Abstract
Objective
To describe the trend of acute self-poisoning in the emergency and intensive care.
Methods
Electronic charts of adults who presented to the emergency department of the University Hospital Leipzig with self-poisoning following a suicide attempt (suicide group), intoxication (intoxication group), drug overdose for relief of pain or discomfort (drug overdose group) between 2005 and 2012 were analyzed.
Results
3533 adults (62.6 % males) were identified, with the yearly admissions increasing from 305 in 2005 to 624 in 2012. The admission rate in relation to the total emergency department admissions also increased, from 1.2 % in 2005 to 1.9 % in 2012. 31.7 % of the patients were younger than 25 years. The reasons for self-poisoning were suicide attempt (18.1 %), intoxication (76.8 %) and drug overdose (2.9 %). The reason could not be clearly classified in 80 patients. Psychotropic drugs were used in 71.6 % of suicide attempts, while alcohol was the sole cause of intoxication in 80.1 % of cases in the intoxication group. Self-poisoning using at least two substances was observed in 52.0 % of the suicide attempts, 10.3 % of those with intoxication and 29.7 % of those with drug overdose. While alcohol remains the most common cause of intoxication, there was a drastic increase in the consumption of cannabinoids, Crystal Meth and gamma-hydroxybutyrate in the years 2011 and 2012. ICU admission was necessary in 16.6 % of the cases. There were 22 deaths (0.6 % of the study population), of whom 15 were in the suicide group (2.3 %), four (0.15 %) in the intoxication group, and three in the not clearly classified group (3.8 %).
Conclusion
Acute self-poisoning is an increasing medical issue. Psychotropic drugs remain the most common means of suicide attempt. Although alcohol intoxication is very frequent, intake of illicit drugs as the cause of emergency admission is increasing.
Zusammenfassung
Ziel
Beschreibung des Trends der akuten Selbstvergiftung in der Notfall- und Intensivmedizin.
Methode
Elektronische Akten erwachsener Patienten, die zwischen 2005 und 2012 wegen einer akuten Selbstvergiftung infolge eines Selbstmordversuches (Selbstmordgruppe), einer Berauschung (Intoxikationsgruppe) oder Medikamentenüberdosierung zwecks Schmerzlinderung (Überdosierungsgruppe) in der Notaufnahme des Universitätsklinikums Leipzig eingewiesen worden waren, wurden ausgewertet.
Ergebnisse
3533 Patienten (62,6 % männlich) wurden identifiziert, mit einem Anstieg von 305 Fällen im Jahre 2005 auf 624 in 2012. Die Aufnahmerate bezogen auf die Gesamtaufnahmen stieg von 1,2 % im Jahre 2005 auf 1,9 % im Jahre 2012 an. 31,7 % der Patienten waren < 25 Jahre alt. Die Ursachen der Selbstvergiftung waren Suizidversuch (18,1 %), Intoxikation (76,8 %) und Medikamentenüberdosierung (2,9 %). Bei 80 Fällen war eine genaue Gruppenzuordnung nicht möglich. Während psychotrope Medikamente bei 71,6 % der Suizidversuche angewandt wurden, war Alkoholintoxikation die Ursache bei 80,1 % der Fälle in der Intoxikationsgruppe. Selbstvergiftung mit mindestens zwei Substanzen lag bei 52,0 % der Suizidversuche, 10,3 % der Intoxikationsgruppe und 29,7 % der Gruppe mit Medikamentenüberdosierung vor. Während die Alkoholintoxikation nach wie vor am häufigsten vorkam, gab es eine drastische Zunahme der Intoxikationen mit Cannabinoiden, Crystal Meth und Gamma-Hydroxybuttersäure in den Jahren 2011 und 2012. Eine Aufnahme auf die Intensivstation war bei 16,6 % der Fälle erforderlich. Es gab 22 Todesfälle (0,6 % der gesamten Studienpopulation), von denen 15 aus der Suizidgruppe (2,3 %), vier aus der Intoxikationsgruppe (0,15 %), und drei aus der nicht eindeutig zugeordneten Gruppe (3.8 %) waren.
Zusammenfassung
Akute Selbstvergiftung ist ein zunehmendes medizinisches Problem. Psychotrope Medikamente stellen nach wie vor die häufigsten Suizidversuchsmittel dar. Obwohl die Alkoholintoxikation weiterhin am häufigsten vorkommt, nehmen illegale Drogen als notfallmedizinischer Einweisungsgrund zu.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Poisoning with alcohol or drugs is defined by the World Health Organization as a state of major disturbance of consciousness level, vital functions, and behavior following the administration in excessive dosage (deliberately or accidentally) of a psychoactive substance [1]. The physiological reaction to poisoning is highly dependent on the type and dose of the substance, and is influenced by the individual’s level of tolerance and organ function. Self-harm is defined as any act of self-poisoning or self-injury carried out by an individual irrespective of motivation [2]. Acute self-poisoning is one of the frequent causes of medical emergencies, and it presents a considerable burden to the health service system. Self-poisoning makes up for 0.6–2.1 % of all emergency department visits [3–5] and up to 17.3 % of intensive care unit (ICU) admissions [6–9]. Causes of self-poisoning are either a suicide attempt or accidental, whereby the latter group includes overdose with recreational drugs or alcohol intoxication, as well as drug overdose for alleviation of pain or discomfort without any suicidal intention. Self-poisoning represents a common method of suicide attempt and deliberate self-harm all over the world [4, 10–16].
The aim of this study is to present data on acute self-poisoning from the emergency department of a university hospital over a period of 8 years and to identify trends relating to epidemiology and substance used.
Methods
This is a retrospective study conducted at the University Hospital Leipzig in Germany. Consent for data acquisition and analysis were given by the Institutional Review Board of the University of Leipzig. Electronic charts of adult patients (≥ 18 years) who presented due to acute self-poisoning to the emergency department of the University Hospital Leipzig between January 2005 and December 2012 were included. Inclusion criterion was presentation with signs of acute poisoning, regardless of the type and amount of substance ingested. We have applied the definition of the World Health Organization regarding poisoning/intoxication versus substance abuse in identifying patients [1]. We have included only those patients who required emergency medical management for proven acute self-poisoning based on history, physical examination and drug screening. Since the physiological reaction to acute poisoning or intoxication is influenced by the individual’s level of tolerance and organ function, the symptoms and signs of acute poisoning or intoxication rather than drug levels were the mainstay of patient inclusion.
Patients treated in the emergency department for other reasons (commonly trauma) and in whom drug abuse was detected in the process were excluded, because these patients did not primarily present with signs of intoxication requiring medical attention by itself. Patients who presented to the emergency department for signs of poisoning despite appropriate intake of prescribed medication and those with accidental poisoning at workplaces or at home were also excluded from the analysis.
The following data were collected: patient characteristics, reason for and mechanisms of self-poisoning, admission time (month, weekday and daytime), repeated admissions, need for ICU admission, and outcome. In those patients with ICU admission, data on the drugs used for self-poisoning, length of ICU stay and ICU management were documented. Identification of drugs used for self-poisoning was based on history (the patient or relatives) and laboratory screening in blood and urine samples.
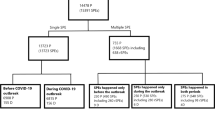
Depending on the trigger, patients were classified into three groups: suicide attempt (suicide group); intoxication with alcohol or recreational drugs (intoxication group), drug overdose in relation to relief of pain or discomfort (drug overdose group). If the trigger for self-poisoning could not be undoubtedly specified, patients were grouped as “not clearly classified”. This last group was not further analyzed due to the small size, except for mortality.
The data were analyzed using SPSS for Windows, version 20.0. Numerical data were analyzed for homogeneity using Kolmogorov-Smirnov and Shapiro-Wilk tests. Depending on their normal distribution, numerical data are given either as median with interquartile range [IQR] in square brackets or mean with standard deviation. Numerical data comparisons were conducted with either the Student’s t-test or Mann-Whitney U-test depending on their normal distribution. Categorical data comparison was carried out using chi square test. A p value < 0.05 was considered statistically significant.
Results
A total of 3.533 adults with acute self-poisoning (62.6 % males and 37.4 % females) were identified. The number of emergency department presentations continuously increased during the study period, from 305 in the year 2005 up to 624 in 2012 (an increase by 104.6 %). The yearly number of emergency department admissions for the intoxication group showed a continuous rise throughout the study period. During the same period, admission figures for self-poisoning as a suicide attempt showed an increase only in the year 2012, while there was no relevant increase in the drug overdose group (Fig. 1). The proportion of patients with acute self-poisoning in relation to the total emergency department admissions has also increased over the years (Table 1).
The median age of the study population was 35.0 [IQR 25.0] years for males and 29.0 [24.0] years for females (p < 0.001). 31.7 % of the patients were younger than 25 years, while 21.3 % belonged to the age group 25–34 years. Suicide attempts and drug overdose were more common in females than in males, while intoxication was more common in males than in females. The intoxication group included the youngest population compared to the other two groups (p < 0.001) (Table 2).
There was no age difference among males and females in the suicide group (median age 42.0 [23] vs. 37 [29] years, p = 0.093) and drug overdose group (36.5 [27] vs. 41.0 [45] years, p = 0.45), while females were significantly younger than males in the intoxication group (25.0 [20] years vs. 34.0 [14.9], p < 0.001).
The monthly distribution did not show any predilection. Presentations due to self-poisoning for suicide attempts were frequent on Mondays and Tuesdays (accounting for 32.7 % of the cases), with a gradual decrease until Saturdays. However, the daily differences were not significant. The most frequent presentation period (65.1 %) throughout the day was between noon and midnight. On the contrary, patients in the intoxication group frequently presented on Fridays (13.6 %), Saturdays (21.3 %) and Sundays (21.2 %), peak time of the day being 8 pm to midnight (21.9 %) and midnight to 4 am (29.8 %).
The means of self-poisoning are presented in Figs. 2, 3, 4. Benzodiazepines and antidepressants were the most common drugs used among the suicide group, while alcohol was the most common substance used in the intoxication group. Intoxication with alcohol only accounted for 81.0 % of the emergency admissions in the intoxication group. Self-poisoning using two or more substances was observed in 333 (52.0 %) cases in the suicide group, 279 (10.3 %) cases in the intoxication group, and 30 (29.7 %) cases in the drug overdose group. An interesting incident was lead poisoning in the years 2007 and 2008 among the intoxication group following consumption of adulterated street marijuana. This particular incident was already reported [17].
There was no significant trend change for drugs used in the suicide group and the drug overdose group throughout the study period. Regarding the intoxication group, while the yearly admission rate due to the sole alcohol intoxication remained almost unchanged around 80 % throughout the study period, there was a marked increase in the admission rate due to overdose of amphetamines/methamphetamines (“Crystal Meth”), cannabinoids and gamma-hydroxybutyrate (GHB)/gamma butyrolactone (GBL) in the years 2011 and 2012. The admission rate for opioid and benzodiazepine overdose in the intoxication group was the highest in 2007, with a gradual decrease afterwards (Fig. 5).
Repeated emergency department admissions for acute self-poisoning were observed in 427 cases (12.1 % of the total study population), which involved 7.5 % of the cases in the suicide group, 13.4 % of the intoxication group and 6.9 % of the drug overdose group. Admission to the ICU was considered necessary in 588 cases (16.6 %), with 61.4 % of the suicide group, 4.6 % of the intoxication group and 43.6 % of the drug overdose group being admitted. The top ten drugs that led to ICU admission are shown in Table 3. Acute poisoning with two or more drugs was observed in 48.6 % of the ICU admissions.
The most common reason for ICU admission was the need for vital sign monitoring (75.9 %). A Glasgow coma scale of ≤ 8 (25.2 %), respiratory insufficiency (2.7 %) and hypotension (1.7 %) were further indications. The median length of stay in the ICU was 27 [29.5] hours. The following management procedures were required during the ICU stay: mechanical ventilation (27.0 % of the cases), vasopressor support (9.4 %), administration of an antidote (27.8 %) and hemodialysis (3.6 %).
The need for immediate psychiatric treatment following completion of the medical management was significantly different between the groups (p < 0.001). 82.7 % of the patients in the suicide group, 31.7 % of those in the drug overdose group, but only 6.6 % of those in the intoxication group were transferred for subsequent immediate psychiatric treatment after conclusion of the medical management.
A total of 22 patients died (0.6 % of the total study population), of whom 15 were in the suicide group (2.3 %), four in the intoxication group (0.15 %), while three cases belonged to the not clearly classified group (3.8 %), with a statistically significant difference among the groups (p < 0.001). The causes of death were prolonged hypoxia (10), cardiac arrest (5) and multiple organ dysfunction (13). While 20 patients died in the ICU, two patients (from the intoxication group) died in the emergency department following a refractory cardiac arrest. There were no fatalities in the drug overdose group.
Discussion
This study included a large period of time, which gives an overview on the trend of clinically relevant acute self-poisoning in a German population. Although the presented data were from one center only, the Leipzig university hospital is responsible for the management of patients with acute self-poisoning from a large catchment area with a population of about 1.3 million.
Self-poisoning is a considerable issue in emergency medicine and its incidence is increasing. This is related to suicide attempts as well as intoxications with alcohol and recreational drugs. In our study, the yearly number of presentations for clinically relevant self-poisoning more than doubled between 2005 and 2012, intoxication being the major cause for this increase.
Acute intoxication has become an increasing concern. Similar to a study from the UK, young and male patients represent the majority [18]. Alcohol is still the leading means of intoxication, which is also observed elsewhere [7, 19]. Although the majority of these patients with the sole alcohol intoxication could be discharged after a short stay in the emergency department, alcohol intoxication remains a leading cause of hospital admission [20]. Observational data from emergency units are not uniform and depend on patient selection [7–9, 13, 21].
The increasing use of illegal drugs in the younger population is alarming. In our study, this was the case with amphetamines/methamphetamines, cannabinoids and GHB. Particularly, intoxication with amphetamines/methamphetamines (Crystal Meth) markedly increased since 2011. According to the German drug and addiction report for 2012 and 2013, this issue is strongly related to the German-Czech border regions, mainly affecting the Free State of Saxony, Germany. Since 2009, the number of Crystal Meth consumers in this German state that directly borders with the Czech Republic increased yearly by 25 %, probably because several Crystal Meth laboratories exist in the Czech Republic. The need for counseling of Crystal Meth consumers in 2011 in the State of Saxony was four times more than the German average [22].
The incidence of intoxication with GHB and its precursor GBL in our study cohort is generally not that high. However, this increased rapidly by the year 2012. Although GHB is an illicit drug, its precursor GBL, which is metabolized to GHB in the human body, is legally available as an industrial product. While the drug is a stimulant at lower doses, it results in unconsciousness in higher doses, which is the common cause of emergency department presentation among its consumers. The lack of appropriate laboratory detection methods may have influenced the true incidence of intoxication with GHB.
Although suicidal self-poisoning is not as frequent as intoxication, it is the major cause of ICU admission. The rates of ICU admissions for acute self-poisoning in the literature range from 2.2 to 29.2 % [23–27], with suicidal and parasuicidal self-poisoning being the most frequent cause. Patients in this group are older and the majority are females [12, 13, 21, 28]. The distribution of drugs used for suicidal attempts in our study is not different from previous European reports, with psychotropic drugs, especially benzodiazepines and antidepressants, being the leading substances [12, 13, 21, 23]. Only in the UK was paracetamol the most frequently used drug for suicidal attempts [29, 30]. The use of these drugs is frequently associated with a simultaneous alcohol intoxication [13].
Another concern is the abuse of drugs, particularly analgesics and sedatives, for relief of discomfort, which mainly affects females. Although the incidence of such an abuse leading to emergency consultation did not increase throughout the investigated period of our study, this does not reflect the true dimension of this problem. Appropriate health education and sales control may be necessary preventive measures.
More than 10 % of the patients with self-poisoning were re-admitted at least once during our study period. Figures from other publications vary between 8 and 21 % [31–33]. Risk factors for readmission are young age, past psychiatric admission, drug addiction, abuse of antidepressants and mixed self-poisoning [32, 33].
The Glasgow Coma Scale seems to be a major indication for ICU admission [34]. Future investigations should evaluate whether this scale alone should be taken as a major reason for ICU resource utilization. However, this issue is also dependent on the emergency department organization, such as the capacity to monitor such patients for several hours. The length of ICU stay in our study was similar to the literature report [8, 35].
Emergency management of poisoning mainly involves maintaining vital functions. Primary and secondary poison elimination can be implemented, depending on the type of the drug, the time frame, and organ function (particularly liver and kidney function). Antidotes are available for a few substance groups only [36]. Even then, their use is mostly limited, particularly regarding benzodiazepine and opioid overdose, because their half-life is shorter than that of the toxic drug. However, they can be useful as a differential diagnosis tool, in case the cause of poisoning is not clear. Patients with self-poisoning die in the early stage either due to respiratory or cardiac arrest. Late deaths are mostly due to organ dysfunctions and the resultant complications. Therefore, community education and early identification of a poisoning are essential to prevent tragic consequences.
Psychiatric counseling and therapy is commonly recommended for those patients with suicidal or parasuicidal self-poisoning, which is similar to another German study [13]. However, this figure varies depending on the patient population. In Norway, only 38 % of the patients with suicidal self-poisoning received further psychiatric management [37]. Psychiatric counseling among patients with intoxication is low. Most of these patients left the emergency department and the ICU on their own after stabilization of their acute condition. Another reason for the low psychiatric counseling in this subgroup of our study population may be that the initial psychiatric consultation was targeted to rule out a suicide attempt in order to avoid possible medico-legal issues. The relatively high rate of need for psychiatric counseling among those with self-poisoning for relief of pain or discomfort may indicate an underlying psychiatric disorder.
Mortality following self-poisoning is generally low [7, 19, 26, 38]. In our study, we considered only hospital mortality. A recent study showed a hospital mortality rate of 2.1 % for acute poisoning, with a rise to 9.3 % 24 months after ICU admission [38].
Our study has certain limitations. Firstly, it is retrospective, so that details regarding medical and social history of the patients were not complete. Secondly, this study included only those patients who were brought to the emergency department, thus not representing the true incidence of self-poisoning in the general population. However, it represents the epidemiology of clinically relevant acute self-poisoning.
Conclusion
Acute self-poisoning is a major concern in emergency medicine. Psychotropic drugs are still the leading cause among suicidal self-poisoning. While alcohol is still a major issue, the incidence of illicit drug intake is increasing among those with acute intoxication. The experience in certain European border regions regarding illicit drugs makes the need for international cooperation in preventive measure more than obvious. Self-poisoning related to relief of pain or discomfort implicates the need for appropriate public education, increased psychiatric counseling as a preventive measure and proper drug control.
References
Babor T, Campbell R, Room R, Saunders J (1994) Lexicon of alcohol and drug terms. World Health Organization, Geneva
National Institute for Clinical Excellence (2004) Self-harm. The short-term physical and psychological management and secondary prevention of self-harm in primary and secondary care. National Clinical Practice Guideline Number 16. Stanley L. Hunt Ltd., Northamptonshire
Cook R, Allcock R, Johnston M (2008) Self-poisoning: current trends and practice in a U.K. teaching hospital. Clin Med 8:37–40
Prescott K, Stratton R, Freyer A, Hall I, Le Jeune I (2009) Detailed analyses of self-poisoning episodes presenting to a large regional teaching hospital in the UK. Br J Clin Pharmacol 68:260–268
Hendrix L, Verelst S, Desruelles D, Gillet J-B (2012) Deliberate self-poisoning: characteristics of patients and impact on the emergency department of a large university hospital. Emerg Med J 30:e9
Buchanan WJ (1991) A year of intentional self poisoning in Christchurch. N Z Med J 104:470–472
Fürst S, Habscheid W (1993) Acute poisoning in patients of a medical intensive care unit. Dtsch Med Wochenschr 118:849–853
Viertel A, Weidmann E, Brodt HR (2001) Cases of acute poisoning admitted to a medical intensive care unit. Dtsch Med Wochenschr 126:1159–1163
Schwake L, Wollenschlager I, Stremmel W, Encke J (2009) Adverse drug reactions and deliberate self-poisoning as cause of admission to the intensive care unit: a 1-year prospective observational cohort study. Intensive Care Med 35:266–274
Weir P, Ardagh M (1998) The epidemiology of deliberate self poisoning presenting to Christchurch Hospital Emergency Department. N Z Med J 111:127–129
Bentur Y, Raikhlin-Eisenkraft B, Lavee M (2004) Toxicological features of deliberate self-poisonings. Hum Exp Toxicol 23:331–337
Mauri MC, Cerveri G, Volonteri LS, Fiorentini A, Colasanti A, Manfré S, Borghini R, Pannacciulli E (2005) Parasuicide and drug self-poisoning: analysis of the epidemiological and clinical variables of the patients admitted to the Poisoning Treatment Centre (CAV), Niguarda General Hospital, Milan. Clin Pract Epidemiol Ment Health 1(1):5
Eisenbach C, Ungur AL, Unger J, Stremmel W, Encke J (2008) Admission to intensive care for parasuicide by self-poisoning: Variation by time cycles, climate and the lunar cycle. Psychiatry Res 161:177–184
Ghazinour M, Emami H, Richter J, Abdollahi M, Pazhumand A (2009) Age and gender differences in the use of various poisoning methods for deliberate parasuicide cases admitted to loghman hospital in Tehran (2000–2004). Suicide Life Threat Behav 39:231–239
Tsirigotis K, Gruszczynski W, Tsirigotis M (2011) Gender differentiation in methods of suicide attempts. Med Sci Monit 17:65–70
Kupferschmid S, Gysin-Maillart A, Bühler SK, Steffen T, Michel K, Schimmelmann BG, Reisch T (2013) Gender differences in methods of suicide attempts and prevalence of previous suicide attempts. Z Kinder Jugendpsychiatr Psychother 41:401–405
Busse F, Omidi L, Timper K, Leichtle A, Windgassen M, Kluge E, Stumvoll M (2008) Lead poisoning due to adulterated marijuana. N Engl J Med 358:1641–1642
Haw CM, Hawton K (2011) Problem drug use, drug misuse and deliberate self-harm: trends and patient characteristics, with a focus on young people, Oxford, 1993–2006. Soc Psychiatry Psychiatr Epidemiol 46:85–93
Oksa H, Pitkäjärvi T, Koskelainen J, Ruosteenoja R, Kataja M (1981) Self-poisoning patients in an intensive care unit. Ann Clin Res 13:96–101
Balsa AI, French MT, Maclean JC, Norton EC (2009) From pubs to scrubs: alcohol misuse and health care use. Health Serv Res 44:1480–1503
Weilemann LS, Hilgers HJ, Reckmann A (1996) Current aspects of para-suicidal poisoning. Med Klin (Munich) 91:355–358
Die Drogenbeauftragte der Bundesregierung, Bundesministerium für Gesundheit (2013) Drogen- und Suchtbericht. enka-druck GmbH, Berlin
Islambulchilar M, Islambulchilar Z, Kargar-Maher MH (2009) Acute adult poisoning cases admitted to a university hospital in Tabriz, Iran. Hum Exp Toxicol 28:185–190
Hatzitolios AI, Sion ML, Eleftheriadis NP, Toulis E, Efstratiadis G, Vartzopoulos D, Ziakas AG (2001) Parasuicidal poisoning treated in a Greek medical ward: epidemiology and clinical experience. Hum Exp Toxicol 20:611–617
Verstraete AG, Buylaert WA (1995) Survey of patients with acute poisoning seen in the Emergency Department of the University Hospital of Gent between 1983 and 1990. Eur J Emerg Med 2:217–223
Hall AK, Curry C (1994) Changing epidemiology and management of deliberate self poisoning in Christchurch. N Z Med J 107:396–399
Mowry JB, Spyker DA, Cantilena LR Jr, Bailey JE, Ford M (2013) 2012 Annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 30th annual report. Clin Toxicol (Phila) 51:949–1229
Spiller HA, Appana S, Brock GN (2010) Epidemiological trends of suicide and attempted suicide by poisoning in the US: 2000–2008. Leg Med (Tokyo) 12:177–183
Bergen H, Hawton K, Waters K, Cooper J, Kapur N (2010) Epidemiology and trends in non-fatal self-harm in three centres in England: 2000–2007. Br J Psychiatry 197:493–498
Camidge DR, Wood RJ, Bateman DN (2003) The epidemiology of self-poisoning in the UK. Br J Clin Pharmacol 56:613–619
McEvedy CJ (1997) Trends in self-poisoning: admissions to a central London hospital, 1991–1994. J R Soc Med 90:496–498
Oh SH, Park KN, Jeong SH, Kim HJ, Lee CC (2011) Deliberate self-poisoning: factors associated with recurrent self-poisoning. Am J Emerg Med 29:908–912
Payne RA, Oliver JJ, Bain M, Elders A, Bateman DN (2009) Patterns and predictors of re-admission to hospital with self-poisoning in Scotland. Public Health 123:134–137
Maignan M, Pommier P, Clot S, Saviuc P, Debaty G, Briot R, Carpentier F, Danel V (2014) Deliberate drug poisoning with slight symptoms on admission: are there predictive factors for intensive care unit referral? A three-year Retrospective Study. Basic Clin Pharmacol Toxicol 114:281–287
McMahon A, Brohan J, Donnelly M, Fitzpatrick GJ (2013) Characteristics of patients admitted to the intensive care unit following self-poisoning and their impact on resource utilisation. Ir J Med Sci 183:391–395
Weidhase L, Hentschel H, Mende L, Schulze G, Petros S (2014) Acute poisoning in adults. Internist (Berl) 55:281–294
Bjornaas MA, Hovda KE, Heyerdahl F, Skog K, Drottning P, Opdahl A, Jacobsen D, Ekeberg O (2010) Suicidal intention, psychosocial factors and referral to further treatment: a one-year cross-sectional study of self-poisoning. BMC Psychiatry 10:58
Brandenburg R, Brinkman S, de Keizer NF, Meulenbelt J, de Lange DW (2014) In-hospital mortality and long-term survival of patients with acute intoxication admitted to the ICU. Crit Care Med 42:1471–1479
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Sorge, L. Weidhase, M. Bernhard, A. Gries, S. Petros declare no conflict of interest.
The accompanying manuscript does not include studies on humans or animals.
Rights and permissions
About this article
Cite this article
Sorge, M., Weidhase, L., Bernhard, M. et al. Self-poisoning in the acute care medicine 2005–2012. Anaesthesist 64, 456–462 (2015). https://doi.org/10.1007/s00101-015-0030-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00101-015-0030-x