Abstract
Diet is an important environmental factor interacting with our genes to modulate the likelihood of developing lipid disorders and, consequently, cardiovascular disease risk. Our objective was to study whether dietary intake modulates the association between APOA5 gene variation and body weight in a large population-based study. Specifically, we have examined the interaction between the APOA5–1131T>C and 56C>G (S19W) polymorphisms and the macronutrient intake (total fat, carbohydrate, and protein) in their relation to the body mass index (BMI) and obesity risk in 1,073 men and 1,207 women participating in the Framingham Offspring Study. We found a consistent and statistically significant interaction between the −1131T>C single-nucleotide polymorphism (SNP; but not the 56C>G) and total fat intake for BMI. This interaction was dose-dependent, and no statistically significant heterogeneity by gender was detected. In subjects homozygous for the −1131T major allele, BMI increased as total fat intake increased. Conversely, this increase was not present in carriers of the −1131C minor allele. Accordingly, we found significant interactions in determining obesity and overweight risks. APOA5–1131C minor allele carriers had a lower obesity risk (OR, 0.61, 95%; CI, 0.39–0.98; P = 0.032) and overweight risk (OR, 0.63, 95%; CI, 0.41–0.96; P = 0.031) compared with TT subjects in the high fat intake group (≥30% of energy ) but not when fat intake was low (OR, 1.16, 95%; CI, 0.77–1.74; P = 0.47 and OR = 1.15, 95%; CI, 0.77–1.71; P = 0.48) for obesity and overweight, respectively). When specific fatty acid groups were analyzed, monounsaturated fatty acids showed the highest statistical significance for these interactions. In conclusion, the APOA5–1131T>C SNP, which is present in approximately 13% of this population, modulates the effect of fat intake on BMI and obesity risk in both men and women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Genetic variability has been reported for all the identified candidate lipid-related genes; however, associations between many of these variants and lipid profiles have been highly controversial [1–4]. One of the most accepted arguments to explain the lack of replication among studies has been the existence of gene–environment interactions [5–7]. Overall, gene–environment interaction refers to the differential phenotypic effects of diverse environments on individuals with the same genotype or to the discrepant effects of the same environment on individuals with different genotypes [5–8]. The investigation of gene–environment interactions will assist in increasing replication among studies and, consequently, in facilitating cardiovascular disease prevention. Nutrition is part of every individual from conception to death. Therefore, it is considered one of the most important environmental factors interacting with our genes to increase or decrease the likelihood of developing lipid disorders and further cardiovascular risk [9–11]. Currently, there is an increasing number of published studies reporting gene–diet interactions in relation to lipid metabolism [12]. Among dietary factors, total fat, specific fatty acids, alcohol, carbohydrate, and total energy intake have been the most studied [13–17]. On the other hand and directly related to nutrition, obesity has been another factor widely reported to modulate genetic effects on lipid metabolism and cardiovascular risk [18–20].
In this regard, the apolipoprotein A5 (APOA5) gene is a good example of recently reported gene–diet and gene–obesity interactions [21, 22]. In the Framingham Heart Study, we have reported a gene–diet interaction between the APOA5 gene variation and the polyunsaturated fatty acids (PUFA) in relation to plasma lipid concentrations and lipoprotein particle size [21]. Furthermore, we have demonstrated that obesity modulates the effect of the APOA5 gene variation in carotid intimal medial thickness (IMT), a surrogate measure of atherosclerosis burden. This association remained significant even after the adjustment for triglycerides [22]. The APOA5 gene variation has been associated with increased triglyceride concentrations [23–27]. Five common APOA5 single-nucleotide polymorphisms (SNPs) have been reported in several populations: −1131T>C, −3A>G, 56C>G IVS3+476G>A, and 1259T>C [24–27]. With the exception of the 56C>G SNP, the SNPs are reported to be in significant linkage disequilibrium [25–28]. Moreover, the −1131T>C and the 56C>G (S19W) are considered tag SNPs, representing three APOA5 haplotypes. The precise mechanism by which APOA5 influences plasma triglycerides and related measures remains to be determined [29]. However, the activation of lipoprotein lipase has been suggested as one of the potential APOA5 hypotriglyceridemic mechanisms [30]. Lipoprotein lipase has also been implicated in the development of obesity [31, 32] and so are some of the APOA5 gene regulators (i.e., peroxisome proliferator-activated receptors, PPARs; insulin, and thyroid hormones [33, 34]). Therefore, our objective was to study whether dietary intake modulates the association between the APOA5 gene variation (examined using the two tag SNPs, −1131T>C and 56C>G) and body mass index (BMI) and obesity in a large population-based study, the Framingham Heart Study.
Materials and methods
Subjects and study design
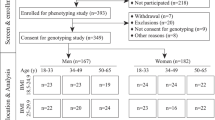
The study sample consisted of 2,280 subjects who participated in the Framingham Offspring Study (FOS) [35]. Anthropometric, clinical, and biochemical variables, as well as dietary intake and other lifestyle variables, were recorded for subjects who participated in the fifth examination visit conducted between 1992 and 1995 (n = 3515). DNA was obtained during 1987–1991. The Institutional Review Board for Human Research at Boston University and Tufts University/New England Medical Center approved the protocol of the study reported in this paper. All participants provided written informed consent. Only subjects with phenotypic data and complete dietary information for whom APOA5 gene variants were examined were included in this study. In addition, subjects with any missing data regarding control variables (age, BMI, tobacco smoking, alcohol consumption, and diabetes status) were excluded from our analyses. Thus, the data for 1,073 men and 1,207 women who met the above criteria were analyzed. Because nearly all subjects were non-Hispanic whites, no control for ethnicity was needed. Although in the Framingham Study recruitment of families was planned [35], in this specific sample, most participants were unrelated, and the number of individuals within each family included in the present study was very low. Thus, participants were distributed in 1,483 pedigrees, of which 83% were singletons. In the non-singletons, most participants were siblings and cousins. Alcohol consumption was estimated based on the reported alcoholic beverages consumed in the previous year for each of the individual, and the subjects were classified as non-drinkers (those who did not report consumption of alcohol) and drinkers [15]. Smokers were defined as those who smoked at least one cigarette per day. Physical activity was assessed as a weighted sum of the proportion of a typical day spent sleeping and performing sedentary, slight, moderate, or heavy physical activities. The subjects were classified as having type 2 diabetes if they were on hypoglycemic drug therapy for diagnosed type 2 diabetes at any study examination, or if they had fasting plasma glucose levels of at least 7.0 mmol/l at two or more exams [36].
Anthropometric and biochemical determinations
Height and weight were measured with the individual dressed in an examining gown and wearing no shoes [19]. The BMI was calculated as weight in kilograms divided by the square of height in meters. Obesity was defined as the BMI at ≥ 30 kg/m2, and overweight as the BMI at ≥ 25 kg/m2. According to these international criteria, there were 550 obese (288 men and 262 women) and 1,507 overweight (854 men and 653 women) subjects in our study population. Fasting glucose, plasma lipids, and lipoproteins were measured as previously described [16, 26, 36].
Dietary information
Dietary intake was estimated with a semiquantitative food frequency questionnaire described and validated by Rimm et al. [37]. The mean daily intake of nutrients was calculated by multiplying the frequency of consumption of each item by its nutrient content per serving and totaling the nutrient intake for all food items. The Harvard University food composition database derived from the US Department of Agriculture sources and supplemented with manufacturer information was used to calculate the nutrients and total energy intake. Intakes of carbohydrate, protein, total fat, saturated fatty acids (SFA), monounsaturated fatty acids (MUFA), and total PUFA were calculated for each individual. These measures were included in the analyses as both continuous and categorical variables.
Genetic analyses
DNA was isolated from blood samples using DNA Blood Midi Kits (Qiagen, Hilden, Germany). The −1131T>C and the 56C>G SNPs at the APOA5 locus were determined using the ABI Prism SNapShot multiplex system (Applied Biosystems, Foster City, CA, USA). The primers and probes used for genotyping were described previously [25].
Statistical analyses
We examined all continuous variables for normality of distribution. Triglyceride concentrations were log transformed. Pearson χ 2 and Fisher tests were used to test differences between observed and expected genotype frequencies, assuming Hardy–Weinberg equilibrium, and to test differences in percentages. The pair-wise linkage disequilibria (LDs) between SNPs at the APOA5 locus were estimated with the coefficient R 2 with the HelixTree program. Due to the low frequency of the variant alleles, carriers and non-carriers of the minor allele for each polymorphism were grouped and compared with wild-type homozygotes. T tests were applied to compare crude means. The relationships between the APOA5 genotype, dietary macronutrient intake, and BMI were evaluated by the analysis of covariance techniques, and the adjusted means were estimated. In these analyses, we used several different models to test the consistency of results and to adjust for potential confounders. Dietary macronutrient intakes were included in the analyses as both continuous and categorical variables. To construct the categorical variables, the intakes were classified into two groups divided by the mean value of the population. The interactions between the dietary macronutrients (as categorical or as continuous variables) and the APOA5 polymorphisms were tested in a hierarchical multivariate interaction model after controlling for potential confounders, including sex, age, smoking, alcohol consumption, total energy intake, and diabetes status. Additional control for the other macronutrients and for plasma triglyceride concentrations was carried out. Because the present study involved some correlated data that were due to familial relationships (siblings and cousins), we also controlled for familial relationships. We used two approaches to accomplish these analyses. First, a generalized linear mixed model approach that assumed an exchangeable correlation structure among all members of a family (Proc mixed in SAS, Cary, NC, USA), was used. Second, because this approach could not accurately represent the true correlation structure within these pedigrees, we used a measured genotype approach as implemented in SOLAR, a variance component analysis computer package for quantitative traits measured in pedigrees of arbitrary size. After having checked that the results obtained using the generalized mixed model were similar to those of the SOLAR approach because of the large number of unrelated subjects in this sample, we decided to present the data obtained with the generalized mixed model for the adjustment of familial relationships. Statistical analyses were performed for the whole sample and for men and women separately to evaluate the homogeneity of the effect. Standard regression diagnostic procedures, including multicollinearity tests, homogeneity of variance tests and normal plots of the residuals, were used to ensure the appropriateness of these models. When total fat intake was considered as a continuous variable, its interaction with the corresponding APOA5 polymorphism was depicted by computing the predicted values for each individual from the adjusted regression model and plotting these values against fat intake by the APOA5 genotype.
For a dichotomous outcome, obesity was defined as BMI ≥ 30 kg/m2 and overweight BMI ≥ 25 kg/m2. The logistic regression models were fitted to estimate the odds ratio (OR) and 95% confidence interval (CI) of obesity and overweight associated with the presence of each genetic variant as compared with the wild-type. Logistic regression applies maximum likelihood estimation after transforming the dependent into a logit variable (the natural log of the odds of the dependent occurring or not). In this way, logistic regression estimates the probability of a certain event occurring. Logistic regression models were also fitted to control for the effect of covariates (gender, age, tobacco smoking, alcohol consumption, diabetes, total energy intake, protein, carbohydrate, plasma triglycerides) and familial relationships and to test the statistical significance of the corresponding gene–diet interaction terms. Statistical analyses were carried out using SAS software. All reported probability tests were two-sided.
Results
Table 1 displays the demographic, anthropometric, clinical, biochemical, lifestyle, and genetic characteristics of the studied population. Genotype frequencies did not deviate from the Hardy–Weinberg equilibrium expectations. Pair-wise LD coefficient R between the −1131T>C and 56C>G SNPs was 0.063, indicating the haplotypic independence of both markers. Neither the −1131T>C nor the 56C>G SNPs were statistically associated with BMI in crude analyses (P = 0.73; P = 0.58, respectively) or after the control for potential confounders. Then, we examined if the macronutrient intake modulates the association between these polymorphisms and BMI in the whole population. As a first approach, we examined the effect of macronutrients as categorical variables. The total fat, carbohydrate, and protein intakes were classified into two groups according to the mean value of the population (30, 50, and 15%, respectively). We found a gene–diet interaction between the −1131T>C polymorphism and fat intake in relation to the BMI (P = 0.001) that remained statistically significant after controlling for sex, age, alcohol consumption, tobacco smoking, physical activity, diabetes status, total energy, protein, and carbohydrate intake (P = 0.018) and after the additional adjustment of this multivariate model for familial relationships (0.047). Further adjustment for physical activity index did not modify the significance of the results for this and all the subsequent models. This interaction was not found for carbohydrate intake or for protein intake neither in the crude model nor in the multivariate model adjusted for familial relationships (P = 0.39 and P = 0.56, respectively). Table 2 shows the BMI and P values for men and women combined, depending on the amount of the macronutrient consumed in the diet and the APOA5 polymorphism. The interaction effect of the −1131T>C polymorphism with the total fat on the BMI revealed that the increase in BMI associated with a higher fat intake (≥30% of energy from fat) observed in subjects homozygotes for the −1131T major allele was not present in carriers of the −1131C minor allele at the APOA5 locus (approximately 13% of the population). This interaction was not observed for the 56C>G polymorphism (P = 0.55). Taking into account that APOA5 polymorphisms have been associated with triglycerides in several studies, an additional adjustment for plasma triglyceride concentrations was carried out. After this additional adjustment, the gene–diet interaction between the −1131T>C SNP and the total fat intake in determining the BMI remained statistically significant (P = 0.044). Moreover, there was no evidence that the effect of this interaction differed between men and women (P for heterogeneity by gender=0.477). Likewise, no heterogeneity by sex was observed when there was no interaction between the 56C>G polymorphism and total fat intake as dichotomous on BMI (P = 0.985). To explore a possible dose-response relationship in the −1131T>C–fat interaction and to avoid the problem of selection of cut-off points, total fat intake was considered as a continuous variable. As no heterogeneity of the effect by sex was observed (P for interaction with sex=0.93), subsequent analyses combined men and women and the model additionally adjusted for sex. In agreement with the data obtained using the total fat as a qualitative variable, the modification of the effect of the −1131T>C polymorphism by total fat intake appeared to be linear in determining the BMI (Fig. 1a). After the adjustment for covariates, including plasma triglyceride concentrations, a statistically significant interaction (P = 0.048) between total fat intake as a continuous variable and the −1131T>C polymorphism in determining BMI was found. Thus, in subjects homozygous for the −1131T allele, BMI increased as total fat intake increased. In contrast, among carriers of the −1131C allele, the expected increase was not observed and those with higher fat intake appeared to have lower BMI. On the other hand, no significant interaction between the 56C>G polymorphism and the total fat (P = 0.57) was detected when the same regression model was fitted (Fig. 1b). In both wild type and carriers of the variant allele, the BMI increased as total fat intake increased. Furthermore, we examined the effect of specific fatty acids on the interaction between the −1131T>C polymorphism and fat in relation to BMI. When each fatty acid intake was examined separately as a dichotomous variable by population mean (10% energy for SFA, 11% for MUFA, and 6% for PUFA), although the direction of the effect was similar for each of these fatty acids, only the interaction between the −1131T>C polymorphism and the MUFA intake reached statistical significance (P = 0.024 in the multivariate model adjusted for sex, age, tobacco smoking, alcohol consumption, diabetes status, total energy, protein, carbohydrate, plasma triglycerides and familial relationships). No significant interactions between specific fatty acids and the 56C>G polymorphism on the BMI were detected. No statistically significant heterogeneity by sex was detected neither for the −1131T>C nor for the 56C>G polymorphisms. Figure 2 shows the mean BMI depending on the −1131T>C polymorphism (a) or the 56C>G polymorphism (b), and the MUFA intake in men and women. Finally, the effect of the APOA5–fat interaction on the obesity risk was examined. There were 550 obese subjects and 1,730 non-obese. As expected, and after the adjustment for sex, age, tobacco smoking, alcohol consumption, diabetes, total energy intake, protein, carbohydrate, plasma triglyceridesm, and familial relationships, we found a statistically significant interaction between the −1131T>C polymorphism and total fat intake as a dichotomous variable (less or more than 30%) in obesity risk (P = 0.049). No statistically significant interaction was found for the 56C>G polymorphism (P = 0.24) when the same logistic regression model was fitted. A stratified analysis by fat intake (Table 3) clearly provides evidence of the gene–diet interaction effect between the −1131T>C polymorphism and total fat intake in determining the risk of obesity: When the level of fat intake was low (<30% of energy), subjects with the −1131C allele had a non-significant modest increase in obesity risk. However, in subjects consuming ≥30% of energy from fat, carriers of the −1131C allele have about one third the risk of obesity (OR, 0.61, 95%; CI, 0.39–0.98; P = 0.032) compared with the −1131T homozygotes. When the specific fatty acids were analyzed, we observed a statistically significant interaction (P = 0.026) between the MUFA intake and the −1131C>T polymorphism on the obesity risk after the adjustment for sex, age, tobacco smoking, alcohol consumption, diabetes, total energy intake, protein, carbohydrate, plasma triglycerides, and familial relationships. Thus, in subjects consuming ≥11% of energy from MUFA, carriers of the −1131C allele have 38.2% lower obesity risk (OR, 0.62, 95%; CI, 0.41–0.94; P = 0.026) compared with the −1131T homozygotes. No heterogeneity of this effects by sex was observed (P for the interaction sex–genotype–fat > 0.05). Moreover, when the risk of being overweight was studied (1,507 overweight and 773 non-overweight subjects), we also obtained a significant interaction between the −1131T>C polymorphism and the total fat intake that remained statistically significant after the adjustment for sex, age, tobacco smoking, alcohol consumption, diabetes, total energy intake, protein, carbohydrate, plasma triglycerides, and familial relationships (P = 0.029). Table 3 shows the OR estimations of overweight for the −1131T>C polymorphism in the stratified analyses by total fat intake. In line with the previous results concerning obesity risk, the −1131C minor allele was associated with a 37% reduction of overweight risk (P = 0.031) in subjects consuming ≥30% of energy from fat when compared with TT homozygotes. No reduction of the overweight risk in carriers of the −1131C minor allele was found if the level of total fat intake was lower. No statistically significant interaction between total fat intake and the 56C>G polymorphism in determining the risk of overweight was found (P = 0.79). No statistical significant heterogeneity by sex in the tested interactions on overweight risk was detected.
Predicted values of BMI by the −1131T>C (a) and the C56G polymorphisms (b) depending on the total fat consumed (as continuous) in both men and women. Predicted values were calculated from the regression models containing the total fat intake, the corresponding APOA5 polymorphism, their interaction term, and the potential confounders [sex, age, tobacco smoking, alcohol consumption, diabetes status, total energy intake, carbohydrate (as dichotomous), protein (as dichotomous), plasma triglycerides, and familial relationships]. P values for the interaction terms between fat intake (as continuous) and the corresponding APOA5 polymorphism were obtained in the hierarchical multivariate interaction model containing total fat intake, the APOA5 SNP, and the additional control for the other covariates. Open symbols represent estimated values for wild-type homozygotes and solid symbols represent estimated values for the variant allele
Mean BMI in both men and women depending on the −1131T>C polymorphism (a) or the C56G polymorphism (b) at the APOA5 gene according to the level of MUFA intake (below and above the population mean, 11% of energy). Estimated means were adjusted for sex, age, tobacco smoking, alcohol consumption, diabetes status, total energy intake, carbohydrate (as dichotomous), protein (as dichotomous), plasma triglycerides, and familial relationships. P values for the interaction terms between fat intake and the corresponding polymorphism were obtained in the hierarchical multivariate interaction model containing MUFA intake as a categorical variable, the APOA5 SNP, and additional control for the other covariates. Bars indicate standard error (SE) of means
Discussion
We found a consistent gene–diet interaction between the −1131T>C polymorphism in the APOA5 gene and total fat intake in determining obesity-related measures (BMI, overweight, and obesity) in a large US population-based study. This gene–diet interaction was not observed when we examined another genetic marker within the same gene, namely the 56C>G (S19W) polymorphism. Previous reports have demonstrated that these two SNPs are not in LD and are considered two tag SNPs representing three APOA5 haplotypes [25, 26, 28]. Although both SNPs have been associated with higher plasma triglyceride concentrations in several populations [25, 27, 28, 38–40], they appear to differ in their associations with other cardiovascular risk factors [26, 41]. Moreover, in a recent report in the Framingham Heart Study [22], we have demonstrated gene–diet interactions between the APOA5 gene variation and the PUFA intake in determining plasma fasting triglycerides, remnant lipoprotein concentrations, and lipoprotein particle size that were exclusive for the −1131T>C polymorphism. Specifically, we found that higher n-6 (but not n-3) PUFA intake increased fasting triglycerides, remnant-like particle concentrations, and very low density lipoprotein size and decreased low-density lipoprotein size in APOA5 -1131C minor allele carriers, but such interactions were not observed in carriers of the variant allele for the APOA5 56C>G polymorphism, suggesting different mechanisms driving the biological effects associated with these APOA5 gene variants or haplotypes.
In this study, we found that subjects homozygous for the −1131T major allele presented the expected positive association between the fat intake and the BMI. Conversely, in subjects carrying the APOA5 −1131C minor allele (approximately 13% of this population), higher fat intakes were not associated with higher BMI. In contrast, this gene–fat interaction was not detected in carriers of the 56G minor allele. In these individuals, the BMI increased as the total fat intake increased following the same trend observed for subjects homozygous for the APOA5 56C major allele. This gene–diet interaction between total fat intake and the −1131T>C polymorphism was consistently found whether fat intake was considered as a categorical or as a continuous variable. In addition, this interaction effect was homogeneously found in both men and women adding support to its potential causal role.
Furthermore, when we considered BMI dichotomously to estimate the effect of this gene–diet interaction on obesity risk, we also found a statistically significant interaction between total fat intake and the APOA5 −1131T>C polymorphism. Considering that our data revealed that, in carriers of the −1131C minor allele, a higher fat intake was not associated with a higher BMI, we should expect a reduced obesity risk among −1131C minor allele carriers consuming a high-fat diet. Consistent with this hypothesis, we found one third the risk of obesity in subjects carrying the −1131C minor allele compared with−1131T homozygotes only in the high category of total fat intake (≥30% of energy). In the low category of total fat intake (<30% energy from fat), the −1131C allele was not associated with a lower obesity risk. These results were consistently found when risk of overweight instead obesity was considered and no heterogeneity by sex was detected.
There are no published studies focusing on reported interactions between dietary fat, the APOA5 −1131T>C SNP, and BMI or obesity to compare with our results. To our knowledge, only one related paper reporting an association between the −1131T>C polymorphism and weight loss after short-term diet [42] has been published. In this research, Aberle et al. [42] investigated how a short-term diet in a group of 606 hyperlipemic men from Hamburg affected BMI and lipid traits depending on the −1131T>C polymorphism. In their study, the investigators found no differences in BMI at baseline between TT homozygotes and carriers of the −1131C allele. However, after 3 months of energy restriction, patients with the −1131C allele lost significantly more weight (13.4%) than did TT homozygotes (0.04%; P = 0.002). Although the results of this study are not directly comparable with our results because of the different design, it is important to note that at least another study has found an interaction between the −1131T>C polymorphism and fat intake in determining body-weight changes. Aberle et al. [42] suggested that the impaired ribosomal translation efficiency linked to the −1131C allele [43] may cause a reduced lipoprotein lipase-mediated triglyceride uptake into adipocytes and a more efficient decrease in BMI in response to fat intake. In addition, Koike et al. [32] have reported that the over-expression of lipoprotein lipase significantly suppressed high-fat-diet-induced obesity and insulin resistance in transgenic Watanabe heritable hyperlipemia rabbits. Other potential mechanisms may involve a different regulation of the APOA5 gene by thyroid hormones [34] or PPARs [33], depending on the promoter allele and the fat intake. However, the design of our study cannot address the mechanisms by which dietary fat interacts with the −1131T>C polymorphism in determining the BMI, and further studies are needed.
Another interesting finding from our study came from the specific analysis of the effects of different dietary fats. We found that only MUFA provided an interaction term that was statistically significant. However, in this US population, MUFA and SFA are highly correlated [13]. Therefore, studies in other populations consuming a Mediterranean-type diet, in which such correlation is lower, are needed to confirm the specific benefit of a high-MUFA diet in carriers of the −1131T>C polymorphism. The paradoxical association between a higher MUFA consumption and a lower BMI in carriers of the C allele has been previously described for another polymorphism by Memisoglu et al. [44] in the Nurses’ Health Study. They found that the PPAR gamma proline to alanine substitution polymorphism (Pro12Ala) modifies the association between dietary fat and BMI. Thus, MUFA intake was not associated with BMI among homozygous wild-type women but was inversely associated with BMI among 12Ala variant allele-carriers (mean in lowest quintile=27.6 versus mean in highest quintile=25.5 kg/m2; P-trend=0.006; P-interaction=0.003).
Despite the general consistency regarding the association of the APOA5 variant alleles with higher triglyceride concentrations, their relation with coronary artery disease remains highly controversial. Therefore, a careful investigation of this gene–diet interaction may help to explain these contradictory results with clinical outcomes [26, 40, 41, 45–48]. Based on our findings, carriers of the −1131C allele, despite their increase in plasma triglycerides, have a lower likelihood of obesity when consuming a high-fat (specifically, high MUFA) diet as compared with subjects homozygous for the −1131T allele. This circumstance may mask the risk estimation of cardiovascular disease if this interaction is not considered. Supporting this hypothesis are our recent results in the Framingham Study [21], where we found that the association between the haplotype defined by the 56C>G polymorphism (for which no gene–fat interaction in determining obesity risk is present) was associated with higher carotid IMT compared with the wild-type haplotype, whereas the haplotypes defined by the presence of the rare allele in the −1131T>C, −3A>G, IVS+476G>A, and 1259T>C genetic variants were associated with higher carotid IMT only in obese subjects.
In summary, we have found a gene–diet interaction between the −1131T>C polymorphism (but not the 56C>G) in the APOA5 gene and total fat intake in relation to BMI, overweight, and obesity risk. The homogeneity of this interaction is detected in both men and women and follows a dose-response relationship. In comparison with wild-type subjects, the carriers of the variant C allele appear to be protected from the increase in body weight when consuming more dietary fat. When specific fatty acid families were analyzed, the MUFA were the most significantly implicated. Despite the higher consistence of our results, further studies are required to replicate these findings and to characterize the potential mechanisms involved before making nutritional recommendations.
References
Cambien F (2005) Coronary heart disease and polymorphisms in genes affecting lipid metabolism and inflammation. Curr Atheroscler Rep 7:188–195
Lai CQ, Parnell LD, Ordovas JM (2005) The APOA1/C3/A4/A5 gene cluster, lipid metabolism and cardiovascular disease risk. Curr Opin Lipidol 16:153–166
Pajukanta P (2004) Do DNA sequence variants in ABCA1 contribute to HDL cholesterol levels in the general population? J Clin Invest 114(9):1244–1247
Semple RK, Chatterjee VK, O’Rahilly S (2006) PPAR gamma and human metabolic disease. J Clin Invest 116:581–589
Yang Q, Khoury MJ (1997) Evolving methods in genetic epidemiology. III. Gene–environment interaction in epidemiologic research. Epidemiol Rev 19:33–43
Khoury MJ, Davis R, Gwinn M, Lindegren ML, Yoon P (2005) Do we need genomic research for the prevention of common diseases with environmental causes? Am J Epidemiol 161:799–805
Hunter DJ (2005) Gene-environment interactions in human diseases. Nat Rev Genet 6:287–298
Grigorenko EL (2005)The inherent complexities of gene-environment interactions. J Gerontol B Psychol Sci Soc Sci 60:53–64
Ordovas JM, Corella D (2004) Nutritional genomics. Annu Rev Genomics Hum Genet 5:71–118
Mutch DM, Wahli W, Williamson G (2005) Nutrigenomics and nutrigenetics: the emerging faces of nutrition. FASEB J 19:1602–1616
Afman L, Muller M (2006) Nutrigenomics: from molecular nutrition to prevention of disease. J Am Diet Assoc 106:569–576
Corella D, Ordovas JM (2005) Single nucleotide polymorphisms that influence lipid metabolism: interaction with dietary factors. Annu Rev Nutr 25:341–390
Ordovas JM, Corella D, Demissie S, Cupples LA, Couture P, Coltell O, Wilson PW, Schaefer EJ, Tucker KL (2002) Dietary fat intake determines the effect of a common polymorphism in the hepatic lipase gene promoter on high-density lipoprotein metabolism: evidence of a strong dose effect in this gene-nutrient interaction in the Framingham Study. Circulation 106:2315–2321
Dwyer JH, Allayee H, Dwyer KM, Fan J, Wu H, Mar R, Lusis AJ, Mehrabian M (2004) Arachidonate 5-lipoxygenase promoter genotype, dietary arachidonic acid, and atherosclerosis. N Engl J Med 350:29–37
Corella D, Tucker K, Lahoz C, Coltell O, Cupples LA, Wilson PW, Schaefer EJ, Ordovas JM (2001) Alcohol drinking determines the effect of the APOE locus on LDL-cholesterol concentrations in men: the Framingham Offspring Study. Am J Clin Nutr 73:736–745
Memisoglu A, Hu FB, Hankinson SE, Manson JE, De Vivo I, Willett WC, Hunter DJ (2003) Interaction between a peroxisome proliferator-activated receptor gamma gene polymorphism and dietary fat intake in relation to body mass. Hum Mol Genet 12:2923–2929
Miyaki K, Sutani S, Kikuchi H, Takei I, Murata M, Watanabe K, Omae K (2005) Increased risk of obesity resulting from the interaction between high energy intake and the Trp64Arg polymorphism of the beta3-adrenergic receptor gene in healthy Japanese men. J Epidemiol 15:203–210
Marques-Vidal P, Bongard V, Ruidavets JB, Fauvel J, Hanaire-Broutin H, Perret B, Ferrieres J (2003) Obesity and alcohol modulate the effect of apolipoprotein E polymorphism on lipids and insulin. Obes Res 11:1200–1206
Elosua R, Demissie S, Cupples LA, Meigs JB, Wilson PW, Schaefer EJ, Corella D, Ordovas JM (2003) Obesity modulates the association among APOE genotype, insulin, and glucose in men. Obes Res 11:1502–1508
Corella D, Ordovas JM (2004) The metabolic syndrome: a crossroad for genotype–phenotype associations in atherosclerosis. Curr Atheroscler Rep 6:186–196
Elosua R, Ordovas JM, Cupples LA, Lai CQ, Demissie S, Fox CS, Polak JF, Wolf PA, D’Agostino RB Sr, O’donnell CJ (2006) Variants at the APOA5 locus, association with carotid atherosclerosis, and modification by obesity: the Framingham Study. J Lipid Res 47:990–996
Lai CQ, Corella D, Demissie S, Cupples LA, Adiconis X, Zhu Y, Parnell LD, Tucker KL, Ordovas JM (2006) Dietary intake of n-6 fatty acids modulates effect of apolipoprotein A5 gene on plasma fasting triglycerides, remnant lipoprotein concentrations, and lipoprotein particle size: the Framingham Heart Study. Circulation 113:2062–2070
Pennacchio LA, Olivier M, Hubacek JA, Cohen JC, Cox DR, Fruchart JC, Krauss RM, Rubin EM (2001) An apolipoprotein influencing triglycerides in humans and mice revealed by comparative sequencing. Science 294:169–173
Talmud PJ, Hawe E, Martin S, Olivier M, Miller GJ, Rubin EM, Pennacchio LA, Humphries SE (2002) Relative contribution of variation within the APOC3/A4/A5 gene cluster in determining plasma triglycerides. Hum Mol Genet 11:3039–3046
Lai CQ, Tai ES, Tan CE, Cutter J, Chew SK, Zhu YP, Adiconis X, Ordovas JM (2003) The APOA5 locus is a strong determinant of plasma triglyceride concentrations across ethnic groups in Singapore. J Lipid Res 44:2365–2373
Lai CQ, Demissie S, Cupples LA, Zhu Y, Adiconis X, Parnell LD, Corella D, Ordovas JM (2004) Influence of the APOA5 locus on plasma triglyceride, lipoprotein subclasses, and CVD risk in the Framingham Heart Study. J Lipid Res 45:2096–2105
Hodoglugil U, Tanyolac S, Williamson DW, Huang Y, Mahley RW (2006) Apolipoprotein A–V: a potential modulator of plasma triglyceride levels in Turks. J Lipid Res 47:144–153
Pennacchio LA, Olivier M, Hubacek JA, Krauss RM, Rubin EM, Cohen JC (2002) Two independent apolipoprotein A5 haplotypes influence human plasma triglyceride levels. Hum Mol Genet 11:3031–3038
Merkel M, Heeren J (2005) Give me A5 for lipoprotein hydrolysis! J Clin Invest 115:2694–2696
Merkel M, Loeffler B, Kluger M, Fabig N, Geppert G, Pennacchio LA, Laatsch A, Heeren J (2005) Apolipoprotein AV accelerates plasma hydrolysis of triglyceride-rich lipoproteins by interaction with proteoglycan-bound lipoprotein lipase. Biol Chem 280:21553–21560
Mead JR, Irvine SA, Ramji DP (2002) Lipoprotein lipase: structure, function, regulation, and role in disease. J Mol Med 80:753–769
Koike T, Liang J, Wang X, Ichikawa T, Shiomi M, Liu G, Sun H, Kitajima S, Morimoto M, Watanabe T, Yamada N, Fan J (2004) Overexpression of lipoprotein lipase in transgenic Watanabe heritable hyperlipidemic rabbits improves hyperlipidemia and obesity. J Biol Chem 279:7521–7529
Prieur X, Coste H, Rodriguez JC (2003) The human apolipoprotein AV gene is regulated by peroxisome proliferator-activated receptor-alpha and contains a novel farnesoid X-activated receptor response element. J Biol Chem 278:25468–25480
Prieur X, Huby T, Coste H, Schaap FG, Chapman MJ, Rodriguez JC (2005) Thyroid hormone regulates the hypotriglyceridemic gene APOA5. J Biol Chem 280:27533–27543
Feinleib M, Kannel WB, Garrison RJ, McNamara PM, Castelli WP (1975) The Framingham Offspring Study. Design and preliminary data. Prev Med 4:518–525
Osgood D, Corella D, Demissie S, Cupples LA, Wilson PW, Meigs JB, Schaefer EJ, Coltell O, Ordovas JM (2003) Genetic variation at the scavenger receptor class B type I gene locus determines plasma lipoprotein concentrations and particle size and interacts with type 2 diabetes: the Framingham Study. J Clin Endocrinol Metab 88:2869–2879
Rimm EB, Giovannucci EL, Stampfer MJ, Colditz GA, Litin LB, Willett WC (1992) Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. Am J Epidemiol 135:1114–1126
Henneman P, Schaap FG, Havekes LM, Rensen PC, Frants RR, van Tol A, Hattori H, Smelt AH, van Dijk KW (2006) Plasma apoAV levels are markedly elevated in severe hypertriglyceridemia and positively correlated with the APOA5 S19W polymorphism. Atherosclerosis (in press)
Klos KL, Hamon S, Clark AG, Boerwinkle E, Liu K, Sing CF (2005) APOA5 polymorphisms influence plasma triglycerides in young, healthy African Americans and whites of the CARDIA Study. J Lipid Res 46:564–571
Hubacek JA, Skodova Z, Adamkova V, Lanska V, Poledne R (2004) The influence of APOAV polymorphisms (T-1131>C and S19>W) on plasma triglyceride levels and risk of myocardial infarction. Clin Genet 65:126–130
Lee KW, Ayyobi AF, Frohlich JJ, Hill JS (2004) APOA5 gene polymorphism modulates levels of triglyceride, HDL cholesterol and FERHDL but is not a risk factor for coronary artery disease. Atherosclerosis 176:165–172
Aberle J, Evans D, Beil FU, Seedorf U (2005) A polymorphism in the apolipoprotein A5 gene is associated with weight loss after short-term diet. Clin Genet 68:152–154
Martin S, Nicaud V, Humphries SE, Talmud PJ; EARS Group (2003) Contribution of APOA5 gene variants to plasma triglyceride determination and to the response to both fat and glucose tolerance challenges. Biochim Biophys Acta 1637:217–225
Memisoglu A, Hu FB, Hankinson SE, Manson JE, De Vivo I, Willett WC, Hunter DJ (2003) Interaction between a peroxisome proliferator-activated receptor gamma gene polymorphism and dietary fat intake in relation to body mass. Hum Mol Genet 12:2923–2929
Martinelli N, Trabetti E, Bassi A, Girelli D, Friso S, Pizzolo F, Sandri M, Malerba G, Pignatti PF, Corrocher R, Olivieri O (2006) The −1131 T>C and S19W APOA5 gene polymorphisms are associated with high levels of triglycerides and apolipoprotein C-III, but not with coronary artery disease: an angiographic study. Atherosclerosis (in press)
Liu H, Zhang S, Lin J, Li H, Huang A, Xiao C, Li X, Su Z, Wang C, Nebert DW, Zhou B, Zheng K, Shi J, Li G, Huang D (2005) Association between DNA variant sites in the apolipoprotein A5 gene and coronary heart disease in Chinese. Metabolism 54:568–572
Ruiz-Narvaez EA, Yang Y, Nakanishi Y, Kirchdorfer J, Campos H (2005) APOC3/A5 haplotypes, lipid levels, and risk of myocardial infarction in the Central Valley of Costa Rica. J Lipid Res 46:2605–2613
Szalai C, Keszei M, Duba J, Prohaszka Z, Kozma GT, Csaszar A, Balogh S, Almassy Z, Fust G, Czinner A (2004) Polymorphism in the promoter region of the apolipoprotein A5 gene is associated with an increased susceptibility for coronary artery disease. Atherosclerosis 173:109–114
Acknowledgment
This study was supported by the National Heart, Lung, and Blood Institute contract N01-HC-25195 and grant HL-54776, by contracts 53-K06-5-10 and 58-1950-9-001 from the US Department of Agriculture Research Service, and by grants from the American Heart Association (0335432T) and the Spanish Ministerio de Educación y Ciencia (PR2006-0258) and the Spanish Ministeriode Sanidad (CB06/03/0035).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Corella, D., Lai, CQ., Demissie, S. et al. APOA5 gene variation modulates the effects of dietary fat intake on body mass index and obesity risk in the Framingham Heart Study. J Mol Med 85, 119–128 (2007). https://doi.org/10.1007/s00109-006-0147-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00109-006-0147-0