Abstract
Purpose
The aim of this study was to compare tracheal intubation conditions after induction of anesthesia with a bolus of propofol-sufentanil or propofol-remifentanil and a rapid induction technique.
Material and methods
A total of 70 patients (American Society of Anesthesiologists (ASA) classification I‑II) undergoing outpatient surgery under general anesthesia with intubation for tooth extraction were randomly assigned to two groups in this double-blind study. Patients received either a bolus of remifentanil (3 μg/kg) or sufentanil (0.3 μg/kg) together with 2.5 mg/kg propofol for intubation. The primary outcome was the percentage of excellent intubation conditions and the secondary outcomes were the percentage of patients with a decrease of over 20% in mean arterial pressure (MAP) or heart rate (HR), time to achieve spontaneous respiration, time between the end of surgery and extubation and time to achieve an Aldrete score of 10. VAS pain score was >3 or having laryngeal pain 15 min after arriving in the postanesthesia care unit (PACU) were also analyzed.
Results
Intubating conditions (perfect + good conditions) were significantly better with remifentanil than with sufentanil (88.5% vs. 68.6%; p = 0.01). When using remifentanil, the hemodynamic conditions were good. Using remifentanil did not significantly increase the pain score or the laryngeal pain in the recovery room. This was confirmed by no significant differences between the groups for morphine consumption. Remifentanil significantly decreased the time to achieve an Aldrete score of 10.
Conclusion
When intubation without muscle relaxants is required, intubating conditions are much better when a remifentanil bolus is used compared to a sufentanil bolus. The remifentanil/propofol rapid induction technique is a valuable technique to quickly intubate and achieve good conditions.
Zusammenfassung
Zweck
Ziel dieser Studie war es, die Bedingungen der Trachealintubation nach Narkoseeinleitung mit einem Bolus Propofol-Sufentanil oder Propofol-Remifentanil und einer schnellen Induktionstechnik zu vergleichen.
Material und Methoden
In dieser Doppelblindstudie wurden insgesamt 70 Patienten (American Society of Anesthesiologists(ASA)-Klassifikation I–II), bei denen ambulant unter Vollnarkose mit Intubation eine Operation zur Zahnextraktion durchgeführt wurde, in 2 Gruppen randomisiert. Die Patienten erhielten entweder einen Bolus Remifentanil (3 μg/kg) oder Sufentanil (0,3 μg/kg), zusammen mit 2,5 mg/kg Propofol zur Intubation. Das primäre Ergebnis war der Prozentsatz ausgezeichneter Intubationsbedingungen, und die sekundären Ergebnisse waren der prozentuale Anteil der Patienten mit einer Senkung des mittleren arteriellen Drucks (MAP) oder der Herzfrequenz (HR) um mehr als 20 %, die Zeit bis zum Erreichen der Spontanatmung, die Zeit zwischen dem Ende der Operation und der Extubation sowie die Zeit bis zum Erreichen eines Aldrete-Scores von 10. Der prozentuale Anteil der Patienten mit einem Schmerzscore >3 oder mit Kehlkopfschmerzen 15 min nach Ankunft auf der „postanesthesia care unit“ (PACU) wurde ebenfalls analysiert.
Ergebnisse
Die Intubationsbedingungen waren mit Remifentanil signifikant besser als mit Sufentanil (51,4 % vs. 20 %; p = 0,0064). Bei der Verwendung von Remifentanil waren die hämodynamischen Bedingungen gut. Die Verwendung von Remifentanil führte zu keiner signifikanten Erhöhung des Schmerzscores oder der Kehlkopfschmerzen im Aufwachraum. Dies wurde dadurch bestätigt, dass es keine signifikanten Unterschiede in den Gruppen für die Morphineinnahme gab. Remifentanil verkürzte die Zeit bis zum Erreichen eines Aldrete-Scores von 10 signifikant.
Schlussfolgerung
Wenn eine Intubation ohne Muskelrelaxanzien erforderlich ist, sind die Intubationsbedingungen bei Verwendung eines Remifentanil-Bolus wesentlich besser als bei Verwendung eines Sufentanil-Bolus. Die Methode der schnellen Induktion durch Remifentanil/Propofol ist eine wertvolle Technik, mit der eine schnelle Intubation möglich ist und gute Bedingungen erreicht werden können.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Administering a muscle relaxant to supplement the drugs given to induce general anesthesia is not mandatory but usually facilitates tracheal intubation [1]. Muscle relaxants are allergenic and may produce prolonged neuromuscular blockade, delaying the return of spontaneous ventilation and are therefore not justified for short surgical procedures [2]. Moreover, the use of neuromuscular blocking drugs in general anesthesia is associated with an increased risk of postoperative pulmonary complications [3,4,5]. When rapid surgical procedures, such as tooth extraction, are realized the use of muscle relaxants for intubation is undesirable. Recovery time is much longer than the time needed to perform the operation. Ambulatory turnover is an important factor in short procedures and is delayed when muscle relaxants are used.
Intubation where a muscle relaxant is not used entails a theoretical increased risk of lesions of the upper airways during the laryngoscopy when the intubating conditions are not good [6]. Where muscle relaxants are not used it is desirable to administer alternative induction agents to provide good intubation conditions. Intubation without a muscle relaxant is an induction technique that is frequently used (450,000 per year in France in 1996) [7]. The injection of opioids with propofol (Propofol Lipuro, B-Braun, Melsungen AG, Germany) creates good intubation conditions [8]. The use of sufentanil (Mylan Médical SAS, Paris, France) is standard but it is less effective for achieving excellent intubation conditions than a muscle relaxant [6, 9]. A bolus of 0.3 μg/kg provides excellent intubation conditions in 40% of cases [9]; however, this dose delays the return of spontaneous ventilation and patient awakening. Furthermore, the maximum effects of sufentanil are not obtained until 6 min after injection [9].
Remifentanil (Mylan Médical SAS, Paris, France) is an opioid with good potential: its maximum effects are obtained between 60 s and 90 s after injection, it has a short duration of action and its elimination is independent of liver or renal metabolism [10]. Several studies have reported that remifentanil, administered in combination with propofol where a muscle relaxant is not used, provides adequate intubation conditions, a good hemodynamic stability and early recovery [8, 11,12,13,14,15,16,17,18]. Because remifentanil achieves adequate cerebral concentration levels more rapidly than propofol, intubation and hemodynamic conditions are improved when remifentanil is injected after propofol [8, 11,12,13,14,15,16,17]. A dose of 3 μg/kg [1] provides excellent intubation conditions in 80% of cases [12, 19]; however, to our knowledge this combination has never been compared with the standard propofol-sufentanil combination used as common practice in hospitals. Thus, the aim of this study was to compare tracheal intubation conditions after a bolus injection of propofol combined with sufentanil as compared to propofol combined with remifentanil rapid induction technique in patients undergoing surgical tooth extraction.
Methods
This single center, prospective, randomized, double blind, intention-to-treat analysis, parallel group study was conducted at Toulouse University Hospital (France). All patients undergoing ambulatory surgery under general anesthesia with intubation for tooth extraction were enrolled in this study. All patients were between 18 and 60 years old, had ASA scores of 1 or 2 and were affiliated to a social security system. Exclusion criteria were: a history of chronic alcoholism or opiate use, treatment with beta-blockers or calcium channel blockers and paracetamol or ketoprofen allergies. This study was approved by the research ethics board (protocol number 09.001.03, favorable opinion of the CPP Sud-Ouest et Outre-Mer 1 dated 19 January 2011) and written informed consent was obtained from each patient. This trial was registered at ClinicalTrials.gov (NCT01910285).
The primary outcome was the comparison of the percentage of excellent intubation conditions using the Scandinavian scale. The secondary outcomes were the percentage of patients with a decrease of over 20% in MAP or HR, time to spontaneous respiration, time between the end of surgery and extubation and time to obtain an Aldrete score of 10. The percentage of patients able to get into bed unassisted, with a VAS pain score >3 or with laryngeal pain 15 min after arriving in the PACU were also analyzed. Randomization of the patients was performed by the methodologist of the study using STATA software (Stata Corp LP, College Station, TX, USA), and was centralized in the Clinical Pharmacology Service. A physician investigator opened the envelope corresponding to the patient’s inclusion number and prepared 3 syringes numbered 1, 2 and 3. The remifentanil dose was prepared in a total volume of 20 mL by adding saline 0.9%, and the sufentanil dose was prepared in a total volume of 10 mL. Both care providers and the anesthesiologist assessing the outcomes were blinded to the study groups. The patients were randomized into two groups according to the opioid to be administered in combination with propofol (2.5 mg/kg): the remifentanil group (group R: 3 μg/kg; n = 35) and the sufentanil group (group S: 0.3 μg/kg; n = 35). No premedication was administrated to any of the patients. On arrival in the operating room each patient was infused and preoxygenated for 3 min. The chronometer was activated on injection of syringe 1, which contained 0.3 μg/kg of sufentanil in the sufentanil group and 0.9% saline in the remifentanil group. After waiting 4 min, 3 mg/kg of propofol was injected in 30 s immediately followed by syringe 2, which was injected in 30 s. Syringe 2 contained 0.9% saline in the sufentanil group and 3 μg /kg of remifentanil in the remifentanil group. After waiting 30 s, mask ventilation was attempted. Laryngoscopy and nasal intubation were attempted using a Macintosh 4 laryngoscope blade and a size 6.5 (men) or a size 6 (women) endotracheal tube. A supplementary dose of propofol (1 mg/kg) could be injected; a maximum of twice if required. Patients who could not be intubated after these two supplementary doses of propofol were intubated with succinylcholine 1 mg /kg. The anesthesiologist performing the intubation assessed ease of mask ventilation, jaw relaxation and oropharyngeal resistance to laryngoscopy, Cormack score, vocal cord position, patient reaction to insertion of the tracheal tube and cuff inflation (diaphragmatic movement and coughing), traction force and the need for a Sellick maneuver. The numbers of laryngoscopies, operators and alternative techniques were also recorded. These criteria were used to score intubating conditions using the Scandinavian scale as excellent, good or poor (this is the recommended scale for the evaluation of intubating conditions) [20]. The intubation difficulty scale (IDS) was also calculated to determine the incidence of difficult intubation [21]. Once intubated, controlled ventilation was initiated with a volume of 6–8 mL /kg. Maintenance of anesthesia was provided by desflurane. Ventilation was adapted to each patient to obtain exhaled CO2 between 45 mm Hg and 50 mm Hg. Syringe 3, which contained 0.05 μg/kg of sufentanil in the remifentanil group and 0.9% saline in the sufentanil group, was injected 5 min before incision. Spontaneous ventilation was initiated as soon as possible. Postoperative analgesia was injected as soon as the induction was finished with 1 g of paracetamol and 100 mg of ketoprofen. Intraoperative analgesia was conducted using a 0.05 μg/kg bolus of sufentanil (to maintain spontaneous breathing frequency between 8 and 12 cycles/min). Heart rate (HR), mean arterial pressure (MAP), peripheral oxygen saturation (SpO2) and exhaled CO2 were recorded every 2 min. Where systolic pressure was less than 80 mm Hg, a bolus dose of 6 mg of ephedrine was injected. Where HR was lower than 40 beats/min, a bolus dose of 10 μg/kg of atropine was injected. At the end of the surgery, all anesthetic agents were discontinued and the patients were ventilated with 100% O2. The patients were extubated as soon as they opened their eyes or could answer a simple question. Patients were then transferred to the PACU where tramadol or morphine was administered as necessary. Tramadol was administered where the VAS pain score was >3 and morphine was administered if the VAS remained >3 after administration of the tramadol. The times elapsed from the injection of syringe 1 to laryngoscopy, cuff inflation, initiation of spontaneous respiration, surgical incision, end of surgery and tracheal extubation were recorded. The Aldrete’s scoring system is a commonly used scale for determining when people can be safely discharged from the PACU to the postsurgical ward. With a score of 10 the patient can safely go to the ward. Laryngeal pain, pain score and ability to get into bed unassisted were also recorded.
Data monitoring was done by the direction de la recherche Clinique (DRC) of the CHU of Toulouse. Access to data was limited only to statistician of the study.
The ideal weight was calculated using the Lorentz formula. The formula for men is as follows: Ideal weight (man) = H - 100 - ((H - 150)/4). The formula for women is as follows: Ideal weight (woman) = H - 100 - ((H - 150)/2.5).
Statistical analysis
Demographic data and scores were abstracted and described through descriptive statistical analysis. A study of the distribution of the values was carried out using a Kolmogorov-Smirnov test with parallel analyses of kurtosis and skewness. Results were expressed as the median and confidence interval CI 95% [CI95] and as mean (SD) for quantitative variables and in numbers and percentages n(%) for qualitative variables.
The study population was separated into two groups: the remifentanil group and the sufentanil group. Patient characteristics for the two groups were compared using:
Non-parametric tests (Mann-Whitney U-test) for continuous variables, because of the non-Gaussian distribution of the majority of the variables;
The χ2-test or Fisher’s exact test for qualitative variables.
The non-parametric Mann–Whitney U‑test was used was used to compare repeat HR and MAP measurement.
Sample size calculation
The hypothesis of the study was that the proportion of patients with perfect intubation conditions in the sufentanil group is 41% [9] and 83% [12, 19] in the remifentanil group. The expected difference is 42%, with an alpha risk of 5% and a beta risk of 90%, in bilateral hypothesis, the number required for the study is 35 patients per group. The total number to be included in the study is therefore 70 subjects. The study was carried out using MedCalc® statistical software version 15 (Mariakerke, Belgium). A p < 0.05 was considered statistically significant.
Results
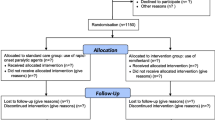
A total of 70 patients were initially included in the study but 8 of the patients had to be excluded (error in procedure, material problem). And a further 8 patients were substituted. Of the 70 patients who completed the study there were an equal number in each group (Fig. 1). There were no demographic differences between the two groups in term of age, weight, size, BMI and ASA score (Table 1). The duration of the surgery was 30 min (7) in the sufentanil groups and 29 min (8) in the remifentanil group (p = 0.74).
Using the Scandinavian scale, the percentage of patients presenting excellent intubating conditions was statistically higher in the remifentanil group (51.4%) than in the sufentanil group (20%) (p = 0.0064). Furthermore, 31.4% of patients in the sufentanil group presented with poor intubation conditions as against only 11.4% in the remifentanil group (p = 0.0133) (Fig. 2). There was no difference between the two groups in the incidence of difficult intubation according to the IDS scale.
Before induction, there were no significant differences in HR or MAP between the two groups. Figs. 3 and 4 represent the variation of MAP profile and HR for the two groups. After intubation, MAP and HR increased but without significant difference between the two groups. Using remifentanil for induction did not significantly increase the pain score or laryngeal pain in the PACU. This is confirmed by the fact that morphine consumption did not differ significantly between the two groups (Table 2). Injecting remifentanil as opposed to sufentanil did not reduce the time to obtain spontaneous respiration or the time between the end of the surgery and extubation but it significantly decreased the time to obtain an Aldrete score of 10 (Table 2). The percentage of patients able to get into bed unassisted was comparable between the two groups. It was also noticed that there were more reactions to the insertion of the tracheal tube and cuff inflation in the sufentanil group than in the remifentanil group, since there was significantly more propofol reinjection in the sufentanil group (48.8% vs. 19.4%, p = 0.013).
Change in mean arterial pressure (MAP) in the 2 groups. The values recorded at T0 are the preinduction ones. Propofol was injected at T4 and T6 represents the values recorded after the injection of remifentanil (or saline serum for the sufentanil group). Intubation was realized between T6 and T8. Mean arterial pressure and heart rate decreased in the two groups after induction. Asterisk statistically significantly different when comparing the remifentanil and the sufentanil groups
Change in heart rate in groups. The values recorded at T0 are the preinduction ones. Propofol was injected at T4 and T6 represents the values recorded after the injection of remifentanil (or saline serum for the sufentanil group). Intubation was realized between T6 and T8. Mean arterial pressure and heart rate decreased in the two groups after induction. Asterisk statistically significantly different when comparing the remifentanil and the sufentanil groups
Discussion
This study showed that a 3 μg/kg IV bolus dose of remifentanil in combination with 3 mg/kg of propofol, provided excellent intubating conditions according to the Scandinavian scale in 51.4% of patients as against only 20% in the sufentanil group. To our knowledge, this is the first study to compare intubation conditions between sufentanil and remifentanil. Intubation conditions were studied using the Scandinavian scale as the reference scale [20]. For greater reliability, we studied excellent intubating conditions only. But if take into account the intubating conditions (perfect + good conditions) the results were also significantly better with remifentanil than with sufentanil (88.5% vs. 68.6%; p = 0.01). There are many variations in the protocols studied in the literature (inhomogeneous distribution of doses, speed of administration of agents, injection duration and time elapsed between injection and intubation), which, together with age and gender differences between groups and the use of different assessment scales for assessing intubating conditions, may account for the differences observed between studies. In many studies, remifentanil was administered before propofol, whereas in this study the drug was administered as a rapid bolus after the induction agent as recommended [14]. Remifentanil and propofol doses vary in the studies. In each case a lower dose of remifentanil was compensated by a higher dose of propofol and vice versa. A minimum dose of remifentanil (3 μg/kg) seems to be mandatory for successful intubation [8, 12, 19]. In this study, intubation conditions using sufentanil were studied 6 min after its injection (to allow correlation between the onset of action of sufentanil and the laryngoscopy). This 6 min delay is hard to respect during daily sequence induction and creates an increased risk of difficult intubation. The use of remifentanil as a strategy of anesthesia for short procedures where a rapid ambulatory turnover is needed is therefore particularly appropriate. Moreover, the Aldrete recovery score was found to be significantly higher than when remifentanil was used, as previously described [16]. This result is highly relevant because it shows that induction with remifentanil allows faster output in the PACU and helps to improve outpatient turnover.
Several studies showed that induction with remifentanil without muscle relaxants provided intubation conditions approaching that provided by succinylcholine and also that remifentanil was superior to succinylcholine with respect to hemodynamic stability and recovery duration [15,16,17]. In the present study, the patients who were given remifentanil had a good hemodynamic tolerance. Induction using a propofol/remifentanil combination avoids the increase of intraocular pressure and controls the hemodynamic stress response to laryngoscopy and intubation, in contrast to when a succinylcholine/propofol combination is used [15]. According to these results and taking into account the side effects of succinylcholine, rapid sequence induction with remifentanil in place of succinylcholine in ASA 1 or 2 patients presenting an allergic risk, not suffering from shock or those suffering from hyperintraocular pressure could be appropriate but furthers studies are needed.
When intubating without using a muscle relaxant, the most effective drug combinations are those that include either alfentanil or remifentanil as the opioid [11, 22, 23]; however, high doses of alfentanil are necessary. An initial bolus of 40 μg/kg seems to provide the best intubating conditions [23]. Where the dosage is below this level, up to 35% of patients may have closed vocal cords during laryngoscopy [23]. The relatively large doses of alfentanil recommended to facilitate tracheal intubation without a muscle relaxant has a clinical duration of action that may be inappropriate for many procedures in ambulatory surgery [24, 25]. Moreover, alfentanil may cause muscle rigidity and in particular cardiovascular depression in high doses [25]. Remifentanil is 20–30 times more potent than alfentanil and its elimination half-time is 3.8–8.3 min. Compared to alfentanil, remifentanil’s effect is reduced much more quickly after intubation, which is an important advantage over alfentanil, especially in short procedures and ambulatory surgery. The use of fentanyl for intubating without muscle relaxants leads to good intubation scores in only 17% of patients [24].
Hemodynamic tolerance was similar and acceptable in both groups of this study. The MAP values decreased significantly by more than 20% after induction in the remifentanil group but never dropped below 67 mm Hg. There was no significant increase in the requirement for ephedrine administration across the two groups and HR never dropped below 20% in either group. Several studies reported similar acceptable decreases in MAP or HR (using a value of 30%) when using remifentanil and propofol [8, 12, 14, 15, 19]. Hanna et al. showed that induction with 4 μg/kg of remifentanil injected after 2 mg/kg of propofol caused a significant change in HR [15]. This dose of remifentanil is higher than the one used in the present study.
With respect to laryngeal pain after intubation, remifentanil seems to be relatively safe. Only 46.4% of the patients intubated with remifentanil in this study had laryngeal pain after intubation against 43% of the patients intubated with rocuronium [6]. This is in contrast to 53.6% suffering from laryngeal pain in the sufentanil group and 57% in the alfentanil group of Combes et al. [6].
The limitations of this study are that the results are only applicable to ASA 1 and 2 patients aged from 18 to 60 years. Indeed, hemodynamic tolerance may be different in ASA 3 or 4 patients, particularly those suffering from severe heart disease. Hemodynamic tolerance may be also different in old patients or patients suffering hypovolemia. Authors found that combined with 1 mg/kg propofol, 1.39 μg/kg of remifentanil resulted in acceptable intubating conditions within 60 s in 95% of old patients [26]. The MAP and HR decreased significantly after propofol and remifentanil administration but were within 30% of baseline values [26].
In conclusion, intubation conditions are significantly better when remifentanil is used in comparison with sufentanil where muscle relaxants are not used: excellent intubation conditions in 51.4% of cases using remifentanil as opposed to 20% for sufentanil. The hemodynamic conditions were acceptable since MAP remained above 67 mm Hg and there was no statistical diminution of HR. The pain score was not modified and laryngeal pain was comparable to that described where muscle relaxants are used. Finally, the time elapsed in the PACU was decreased, which can facilitate ambulatory turnover. Therefore, the use of remifentanil for ASA 1 and 2 patients aged between 18 and 60 years is highly recommend when it is necessary to intubate without muscle relaxants. The remifentanil/propofol rapid induction technique is a valuable technique to intubate quickly and in good conditions.
Abbreviations
- ASA:
-
American Society of Anesthesiologists
- BMI:
-
Body mass index
- HR:
-
Heart rate
- IDS:
-
Intubation difficulty scale
- IV:
-
Intravenous
- MAP:
-
Mean arterial pressure
- PACU:
-
Post anesthesia care unit
- SpO2 :
-
Oxygen saturation
- VAS:
-
Visual analog scale
References
Baillard C, Adnet F, Borron SW et al (2005) Tracheal intubation in routine practice with and without muscular relaxation: an observational study. Eur J Anaesthesiol 22:672–677
Heerdt PM, Sunaga H, Savarese JJ (2015) Novel neuromuscular blocking drugs and antagonists. Curr Opin Anaesthesiol 28:403–410
Bulka CM, Terekhov MA, Martin BJ, Dmochowski RR, Hayes RM, Ehrenfeld JM (2016) Nondepolarizing neuromuscular blocking agents, reversal, and risk of postoperative pneumonia. Anesthesiology 125:647–655
Grosse-Sundrup M, Henneman JP, Sandberg WS et al (2012) Intermediate acting non-depolarizing neuromuscular blocking agents and risk of postoperative respiratory complications: prospective propensity score matched cohort study. BMJ 345:e6329
Kirmeier E, Eriksson LI, Lewald H et al (2019) Post-anaesthesia pulmonary complications after use of muscle relaxants (POPULAR): a multicentre, prospective observational study. Lancet Respir Med 7(2):129–140. https://doi.org/10.1016/S2213-2600(18)30294-7
Combes X, Andriamifidy L, Dufresne E et al (2007) Comparison of two induction regimens using or not using muscle relaxant: impact on postoperative upper airway discomfort. Br J Anaesth 99:276–281
Laxenaire MC, Auroy Y, Clergue F, Péquignot F, Jougla E, Lienhart A (1998) Organization and techniques of anesthesia. Ann Fr Anesth Reanim 17:1317–1323
Alexander R, Olufolabi AJ, Booth J, El-Moalem HE, Glass PS (1999) Dosing study of remifentanil and propofol for tracheal intubation without the use of muscle relaxants. Anaesthesia 54:1037–1040
Adamus M, Koutná J, Gabrhelík T, Zapletalová J (2008) Tracheal intubation without muscle relaxant—the impact of different sufentanil doses on the quality of intubating conditions: a prospective study. Cas Lek Cesk 147:96–101
Minto CF, Schnider TW, Shafer SL (1997) Pharmacokinetics and pharmacodynamics of remifentanil. II. Model application. Anesthesiology 86:24–33
Alexander R, Booth J, Olufolabi AJ, El-Moalem HE, Glass PS (1999) Comparison of remifentanil with alfentanil or suxamethonium following propofol anaesthesia for tracheal intubation. Anaesthesia 54:1032–1036
Demirkaya M, Kelsaka E, Sarihasan B, Bek Y, Üstün E (2012) The optimal dose of remifentanil for acceptable intubating conditions during propofol induction without neuromuscular blockade. J Clin Anesth 24:392–397
Bouvet L, Stoian A, Rimmelé T, Allaouchiche B, Chassard D, Boselli E (2009) Optimal remifentanil dosage for providing excellent intubating conditions when co-administered with a single standard dose of propofol. Anaesthesia 64:719–726
Trabold F, Casetta M, Duranteau J et al (2004) Propofol and remifentanil for intubation without muscle relaxant: the effect of the order of injection. Acta Anaesthesiol Scand 48:35–39
Hanna SF, Ahmad F, Pappas ALS et al (2010) The effect of propofol/remifentanil rapid-induction technique without muscle relaxants on intraocular pressure. J Clin Anesth 22:437–442
Gulhas N, Topal S, Erdogan Kayhan G et al (2013) Remifentanil without muscle relaxants for intubation in microlaryngoscopy: a double blind randomised clinical trial. Eur Rev Med Pharmacol Sci 17:1967–1973
Naziri F, Amiri HA, Rabiee M et al (2015) Endotracheal intubation without muscle relaxants in children using remifentanil and propofol: comparative study. Saudi J Anaesth 9:409–412
Erhan E, Ugur G, Alper I, Gunusen I, Ozyar B (2003) Tracheal intubation without muscle relaxants: remifentanil or alfentanil in combination with propofol. Eur J Anaesthesiol 20:37–43
Stevens JB, Wheatley L (1998) Tracheal intubation in ambulatory surgery patients: using remifentanil and propofol without muscle relaxants. Anesth Analg 86:45–49
Fuchs-Buder T, Claudius C, Skovgaard LT et al (2007) Good clinical research practice in pharmacodynamic studies of neuromuscular blocking agents II: the Stockholm revision. Acta Anaesthesiol Scand p:789–808
Adnet F, Borron SW, Racine SX et al (1997) The intubation difficulty scale (IDS): proposal and evaluation of a new score characterizing the complexity of endotracheal intubation. Anesthesiology 87:1290–1297
Hanci V (2012) Tracheal intubation without use of muscle relaxants: comparison of remifentanil and alfentanil. Anesth Pain Med 1:210–211
Scheller MS, Zornow MH, Saidman LJ (1992) Tracheal intubation without the use of muscle relaxants: a technique using propofol and varying doses of alfentanil. Anesth Analg 75:788–793
Jabbour-Khoury SI, Dabbous AS, Rizk LB et al (2003) A combination of alfentanil-lidocaine-propofol provides better intubating conditions than fentanyl-lidocaine-propofol in the absence of muscle relaxants. Can J Anaesth 50:116–120
Klemola UM, Mennander S, Saarnivaara L (2000) Tracheal intubation without the use of muscle relaxants: remifentanil or alfentanil in combination with propofol. Acta Anaesthesiol Scand 44:465–469
Goo E‑K, Oh A‑Y, Cho S‑J, Seo K‑S, Jeon Y‑T (2012) Optimal remifentanil dosage for intubation without muscle relaxants in elderly patients. Drugs Aging 29:905–909
Acknowledgements
The authors thank Leonie Smith for the English editing of this article.
Funding
Support was provided solely from institutional and department sources. CHU Toulouse supported this work.
Author contributions
Conceived and designed the experiments: CR, VM. Performed the experiments: CR, LB, FF, AD. Wrote the paper: JMC, AD, LB, CR, VM.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Dolsan, L. Bruneteau, C. Roche, F. Ferré, F. Labaste, A. Sommet, J.-M. Conil and V. Minville declare that they have no competing interests..
Ethical standards
All procedures performed in studies involving human participants or on human tissue were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the research ethics board (protocol number 09.001.03, favorable opinion of the CPP Sud-Ouest et Outre-Mer 1) and written informed consent was obtained from each patient. This trial was registered at ClinicalTrials.gov (NCT01910285 dated July 29, 2013)
Additional information
The authors A. Dolsan and L. Bruneteau contributed equally to the manuscript.
Rights and permissions
About this article
Cite this article
Dolsan, A., Bruneteau, L., Roche, C. et al. Comparison of intubating conditions after induction with propofol and remifentanil or sufentanil. Anaesthesist 69, 262–269 (2020). https://doi.org/10.1007/s00101-020-00739-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00101-020-00739-0