle (soleus) and white adipose tissue (inguinal) of non-diabetic mice, type 2 diabetic mice (BAP-agouti transgenic mice) and type 2 diabetic mice supplemented with carnitine for 3 weeks (Fig. 4; Electronic supplementary material [ESM] Tables 1 and 2). The skeletal muscle content of most acyl-carnitine species tended to be lower in the diabetic than in non-diabetic mice, but on the whole changes in total acyl-carnitines did not achieve statistical significance (p = 0.08) (Fig. 4, ESM Table 1). Acetyl-carnitine accounted for 86% of the total skeletal muscle acyl-carnitine pool and was reduced by 25% in the type 2 diabetic mice (p = 0.08). Carnitine supplementation increased skeletal muscle acetyl-carnitine content 75% (p < 0.01), thus restoring levels in diabetic mice to those observed in their non-diabetic counterparts. Additionally, skeletal muscle acyl-carnitines as a whole were significantly elevated in the carnitine-supplemented type 2 diabetic mice (p < 0.01) when compared with the non-supplemented type 2 diabetic mice. Acyl-carnitine content in liver was similar between diabetic and control animals, but several species were elevated by carnitine supplementation. In adipose tissue, several of the short/odd-chain and dicarboxylic species were decreased by diabetes, whereas the long-chain acyl-carnitines were dramatically elevated in the diabetic state. Similar to skeletal muscle, carnitine supplementation increased most acyl-carnitine species in adipose tissue (Fig. 4).
Effect of carnitine supplementation on acyl-carnitine concentrations in plasma (a), soleus muscle (b), liver (c) and white adipose tissue (d). Acyl-carnitines were measured by tandem mass-spectrometry in tissues from lean non-diabetic mice (control, white bars), transgenic (BAP-agouti, black bars) obese diabetic mice and transgenic (BAP-agouti, grey bars) obese diabetic mice + dietary 0.5% l-carnitine as described in Materials and methods. Data are means±SEM. n = 5 per group. ** p < 0.01 for difference from control mice. # p < 0.01 for difference from diabetic mice. SCAC, short-chain acyl-carnitine (C2–C6); MCAC, medium-chain acyl-carnitine (C8–C12); LCAC, long-chain acyl-carnitine (C14–C22)
The most striking finding was the effect of carnitine supplementation on circulating acyl-carnitines (Fig. 4, ESM Table 1). Plasma levels of most acyl-carnitine species increased in response to carnitine supplementation, and the magnitude of these systemic increases was much greater than in tissues. For instance, plasma acetyl-carnitine concentration, which was approximately 700 pmol/100 μl before supplementation, increased more than twofold after supplementation. The robust changes in plasma acyl-carnitine levels, relative to those measured in tissues, implies efficient export of these metabolites from the source tissues into the general circulation.
PDH plays a key role in shifting mitochondrial substrate selection between glucose and fatty acids. When PDH is active, the acetyl-CoA entering the tricarboxylic acid cycle for ATP production is derived primarily from glucose. Conversely, high rates of fatty acid β-oxidation lead to a rise in mitochondrial acetyl-CoA concentration, which in turn inhibits PDH activity and glucose oxidation. Because supplemental carnitine promoted glucose oxidation in diabetic mice, we reasoned that the improvements in glucose disposal might be related to an increase in PDH activity. To address this possibility, we examined the effect of carnitine on PDH activity in red and white skeletal muscle as described in the Materials and methods section. Addition of 0.5 mmol/l carnitine to the assay buffer increased PDH activity in red and white skeletal muscle (Fig. 5). Carnitine-induced stimulation of PDH activity has also been reported in isolated human skeletal muscle mitochondria [22].
Effects of carnitine on pyruvate dehydrogenase activity. PDH activity was assessed in red and white skeletal muscle ±0.5 mmol/l l-carnitine as described in Materials and methods. Black bars, red muscle; grey bars, white muscle. ** p < 0.01 for difference from control group
Discussion
Considerable evidence supports the notion that elevated circulating NEFA lead to ectopic accumulation of lipids in skeletal muscle and liver. In addition, numerous studies have demonstrated a strong association between tissue triacylglycerol content and the pathogenesis of insulin resistance [23–26]. Rather than acting as a direct insulin-desensitising mediator, intramuscular triacylglycerol is thought to serve as a marker and/or precursor of other lipid metabolites that impede insulin signalling. Leading candidate molecules include the long-chain fatty acyl CoAs, which have been shown to activate protein kinase C theta [27], resulting in serine phosphorylation and subsequent inhibition of IRS-1 tyrosine phosphorylation. Long-chain CoAs are also precursors of diacylglycerols and ceramide. Diacylglycerol levels are elevated in many models of insulin resistance [28] and directly activate protein kinase C [29–32]. Ceramides activate a protein phosphatase that dephosphorylates AKT/protein kinase B, resulting in inhibition of GLUT4 translocation and glycogen synthesis [33, 34]. Thus, strong evidence suggests that intramuscular long-chain CoA accumulation is detrimental to insulin signalling. Accordingly, treatments that lower long-chain CoA accumulation, such as carnitine, would be expected to improve insulin sensitivity.
More than four decades ago, Randle [35] proposed that increased fatty acid oxidation inhibits glucose oxidation in part due to the intramitochondrial accumulation of acetyl-CoA. High intramitochondrial acetyl-CoA concentrations activate pyruvate dehydrogenase kinase, which in turn phosphorylates PDH, rendering the enzyme less active. Through metabolic conversions that have been well-characterised, intramitochondrial acetyl-CoA can be oxidised via the tricarboxylic acid cycle or transported into the cytosol as citrate. Alternatively, the CoA moiety of the acetyl unit can be exchanged for a carnitine via the action of carnitine acetylransferase, an enzyme present in the mitochondrial matrix. The product of this under-appreciated reaction, acetyl-carnitine, can then be transported out of the mitochondria. Indeed, in vitro experiments have demonstrated that addition of carnitine to isolated mitochondria decreases the acetyl-CoA:CoA ratio [36, 37] and increases PDH activity [22].
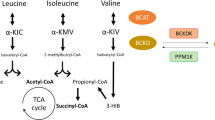
In the present study, carnitine supplementation significantly increased both tissue and plasma acetyl-carnitine levels in type 2 diabetic mice (Fig. 4). Carnitine supplementation also increased basal and insulin-stimulated whole-body RER (Fig. 2) as well as PDH activity (Fig. 5). Therefore, it is possible that high levels of carnitine short-circuit the Randle cycle by sequestering inhibitory acetyl-CoA units as acetyl-carnitine and concomitantly increasing free CoA levels. Lowering of the mitochondrial acetyl-CoA:CoA ratio would then favour glucose oxidation (Fig. 6). Surprisingly, plasma levels of NEFA, β-hydroxybutyrate, glycerol and lactate were not significantly different between the non-supplemented and carnitine-supplemented mice after 8 weeks on the high-fat diet. Thus, at least in the diet-induced obesity model, the underlying mechanism of action appears unrelated to whole-body fatty acid oxidation. Recent evidence suggests that mitochondrial fatty acid overload, resulting in incomplete β-oxidation and intramuscular accumulation of ‘lipotoxic metabolites,’ might contribute to mitochondrial dysfunction and insulin resistance [27, 38]. Thus, carnitine-mediated sequestering of toxic lipid metabolites may have benefited both mitochondrial performance and insulin signalling.
Potential mechanisms for carnitine’s effects on insulin sensitivity. Increased lipid supply to skeletal muscle results in an accumulation of long-chain acyl-CoA (LC-COA), diacylglycerols (DAG), ceramides and acetyl-CoA, which are potent inhibitors of insulin signalling and glucose oxidation. LC-COA and DAG can activate protein kinase C (PKC) theta, resulting in serine phosphorylation and subsequent inhibition of IRS-1 tyrosine phosphorylation. Ceramides activate protein phosphatase that dephosphorylates AKT/protein kinase B (PKB) resulting in inhibition of GLUT4 translocation. Acetyl-CoA activates pyruvate dehydrogenase kinase (PDK), which inactivates pyruvate dehydrogenase (PDH) by phosphorylation. Supplemental carnitine will sequester the acyl moieties and improve insulin signalling and glucose oxidation
The well-known essential role of carnitine in permitting long-chain fatty acid oxidation has prompted 20 years of weight loss and exercise performance studies to examine the potential metabolic benefits of this nutrient. Yet this rather large body of literature still lacks convincing evidence of measurable gains in healthy individuals. The positive effects of carnitine supplementation observed in the current experiments suggest that chronic metabolic stress can result in secondary carnitine deficiency, particularly in skeletal muscle. This contention is further supported by our finding that most acyl-carnitine species in skeletal muscle were reduced under the severe diabetic conditions of the agouti transgenic mice, which was not the case in plasma, liver or white adipose tissue. Perhaps a persistently high fatty acid burden on muscle mitochondria eventually exhausts the tissue’s free carnitine pool, in a failed attempt to detoxify the accumulating lipid metabolites. In mammals, carnitine can be synthesised endogenously from lysine and methionine or obtained from the diet, primarily from red meat [1]. Additionally, diabetic renal dysfunction may also contribute to secondary carnitine deficiency, because the kidneys are not only responsible for reabsorption, but also serve as a major site of carnitine biosynthesis. Moreover, excretion of acyl-carnitines is increased in type 2 diabetes [39]. Thus, a number of factors (poor diet, decreased carnitine synthesis, increased tissue acyl-carnitine synthesis and increased urinary excretion) may lead to a secondary carnitine deficiency in diabetic subjects.
Most carnitine research has focused on carnitine palmitoyl transferase and long-chain fatty acid oxidation. However, short-chain acyl-carnitines (6C or less) are the most abundant acyl-carnitines, constituting 99% of the total acyl-carnitines in skeletal muscle, 95% in plasma, 96% in white fat and 93% in liver. Given the overwhelming abundance of these species, more attention to metabolism of short-chain CoAs and the precise function of carnitine acetyl transferase appears warranted. Also worth consideration is the possibility that carnitine acts through mechanisms that are independent of this putative detoxifying role and/or that acyl-carnitines themselves function as signalling molecules.
In summary, we have shown that carnitine supplementation can produce dramatic improvements in whole-body glucose homeostasis in multiple mouse models of obesity and diabetes. l-Carnitine is a US Food and Drug Administration-approved nutraceutical treatment for inborn mitochondrial disorders; however, little consideration has been given to its potential use as an adjunctive diabetes therapy. Notably, growing evidence implicates mitochondrial dysfunction as a central component of both acquired and inherited forms of insulin resistance [25]. In light of this emerging viewpoint, perhaps type 2 diabetes should be approached as yet another mitochondrial disorder that requires carnitine supplementation. Carefully controlled clinical trials are now warranted.
Abbreviations
- CEACAM1:
-
carcinoembryonic antigen-related cell adhesion molecule 1
- BAP-agouti:
-
beta actin promoter agouti
- CoA:
-
coenzyme A
- FFM:
-
fat-free mass
- PDH:
-
pyruvate dehydrogenase
- RER:
-
respiratory exchange ratio
- SET:
-
sucrose EDTA medium
- VO2 :
-
oxygen consumption
References
Vaz FM, Wanders RJ (2002) Carnitine biosynthesis in mammals. Biochem J 361:417–429
Rhew TH, Sachan DS (1986) Dose-dependent lipotropic effect of carnitine in chronic alcoholic rats. J Nutr 116:2263–2269
Sachan DS, Dodson WL (1992) Effects of l-carnitine on carbon tetrachloride-induced changes in serum and liver lipids and acylcarnitines. J Environ Pathol Toxicol Oncol 11:125–129
Sachan DS, Ruark RA (1985) Distribution of carnitine and acylcarnitine in small intestine of carnitine-supplemented and fasted rats. J Nutr 115:865–871
Sachan DS, Yatim AM (1992) Suppression of aflatoxin B1-induced lipid abnormalities and macromolecule-adduct formation by l-carnitine. J Environ Pathol Toxicol Oncol 11:205–210
Capaldo B, Napoli R, Di Bonito P, Albano G, Sacca L (1991) Carnitine improves peripheral glucose disposal in non-insulin-dependent diabetic patients. Diabetes Res Clin Pract 14:191–195
De Gaetano A, Mingrone G, Castagneto M, Calvani M (1999) Carnitine increases glucose disposal in humans. J Am Coll Nutr 18:289–295
Giancaterini A, De Gaetano A, Mingrone G et al (2000) Acetyl-l-carnitine infusion increases glucose disposal in type 2 diabetic patients. Metabolism 49:704–708
Mingrone G (2004) Carnitine in type 2 diabetes. Ann N Y Acad Sci 1033:99–107
Mingrone G, Greco AV, Capristo E et al (1999) l-Carnitine improves glucose disposal in type 2 diabetic patients. J Am Coll Nutr 18:77–82
Liang Y (1998) The effects of oral l-carnitine treatment on blood lipid metabolism and the body fat content in the diabetic patient. Asia Pac J Clin Nutr 7:192–195
Derosa G, Cicero AF, Gaddi A, Mugellini A, Ciccarelli L, Fogari R (2003) The effect of l-carnitine on plasma lipoprotein(a) levels in hypercholesterolemic patients with type 2 diabetes mellitus. Clin Ther 25:1429–1439
Rahbar AR, Shakerhosseini R, Saadat N, Taleban F, Pordal A, Gollestan B (2005) Effect of l-carnitine on plasma glycemic and lipidemic profile in patients with type II diabetes mellitus. Eur J Clin Nutr 59:592–596
Yoshikawa Y, Ueda E, Sakurai H, Kojima Y (2003) Anti-diabetes effect of Zn(II)/carnitine complex by oral administration. Chem Pharm Bull (Tokyo) 51:230–231
Dai T, Abou-Rjaily GA, Al-Share QY et al (2004) Interaction between altered insulin and lipid metabolism in CEACAM1-inactive transgenic mice. J Biol Chem 279:45155–45161
Klebig ML, Wilkinson JE, Geisler JG, Woychik RP (1995) Ectopic expression of the agouti gene in transgenic mice causes obesity, features of type II diabetes, and yellow fur. Proc Natl Acad Sci USA 92:4728–4732
Albarado DC, McClaine J, Stephens JM et al (2004) Impaired coordination of nutrient intake and substrate oxidation in melanocortin-4 receptor knockout mice. Endocrinology 145:243–252
An J, Muoio DM, Shiota M et al (2004) Hepatic expression of malonyl-CoA decarboxylase reverses muscle, liver and whole-animal insulin resistance. Nat Med 10:268–274
Millington DS, Kodo N, Norwood DL, Roe CR (1990) Tandem mass spectrometry: a new method for acylcarnitine profiling with potential for neonatal screening for inborn errors of metabolism. J Inherit Metab Dis 13:321–324
Lowry OH, Passonneau JV (1972) A flexible system of enzymatic analysis. Academic, New York
Laurell S, Tibbling G (1966) An enzymatic fluorometric micromethod for the determination of glycerol. Clin Chim Acta 13:317–322
Uziel G, Garavaglia B, Di Donato S (1988) Carnitine stimulation of pyruvate dehydrogenase complex (PDHC) in isolated human skeletal muscle mitochondria. Muscle Nerve 11:720–724
Boden G, Shulman GI (2002) Free fatty acids in obesity and type 2 diabetes: defining their role in the development of insulin resistance and beta-cell dysfunction. Eur J Clin Investig 32(Suppl 3):14–23
McGarry JD (2002) Banting lecture 2001: dysregulation of fatty acid metabolism in the etiology of type 2 diabetes. Diabetes 51:7–18
Shulman GI (2000) Cellular mechanisms of insulin resistance. J Clin Invest 106:171–176
Unger RH (2002) Lipotoxic diseases. Annu Rev Med 53:319–336
Kelley DE, Mandarino LJ (2000) Fuel selection in human skeletal muscle in insulin resistance: a reexamination. Diabetes 49:677–683
Schmitz-Peiffer C (2002) Protein kinase C and lipid-induced insulin resistance in skeletal muscle. Ann N Y Acad Sci 967:146–157
Kishimoto A, Takai Y, Mori T, Kikkawa U, Nishizuka Y (1980) Activation of calcium and phospholipid-dependent protein kinase by diacylglycerol, its possible relation to phosphatidylinositol turnover. J Biol Chem 255:2273–2276
Nishizuka Y (1984) Turnover of inositol phospholipids and signal transduction. Science 225:1365–1370
Ishizuka T, Cooper DR, Hernandez H, Buckley D, Standaert M, Farese RV (1990) Effects of insulin on diacylglycerol-protein kinase C signaling in rat diaphragm and soleus muscles and relationship to glucose transport. Diabetes 39:181–190
Kawakami T, Kawakami Y, Kitaura J (2002) Protein kinase C beta (PKC beta): normal functions and diseases. J Biochem (Tokyo) 132:677–682
Chavez JA, Knotts TA, Wang LP et al (2003) A role for ceramide, but not diacylglycerol, in the antagonism of insulin signal transduction by saturated fatty acids. J Biol Chem 278:10297–10303
Long SD, Pekala PH (1996) Lipid mediators of insulin resistance: ceramide signalling down-regulates GLUT4 gene transcription in 3T3-L1 adipocytes. Biochem J 319:179–184
Randle PJ, Newsholme EA, Garland PB (1964) Regulation of glucose uptake by muscle. 8. Effects of fatty acids, ketone bodies and pyruvate, and of alloxan-diabetes and starvation, on the uptake and metabolic fate of glucose in rat heart and diaphragm muscles. Biochem J 93:652–665
Lysiak W, Lilly K, DiLisa F, Toth PP, Bieber LL (1988) Quantitation of the effect of l-carnitine on the levels of acid-soluble short-chain acyl-CoA and CoASH in rat heart and liver mitochondria. J Biol Chem 263:1151–1156
Ramsay RR, Zammit VA (2004) Carnitine acyltransferases and their influence on CoA pools in health and disease. Mol Aspects Med 25:475–493
Koves TR, Li P, An J et al (2005) Peroxisome proliferator-activated receptor-gamma co-activator 1alpha-mediated metabolic remodeling of skeletal myocytes mimics exercise training and reverses lipid-induced mitochondrial inefficiency. J Biol Chem 280:33588–33598
Moder M, Kiessling A, Loster H, Bruggemann L (2003) The pattern of urinary acylcarnitines determined by electrospray mass spectrometry: a new tool in the diagnosis of diabetes mellitus. Anal Bioanal Chem 375:200–210
Acknowledgements
The authors thank J. Daily for his critical reading of the manuscript. We also thank the Pennington Biomedical Research Center Function Foods Division Pilot Study Program for financial support. This work was partially supported by a Clinical Nutrition Research Unit Center Grant no. 1P30 DK072476 entitled Nutritional Programming: Environmental and Molecular Interactions, sponsored by National Institute of Diabetes and Digestive and Kidney Diseases.
Duality of interest
The authors declare that they have no duality of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Power, R.A., Hulver, M.W., Zhang, J.Y. et al. Carnitine revisited: potential use as adjunctive treatment in diabetes. Diabetologia 50, 824–832 (2007). https://doi.org/10.1007/s00125-007-0605-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-007-0605-4