Abstract
Background
The rehabilitation of patients with single-sided deafness (SSD) or asymmetric hearing loss can be achieved with conventional (Bi)CROS hearing aids ((Bi)CROS-HA, (Bi)CROS), bone conduction devices (BCI) or with cochlear implants (CI). Unfortunately, only small case series have been published on the treatment outcomes in SSD patients after CI surgery and there are only a few comparative studies evaluating rehabilitation outcomes.
Objective
The aim of this study was to provide evidence of successful treatment of SSD and asymmetric hearing loss with a CI compared to the untreated, monaural hearing condition and the therapy options of BCI and (Bi)CROS in a large number of patients.
Materials and methods
In a single-centre study, 45 patients with SSD and 40 patients with asymmetric hearing loss were treated with a CI after careful evaluation for CI candidacy. Monaural speech comprehension in noise and localisation ability were examined with (Bi)CROS-HA and BCI devices (on a test rod) both preoperatively and at 12 months after CI switch-on. At the same intervals, subjective evaluation of hearing ability was conducted using the Speech, Spatial and Qualities of Hearing Scale (SSQ).
Results and discussion
This report presents the first evidence of successful binaural rehabilitation with CI in a relatively large patient cohort and the advantages over (Bi)CROS and BCI in smaller subgroups, thus confirming the indication for CI treatment. Moreover, patients with long-term acquired deafness (>10 years) show a benefit from the CI comparable to that observed in patients with shorter-term deafness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite near-normal hearing levels in one ear and the ability to understand speech in quiet conditions, people with single-sided deafness experience significant impairment in many everyday situations. This becomes especially apparent when speech signals reach the deaf ear in the presence of background noise. Impaired hearing can lead to fatigue due to the additional effort required to hear and may influence psychosocial factors such as self-esteem, self-confidence and the feeling of security [3, 31]. Moreover, the ability to localize sound is considerably limited in patients with single-sided deafness since binaural hearing is a prerequisite to spatial hearing ability [9, 14, 32].
Patients with single-sided deafness can be rehabilitated with conventional Contralateral Routing of Signals (CROS) or BiCROS hearing aids, bone conduction devices (BCI) or cochlear implants (CI).
Conventional (Bi)CROS hearing aids conduct the acoustic signals either wirelessly or via cable and BCI via bone to the inner ear of the better-hearing side. Since the deaf ear is not rehabilitated in using these therapy options, restoration of binaural hearing is not possible. Single-sided deafness (SSD) with near-normal hearing on the contralateral side is the extreme condition in asymmetric hearing loss (AHL). In the case of asymmetrical hearing loss, the better-hearing ear also has hearing loss, up to a moderate degree, and the difference between the two ears is sufficiently large to fulfill the criterion for asymmetry [7, 10].
Therapy of patients with single-sided deafness with a CI was first described in 2008 by Van de Heyning [26]. The primary intention of the authors was not, however, the rehabilitation of single-sided deafness, but to treat intractable tinnitus. The patients not only reported a reduction or even total suppression of their tinnitus, but also improved speech comprehension in background noise and improved localisation ability. As a consequence, other researchers adopted CI treatment as a therapy option for SSD patients and also reported successful outcomes [1, 2, 5, 15, 26, 27]. To date, only case series with smaller groups of patients have been published, leaving reimbursement agencies still in doubt concerning the success of this therapy option [8, 13, 18, 25]. Similarly, with limited evidence from earlier studies, treatment of patients presenting with postlingual-acquired deafness of long duration also remained in question with the consequence that duration of deafness was restricted to a maximum of 10 years and cohorts reported in studies are still small [14, 23]. With 28 SSD patients, the publication by Távora-Vieira et al. reports on the largest patient population with significant improvement in speech comprehension in background noise after CI treatment [24]. To date, very few studies report outcomes from comparison of the available treatment options in patients with single-sided deafness, and the number of subjects involved is relatively small [1, 2].
The comparative prospective study reported here represents a single-centre study of the clinical use of unilateral electrical stimulation via a CI in a large group of patients presenting with single-sided deafness and their long-term outcomes. The study also demonstrates for the first time comparison of hearing treatment options and outcomes, including BCI and (Bi)CROS hearing aids in smaller subgroups of hearing impaired patients.
Materials and methods
The prospective clinical study presented in this manuscript was conducted in compliance with the Guidelines of the Declaration of Helsinki (Washington, 2002) and ISO 14155 governing clinical investigation (“Clinical Testing of Medical Products in Humans – Good Clinical Practice”: Parts 1 and 2) and was approved by the Ethics Commission of the University of Freiburg.
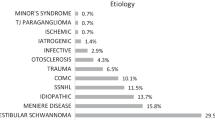
A total of 85 adult patients (age > 18 years) with single-sided, postlingual-acquired deafness, who had undergone CI surgery since 2008 in our clinic, had at least one year of experience with the CI and fulfilled the audiometric inclusion criteria, described below, were included in the assessment. In addition, subjectively inadequate hearing rehabilitation with conventional hearing aids was also an inclusion criterion. Eleven patients reported in 2011 in this journal were also included [12]. The patients were assigned to two groups with respect to pure tone audiometric hearing levels measured in the better-hearing ear. Patients with hearing loss ≤30 dB in the frequencies 125, 250, 500, 1000, 2000, 3000 and 4000 Hz (up to 4 kHz) were assigned to the group “single-sided deafness” (SSD). This SSD criterion applied to 45 patients of the collective cited above. Patients with audiometric hearing loss in the better-hearing ear of ≤60 dB to 4 kHz and >30 dB in at least one frequency up to 4 kHz were assigned to the “asymmetric hearing loss” (AHL) group. Forty patients were assigned accordingly to this group. In both subgroups, the asymmetry criterion was set at an interaural difference of ≥30 dB between the PTA4 (pure tone average: mean of air-conduction threshold at the frequencies 0.5, 1, 2 and 4 kHz) in the poorer ear and the PTA4 of the better ear. In both the SSD and the AHL groups, only patients who presented with a mean air-conduction hearing loss of more than 80 dB for the frequencies 0.1, 1, 2 and 4 kHz in the poorer ear were included. The audiometric data of the two patient groups are shown in Fig. 1 and the demographic data in Table 1. We described the preoperative diagnostic measures in detail in our article published in 2011 [2].
Prior to determining candidacy for CI surgery, an evaluation test phase was conducted with a conventional CROS (in SSD patients) or BiCROS hearing aid (in AHL patients) and a bone-conduction implant (on a Softband or test rod). The indication for bone-anchored hearing systems is recommended by the respective manufacturers for single-sided deaf patients with a maximum hearing loss of 20 dB in the better-hearing ear. According to manufacturers’ information, these systems were indicated as a therapy option only in our SSD patients. Due to repeated demands from reimbursement agencies to submit evidence with BCI testing, the same evaluation protocol was performed in the present study for all AHL patients, who consented to the additional test phase. Speech comprehension in background noise and sound localisation ability were evaluated and recorded for all patients, preoperatively monaurally (i. e. in SSD patients without hearing aid and in AHL patients with hearing aid on the better-hearing ear as available), and with the specific test device after optimization of the settings. Additionally both evaluations were performed post implant for the CI group in the CI condition 12 months after initial switch-on. The adjustments of the CI speech processors and the test devices ((Bi)CROS hearing aids and BCI audio processors) were made at our clinic using uniform procedures, independent of the audiologist, based on recommendations by the manufacturer of the hearing system. Optimisation of the settings was made based on various hearing test results obtained with the hearing systems, such as hearing threshold and speech comprehension, as well as feedback from the patients. After the initial CI switch-on, a series of 3‑day rehabilitation sessions were scheduled in our CI centre every 3 months, with appropriate technical adjustments, speech training, hearing exercises and recommendations for hearing training at home provided. AHL patients were tested 12 months after initial CI fitting in the bilateral condition with CI and the individually adjusted hearing aid in the better ear.
For audiological tests in noise, the adaptive Oldenburger Sentence Test (Satztest, OlSa) was used to determine the speech reception threshold (SRT), a fixed noise level of 65 dB SPL and a starting speech level of 65 dB SPL were applied [29, 30]. The SRT was determined in 3 presentation conditions: S0°N0°, S + 45°N − 45° and S − 45°N + 45°. Considering the patient’s better and poorer ear, these conditions were individually assigned with the presentation configurations S0N0 (speech and noise from the front), SnhNssd (speech from the hearing side/noise from the deaf side) and SssdNnh (speech from the deaf side/noise from the hearing side) [2].
Examination of localisation was made with seven loudspeakers, arranged at an angle interval of 30° in a semicircle at the height of the patient’s head. The OlSa sentences were used as stimuli for measurement of localisation ability. Each localisation test consisted of 70 sentences at sound levels of 59, 62, 65, 68 and 71 dB SPL and a mean sound level of 65 dB SPL, presented in random sequence from one of the 7 loudspeakers.
For each patient and each condition, the localisation ability was measured as the angle error in degrees, that is, as the mean angle distance between the presentation loudspeaker and the loudspeaker identified by the patient. The angle error corresponding to chance correct identification of localisation for our study set-up was 68.6° [1].
The standardized Speech, Spatial and Quality of Hearing Scale (SSQ questionnaire, Version 3.1.2) [11] was used for the subjective assessment of therapy with a CI. The questionnaire consists of three sections, in which the patient’s subjective assessments of speech comprehension, spatial hearing and quality of hearing are rated for each of the 50 questions with a score between 0 and 10. A higher score corresponds to better subjective rating of the condition in question. The subjective assessment with the SSQ questionnaire was recorded at the first preimplant appointment and 1 year after the initial CI fitting.
Individual CI use by the patient was recorded in hours/day at each fitting session.
Statistical analysis
Data analysis was made using the statistics program Gnu R Version 3.3.0 (R Foundation for Statistical Computing, Vienna, Austria). For each of the two patient groups (AHL and SSD), the various hearing/treatment conditions (preoperative untreated, preoperative with (Bi)CROS-HA, preoperative with BCI and postoperative with CI after 12 months) were compared with respect to each of the measured audiometric and subjective parameters (speech comprehension threshold in three presentation conditions, three SSQ scores) using ANOVA. Tukey’s Honest Significant Difference test was used for the post hoc analysis. The Wilcoxon sign rank test with Holm’s correction for multiple testing was applied for both patient groups for comparison of the various hearing/treatment conditions with respect to localisation ability. In both groups (SSD und AHL), the benefit obtained by CI treatment compared to the untreated condition was calculated with respect to the speech comprehension threshold in the three conditions, the localisation ability and the three SSQ scores for patients with shorter duration of deafness and for patients with longer duration of deafness. All comparisons were based on a significance level of 0.05. The package “pwr”, Version 1.1-3 by Champely et al. was used to calculate the power effect (https://github.com/heliosdrm/pwr). The assumptions made here, especially for estimation of the power effect, are based upon Cohen [6].
Results
Due to the ceiling effect in sentence scores observed when using the Hochmair–Schulz–Moser (HSM) sentence test, assessments after 2011 included the Oldenburger Sentence Test (OlSa) for testing speech comprehension in noise instead of the HSM. As a result, speech recognition data are available for only 20/45 SSD patients and 17/40 AHL patients for comparison test results for the monaural preoperative condition with the (Bi)CROS hearing aid, BCI and the 12 months post implant CI. The comparison of the monaural preoperative condition with the CI at 12 months after the initial fitting is shown for all patients. Four SSD and 11 AHL patients had been deaf for more than 10 years.
Monoaural vs. binaural speech comprehension
Comparison of monaural vs. binaural speech comprehension (SC) in noise and the localisation ability of all SSD and AHL patients.
A detectable power effect of 0.34 (AHL) and 0.32 (SSD) was calculated assuming the usual error values (α = 0.05 and β = 0.15) and the group size of 40 (AHL) and 45 (SSD). This corresponds to the estimated mean effect power using the Cohen method.
The results of speech comprehension in the OlSa and the localisation ability of the 45 SSD and 40 AHL patients in the preoperative monaural condition and after 12 months of CI experience in the 3 presentation configurations are shown in Fig. 2. Significant improvements in speech comprehension could be confirmed in both groups after 12-month experience with the CI in the configuration SssdNnh compared to the preoperative condition (SSD group: p < 0.001, AHL group: p < 0.001). For the constellation S0N0, there was significant improvement in the SSD group, but only a trend towards improvement in the AHL group (SSD group: p < 0.01; AHL group: p = 0.062). There was no difference in speech comprehension in the SSD group in the condition SnhNssd (p = 0.559), whereas the AHL group profited significantly (p < 0.05). With the CI, the patients achieved significantly better localisation ability compared to the preoperative condition 12 months after initial fitting (SSD group: p < 0.001; AHL group: p < 0.001).
Whisker box plots of speech comprehension thresholds in noise assessed with the OlSa for 3 presentation configurations in the hearing conditions monaural preoperative and post implant binaural with CI at 12 months after initial CI fitting (a SSD patients (n = 45); b AHL patients (n = 40)). c Whisker box plots of the angle error for 48 SSD and 40 AHL patients in monaural preoperative and postimplant with CI at 12 months after initial CI fitting. AHL asymmetric hearing loss; CI cochlear implant; OlSa Oldenburg sentence test; SSD single-sided deafness; S0N0 speech and noise from the front; SnhNssd speech from the hearing side/noise from the deaf side; SssdNnh speech from the deaf side/noise from the hearing side
Comparison of (Bi)CROS—BCI—CI
Comparison of monaural SC vs. SC with (Bi)CROS and BCI vs. SC with CI in noise and the localisation ability of SSD and AHL patients (17/40 AHL, 20/45 SSD).
A detectable power effect of 0.44 (AHL) or 0.40 (SSD) was calculated assuming the usual error values (α = 0.05 and β = 0.15) and the group size of 17 (AHL) and 20 (SSD). This corresponds to a high power effect using the Cohen method.
The results of speech comprehension and the localisation ability of 20 SSD and 17 AHL patients in the monaural condition and in the treated condition with the 3 various therapy options are presented in Fig. 3.
Whisker box plots of speech comprehension scores in noise assessed with the OlSa for 3 presentation configurations in the hearing conditions: monaural, with (Bi)CROS-HA or BCI and postimplant binaural with CI at 12 months after initial CI fitting (a SSD patients (n = 20); b AHL patients (n = 17)). c Whisker box plots of the angle error for 21 SSD and 17 AHL patients in the hearing conditions: monaural, with (Bi)CROS or BCI and postimplant binaural with CI at 12 months after initial CI fitting. AHL asymmetric hearing loss; CI cochlear implant; OlSa Oldenburg sentence test; SSD single-sided deafness; (Bi)CROS (bilateral) contralateral routing of signals; BCI bone conduction devices; S0N0 speech and noise from the front; SnhNssd speech from the hearing side/noise from the deaf side; SssdNnh speech from the deaf side/noise from the hearing side
SSD group
The SSD group consisted of 20 people. The binaural SC with CI in the configuration SssdNnh was significantly superior to the monaural condition and to the SC with either BCI or CROS (CI vs. monaural and CI vs. BCI: p < 0.001; CI vs. CROS: p = 0.0018). Moreover, with the CROS-HA, significantly better SRT could be demonstrated compared to the monaural condition (p = 0.004). The results with the BCI showed no significantly improved values in this condition compared to the monaural condition (p = 0.062) or in the comparison CROS vs. BCI (p = 0.755).
In the configuration S0N0, there was significant improvement in SRT with the CI compared to the monaural condition and to CROS (CI vs. monaural: p = 0.0024347 → p < 0.01 and CI vs. CROS: p = 0.0010357 → p < 0.01). No significant improvement was seen in the comparison of CI and BCI (p = 0.084) or in comparison of BCI with the monaural condition (p = 0.584).
In the easiest test configuration for single-sided deaf patients (SnhNssd), significantly better SRT was demonstrated with the CI compared to the CROS and BCI (CI vs. BCI: p = 0.0160; CI vs. CROS: p < 0.001). The SRT values did not differ significantly between the CI and monaural hearing conditions (p = 0.461). The SRT with BCI was significantly better than with CROS (p = 0.0084). In the monaural condition, there was significant improvement in SRT compared to the CROS (p < 0.001) but no significantly better SRT compared to the BCI (p = 0.389).
Localisation ability was significantly better at 12 months postimplant with the CI than in the monaural condition or with the BCI test device (CI vs. monaural p = 0.037; CI vs. BCI p = 0.029). There were no statistically significant differences between outcomes for CI and CROS-HA or the monaural and CROS or BCI conditions.
AHL group
The AHL group consisted of 17 people. In the most difficult test configuration for single-sided deaf patients (SssdNnh), binaural SC with the CI is superior to monaural SC in the AHL patients (p = 0.0033). The SRT with the BiCROS was found to be significantly better than the monaural hearing condition (p = 0.0065). The SRT in the other modalities showed no significant differences.
No significant differences in SRT could be determined among the four hearing conditions in the presentation of speech and noise from the front (S0N0).
Consistent with results for the SSD patients, the SRT with the CI in the presentation configuration SnhNssd was significantly better than that achieved in any of the other conditions: SRT (CI vs. monaural: p = 0.013, CI vs. BCI: p = 0.045, CI vs. BiCROS: p < 0.001). No significant differences were noted between SRT values in the other test conditions.
The localisation ability with the CI after 12 months was significantly better than the monaural hearing condition and in comparison with use of the BiCROS (CI vs. monaural p = 0.009, CI vs. BiCROS p = 0.039). No difference in localisation ability was demonstrable between CI and BCI, the monaural condition and BiCROS or BCI or also between BiCROS and BCI.
Benefit of CI in speech comprehension
Comparison of benefit of the CI in speech comprehension in noise and sound localisation in AHL and SSD patients with shorter and longer duration of deafness.
The benefit measured with the HSM Sentence Test in the individual loudspeaker configurations and the change in localisation ability due to CI treatment did not depend significantly on the duration of deafness in the SSD patients (SssdNnh: p = 0.0527; S0N0: p = 0.0527; SnhNssd: p = 0.742; localisation: p = 0.81). For the AHL patients, significant influence of the duration of deafness was observed only in the test condition SssdNnh (p = 0.0173). No influence of the duration of deafness was found in the other test conditions (S0N0: p = 0.1028, SnhNssd: p = 0.3712, localisation: p = 0.43).
Speech discrimination of the SSD and AHL patients in quiet.
After 12 months postimplant, the SSD group achieved Freiburger monosyllabic word discrimination scores in quiet of 48 ± 25% (mean ± standard deviation) at a presentation level of 65 dB SPL. The AHL group achieved comparable speech comprehension word scores of 41 ± 26%.
Device usage for SSD and AHL patients.
SSD patients wore the CI on average 9 h per day (min. 3–max. 19 h). Device use was comparable for the AHL patients, on average 10 h per day (min. 4–max. 18 h).
Questionnaire survey
Subjective assessment of hearing ability—Speech, Spatial and Quality of Hearing Scale (SSQ).
Repeated subjective measures via completed questionnaires filled out preoperatively, representing the monaural condition and at 12 months postimplant CI, representing the bilateral listening condition (i. e. everyday condition) were available for analysis from 36 SSD patients and 13 AHL patients. The results of the three subcategories of the SSQ questionnaires for the patient groups are shown in Fig. 4.
SSD group
The SSD group consisted of 36 people. Subjective assessment of speech comprehension with the CI postimplant showed, on average, a significantly better result than in the preoperative monaural condition (p < 0.001). The patients also rated spatial hearing ability with the CI as significantly better (p < 0.001). No significant difference was observed for subjective assessment of sound quality between the monaural and binaural hearing condition.
AHL group
The AHL group consisted of 13 people. Both speech comprehension and spatial hearing were rated by AHL patients as significantly better in the binaural hearing condition with the CI than in the preoperative monaural condition (speech comprehension: p < 0.001; spatial hearing: p < 0.001). No significant difference was observed in assessment of sound quality.
Discussion
Since the first description by Van de Heyning et al., many authors have shown that hearing performance achieved with a CI is superior to the monaural condition in patients with single-sided deafness who have undergone thorough preoperative audiological diagnostics and patient selection [1, 2, 5, 8, 13, 15, 17, 25–27]. Application of CI in patients with single-sided deafness has not been limited to patients with contralateral normal hearing (single-sided deafness, SSD). Van de Heyning et al. also described patients within their cohorts who presented with moderate deafness in the contralateral ear [26]. In such cases the asymmetry of the hearing loss configuration could be offset for speech comprehension in noise and spatial hearing by the use of a hearing aid in the contralateral ear in combination with a CI in the implanted ear [7, 26, 27].
Speech comprehension
Of relevance for the success of treatment of AHL patients is not the achievement of identical scores with the CI compared to that achieved for SSD patients, but rather the comparison of performance with the CI over monaural hearing. For this reason, we divided our study patients into two groups, SSD and AHL, even before the indication for cochlear implantation was clinically defined. For consistency across the increasing number of publications on the topic of asymmetric hearing loss, we suggested a clinical definition of SSD and AHL at the AHL Symposium in 2012 in Berlin, and later published in 2015 by Boyd [4, 28].
Given the relatively large number of patients in both the SSD and AHL groups, our results confirm significantly better speech comprehension in noise with the CI after 12 months compared to preoperative monaural hearing. This result was shown in the presentation configuration SssdNnh in both groups. In the S0N0 test configuration, the SSD group demonstrated significantly better speech comprehension and a trend for better results was observed in the AHL group. In addition, the AHL group demonstrated significant benefits from the CI in the test configuration SnhNssd. Thus, a clear advantage with the CI over no treatment can be demonstrated by these results in both groups.
The lack of change in speech comprehension in the presentation configuration SnhNssd in the SSD group is considered a positive result. It shows that when noise is presented to the CI-treated ear, it does not impair speech comprehension in the better-hearing ear. The results published by Arndt et al. [1, 2] have now been confirmed in a considerably larger number of patients. Contrary to the data published in 2011, a significant advantage can be demonstrated with the CI when both speech and noise are presented from the front. Távora-Viera et al. also report a significant improvement in speech comprehension in noise with a CI for this presentation configuration [24]. Other authors have also described the benefits of CI, especially with respect to overcoming the head shadow effect and in the S0N0 condition [1, 2, 8, 13, 14, 18, 25–27].
Localisation ability
In the present study, the localisation ability also improved 12 months after CI surgery with a reduction of the angle error of 13.5° for the AHL patients and 22.7° for the SSD patients. This corresponds to the consistent results in the literature, which show significant improvement in directional hearing with CI, but with considerably smaller patient cohorts [1, 2, 5, 7, 13, 15, 33].
Thus, in SSD patients, it appears that binaural integration of stimuli from the electrically stimulated CI ear and from the acoustically/physiologically stimulated normal-hearing ear is possible and very successful. However, evaluation of binaural integration remains difficult. The evidence for improved localisation ability in single-sided deaf patients, as well as the occurrence of the summation effect when using the CI, leads to the assumption that, in these patients, binaural processing of the peripheral stimulation response of the acoustically stimulated normal-hearing ear and the deaf ear electrically stimulated by CI takes place in the auditory brain stem.
Comparison with conventional care
The indications for cochlear implantation in single-sided deafness also include educating patients about the alternative therapy options, their advantages and disadvantages. We also tested the alternative treatment methods (conventional treatment with (Bi)CROS-HA and with BCI) to obtain the most reliable information possible with respect to the results with these treatment alternatives. The comparative results are compelling. In the SSD group, the speech comprehension results with the CI in all three presentation configurations were significantly superior to results obtained with the CROS or with BCI. No essential difference could be determined in speech comprehension in noise with the CROS-HA versus the BCI. Significantly better results with the BCI than with the CROS could only be observed in the condition SnhNssd. This result can be attributed to the applied test method. In hearing tests with the BCI, the BCI was used on a Softband, simulating transcutaneous coupling, which can yield a sound attenuation of up to 10–15 dB compared to percutaneous coupling. This reduction in transmission cannot be adequately offset by adjustments [12]. This means that noise is damped in the SnhNssd condition and, thus, speech comprehension in the better ear is less negatively influenced by the BCI.
As expected, the localisation results with the CI are significantly better compared both to the monaural condition and with the BCI. The literature contains several discussions on this topic and recognises that localisation of sounds is only possible with binaural hearing [2, 9, 14, 17–21, 24, 31, 32].
Similarly positive results can be reported for the AHL group in this study. In the configuration SnhNssd, the results of speech comprehension with the CI were significantly superior to both the BiCROS and the BCI. No outstanding advantage of either system, BiCROS or BCI, over the other was apparent. For localisation, significant advantages of the CI were found compared to the monaural condition and the BiCROS. On the other hand, no difference could be demonstrated between CI and BCI or between BCI and BiCROS. In the presentation configuration SnhNssd, speech comprehension with the (Bi)CROS-HA and BCI test device is poorer than with CI or a monaural condition since the head shadow effect is circumvented. The (Bi)CROS-HA and the BCI test device each transmit noise largely undamped (SSD) or even augmented (AHL) to the contralateral hearing ear, thus worsening the signal–noise ratio of the speech presented in noise to that ear.
Limitations
One weakness of these therapy-option comparisons is the small number of patients resulting from the switch to speech comprehension tests in noise undertaken in our clinic. Since we were able to achieve comparable results with the HSM test in our study published in 2011, it can be assumed that analogous results were achieved in using the same test for the patients in the current study [1].
In general, publications on the use of (Bi)CROS hearing aids in single-sided deaf patients report limited benefit and low acceptance due to a number of factors including social stigmatization, occlusion of the good ear and poor tone quality [16, 19, 20]. In an extensive survey article, Peters et al. report on the available comparison studies with (Bi)CROS hearing aids and BCI in single-sided deafness. In addition to very inhomogeneous results due to different study designs, no general advantage could be demonstrated for one type of device over the others. The authors also found only improved responsiveness from the deaf side associated with overcoming the head shadow, and no improvement in localisation ability due to the absence of bilateral input [20].
Duration of deafness
In our pilot study, we initially limited the indication criterion for CI treatment of single-sided deaf patients to a duration of deafness of maximum 10 years in order to show that binaural rehabilitation with the CI is possible and successful [2]. Single case reports or case series had already reported success in single-sided, long-term deaf patients [15, 23]. The publication with the largest number of long-term deaf patients (n = 5) with a duration of deafness between 27 and 40 years was published by Távora-Vieira et al. [23]. They were able to demonstrate both an objective improvement in the hearing of patients in three different speech–noise configurations and a significant subjective improvement based on the SSQ categories. In addition to intensive modified rehabilitation programs, the patient’s motivation was shown to be definitely decisive in our study.
We also investigated the influence of the duration of deafness on speech comprehension and localisation ability after CI surgery. In the SSD patients, no influence of the duration of deafness could be determined. In the AHL patients, the analysis revealed a significant influence of the duration of deafness in the presentation configuration SssdNnh. Our results show that early CI treatment of the near-deaf or deaf ear should thus be the goal, especially in patients with hearing loss on the contralateral side (AHL patients). Moreover, the present positive results should motivate professionals and the reimbursement agencies to provide a CI to patients, even those with acquired, long-term deafness, if appropriate pretherapy diagnostic outcomes are positive [15, 23].
Subjective rating
Not only are the objective audiological data important in demonstrating the success of CI treatment in single-sided deaf patients, but also a patient’s subjective rating and device usage behaviour (wear time/day). The SSQ questionnaire return rate after 12 months experience with the CI was 75% in the SSD group and 42.5% in the AHL group.
The SSD patients rated their hearing with the CI as significantly better than in the preoperative condition in the categories of speech and spatial hearing but not with respect to sound quality. Thus, we obtained results analogous to those published earlier by Vermeire et al. and Arndt et al. [1, 2, 26]. Although the rating of hearing quality with the CI did not differ from the rating at baseline, it does emphasize that acoustic hearing with the normal-hearing side and “electric” hearing with the CI is possible without negative influence upon sound quality for bilateral hearing [2]. In contrast, Távora-Vieira et al. showed a significant improvement after CI rehabilitation in all three categories, including sound quality [23].
The group of AHL patients likewise rated CI treatment as significantly better than at baseline in the categories speech and spatial hearing, but no difference was recorded for sound quality. Overall, the reported scores were lower than those of the SSD patients, both pre- and postoperatively. The improvement in quality of life after CI surgery in 20 single-sided deaf patients was recently described by Rösli et al. They used questionnaires that addressed the hearing handicap and the increase in quality of life after CI surgery [22].
CI daily use
All of the patients we have presented here use the CI daily (3–19 h), which is also proof of the success of this treatment. The indication criteria for SSD and AHL patients, the minimum requirements for hearing tests and the recommended questionnaires were defined in a recently published summary of a Round Table held during the AHL Symposium in Toulouse in 2014 [26]. It was pointed out that the success of rehabilitation or the binaural benefit can be demonstrated especially by improved localisation ability. Moreover, due to the lack of SSD-specific questionnaires, the SSQ Scale was recommended for subjective rating of CI treatment and the Health Utilities Index Mark 3 (HUI3) for rating quality of life. Recording CI wearing time is a very important criterion that describes the benefit patients receive from CI treatment.
Future
The present study is the first to verify in a considerably large number of patients, 45 SSD and 40 AHL, the subjective limitations experienced due to single-sided hearing loss, the success of binaural rehabilitation with CI treatment and, in 20 SSD and 17 AHL patients, the superiority of CI treatment over alternative therapies with (Bi)CROS hearing aids and BCI. These findings thus confirm the indications for CI intervention. Both the audiometric data and the subjective results of the questionnaires and patient’s device usage behaviour support this statement. Moreover, based on our data, it can now be demonstrated that the duration of deafness in SSD patients has no negative influence on the results after CI surgery. Patients with additional hearing loss in the better-hearing ear should receive CI treatment for the deaf ear early on in order to obtain the best possible benefit from the CI for speech comprehension.
Practical conclusions
-
Cochlear implant treatment is a possibility for rehabilitation of binaural hearing in adult patients with single-sided deafness.
-
Cochlear implant treatment is significantly superior to the alternative therapy options (CROS-/BiCROS and BCI) in speech comprehension in noise and in sound localisation.
-
In adults with acquired deafness and appropriate, supporting pretherapy diagnostics, CI treatment is indicated independent of the duration of deafness.
Literatur
Aschendorff A, Laszig R, Beck R, Schild C, Kroeger S, Ihorst G, Wesarg T (2011) Comparison of pseudobinaural hearing rehabilitation to real binaural hearing after cochlear implantation in patients with unilateral deafness and tinnitus. Otol Neurotol 32:39–47
Arndt S, Laszig R, Aschendorff A, Beck R, Schild C, Hassepass F, Ihorst G, Kroeger S, Kirchem P, Wesarg T (2011) Einseitige Taubheit und Cochleaimplantat-Versorgung – Audiologische Diagnostik und Ergebnisse. HNO 59:437–446
Borton S, Mauze E, Lieu J (2010) Quality of life in children with unilateral hearing loss: a pilot study. Am J Audiol 19:61–72
Boyd PJ (2015) Potential benefits from cochlear implantation of children with unilateral hearing loss. Cochlear Implants Int 16:121–136
Buechner A, Brendel M, Lesinski-Schiedat A, Wenzel G, Frohne-Buechner C, Jaeger B, Lenarz T (2010) Cochlear implantation in unilateral deaf subjects associated with ipsilateral tinnitus. Otol Neurotol 31:1381–1385
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2 edn. Lawrence Erlbaum, Hillsdale
Firszt JB, Holden LK, Reeder RM, Cowdrey L, King S (2012) Cochlear implantation in adults with asymmetric hearing loss. Ear Hear 33:521–533
Firszt JB, Holden LK, Reeder RM, Waltzman SB, Arndt S (2012) Auditory abilities after cochlear implantation in adults with unilateral deafness: a pilot study. Otol Neurotol 33:1339–1346
Flynn M, Sammeth C, Sadeghi A, Cire G, Halvarsson G (2010) Baha for single-sided sensorineural deafness: review and recent technological innovations. Semin Hear 31:326–349
Franko-Tobin E, Camilon PR, Camposeo E, Holcomb MA, Meyer TA (2015) Outcomes of cochlear implantation in adults with asymmetric hearing loss. Otol Neurotol 36(3):409–415
Gatehouse S, Noble W (2004) The Speech, Spatial and Qualities of Hearing Scale (SSQ). Int J Audiol 43(2):85–99
Grunder I, Seidl RO, Ernst A, Todt I (2008) Wertigkeit der BAHA-Testung für das postoperative Hörergebnis. HNO 56:1020–1024
Hansen MR, Gantz BJ, Dunn C (2013) Outcomes after cochlear implantation for patients with single-sided deafness, including those with recalcitrant Ménière’s disease. Otol Neurotol 34(9):1681–1687
Hol M, Kunst S, Snik A, Bosman A, Mylanus E, Cremers C (2010) Bone-anchored hearing aids in patients with acquired and congenital unilateral inner ear deafness (Baha CROS): clinical evaluation of 56 cases. Ann Otol Rhinol Laryngol 119:447–454
Jacob R, Stelzig Y, Nopp P, Schleich P (2011) Audiologische Ergebnisse mit Cochlear implant bei einseitiger Taubheit. HNO 59:453–460
Kenworthy OT, Klee T, Tharpe AM (1990) Speech recognition ability of children with unilateral sensorineural hearing loss as a function of amplification, speech stimuli and listening condition. Ear Hear 11:264–270
Linstrom CJ, Silverman CA, Yu GP (2009) Efficacy of the bone-anchored hearing aid for single-sided deafness. Laryngoscope 119:713–720
Nawaz S, McNeill C, Greenberg SL (2014) Improving sound localization after cochlear implantation and auditory training for the management of single-sided deafness. Otol Neurotol 35(2):271–276
Niparko JK, Cox KM, Lustig LR (2003) Comparison of the bone anchored hearing aid implantable hearing device with contralateral routing of offside signal amplification in the rehabilitation of unilateral deafness. Otol Neurotol 24(1):73–78
Peters JP, Smit AL, Stegeman I, Grolman W (2015) Review: Bone conduction devices and contralateral routing of sound systems in single-sided deafness. Laryngoscope 125(1):218–226
Pfiffner F, Caversaccio MD, Kompis M (2011) Comparisons of sound processors based on osseointegrated implants in patients with conductive or mixed hearing loss. Otol Neurotol 32:728–735
Rösli M, Hoth S, Baumann I, Praetorius M, Plinkert PK (2015) Der Einfluss der CI-Versorgung von einseitig tauben Patienten auf die Lebensqualität. HNO 63(3):182–188
Távora-Vieira D, Boisvert I, McMahon CM, Maric V, Rajan GP (2013) Successful outcomes of cochlear implantation in long-term unilateral deafness: brain plasticity? Neuroreport 24(13):724–729
Távora-Vieira D, Marino R, Krishnaswamy J, Kuthbutheen J, Rajan GP (2013) Cochlear implantation for unilateral deafness with and without tinnitus: a case series. Laryngoscope 123(5):1251–1255
Távora-Vieira D, Marino R, Acharya A, Rajan GP (2015) The impact of cochlear implantation on speech understanding, subjective hearing performance, and tinnitus perception in patients with unilateral severe to profound hearing loss. Otol Neurotol 36:430–436
Van de Heyning P, Vermeire K, Diebl M, Nopp P, Anderson I, De Ridder D (2008) Incapacitating unilateral tinnitus in single-sided deafness treated by cochlear implantation. Ann Otol Rhinol Laryngol 117:645–652
Vermeire K, Van de Heyning P (2009) Binaural hearing after cochlear implantation in subjects with unilateral sensorineural deafness and tinnitus. Audiol Neurootol 14(3):163–171
Vincent C, Arndt S, Firszt JB, Fraysse B, Kitterick PT, Papsin BC, Snik A, Van de Heyning P, Deguine O, Marx M (2015) Identification and evaluation of cochlear implant candidates with asymmetrical hearing loss. Audiol Neurootol 20(Suppl 1):87–89
Wagener K, Kuhnel K, Kollmeier B (1999) Development and evaluation of a German sentence test: I. design of the Oldenburger sentence test. Z Audiol 38:4–15
Wagener K, Brand T, Kollmeier B (1999) Development and evaluation of a German sentence test: part III. evaluation of the Oldenburg sentence test. Z Audiol 38:86–95
Wazen JJ, Spitzer JB, Ghossaini SN, Fayad JN, Niparko JK, Cox K, Brackmann DE, Soli SD (2003) Transcranial contralateral cochlear stimulation in unilateral deafness. Otolaryngol Head Neck Surg 129:248–254
Wie O, Pripp A, Tvete O (2010) Unilateral deafness in adults: effects on communication and social interaction. Ann Otol Rhinol Laryngol 119:772–781
Zeitler DM, Dorman MF, Natale SJ, Loiselle L, Yost WA, Gifford RH (2015) Sound Source Localization and Speech Understanding in Complex Listening Environments by Single-sided Deaf Listeners After Cochlear Implantation. Otol Neurotol 36(9):1467–1471
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S. Arndt received travelling expenses from Advanced Bionics, Stäfa, Switzerland; financial support for research and travelling expenses from Cochlear Ltd, Australia; financial support for research and travelling expenses from Med-El, Innsbruck, Austria and travelling expenses from Oticon, Copenhagen, Denmark.
R. Laszig received financial support for research and travelling expenses from Advanced Bionics, Stäfa, Switzerland; financial support for research, travelling expenses and consultancy fees from Cochlear Ltd, Australia; travelling expenses from Oticon, Copenhagen, Denmark; financial support for research from Med-El, Innsbruck, Austria; financial support for research and travelling expenses from ARRIAG Munich, Germany; travelling expenses from Otologics Boulder, USA; travelling expenses from Sonova Holding, Stäfa, Switzerland; financial support for research from TKIH, Freiburg, Germany; travelling expenses from the General Secretary of the German HNO Society; contract fees, consultancy fees and travelling costs from Medupdate and fees from Springer Medicine EiC.
A. Aschendorff received travelling expenses, Medical advisory board and financial support for research from Advanced Bionics, Stäfa, Switzerland; financial support for research and travelling expenses from Cochlear Ltd, Australia; financial support for research and travelling expenses from Med-El, Innsbruck, Austria; travelling expenses and financial support for research from Oticon, Copenhagen, Denmark.
F. Hassepass received travelling expenses from Advanced Bionics, Stäfa, Switzerland and Cochlear Ltd, Australia.
R. Beck received travelling expenses from Cochlear Ltd, Australia.
T. Wesarg received consultancy fees, financial support for research and travelling expenses from Advanced Bionics, Stäfa, Switzerland; consultancy fees, financial support for research and travelling expenses from Med-El, Innsbruck, Austria; financial support for research and travelling expenses from Phonak Communications, Murten, Switzerland.
This article does not contain any studies with human participants or animals performed by any of the authors.
The supplement containing this article is not sponsored by industry.
Additional information
Redaktion
W. Baumgartner, Wien
P. K. Plinkert, Heidelberg
M. Ptok, Hannover
C. Sittel, Stuttgart
N. Stasche, Kaiserslautern
B. Wollenberg, Lübeck
Rights and permissions
About this article
Cite this article
Arndt, S., Laszig, R., Aschendorff, A. et al. Cochlear implant treatment of patients with single-sided deafness or asymmetric hearing loss. HNO 65 (Suppl 2), 98–108 (2017). https://doi.org/10.1007/s00106-016-0297-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00106-016-0297-5