Abstract
Purpose
Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) represents a minimally invasive technique of aortic occlusion (AO). It has been demonstrated to be safe and effective with appropriate training in traumatic hemorrhage with hemodynamic instability; however, its indications are still debated. The aim of this systematic review and meta-analysis is to assess the impact of REBOA on mortality in torso trauma patient with severe non-compressible hemorrhage compared to other temporizing hemostatic techniques.
Study design
The primary outcome is represented by 24-h, and in-hospital mortality. Secondary outcomes are post-procedural hemodynamic improvement (systolic blood pressure—SBP), mean injury severity score (ISS) differences, treatment-related morbidity, transfusional requirements and identification of prognostic factors.
Results
A significant survival benefit at 24 h (RR 0.46; 95% CI 0.27–0.79; I2: 55%; p = 0.005) was highlighted in patients undergoing REBOA. Regarding in-hospital mortality (RR 0.99; 95% CI 0.75–1.32; I2: 73%; p = 0.98) no differences in risk of death were noticed. A hemodynamic improvement—although not significant—was highlighted, with 55.8 mmHg post-AO SBP mean difference between REBOA and control groups. A significantly lower mean number of packed Red Blood Cells (pRBCs) was noticed for REBOA patients (mean difference: − 3.02; 95% CI − 5.79 to − 0.25; p = 0.033). Nevertheless, an increased risk of post-procedural complications (RR 1.66; 95% CI 0.39–7.14; p = 0.496) was noticed in the REBOA group.
Conclusions
REBOA may represent a valid tool in the initial treatment of multiple sites subdiaphragmatic hemorrhage with refractory hemodynamic instability. However, due to several important limitations of the present study, our findings should be interpreted with caution.
Level of evidence
Level III according to ELIS (SR/MA with up to two negative criteria).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The concept of aortic occlusion (AO) in cases of traumatic non-compressible torso hemorrhage (NCTH) is still debated and numerous studies published in the literature have documented survival benefits in case of massive abdominal and pelvic bleeding [1, 2]. Direct (open) aortic cross-clamping via resuscitative thoracotomy (RT) can provide temporary hemodynamic stability, supporting proximal aortic pressure and minimizing subdiaphragmatic hemorrhage: on the other hand, the procedure is extremely invasive and associated with poor survival rates (less than 10% in case of blunt trauma [3]). Extraperitoneal pelvic packing (EPP) is another damage control procedure that appears as a valid alternative in case of exsanguination arising from pelvic ring disruption [4,5,6].
Resuscitative Endovascular Balloon Occlusion of the aorta (REBOA) has emerged as a less invasive alternative to open aortic cross-clamping [7]. The technique consists of placing an aortic balloon through a sheath into the common femoral artery. The balloon can be inflated in Zone 1 (between the left subclavian artery and the celiac axis), Zone 2 (between the celiac axis and the lower margin of the renal arteries), or Zone 3 (between the lower margin of the renal arteries and the iliac bifurcation) [8] (Fig. 1).
REBOA has been shown to be feasible and effective, with appropriate training, compared to RT: in fact, aortic occlusion helps controlling hemorrhages arising from any region below the site of occlusion, allowing for temporary hemodynamic stability before definitive hemostasis can be performed.
However, clear evidence regarding its effectiveness is lacking as well as appropriate patients’ selection and severe complications are described [9].
Our aim is to clarify the role of REBOA in case of traumatic hemorrhagic shock due to NCTH, compared to the most commonly employed emergent hemostatic alternatives—in particular RT and EPP.
Methods
Search strategy
A systematic review of the English-language literature was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and AMSTAR (Assessing the methodological quality of systematic reviews) Guidelines [10, 11]. The meta-analysis was conducted following the MOOSE recommendations.
The systematic review protocol was registered on the International Prospective Register of Systematic Reviews—PROSPERO (registration ID: CRD42021243141).
The PubMed, Scopus, and Web of Science databases were screened without time restrictions up to March 22nd, 2021 using the keywords “trauma”, “traumatic bleeding”, “hemorrhage”, “exsanguination”, “abdominal, pelvic, abdomino-pelvic trauma”, “resuscitative endovascular balloon occlusion of the aorta”, “REBOA”, “intra aortic balloon occlusion”, “IABO”, “aortic occlusion”, “resuscitative thoracotomy” “extraperitoneal pelvic packing”, “preperitoneal pelvic packing”, “EPP”. The research also included all the MeSH Terms. Articles without free full text available were searched through the University of Milan digital library and direct contact with authors. A hand-search of references of included studies and previous reviews on the topic was also performed to include additional relevant studies according to our selection criteria. Two investigators (SF, AB) carried out the literature search independently.
Inclusion criteria
Only clinical studies reporting survival outcomes of patients suffering from traumatic NCTH with hemodynamic instability treated with REBOA were included.
A specific population (P), intervention (I), comparator (C), outcome (O), and study design (S) (PICOS) framework was specified to define study eligibility, as recommended. In particular, the following criteria were outlined:
-
Population (P): patients suffering from blunt or penetrating traumatic torso hemorrhage with hemodynamic instability;
-
Intervention (I): Partial or total aortic occlusion through resuscitative endovascular balloon occlusion of the aorta (REBOA);
-
Comparison (C): patients undergoing other temporary hemostatic procedures such as RT with aortic cross-clamping (ACC), and EPP;
-
Outcomes (O): in-hospital mortality, post-treatment morbidity;
-
Study design (S): all study designs.
Studies with insufficient reporting of the PICOS criteria were excluded.
Exclusion criteria
All preclinical studies were excluded from the review. Studies written in non-English language and studies reporting overlapping series were excluded as well. Similarly, case reports, editorials, previously published reviews, book chapters and commentaries were deemed not eligible.
Systematic review process
Mendeley reference software (Mendeley Ltd, London, UK) was used to identify and remove duplicates among identified records. Overall, 1248 articles were preliminarily identified by the literature search. After exclusion of duplicates, two independent reviewers (SF, AB) screened titles and abstracts of 1245 records. An a priori developed screening form was created to guide study selection. Investigators were blinded to each other's decisions. The disagreement was solved by a third party (SG), who supervised the systematic review process.
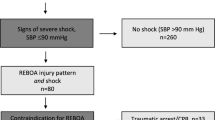
Twenty-five articles were assessed for eligibility. Finally, eight studies fulfilling all inclusion criteria were selected for qualitative and quantitative analysis. The flow-chart depicting the overall review process according to PRISMA is reported in Fig. 2.
Assessment of risk of bias
The risk of bias was assessed for individual studies according to the ROBINS-I tool provided by the Cochrane Collaboration [12] independently by two investigators (SF, SP). The following domains were explored: (1) bias due to confounding; (2) bias in selection of participants into the study; (3) bias in classification of interventions; (4) bias due to departures from intended interventions; (5) bias due to missing data; (6) bias in measurement of outcomes; and (7) bias in selection of the reported results.
Data were collected according to the methodology proposed by Sterne [12] in a computerized spreadsheet. Bar and traffic light plots were created to display the results of the risk of bias assessment graphically.
Data extraction and assessment of included studies
Data were extracted independently by three authors (SG, SF, AB). Information about study design and methodology, participant demographics characteristics, mechanism and site of trauma, vitals on ED arrival and after hemostatic procedure (systolic blood pressure—SBP; heart rate—HR; Glasgow coma scale—GCS), injury severity score (ISS), aortic zone placement, REBOA access, occlusion time, type of occlusion (partial vs total), number of packed red blood cells (pRBCs), fresh-frozen plasma (FFP), platelet pools (PP) were gathered in a computerized spreadsheet (Microsoft Excel 2016; Microsoft Corporation, Redmond; WA). Twenty-four-hour, 48-h, overall survival and complication rates, as well as the increase in systolic blood pressure after hemostatic procedure were collected as well. An attempt to retrieve missing data was done through direct contact with the authors. In case of disagreement, two further investigators (SC, OC) helped resolve it through discussion.
Two authors (SP, FB) independently assessed the quality of evidence provided by each study using the Oxford Center for Evidence-Based Medicine scoring system [13]. The methodological quality of each retrospective comparative study was assessed using the validated Newcastle–Ottawa Scale (NOS) [14]; studies that scored ≥ 7 were considered of high quality.
Primary and secondary endpoints
The primary outcome was represented by 24-h, and in-hospital mortality. Secondary outcomes were represented by post-procedural hemodynamic improvement (SBP), mean ISS differences between the two groups, treatment-related morbidity, transfusional requirements and identification of prognostic factors.
Statistical analysis
Primary outcome measures were expressed in terms of Risk Ratio (RR) and 95% Confidence Intervals (CI) for overall survival and disease-free survival. Meta-analyses of binary outcomes were developed. Moreover, meta-analyses of proportion were performed to explore cumulative survival rates of different subgroups according to the site of injury.
Secondary outcome measures were reported as means/standard deviation (SD) and RR with 95% CI. Mean SBPs were retrieved from each manuscript. Whenever not overtly reported, they were computed from medians, ranges, interquartile ranges (IQR) and sample sizes according to Wan’s method[15]. Meta-analyses of binary outcomes and means were developed.
Fixed and random effects models based on the Mantel–Haenszel method were built to assess the impact of heterogeneity on results. In the presence of low heterogeneity (< 25%), a fixed-effect model was chosen to compute the outcome. The presence of outliers was investigated, and their effect sizes were excluded.
Heterogeneity between studies was quantified by I2 statistic and Cochran’s Q test; cut-off values of 25%, 50%, and 75% were considered as low, moderate, and high, respectively [16]. Sensitivity analyses were conducted after inspecting patterns of effect sizes and heterogeneity of the included studies. To identify studies overly contributing to heterogeneity Graphic Display of Heterogeneity (GOSH) plots were developed, and sensitivity analysis was conducted excluding studies predominantly responsible for heterogeneity. Alternatively, when the limited number of studies precluded the possibility to perform influence analysis through GOSH plots, the leave-one-out method was used.
Mixed-effects meta-regression models were developed to investigate the association between potential predictors of improved survival and effect size differences. For this purpose, only patients undergoing aortic occlusion through REBOA were considered in the analysis. Due to the insufficient number of included studies, the possibility to build multiple meta-regression was precluded. Therefore, the analysis was conducted exploring the moderators one by one.
Funnel plots were developed to explore publication bias, and Egger’s test of the intercept was used to quantify funnel plots’ asymmetry. Duval & Tweedie’s trim-and-fill method was adopted to estimate and adjust the number and outcomes of missing studies each time Egger’s test demonstrated significant asymmetry.
Statistical analysis was conducted with R statistical software (The Comprehensive R Archive Network—CRAN, ver. 4.0.0 × 64) [17], using “meta”, “metafor”, “robvis” and “dmetar” packages [18,19,20,21].
Results
Descriptive noncomparative analysis of included studies and primary endpoint
Eight studies [22,23,24,25,26,27,28,29] were included in the qualitative and quantitative analysis. All of them were retrospective except for the one published by Henry et al. [27]. The excluded studies were deemed ineligible due to lack of separated outcome data for REBOA and control groups, type of hemostatic procedure not specified in the control group, and overlapping series.
In total, 3215 patients were included in the meta-analysis. Six out of 8 studies were conducted in USA trauma centers. The mean age was 44.3 years. The male population represented 79.1% of patients. In 2083 cases (64.8%), patients suffered from blunt trauma. Further study groups characteristics are reported in Table 1.
Primary endpoint
Meta-analysis of binary outcomes: 24-h and in-hospital mortality
Five studies [22, 23, 25, 28, 29] reported 24-h mortality rates. Meta-analysis of binary outcomes pointed out a reduced, although non-significant, risk of death for patients undergoing AO through REBOA (RR 0.71; 95% CI 0.31–1.63; I2: 90.1%; p = 0.416). The pooled mortality of REBOA patients was 23.5% (95% CI 0.15–0.35).
All studies reported data regarding in-hospital mortality. Meta-analysis of binary outcomes highlighted a reduced, although non-significant, risk of death for patients undergoing AO through REBOA (RR 0.90; 95% CI 0.70–1.16; I2: 93.5%; p = 0.42). The pooled in-hospital mortality of REBOA patients was 58.3% (95% CI 0.47–0.69). Four studies reported separated data regarding the aortic zone of balloon deployment. In the studies by Henry et al. [27], all the balloons were inflated in Zone 1, whereas in those by Asmar et al., Mikdad et al., and Frassini et al. [25, 28, 29] they were all deployed in Zone 3. Subgroup analysis pointed out a non-significant survival benefit for patients undergoing AO with REBOA in Zone 1 compared to ACC (RR 0.93; 95% CI 0.86–1.01). On the other hand, an increased, although not significant, mortality was noticed for patients undergoing AO in Zone 3 compared to EPP (RR 1.13; 95% CI 0.62–2.09; I2: 71.2%).
Sensitivity analysis
After conducting sensitivity analysis through the leave-one-out method, we excluded the study by Mikdad et al. [28]. A significant survival benefit at 24 h for patients belonging to the REBOA group was noticed (RR 0.46; 95% CI 0.27–0.79; I2: 55%; p = 0.005).
Regarding in-hospital mortality, GOSH plot analysis allowed to identify the studies by Bukur et al. and Henry et al. [26, 27] as the ones overtly contributing to heterogeneity. After their exclusion, no differences in risk of death were noticed between REBOA and control patients (RR: 0.99; 95% CI: 0.75–1.32; I2:73%; p = 0.98). The pooled in-hospital mortality of REBOA patients after sensitivity analysis was 62.7% (95% CI 0.52–0.72).
Subgroup analysis confirmed an increased mortality for patients undergoing AO in Zone 3 compared to EPP (RR: 1.13; 95% CI 0.62–2.09; I2: 71%).
Meta-analysis of binary outcomes’ forest plots, before and after sensitivity analysis, is shown in Fig. 3. Meta-analysis of proportions’ forest plots, before and after sensitivity analysis, is available in supplementary materials.
Secondary endpoints
Meta-analysis of means: hemodynamic improvement and ISS
Only 4 studies [22, 24,25,26, 29] reported data regarding ED arrival SBP. The study by Abe et al. [22] was excluded from the analysis because it reported medians without interquartile ranges; therefore computing means and SDs was not possible. The mean difference between REBOA and control groups was 6.9 mmHg (95% CI − 37.1 to 50.9; p = 0.65) (Fig. 4A).
Data regarding pre–post-procedural SBP were available only in 2 studies [26, 29]. The mean difference between SBP before and after the procedure was 6.7 mmHg (95% CI − 128.9 to 142.2; p = 0.64) for the control group and 44.7 mmHg (95% CI − 308 to 397.4; p = 0.35) for the REBOA group, respectively.
Only two studies [26, 29] reported data regarding post-AO SBP. The mean difference between REBOA and control groups was 55.8 mmHg (95% CI − 119.7 to 231.4; p = 0.15) (Fig. 4B).
Seven studies [7, 24,25,26,27,28,29] reported information regarding ISS in the two groups. We found a lower, although non-significant, mean ISS for patients undergoing REBOA compared to ACC (mean difference: − 2.97; 95% CI − 6.36 to 0.42; I2: 62.9%; p = 0.076) (Fig. 4C).
Three studies [24, 25, 28] reported data regarding transfusional requirement. A significant lower mean of pRBCs (mean difference: − 3.02; 95% CI − 5.79 to − 0.25; p = 0.033) was noticed for REBOA patients (Fig. 4D).
Meta-analysis of binary outcomes: post-procedural morbidity
Three studies [25, 26, 28] reported data regarding post-procedural morbidity. The comparison between the two groups highlighted an increased risk of complications for patients undergoing AO with REBOA (RR: 1.66; 95% CI: 0.39–7.14; p = 0.496) (Fig. 4D).
Meta-analysis of prognostic factors related to survival
Meta-regression analysis showed that raising ISS (RR 1.14; 95% CI 1.01–1.29; p = 0.035) and increasing number of transfused pRBCs (RR 1.15; 95% CI 1.03–1.28; p = 0.009) were the only variables significantly related to reduced survival. Year of publication, increasing SBP and HR at ED arrival as well as balloon deployment in Zone 3 were moderators associated with a trend towards a reduction in the risk of death. Detailed results are displayed in Table 2. Forest plots of secondary endpoints and bubble plots of meta-regression analysis are available in supplementary materials.
Risk of bias assessment
Figure 5A summarizes the risk of bias evaluation according to the latest version of the Cochrane Collaboration handbook. Serious risk of bias was detected in the domains “bias due to confounding” and “bias due to deviations from intended interventions”. Moderate risk of bias was found mainly in the domain “bias due to selection of participants”.
Assessment of publication bias
Egger’s test of 24-h mortality meta-analyses did not highlight significant asymmetry (p = 0.582), whereas significant asymmetry was detected for in-hospital mortality (p = 0.012). Contour enhanced funnel plots of publication bias are reported in Fig. 5B–C.
Discussion
The present study was designed to evaluate the efficacy of REBOA compared to other temporary hemostatic techniques in hemodynamically unstable patients suffering from major trauma with non-compressible torso hemorrhage. Our analysis evaluated the survival outcome of these patients, the hemodynamic improvement and the incidence of complications related to different treatments.
Compared to the largest systematic review and meta-analysis published to date [9], the current manuscript has been designed to focus exclusively on the use of REBOA in exsanguination from major trauma.
Our results suggested a potential beneficial role of REBOA in NCTH, but several considerations must be made.
First, our analysis highlighted a significant beneficial role for patients treated with REBOA in terms of 24-h mortality. Of notice, the original comparison including five studies failed to point out any significant difference and was burdened by severe heterogeneity (I2 = 88%). Sensitivity analysis allowed us to detect the study published by Mikdad et al. as the one mainly contributing to heterogeneity. After excluding it, I2 value dropped to 55% allowing the achievement of significant results with moderate heterogeneity. It should be kept in mind that the exclusion of the aforementioned study was not on purpose (to obtain results more favorable to REBOA), but it is the product of our statistical methodology that tends to achieve more homogenous results.
Regarding in-hospital mortality, no differences were found between the two groups, neither before, nor after sensitivity analysis. Subgroup analysis underlined a greater survival benefit for patients undergoing REBOA deployment in Zone 1 compared to ACC. Nevertheless, this finding was supported by the results of a single study [27]. Hemorrhagic patients managed with REBOA deployed in Zone 1 could be less severe than patients treated with standard damage control techniques, such as RT, a technique usually reserved to subjects who suffer from cardiac arrest or peri-arrest condition. Anyway, no significant differences in mean ISS were found between the two groups in our analysis. Our findings reinforce what recently reported in the joint statement by Bulger et al. [30]; REBOA is indicated in case of hemorrhagic shock from traumatic bleeding below the diaphragm when patients are refractory to resuscitation.
Conversely, patients suffering mainly from pelvic ring disruption seem to benefit more from EPP. This represents one of the most debated topics of trauma surgery in recent years. The World Society of Emergency Surgery (WSES) 2017 guidelines on pelvic trauma suggest to always consider EPP in patients with pelvic fracture-related hemodynamic instability, especially in the absence of an angiography service [32]. This concept was already hypothesized by Burlew et al. [33] and confirmed by Frassini et al. [4]. On the other hand, the WSES panel states that REBOA in Zone 3 should be considered as a bridge to definitive treatment, but partial should be preferred over total occlusion to decrease the risk of ischemic injuries. Such ambivalence may rely on the relative ease to perform both techniques, even in the Emergency Department [34,35,36]. However, despite our results highlighted better outcomes for EPP patients compared to Zone 3 REBOA, it should be noted that to perform EPP, specific surgical skills are required, whereas REBOA placement can be performed even by other critical care professionals, such as anesthesiologists or emergency physicians. Another consideration that should be made is that one technique does not exclude the other: as a matter of fact, some authors [28] suggest that REBOA can be performed as a temporizing procedure en route to EPP.
Furthermore, the use of REBOA seems to be burdened by a greater, although not significant, morbidity compared to ACC/EPP. Our analysis highlighted a near twofold increased risk of complications including pseudoaneurysms, distal embolism, extremity ischemia, lower extremity compartment syndrome and need for amputation.
Our results support a trend towards hemodynamic improvement for REBOA patients compared to other temporary hemostatic procedures, although this result was not significant and burdened by a wide confidence interval. On the one hand, raising SBP represents a major goal in traumatic exsanguination to maintain adequate cerebral and cardiac perfusion. However, it should be kept in mind the non-negligible risk of fatal hemorrhage related to a sudden increase in SBP, especially in those patients with severe, unrecognized head and chest injuries. Elkbuli et al. [37] in a recent paper questioned whether an increase in SBP by REBOA may support or worsen traumatic brain injuries: improving cerebral perfusion is one of the REBOA targets, but at the same time, transient hypertension due to aortic occlusion may increase cerebral edema and intracranial pressure. Physiological sequelae must be considered when REBOA is compared to other damage control procedures. Some data, while underlining an increased coronary perfusion, demonstrates non-negligible adverse effects as well [8]. REBOA, especially when complete occlusion is performed, produces variable degrees of mesenteric, hepatic, renal, spinal cord and lower extremity ischemia and induces an important ischemia–reperfusion injury when deflated[38].
Based on the aforementioned considerations, there is consensus against REBOA use in case of bleeding site proximal to the left subclavian artery or originating from the neck, whereas no explicit contraindications are stated in case of chest hemorrhage [31, 39].
Another key point of our analysis is represented by transfusion requirement: a significantly lower amount of pRBCs in the first 24 h was detected for patients undergoing AO through REBOA (3 units less than the control group). This finding supports the impact of REBOA as an effective bridge to definitive hemostasis.
Not surprisingly, meta-regression analysis identified raising ISS and increasing number of transfused pRBCs as the only potential predictors of reduced survival. Of notice, all the variables included in meta-regression analysis were burdened by severe heterogeneity.
Considering our data and current evidence [30, 31] from the literature, we propose a new treatment algorithm to summarize abdominal and pelvic hemorrhage management (Fig. 6).
Our research is based on a strict methodology considering only torso trauma patients, and one of its main strengths is represented by robust statistics. Compared to previous similar meta-analyses [9, 40], our study not only focuses selectively on trauma patients but encompasses recent evidences matching survival outcomes of REBOA inflated in Zone 3 and EPP patients. To the best of our knowledge, this is the first meta-analysis providing results of a direct comparison between Zone 1–3 REBOA and ACC-EPP. Similarly, it is the first to analyze the prognostic effect of different variables on survival outcome of patients undergoing AO through REBOA.
However, several limitations need to be underlined. First, the retrospective or observational nature of the studies included, without a random assignment to a treatment arm, contributes to weakening the quality of our results. Furthermore, no high-quality studies (NOS ≥ 7) were present in the current meta-analysis. On the other hand, it is worth noticing that designing a randomized control trial in the field of trauma and emergency surgery is extremely challenging. As a matter of fact, it is difficult to obtain similar treatment arms groups because of multiple variables influencing the outcomes, such as type and combination of injuries, logistics of facilities, availability of hospital services, and of surgical/intensive care expertise. Ethical issues can also be a problem while drafting such kind of RCTs.
Directly connected to the retrospective/observational nature of the studies included is the issue regarding the risk of bias: in almost the totality of the studies included, serious risk of bias was detected in the domain “bias due to confounding”. On the other hand, it should be remembered that is extremely rare to find a low risk of this kind of bias in non-randomized studies. Furthermore, even though in small proportion (< 25%), serious risk of bias was detected also in the domain “bias due to deviation from intended intervention”.
Another major drawback is represented by the lack of a univocal definition of “non-responder” patient. Of note, neither in the latest version of ATLS [41], the volume of crystalloids and the exact number of blood units are well defined.
Furthermore, the time elapsed from ED admission to AO may affect the survival outcome of NCTH patients, but unfortunately, this kind of information is often missing across available publications.
Finally, the wide heterogeneity of included studies burdens the quality of our results. Despite the strict selection criteria and advanced influence analysis techniques, the total variation across studies (I2) remained moderate. This may reflect, besides the unavoidable heterogeneity owing to chance, a prominent effect of systematic differences between the studies.
Our findings suggest that patients suffering from NCTH undergoing AO through REBOA may have an improved survival over the first 24 h. However, considering in-hospital mortality, no survival advantage was detected in comparison to the control group.
Moreover, considering the subset of patients with isolated pelvic injuries, Zone 3 REBOA may have a worse survival trend compared to EPP. Nevertheless, it should be observed that these results are not significant and based on the pooled results of only three studies for a total 466 patients. Furthermore, mortality in pelvic ring fractures is multifactorial and often not only related to pelvic hemorrhage alone.
Conclusions
Due to the limited number, the high risk of bias (at least in several domains) and the wide heterogeneity of the included studies, we retain our findings should be interpreted with extreme caution. Based on all these considerations, it may be worth reading the present study as supporting the non-inferiority of REBOA compared to open aortic occlusion rather than its superiority.
In this setting, REBOA may be considered as a first-line treatment option in case of multiple sites subdiaphragmatic hemorrhage in the presence of refractory hemodynamic instability. Nevertheless, the management of REBOA patients needs the expertise and the resources of tertiary referral trauma centers.
Availability of data and materials
The data and code that support the findings of this study are available from the corresponding author, upon reasonable request.
References
Kauvar DS, Wade CE. The epidemiology and modern management of traumatic hemorrhage: US and international perspectives. Crit Care. 2005;9:S1–9.
Kauvar DS, Lefering R, Wade CE. Impact of hemorrhage on trauma outcome: an overview of epidemiology, clinical presentations, and therapeutic considerations. J Trauma Inj Infect Crit Care. 2006;60:S3–11.
Rabinovici R, Bugaev N. Resuscitative thoracotomy: an update. Scand J Surg. 2014;103:112–9.
Frassini S, Gupta S, Granieri S, et al. Extraperitoneal packing in unstable blunt pelvic trauma: a single-center study. J Trauma Acute Care Surg. 2020;88:597–606.
Tötterman A, Madsen JE, Skaga NO, Røise O. Extraperitoneal pelvic packing: a salvage procedure to control massive traumatic pelvic hemorrhage. J Trauma Inj Infect Crit Care. 2007;62:843–52.
Brenner M, Hoehn M, Rasmussen TE. Endovascular therapy in trauma. Eur J Trauma Emerg Surg. 2014. https://doi.org/10.1007/s00068-014-0474-.
Moore LJ, Martin CD, Harvin JA, et al. Resuscitative endovascular balloon occlusion of the aorta for control of noncompressible truncal hemorrhage in the abdomen and pelvis. Am J Surg. 2016;212:1222–30.
Brenner M, Moore L, Dubose J, Scalea T. resuscitative endovascular balloon occlusion of the aorta (REBOA) for use in temporizing intra-abdominal and pelvic hemorrhage: physiologic sequelae and considerations. Shock. 2020;54:615–22.
Borger van der Burg BLS, van Dongen TTCF, Morrison JJ, et al. A systematic review and meta-analysis of the use of resuscitative endovascular balloon occlusion of the aorta in the management of major exsanguination. Eur J Trauma Emerg Surg. 2018;44:535–50.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097.
Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017. https://doi.org/10.1136/bmj.j4008.
Sterne JAC, Hernán MA, McAleenan A, et al. Assessing risk of bias in a non-randomized study. Cochrane Handb Syst Rev Interv. 2019;2:621–41.
Phillips B, Ball C, Sackett DL. Levels of Evidence and grades of recommendation. Oxf Cent Evid Based Med 1998; 2009.
Wells G, Shea B, O’Connell D, et al. The Newcastle–Ottawa scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. 2012. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014. https://doi.org/10.1186/1471-2288-14-135.
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Br Med J. 2003;327:557–60.
Team RC. R: a language and environment for statistical computing. Austria: Team RC; 2019.
Schwarzer G, Carpenter JR, Rücker G. An introduction to meta-analysis in R. Cham: Springer; 2015.
Viechtbauer W. Conducting meta-analyses in R with the metafor. J Stat Softw. 2010. https://doi.org/10.18637/jss.v036.i03.
McGrath S, Sohn H, Steele R, Benedetti A. Meta-analysis of the difference of medians. Biometr J. 2020;62:69–98.
Harrer M, Cuijpers P, Furukawa T., Ebert DD. Doing meta-analysis in R: a hands-on guide. Prot. Lab 2019.
Abe T, Uchida M, Nagata I, et al. Resuscitative endovascular balloon occlusion of the aorta versus aortic cross clamping among patients with critical trauma: a nationwide cohort study in Japan. Crit Care Critical Care. 2016;20:1–10.
Moore LJ, Brenner M, Kozar RA, et al. Implementation of resuscitative endovascular balloon occlusion of the aorta as an alternative to resuscitative thoracotomy for noncompressible truncal hemorrhage. J Trauma Acute Care Surg. 2015;79:523–32.
Duchesne J, Costantini TW, Khan M, et al. The effect of hemorrhage control adjuncts on outcome in severe pelvic fracture: a multi-institutional study. J Trauma Acute Care Surg. 2019;87:117–24.
Asmar S, Bible L, Chehab M, et al. Resuscitative endovascular balloon occlusion of the aorta vs pre-peritoneal packing in patients with pelvic fracture. J Am Coll Surgeons. 2021;232:17-26.e2.
Bukur M, Gorman E, DiMaggio C, et al. Temporal changes in REBOA utilization practices are associated with increased survival: an analysis of the AORTA registry. Shock. 2021;55:24–32.
Henry R, Matsushima K, Henry RN, et al. Validation of a novel clinical criteria to predict candidacy for aortic occlusion: an aortic occlusion for resuscitation in trauma and acute care surgery study. Am Surg. 2020;86:1418–23.
Mikdad S, van Erp IAM, El MM, et al. Pre-peritoneal pelvic packing for early hemorrhage control reduces mortality compared to resuscitative endovascular balloon occlusion of the aorta in severe blunt pelvic trauma patients: a nationwide analysis. Injury. 2020;51:1834–9.
Frassini S, Gupta S, Granieri S, et al. Emergency management of pelvic bleeding. J Clin Med. 2021;10:129.
Bulger EM, Perina DG, Qasim Z, et al. Clinical use of resuscitative endovascular balloon occlusion of the aorta (REBOA) in civilian trauma systems in the USA, 2019: a joint statement from the American College of Surgeons Committee on Trauma, the American College of Emergency Physicians, the National Association of Emergency Medical Services Physicians and the National Association of Emergency Medical Technicians. Trauma Surg Acute Care Open. 2019;4:e000376.
Borger van der Burg BLS, Kessel B, DuBose JJ, et al. Consensus on resuscitative endovascular balloon occlusion of the Aorta: a first consensus paper using a Delphi method. Injury. 2019;50:1186–91.
Coccolini F, Stahel PF, Montori G, et al. Pelvic trauma: WSES classification and guidelines. World J Emerg Surg. 2017;12(5):10–11. https://doi.org/10.1186/s13017-017-0117-6
Burlew CC, Moore EE, Stahel PF, et al. Preperitoneal pelvic packing reduces mortality in patients with life-threatening hemorrhage due to unstable pelvic fractures. J Trauma Acute Care Surg. 2017;82:233–42.
Romagnoli A, Teeter W, Pasley J, et al. Time to aortic occlusion: it’s all about access. J Trauma Acute Care Surg. 2017;83:1161–4.
Hilbert-Carius P, McGreevy D, Abu-Zidan FM, et al. Successfully REBOA performance: does medical specialty matter? International data from the ABOTrauma Registry. World J Emerg Surg. 2020. https://doi.org/10.1186/s13017-020-00342-z.
Reitano E, Granieri S, Frassini S, et al. Infectious complications of extra-peritoneal pelvic packing in emergency room. Updates Surg. 2021;73:331–7.
Elkbuli A, Kinslow K, Sen-Crowe B, et al. Outcomes of resuscitative endovascular balloon occlusion of the aorta (REBOA) utilization in trauma patients with and without traumatic brain injuries: A national analysis of the American College of Surgeons Trauma Quality Improvement Program data set. Surg (United States). 2021;170:284–90.
Abid M, Neff LP, Russo RM, et al. Reperfusion repercussions: A review of the metabolic derangements following resuscitative endovascular balloon occlusion of the aorta. J Trauma Acute Care Surg. 2020;89:S39–44.
Joseph B, Zeeshan M, Sakran JV, et al. Nationwide analysis of resuscitative endovascular balloon occlusion of the aorta in civilian trauma. JAMA Surg. 2019;154:500.
Manzano Nunez R, Naranjo MP, Foianini E, et al. A meta-analysis of resuscitative endovascular balloon occlusion of the aorta (REBOA) or open aortic cross-clamping by resuscitative thoracotomy in non-compressible torso hemorrhage patients. World J Emerg Surg. 2017. https://doi.org/10.1186/s13017-017-0142-5.
Ramenofsky M, Bell R. ATLS: advanced trauma life support 10th Edition. Advanced trauma life support-ATLS. 2018.
Funding
The authors have not received support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
SG, SF, and AB designed the study; SG collected data, performed statistical analysis, and drafted the manuscript; SF, AB and SP collected data and participated in drafting the manuscript; AC, LL, and FB participated in drafting the manuscript; RB drew the original artwork; SC, SDS, MK and CC supervised the study. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval and consent to participate
The present study is a systematic review of the literature and meta-analysis. Due to the retrospective nature of the study, a specific ethical approval was not deemed necessary.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Granieri, S., Frassini, S., Cimbanassi, S. et al. Impact of resuscitative endovascular balloon occlusion of the aorta (REBOA) in traumatic abdominal and pelvic exsanguination: a systematic review and meta-analysis. Eur J Trauma Emerg Surg 48, 3561–3574 (2022). https://doi.org/10.1007/s00068-022-01955-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-022-01955-6