Abstract
Purpose
There is relatively limited large scale, long-term unified evidence to describe how quality of life (QoL) and functional outcomes are affected after polytrauma. The aim of this study is to review validated measures available to assess QoL and functional outcomes and make recommendations on how best to assess patents after major trauma.
Methods
PubMed and EMBASE databases were interrogated to identify suitable patient-reported outcome measures (PROMs) for use in major trauma, and current practice in their use globally.
Results
Overall, 81 papers met the criteria for inclusion and evaluation. Data from these were synthesised. A full set of validated PROMs tools were identified for patients with polytrauma, as well as critique of current tools available, allowing us to evaluate practice and recommend specific outcome measures for patients following polytrauma, and system changes needed to embed this in routine practice moving forward.
Conclusion
To achieve optimal outcomes for patients with polytrauma, we will need to focus on what matters most to them, including their needs (and unmet needs). The use of appropriate PROMs allows evaluation and improvement in the care we can offer. Transformative effects have been noted in cases where they have been used to guide treatment, and if embedded as part of the wider system, it should lead to better overall outcomes. Accordingly, we have made recommendations to this effect. It is time to seize the day, bring these measures even further into our routine practice, and be part of shaping the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Background
There has been a paradigm shift in how ‘major trauma’ is managed in the United Kingdom (UK) since 2010, following the establishment of Major Trauma Centres (MTCs) and nationwide Trauma Networks to which the most severely injured patients are taken following their accidents. This has resulted in significantly improved survival rates [1]. However, while mortality in the UK has been improved, quantification of the associated morbidity and impact on quality of life (QoL) secondary to the severity of injuries sustained remains poorly understood. The few UK studies which have been done so far do not paint a rosy picture in terms of QoL outcomes [2,3,4].
In the modern healthcare setting, mortality alone is a crude measure of efficacy, and does not reflect the transformations made to a patient’s functional outcome and quality of life, which is of paramount importance to survivors of serious injury. Thus, we may be saving more lives, but could thereby be producing more long-term morbidity. It remains to be seen exactly how this translates to real long-term outcomes on a large scale for all-causes of polytrauma, which raises several pertinent questions to form the basis of regional, national and ultimately international strategies to identify and address any areas for improvement [5,6,7].
Currently in the UK, the Trauma Audit Research Network (TARN) collect broad-brush data using the Euroqol 5-Dimension (EQ-5D) and Glasgow Outcomes Score-Extended (GOSE) at baseline and 6 months with data fed back to individual hospitals and reported at a national level. From this, we know that despite improvements in survival, 61% of patients have a change in ability to work, and 38% of patients see a negative change to their level of independence [8].
The current situation however (data collection on a national level stopping after 6 months) limits the degree of information being captured. Moreover, the questionnaires used are relatively ‘blunt instruments’ with few specific questions. It is therefore difficult to know on a large, unified scale which symptoms patients suffer with most, what their specific care and rehabilitation needs are, and why. One could argue that we need a suitably focussed tool designed to run long-term, capturing both functional outcomes and rehabilitation needs, allowing a focus on patient need (and unmet needs) but also to enable pooling of these data to inform patient care more widely. Specifically, we refer to what post-operative physiotherapy and occupational therapy requirements, including equipment and home adaptions, and basic care needs, as well as what increased medical and emotional support is required to allow a normal return to living, socialisation and work. Without this, it will be difficult to direct rehabilitation where it is needed most or plan bespoke therapy, dependent on predicted need.
Efforts were made to assess and address this by the National Clinical Audit for Specialist Rehabilitation following major Injury (NCASRI), but results reported in 2019 show there is significant room for improvement in identifying patient needs and recording this on a suitable central platform, despite the requirement for all patients to be issued with a ‘rehabilitation prescription’ following discharge [9].
Exploring how quality of life (QoL) and functional outcomes have been defined and measured in the context of trauma is important to understand. The World Health Organisation (WHO) defines health as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” [10] and quality of life as how an individual perceives their position in life in relation to their goals, expectations, standards and concerns set in the context of the culture and value systems in which they live [11]. Functional status (and outcomes) can refer to both physical and mental health as well as social condition [12]. The International Classification of Function, Disability and Health (ICF), developed by the WHO adopts a ‘biopsychosocial’ approach, and broadly defines health in terms of body functions, activities and participation, and environmental facilitators or barriers which ultimately divide into 1400 ‘health concepts’ [13]. It should be noted that ‘activity’ is defined as specific actions and tasks executed, whilst ‘participation’ is involvement in the life events made possible by those actions [14, 15], Fig. 1 [16]. ‘Health Status’ is the impact of disease on patient function as reported by the patient [17].
Biopsychosocial model of the ICF classification system [16]
With regards to what to measure, the 1991 Meran Consensus conference on QoL after surgery recommended that we should view QoL in this context through four domains: physical state, psychological wellbeing, social relations, and functional capacity [18]. The 1999 QoL after Multiple Trauma conference further expanded on this, indicating that brief general outcome measures such as the Glasgow Outcome Score (GOS), and Euroqol 5-Dimension score (EQ-5D), as well as a more detailed general measure such as the Medical Outcomes Study Short Form 36 (SF-36) should be used as a minimum [18]. It was evident however, that a trauma-specific questionnaire was lacking. Noteworthily, large-scale PROMs collection after major trauma has been routine in various countries since the 1990’s [5, 13, 18,19,20,21,22,23].
However, choice of an appropriate ‘preferred’ PROMs tool for use in polytrauma patients remains a challenge. When considering which PROMs measure to use for patients with multiple injuries, one must be aware of both the breadth and depth of the measures being used. One must also understand the relative sensitivity and specificity of the questionnaire tools to assess particular areas of function, according to their relative ‘minimally clinically important difference’ (MCID) levels. A particular challenge is using a measure which avoids ‘floor and ceiling’ effects—whereby outcomes are polarised, impairing nuanced diagnosis or decision-making based on results. Furthermore, especially given the diverse nature of major trauma (polytrauma), one must be sure that the questionnaires (PROMs) used are sufficiently validated for the target population, providing a reliable result which can be used to guide management. It should also be relatively brief to reduce burden and improve uptake. In essence, a balance must be struck between conciseness and completeness [5, 13, 18,19,20,21,22,23,24,25].
Interestingly, since 2009 PROMS have been collected (centrally) in the UK NHS from surgical patients (hip, knee replacement, groin and varicose vein surgery) [26]. With healthcare increasingly becoming more personalised, PROMS have been shown to have a significantly transformative effect on both an individual and aggregate level outcomes when data is linked to direct care [27]. Indeed, the use of PROMS in clinical practice has been shown to improve patient and clinician communication, medical decision making and the process and outcomes of clinical care [28,29,30].
The aim of this narrative review was to evaluate what patient-reported outcome measures (PROMs) have been used most frequently their quality, applicability to trauma, their overall usefulness, and advice on how to use them. In addition, we aimed to use these findings as a basis for suitable recommendations of which measures to use in patients having sustained polytrauma, and how to improve the current systems we use.
Materials and methods
We set out to ascertain as much information as we could on the most commonly used PROMs across all body areas, especially those in trauma, and critique of these measures. Searches were performed using OvidSP interrogating EMBASE and EMBASEClassic, OVID Medline and Epub Ahead of Print, In-Process & Other non-indexed Citations and daily, as well as Google Scholar. Inclusion criteria and search terms for paper selection were wide (all papers which covered PROMs used in trauma, and in specific anatomical locations, and any relevant guidelines or recommendations currently available). We used combinations of the relevant terms to obtain the fullest picture of the most widely used patient-reported outcome measures and their utility. These terms included: [PROM(s), Patient reported outcome(s)/measures, (functional) outcome(s), quality of life, trauma, major trauma, polytrauma, UK, Europe, USA, Global, guideline(s), recommendation(s)]. For the specific body regions, the following terms were combined with these, to search for which PROMs measures were in use for specific anatomical areas: [head, thorax, chest, abdomen, spine, pelvis, upper limb, lower limb].
All papers were screened by title and abstract, with those in the English language relevant to our review included, and their bibliographies were further searched for references. Such details were extracted from the papers that met the inclusion criteria as: which measures were used mostly in cases of polytrauma, their utility, and practicality. A summary table was made of a range of PROMs measures based on these findings. Papers which did not cover these aspects of inclusion criteria (PROMs used for trauma) and those not in the English Language were excluded.
Results
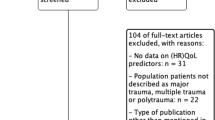
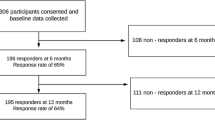
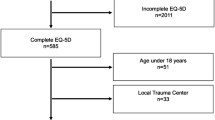
Overall, out of 672 papers identified for the initial screening process, 81 met the inclusion criteria and form the basis of the subsequent analysis [2, 5, 6, 9, 13, 15, 18,19,20,21,22, 31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100].
-
i.
PROMs utilised in polytrauma
There has been a proliferation of both generic and specific measurement tools for most conditions but relatively little work on specific PROMs for multiply injured patients with polytrauma [5, 13]. This has led to widespread discrepancy between PROMs selected to evaluate the recovery of trauma patients. A recent scoping review looking at 7,132 original articles between 1985–2015 found that over 100 different measures were used to assess outcome, with the SF-36 being most predominant (36%), followed by the EQ-5D (15%) and trauma-specific outcome measures in less than 5% [31]. In addition, a systematic review looking at PROMs used in 34 studies which included some 10 Polytrauma patients in their sample found that 38 different measures were in regular used [9] When mapping ICF (International Classification of Functioning, Disease and Health) categories covered by the most widely used PROMs measures, only a fraction (6%) of health categories were covered, and only one measure (TOP) covered environmental factors (4/74 subcategories) which are essential in assessing obstacles to ‘participation’ [13]. We have summarised some of the more common measures used with the aim to evaluate general, validated measures that could be applied to cases of polytrauma, including head, thoracic and abdominal injuries, as opposed to the many musculoskeletal and joint-specific scoring systems, Tables 1, 2 [2, 5, 6, 9, 13, 15, 18,19,20,21,22, 31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78].
-
ii.
Evaluation of disability/rehabilitation
The Glasgow Outcome Scale was originally devised as a 5-level measure to assess patients with traumatic brain injury (TBI). Due to concerns that it lacked sensitivity to detect small changes, a further 3 levels were added, thus improving sensitivity and allowing for a more complete measurement of outcome [32]. Outcomes range as follows: death, vegetative state, lower–upper severe and moderate disability, lower and upper ‘good’ recovery. Although initially designed for TBI, it has gained widespread use as a simple measure of overall outcome after injury, including polytrauma, although this has resulted in ceiling effects where TBI is not the primary pathology [6, 20, 32, 33]. It has been reliably completed away from the hospital setting by post by non-clinicians [87] and has been used in the Victorian State Trauma Registry in Australia since 2000, for 24 months follow-up [6, 20], and similarly utilised in the national German Trauma Registry since 1993 [18, 34], with recommendations from a Department of Health expert consensus meeting to use it for all major trauma patient follow-up to at least 6 months [6].
The Barthel Index is one of the earliest measures of activities of daily living, originally developed in 1965 for those with neurological impairment, and updated versions are still widely used for all types of patients. It consists of 10 items covering feeding, transfers, walking, toileting, continence and personal care. It has been widely used and considered a reliable measure of functional ability. Given its narrow scope however, it may not detect low levels of functional dysfunction e.g. even if the maximal score is obtained, one may still need help with more complex tasks such as shopping. These inherent floor and ceiling effects led to the development of the Functional Independence Measure (FIM) [35,36,37]. The FIM was designed in the United States as a means to calculate remuneration for rehabilitation and care provision. It was based on the level of disability, focussing on the burden of care and how much extra assistance they need for their usual activities of daily living. Patients are scored based on the judgement of a trained ‘observer’, whether this be a clinician or a lay-person, with clinical notes or an interview with the patient used to inform scoring [35]. This was adapted for use in the United Kingdom, and the same group also adapted the US functional assessment measure (FAM) for use in assessing patients with brain or neurological injury, which must only be used in conjunction with the FIM; both have been widely used and validated [38]. A Barthel index can also be derived from the FIM should this be required for comparison [37]. Indeed, national UK audit standards require patients who have experienced polytrauma to have made some progress as measured by the FIM ± FAM (or similar) tools prior to discharge [9].
-
iii.
Evaluation of quality of Life and function
-
(a)
General measures:
The Medical Outcomes Study Short Form-36 (SF-36) is the most commonly used PROM in trauma [13, 31]. It has been widely validated across different countries [39, 40]. It aims to capture wide-ranging information on performance, and to compare these to ‘population norms’. It measures 8 ‘dimensions’ with 36 items—physical functioning, role limitations—physical, bodily pain, social functioning, mental health, role limitations—emotional, vitality, general health perceptions; from these one can calculate physical and mental component scores [35]. The scoring mechanism also matches that of the SF-12, allowing comparison of results [5]. The SF-12 is an abbreviated 12 item version of the SF-36, enabling equivalent information to be gleaned on the same 8 domains whilst reducing patient burden. Both measures, however, lack detailed coordinated questions concerning cognitive function and distress, or activities of daily living such as cooking, and questions about the patient’s environment (See ICF definition) [13, 15, 35]. Both were updated to reduce floor and ceiling effects, and make them more consistent with each other, as well as producing a ‘British’ English version [35]. The updated versions are also proprietary, require a fee to use, and an obligation to use computer software to interpret the results—a manual with complete interpretation instructions is no longer provided. However, a free to use version of these measures, (based on the original versions), is available via RAND Healthcare’s website, but is more liable to floor and ceiling effects, and therefore less sensitive in assessing change [42].
The Euroqol 5-Dimensions (EQ-5D) score is the second-most widely used PROMs measure in trauma [5, 31, 35, 43]. It contains 5 items with a 5-level (5L) response scale; originally, this was developed as a 3-level (3L) scale, which has since been updated to reduce floor and ceiling effects. It covers 5 dimensions: mobility, self-care, usual activities, pain/discomfort, anxiety/depression, as well as a visual analogue scale (VAS) asking patients to grade their general health state from 0–100. It is quick to complete, provides a good snapshot of function, and also allows for calculation of Quality Adjusted Life Years (QALYs) to assess the relative economic benefit of interventions [5, 31, 35, 43]. It is widely used and validated with normative values having multiple translations. It is free to use, and valid for all groups of patients, with a paediatric version also available. By its nature, however, it is very brief, and it is recommended for a greater depth of coverage and to ensure the nature of meaningful change is detected the EQ5D should be used in conjunction with additional PROMs [5, 31, 35, 43].
The WHO Disability Assessment Schedule 2.0 (WHO-DAS 2.0) updated the previous WHO-DAS II in 2010, and comes as both 12 and 36 item versions. For each of the following dimensions using a 5-point response scale it explores: understanding and communicating, getting around, self-care, getting along with people, life activities—household, life activities—school/work, participation in society. It covers a broad range of health concepts and is easy to complete. It is directly linked to ICF, covering specific points on ‘participation’ and barriers. It is widely used, validated and translated internationally with normative values, and free to use for all. Despite this, however, its use remains less ubiquitous than the more established SF-36, and it also lacks questions concerning the patient’s environment which would otherwise help add context [5, 13, 35, 41].
The Short Musculoskeletal Function Assessment (SMFA) questionnaire is also widely used and validated and is a useful tool for routine assessment. It consists of 46 items overall, 34 for the dysfunction index and 12 for the bother index, with all item responses graded 1–5. It assesses all areas of musculoskeletal function/performance, and how much patients are bothered by their symptoms in: recreation, leisure, sleep/rest, work, and family, and offers a very good overall system for scoring upper and lower limb and spine function in one PROM [88]. There has been some concern around reliability of the classification of the extremity dysfunction and mental and emotional problem subscales, which may yield unreliable results, and as such minimally important change values must be interpreted with caution [44, 45].
The Trauma Outcome Profile (TOP) was developed in Germany in 2001 in response to the argument that tools specifically designed for patients with major trauma have been lacking for many years [21]. Its strengths include the way it was designed, by gathering opinions on what most affected major trauma patients, and views of healthcare staff on what was important to measure. This resulted in a 64-item form, covering 4 domains identified by the Meran consensus (physical state-pain; psycho-social wellbeing-depression, anxiety, PTSD, social interaction; functional capacity—physical functioning, daily activities, mental functioning), as well as body image and overall satisfaction with health status. The tool includes 10-item response Likert scales for patients to state their pre and post injury pain levels in a full range of anatomical locations from head to feet, and the level of restriction experienced. It is used along with the EQ-5D and SF-36 as part of the POLO (Polytrauma Outcomes) assessment for all patients in the German Trauma Registry. A copy of the POLO instruction booklet can be obtained from the research group free of charge. It is increasingly used in studies as a general assessment of functional outcome after trauma [2, 13, 18, 19, 21] and covers a wide spectrum of ICF categories, including patient environment, as well as covering aspects of cognition, but its thoroughness makes it very lengthy, which some patients may find burdensome [13, 18, 46, 47].
More recently in 2015, the Trauma Quality of Life (TQoL) form was developed in a similar way to the TOP. It includes 43 items divided into 5 components (emotional well-being, functional engagement, recovery/resilience, peri-traumatic experience, physical wellbeing). It has been recently validated [89], and is among measures considered by the American College of Surgeons for patients with major trauma. However, it is less specific and detailed than the TOP with regards to which anatomical body areas cause morbidity, but still a useful measure, and free to use [5, 48].
The Patient-Reported Outcomes Measurement Information System (PROMIS) and NeuroQoL systems were first validated in 2007. They allow for tailored measures of mental, physical, social, neurological and overall global health. They are available in both paper and electronic forms and can potentially be integrated into the electronic health record. Tailored infrastructure is needed for this and their integration is dependent on which EPR (electronic patient record) system is being used [5, 49].
-
(b)
Body region-specific physical functional measures
There is currently a relative vacuum for trauma-specific PROMs measures for the chest and abdomen. Database searching yields no specific tools which have been validated for use in trauma. The Gastro-Intestinal Quality of Life Index (GIQLI), is widely used in GI surgery to assess outcomes following elective surgery, and has recently been validated for use after emergency laparotomy. However, trauma cases were excluded from this study, therefore caution should be used when interpreting results [50, 51]. No PROMs exist or have been validated for use after chest trauma, however a team in Nottingham (UK) are currently aiming to design one [52]. The majority of studies which have looked at chest trauma use various generic measures, such as the EQ5D and SF-36 [53, 54].
There are numerous joint-specific PROMs, which have been well-validated to assess specific function. In the context of recommending more generic measures to use in polytrauma however, we have sought to review and recommend those which can be most useful and adaptable to varying injury profiles whilst minimising questionnaire burden [55,56,57,58,59,60,61,62,63,64, 82].
For the upper limb, the Disabilities of the Arm, Shoulder and Hand (DASH) measure, is a good ‘catch-all’. It consists of 11 (QuickDASH) or 30 (Full DASH) items with a 5-point response scale. There are optional extra modules for effect of injury on playing a musical instrument/high performance sport, and work: 4 items each, same response scales. It compares very well against joint-specific PROMs measures, and is free to use [55,56,57].
The AAOS Lower Limb Core scale consists of 7 items with various response scales, with domains covering pain, stiffness, swelling, and function. It is a widely used and validated, very brief screening measure which has good reliability and comparable to values of more extensive PROMs and is free to use, but for many will not be detailed enough [58, 59]. A variation focussing on knees, and ‘modules’ which can link into the ‘core’ scale include those focussed on the ‘Foot and Ankle’ and ‘Sports/Knee’ which can be used to supplement results [58].
The Lower Extremity Function Scale (LEFS) contains 20 items with 4-point response scales: it measures physical status and is mapped to the mobility section of ICF’s ‘activity and participation’ chapter. It is widely used and validated, applicable to all lower limb injuries. It is more sensitive to change and lower-functioning patients than the SF-36, and designed to map to ICF criteria, with specific patient input in its design process and is free to use. It may need to be supplemented with a joint or region-specific PROM, but should cover most lower limb issues, including those involving the pelvis [60,61,62,63,64, 82].
Functional outcomes after pelvic injury, however, must be considered from a multifaceted viewpoint given its central location. Patients may complain of lower back, abdominal, sexual, genito-urinary and lower limb dysfunction [79]. Various measures have been designed to assess pelvic function. The most widely used is the Majeed pelvic score, a short tool assessing five areas with varying response scales (pain, work, sitting, sexual intercourse and standing which is broken down into needing walking aids, gait unaided, and walking distance) (Table 2) [82,83,84]. The Iowa Pelvic Score has also been commonly used. However, it also has high ceiling effects and has not been widely validated (Table 2) [80,81,82,83,84]. There have been numerous other measures developed to assess pelvic outcomes, which include the Orlando pelvic score (used only once, combining radiological and clinical outcomes). These have been validated in one relatively small study of 38 patients in which scores correlated well against the physical component score of SF-36 and the SMFA, but all demonstrated high ceiling effects [80,81,82,83,84]. Efforts to remedy problems noted with these measures is ongoing, including the development of the Pelvic Discomfort Index by Borg et al. in 2015, a 6 item questionnaire (pain, walking, and hip motion peripheral neurology, sexual life, and operation scar) which was validated against the SF-36 with which it showed moderate correlation in a study of 73 patients, but has not been subsequently validated elsewhere more thoroughly [85].
There have been various PROMs for patients with spinal problems, however the most widely used specific measure is the Oswestry Disability Index 2.1 (ODI 2.1), originally developed for lower back pain [75, 76]. It has also been used extensively in studies examining lumbo-pelvic and sacro-iliac joint pain and surgery [90,91,92]. For patients with cervical spine pathology, the Neck Disability Index (NDI is widely recommended as the most useful specific PROMs measure, which was developed from the ODI [75, 76]. Both consist of 10 items, with a 6-point response scale for each item, and multiple studies have found them to have excellent reliability, internal consistency and construct validity, as well as test–retest reliability, although there have been some concerns about floor and ceiling effects [75, 76]. Criticism has been levelled at these though, due to the large amount of crossover of questions and lack of distinguishing specific questions for each spinal region, and there have been recent efforts to combine them into one: the Total Disability Index (TDI), which consists of 14 items which has recently been validated. The scoring is strongly correlated with the ODI and NDI, and a transformed score based on these created from responses [77, 78].
-
(c)
Mental health status measures for trauma
The Beck Depression Inventory-II (BDI-II) is a 21-item form, with varying response scales covering: emotion (15 items), behavioural changes (4 items), and somatic issues (6 items). It is widely used and validated as a screening measure. Beck emphasised both the cognitive and somatic symptoms, with questions covering areas including sleep, appetite and energy [2, 13, 22, 35]. Although used in many trauma studies, the somatic elements cross over with normal symptoms experienced because of injury or pain, and could confound results. It is also proprietary, and a fee required for the licence.
The Hospital Anxiety and Depression Scale (HADS) is a 14-item form, with 4 point response scales: 7 for depression and 7 for anxiety. It is widely used and has also been validated for use in trauma patients. As opposed to the BDI-II, it does not ask about any confounding cognitive or somatic symptoms of depression which may be due to injuries. It was designed to indicate ‘caseness’ of depression/anxiety however, and therefore cannot be used to grade severity, which must be borne in mind on interpretation. Unless working in certain institutions, there is a licence fee for use of HADS [13, 35, 65, 66].
The CORE-10 questionnaire is a 10-item form, generated from the longer 34 item (CORE-OM “outcome measure”), with the following domains covered: Depression, Anxiety, Functioning in general and in relationships, Traumatic images/memories, Physical—sleep, and Risk—suicidal ideation, which may be particularly useful for polytrauma patients. It provides equivalent information to the CORE-OM, has proven validity, is free to use, and is an excellent reliable measure to indicate level of psychological distress, and uses various cut-points to screen for depression and anxiety [67]. The CORE-OM is an excellent tool to assess general psychological disturbance in greater detail should this be required [67].
The Impact of Events Scale-Revised (IES-R) is a 22-item form with 3 response options: Intrusion, Avoidance, Hyperarousal. It has been widely used and validated as an excellent screening tool for presence of PTSD according to 3 of 4 DSM-4 criteria clusters (now superseded by DSM-5), and assess severity & progress of symptoms, and is free to use. It is especially good at identifying intrusion phenomena, but best for recent events rather than those in the distant past [68,69,70]. It focuses more on active avoidance rather than emotional numbing, and is not fully diagnostic of PTSD, other measures should be used to supplement full diagnosis, especially as the criteria to diagnose PTSD have changed since it was created [68, 69]. We felt it important to mention the IESR given its common use. The more updated PTSD Check-List for DSM-5 (PCL-5), however, provides the optimal solution. It contains 20 items with 4 response options for the more recent DSM-5 criteria symptom clusters: Intrusions, Avoidance, Negative alterations in cognitions and mood, Alterations in arousal and reactivity. It provides an excellent screening of PTSD against DSM-5 criteria, and high sensitivity to clinical change when compared with a full detailed interview and has better overall consistency than IES-R when diagnosing PTSD on either DSM-4 or DSM-5 criteria. It has been widely used and validated and is free to use [70, 71]. As for the IES-R, the PCL-5 is only able to screen for likely cases of PTSD, but is useful for assessing treatment progress. A tool such as the 30-item Clinician-Administered PTSD Scale-5 (CAPS-5) should always be used to establish formal diagnosis [68,69,70,71].
Discussion
As the value of patient-centred care is being increasingly recognised globally, the use of PROMs are becoming more widespread, however their use in major trauma remains sporadic depending on region. In the UK, calls to progress with routine PROMs where possible, were embedded in the Darzi report into modernising healthcare in 2008 [72], and have since been written into domain 4 of the Major Trauma Centre standard contract and similarly included in a consensus meeting considering major trauma management at the department of health; despite this there has been variable uptake of their use [6, 73]. Interestingly, regular PROMs assessment has been routine practice on continental Europe for some time, particularly in Germany where the majority of this research has taken place [13, 18, 19, 21, 22, 93,94,95], as well as in Australia [20]. Demand is also growing on an international level to investigate and follow-up on quality of life and functional outcome data more closely and long-term, with the American College of Surgeons recently holding a large consensus conference on the subject [5]
On a practical local level, PROMs can be used to guide follow-up; their scores are already being used as a means of deciding who needs telephone or face to face follow-up [96, 97]. Nonetheless, we must remain sensitive to the patient’s psychological need to see their doctor/surgeon in person, not underestimating the benefit and peace of mind obtained from the doctor-patient transaction, and not seek to supplant this important personal experience with mute questionnaires [98]. Overall, we must ensure to implement PROMs into our routine practice in a way which makes patients feel they have a voice, thereby improving their self-esteem and enabling more ownership of their care: when patients are more ‘activated’, it has been shown to improve outcomes [74].
Moving forwards, it would be sensible to recommend that all patients who attend with major trauma are followed up with non-proprietary outcome measures for at least 5 years after their injuries and plan to do this evaluation for at least 10 years where possible, Table 3. At every timepoint, patients must also be asked about ‘unmet need’—to identify areas where systems may be lacking, helping to engender improvement and better outcomes. In this way, we will be able to uncover the ‘unknown unknowns’ and in time, learn to pre-empt them. Without this knowledge or being able to link unmet needs to measure outcome, we cannot fully provide what our patients need in a modern twenty-first century healthcare setting.
Prior to discharge, we recommend a baseline set of outcome measures: FIM ± FAM, GOS-E, EQ-5D, WHODAS 2.0 (One could instead use SF-36 version 1, accepting potential ceiling and floor effects or SF-36 version 2 if funds are available for the licence), and/or Trauma Outcome Profile to capture general outcomes (these have similar questions, one could potentially use either, to reduce burden if desirable); and the CORE-10 to capture and grade psychological function/pathology, although given the item-construct the HADS may suit individual units better as a brief screening tool to indicate caseness of anxiety/depression and prompt further enquiry with the CORE-OM. This will allow for a full assessment of rehabilitation needs to enable planning of supplementary care, and act as a reference point moving forwards. If the therapy team feel that no further assessment with the FIM ± FAM is needed at any point, this can be removed based on clinical need. Otherwise, all evaluation measures should then be repeated at 6, 12, 18, and 24 months, and thereafter annually. At any point, if they trigger on the scoring system that patients are in difficulty, then a system should be in place for providing follow-up including systems to enable score interpretation, and decisions on which health care professionals will receive scores and outputs. Follow up on flagged problems may require use of the more specific PROMs measures discussed. We would however implore clinicians to consider questionnaire burden and limit too many specific PROMs measures, bearing in mind the crossover (and repetition) of information gained from the different measures. [99].
If a specific measure for PTSD is required, we recommend the PCL-5. If a more thorough assessment of anxiety/depression and response to treatment is needed, we recommend the complete CORE-OM measure which is validated and free to use and importantly does not include too many somatic variables for trauma patients. [100].
For follow-up of limb-specific issues we recommend the DASH for upper limb, and LEFS for lower limb in general. For pelvis-specific follow-up, it is difficult to make any specific recommendation as there has been limited validation of any of the measures which exist; the LEFS could be considered for the mechanical aspect of pelvis injury follow-up but has not been formally validated for use in pelvic ring injuries, although does provide a wide-ranging assessment of lower limb function. The Majeed, Iowa and Pelvic Discomfort measures have limited validation, although the Majeed score has been the most widely used pelvis-specific so far. Interestingly however the SF-36 and SMFA are the widest-used measures for pelvis overall [82, 83, 86]. We would therefore recommend individual assessment of these measures and support utilisation of what would work best for different centres, rather than being prescriptive. For spinal injury follow-up, we recommend the TDI if there are multi-level spinal injuries, but as it has not yet been widely validated and if the patient has regional-specific spine injury, we recommend the ODI or NDI.
Finally, throughout the patient’s journey, they should also be formally asked, using a PROM, if they have any unmet needs which may not be obvious to the clinical team, and which they may not discuss otherwise. These PROMs could be locally designed according to services available. Also, it would make sense that all PROMs measures should be uploaded electronically to a national trauma database (such as the TARN) if it exists, to allow for centralised pooling of data for research and innovation.
Evaluation of patient recovery and outcome following polytrauma remains problematic. Herein, we have only recommended a minimum set of PROMs measures according to what currently exists and has been widely validated. The plethora of new PROMs which can be tailored to need, such as the PROMIS system unlocks a treasure trove of opportunity to tailor-design outcome measures to suit almost any purpose for free. Health informatics systems within hospitals are growing ever stronger, and soon in-house designed accessible PROMs measures will be part of our lives. Whilst many individual, tailor-made PROMs measures could be designed, it is important not to work in silos, but use the opportunity to engender communication between teams from different hospitals, and work to implement a national system capable of centrally recording outcome measures, driven by patient need (ideally the same ‘minimum’ data set for all major trauma patients) to allow for large-scale learning for service and care-delivery improvement.
Conclusion
It is clear that measures of global functional outcomes following major trauma are critical for optimal care and have shown benefit: they should be used to help guide and target treatment and follow-up moving forwards. Following our review, we have made recommendations on which specific PROMs measures we feel should be used following polytrauma, which may differ depending on need. Further work and research is needed to assess functional outcomes and unmet needs of patients following major trauma, to assess impact on quality of life and how we can best address their problems, to help patients re-integrate into society and live the fullest life possible. It would seem pertinent in the current climate of patient-centred care that we seize the day, implement positive PROMs change and be part of creating the future.
References
Moran C, et al. Changing the system—major trauma patients and their outcomes in the NHS (England) 2008–17 EClinicalMedicine. The Lancet. 2018. https://doi.org/10.1016/j.eclinm.2018.07.001.
Spreadborough S, et al. A study of outcomes of patients treated at a UK major trauma centre for moderate or severe injuries one to three years after injury. Clin Rehabil. 2018;32(3):410–8.
Folkard SS, et al. Factors affecting planned return to work after trauma: a prospective descriptive qualitative and quantitative study. Injury. 2016;47(12):2664–70.
Sutherland AG, et al. The mind continues to matter: psychologic and physical recovery 5 years after musculoskeletal trauma. J Orthop Trauma. 2011;25(4):228–32. https://doi.org/10.1097/BOT.0b013e3181ee40a9.
Sakran JV, et al. Proceedings from the consensus conference on trauma patient-reported outcome measures. J Am Coll Surg. 2020;230(5):819–35.
Ardolino A, Sleat G, Willett K. Outcome measurements in major trauma—Results of a consensus meeting. Injury. 2012;43(10):1662–6.
Retzer A, et al. Electronic patient reported outcomes to support care of patients with traumatic brain injury: priority study qualitative protocol. BMJ Open. 2019;9(1):
TARN. Measuring Trauma Outcomes. 2020 [cited 2020 07/09/2020]; Trauma Audit Research Network PROMs data]. Available from: https://www.tarn.ac.uk/content/downloads/19/3.%20Measure%20Trauma%20outcomes%202020.pdf.
Turner-Stokes L, NCASRI. Final report of the National Clinical Audit of Specialist Rehabilitation following major Injury. NCASRI: Northwick Park Hospital: London; 2019.
WHO. Basic Documents: WHO Constitution. Vol. 49. Geneva:Switzerland;2020
WHO. WHOQOL User Manual. Department of Mental Health, World Health Organization, 1211 Geneva 27, Switzerland: World Health Authority;1998
Frattali CM. Assessing functional outcomes: an overview. Semin Speech Lang. 1998;19(3):209–20.
Hoffman K, et al. Health outcome after major trauma: What are we measuring? PLoS ONE. 2014;9(7):2014.
Piskur B, et al. Participation and social participation: are they distinct concepts? Clin Rehabil. 2014;28(3):211–20.
WHO, World Health Organization. How to use the ICF: A practical manual for using the international classification of functioning, disability and health (ICF). exposure draft for comment. October, Geneva: WHO, Switzerland: World Health Authority;2013
WHO. Towards a common language for functioning, disability and health: the international classification of functioning, disability and health - beginner's guide. W.H. Organization ed. World Health Organisation:Geneva;2002
Rumsfeld JS. Health status and clinical practice: when will they meet? Circulation. 2002;106(1):5–7.
Pirente N, et al. Quality of life in multiply injured patients: Development of the Trauma Outcome Profile (TOP) as part of the modular Polytrauma Outcome (POLO) Chart. Eur J Trauma. 2006;32(1):44–62.
Kaske S, et al. Quality of life two years after severe trauma: A single centre evaluation. Injury. 2014;45(Supplement3):S100–5.
Gabbe. Victorian State Trauma Registry. 2020. https://www2.health.vic.gov.au/hospitals-and-health-services/patient-care/acute-care/state-trauma-system/state-trauma-registry.
Attenberger C, Amsler F, Gross T. Clinical evaluation of the Trauma Outcome Profile (TOP) in the longer-term follow-up of polytrauma patients. Injury. 2012;43(9):1566–74.
Zwingmann J, et al. Lower health-related quality of life in polytrauma patients long-term follow-up after over 5 years. Medicine. 2016;95(19):2016.
Hoffman KP, et al. Minimum data set to measure rehabilitation needs and health outcome after major trauma: application of an international framework. Eur J Phys Rehabil Med. 2016;52(3):331–46.
Turner GM, et al. An introduction to patient-reported outcome measures (PROMs) in trauma. J Trauma Acute Care Surg. 2019;86(2):314–20.
McMullan C, et al. Care providers’ and patients’ attitudes toward using electronic-patient reported outcomes to support patients with traumatic brain injury: a qualitative study (PRiORiTy). Brain Inj. 2020;34(6):723–31.
NHS. NHS Digital: Background information about PROMs. 2019. Available from: https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/patient-reported-outcome-measures-proms/background-information-about-proms. Accessed 1 Oct 2019.
Marshall S, Haywood K, Fitzpatrick R. Impact of patient-reported outcome measures on routine practice: a structured review. J Eval Clin Pract. 2006;12(5):559–68.
Greenhalgh J, Meadows K. The effectiveness of the use of patient-based measures of health in routine practice in improving the process and outcomes of patient care: a literature review. J Eval Clin Pract. 1999;5(4):401–16.
Velikova G, et al. Measuring quality of life in routine oncology practice improves communication and patient well-being: a randomized controlled trial. J Clin Oncol. 2004;22(4):714–24.
Espallargues M, Valderas JM, Alonso J. Provision of feedback on perceived health status to health care professionals: a systematic review of its impact. Med Care. 2000;38(2):175–86.
Rosenberg GM, et al. Patient-reported outcomes in trauma: a scoping study of published research. Trauma Surg Acute Care Open. 2018;3(1):0002021.
Weir J, et al. Does the extended glasgow outcome scale add value to the conventional glasgow outcome Scale? J Neurotrauma. 2012;29(1):53–8.
McMillan T, et al. The glasgow outcome scale — 40 years of application and refinement. Nat Rev Neurol. 2016;12(8):477–85.
Lefering R, et al. Update of the trauma risk adjustment model of the TraumaRegister DGUTM: the Revised Injury Severity Classification, version II. Critical care (London, England). 2014;18(5):476–476.
McDowell I, Measuring Health: A Guide to Rating Scales and Questionnaires. Third Edition, , editors. Oxford. Oxford University Press: UK; 2006. p. 765.
Mayoral AP, et al. The use of Barthel index for the assessment of the functional recovery after osteoporotic hip fracture: One year follow-up. PLoS ONE. 2019;14(2):e0212000.
Nyein K, McMichael L, Turner-Stokes L. Can a Barthel score be derived from the FIM? Clin Rehabil. 1999;13(1):56–63.
Turner-Stokes L, Siegert RJ. A comprehensive psychometric evaluation of the UK FIM + FAM. Disabil Rehabil. 2013;35(22):1885–95.
Li L, Wang HM, Shen Y. Chinese SF-36 Health Survey: translation, cultural adaptation, validation, and normalisation. J Epidemiol Community Health. 2003;57(4):259–63.
Montazeri A, et al. The Short Form Health Survey (SF-36): translation and validation study of the Iranian version. Qual Life Res. 2005;14(3):875–82.
Üstün T, et al. ManualforWHODisabilityAssessmentSchedule: WHODAS 2.0. Geneva: World Health Organisation; 2010.
RAND-Healthcare. RAND 36-Item Short Form Survey (SF-36)—Version 1. 2020. https://www.rand.org/health-care/surveys_tools/mos/36-item-short-form.html. Accessed 10 Feb 2020.
Payakachat N, Ali MM, Tilford JM. Can the EQ-5D detect meaningful change? A Systematic Review Pharmacoeconomics. 2015;33(11):1137–54.
de Graaf MW, et al. Minimal important change in physical function in trauma patients: a study using the short musculoskeletal function assessment. Qual Life Res. 2020;29(8):2231–9.
Ponzer S, Skoog A, Bergström G. The Short Musculoskeletal Function Assessment Questionnaire (SMFA): cross-cultural adaptation, validity, reliability and responsiveness of the Swedish SMFA (SMFA-Swe). Acta Orthop Scand. 2003;74(6):756–63.
Attenberger C, Amsler F, Gross T. Clinical evaluation of the Trauma Outcome Profile (TOP) in the longer-term follow-up of polytrauma patients. Injury. 1566;43(9):1566–74.
Hamid K, et al. Orthopedic trauma and recovery of quality of life: an overview of the literature. Clinical Medicine Insights. 2016;7:1–8.
Kuorikoski J, et al. Finnish translation and external validation of the trauma quality of life questionnaire. Disabil Rehabil. 2020;2020:1–7.
DeWalt DA, et al. Evaluation of item candidates: the PROMIS qualitative item review. Med Care. 2007;45(5 Suppl 1):S12–21.
Eypasch E, et al. The Gastrointestinal Quality of Life Index. A clinical index for measuring patient status in gastroenterologic surgery. Der Chirurg; Zeitschrift für alle Gebiete der operativen Medizen. 1993;64:264–74.
Kwong E, et al. Feasibility of collecting and assessing patient-reported outcomes for emergency admissions: laparotomy for gastrointestinal conditions. BMJ Open Gastroenterol. 2018;5(1):e000238–e000238.
OTG. OCTS: Outcomes after chest trauma score - Key facts. 2020. Available from: https://www.nottingham.ac.uk/research/groups/orthopaedicsandtrauma/trauma-research/octs.aspx. Accessed Oct 10 2020.
Craxford S, Deacon C, Myint Y, Ollivere B. Assessing outcome measures used after rib fracture: A COSMIN systematic review. Injury. 2019;50(11):1816–1825. https://doi.org/10.1016/j.injury.2019.07.002. Accessed 4 July 2019.
Baker E, et al. The long-term outcomes and health-related quality of life of patients following blunt thoracic injury: a narrative literature review. Scand J Trauma Resusc Emerg Med. 2018;26(1):67.
Darwich A, et al. Outcome measures to evaluate upper and lower extremity: which scores are valid? Z Orthop Unfall. 2020;158(1):90–103.
Williams N. DASH. Occupat Med. 2014;64(1):67–8.
Beaton DE, et al. Measuring the whole or the parts? J Hand Ther. 2001;14(2):128–42.
Johanson NA, et al. American Academy of orthopaedic surgeons lower limb outcomes assessment instruments. J Bone Joint Surg. 2004;86(5):902–9.
Antonios T, et al. A systematic review of patient-reported outcome measures used in circular frame fixation. Strat Trauma Limb Reconstr. 2019;14(1):34–44.
Binkley JM, Stratford PW, Lott SA, Riddle DL. The lower extremity functional scale (LEFS): scale development, measurement properties, and clinical application. North American Orthop Rehabil Res Netw Phys Ther. 1999;79(4):371–83.
Yeung TSM, et al. Reliability, validity, and responsiveness of the lower extremity functional scale for inpatients of an orthopaedic rehabilitation ward. J Orthop Sports Phys Ther. 2009;39(6):468–77.
Shultz S, et al. A systematic review of outcome tools used to measure lower leg conditions. Int J Sports Phys Ther. 2013;8(6):838–48.
Horng Y-S, Hou W-H, Liang H-W. Responsiveness of the modified lower extremity functional scale in patients with low back pain and sciatica: a comparison with pain intensity and the modified Roland-Morris Disability Scale. Medicine. 2019;98(14):e15105–e15105.
Mehta SP, et al. Measurement properties of the lower extremity functional scale: a systematic review. J Orthop Sports Phys Ther. 2016;46(3):200–16.
Hung M, et al. The factor structure of the hospital anxiety and depression scale in orthopedic trauma patients. Journal of clinical medicine research. 2015;7(6):453–9.
Bjelland I et al (2002) The validity of the hospital anxiety and depression scale. An updated literature review. J Psychosom Res 52(2):69–77.
Barkham M, et al. The CORE-10: a short measure of psychological distress for routine use in the psychological therapies. Couns Psychother Res. 2013;13(1):3–13.
Beck JG, et al. The impact of event scale-revised: psychometric properties in a sample of motor vehicle accident survivors. J Anxiety Disord. 2008;22(2):187–98.
Morina N, Ehring T, Priebe S. Diagnostic utility of the impact of event scale-revised in two samples of survivors of war. PLoS ONE. 2013;8(12):e83916.
Murphy D, et al. Exploring optimum cut-off scores to screen for probable posttraumatic stress disorder within a sample of UK treatment-seeking veterans. Eur J Psychotraumatol. 2017;8(1):1398001.
Wortmann JH, et al. Psychometric analysis of the PTSD checklist-5 (PCL-5) among treatment-seeking military service members. Psychol Assess. 2016;28(11):1392–403.
Darzi A et al. High quality care for all, NHS next stage review final report. Department of Health: Office of Public Sector Information, Information Policy Team, Kew, Richmond, Surrey TW9 4DU;2008.
NHS. NHS STANDARD CONTRACT FOR MAJOR TRAUMA SERVICE (ALL AGES): SCHEDULE 2- THE SERVICES A. SERVICE SPECIFICATIONS, N.C. Board ed. NHS England;2013.
Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences. Fewer Data On Costs Health Affairs. 2013;32(2):207–14.
Finkelstein JA, Schwartz CE. Patient-reported outcomes in spine surgery: past, current, and future directions. J Neurosurg Spine. 2019;31(2):155–64.
McCormick JD, Werner BC, Shimer AL. Patient-reported outcome measures in spine surgery. J Am Acad Orthop Surg. 2013;21(2):99–107.
Cruz DL, et al. Validation of the recently developed Total Disability Index: a single measure of disability in neck and back pain patients. J Neurosurg Spine. 2019;2019:1–9.
Spiegel MA et al. (2016) Developing the total disability index based on an analysis of the interrelationships and limitations of oswestry and neck disability index. Spine (Phila Pa 1976) 41(1):74–81.
Harvey-Kelly KF, et al. Quality of life and sexual function after traumatic pelvic fracture. J Orthop Trauma. 2014;28(1):28–35.
Nepola JV, et al. Vertical shear injuries: is there a relationship between residual displacement and functional outcome? J Trauma. 1999;46(6):1024–9.
Templeman D, et al. Internal fixation of displaced fractures of the sacrum. Clin Orthop Relat Res. 1996;329:180–5.
Banierink H, et al. Patient-reported physical functioning and quality of life after pelvic ring injury: a systematic review of the literature. PLoS ONE. 2020;15(7):0233226.
Lefaivre KA, et al. What outcomes are important for patients after pelvic trauma? Subjective responses and psychometric analysis of three published pelvic-specific outcome instruments. J Orthop Trauma. 2014;28(1):23–7.
Majeed SA. Grading the outcome of pelvic fractures. J Bone Joint Surg Br. 1989;71(2):304–6.
Borg T, et al. Development of a pelvic discomfort index to evaluate outcome following fixation for pelvic ring injury. J Orthop Surg (Hong Kong). 2015;23(2):146–9.
Lefaivre KA, et al. Reporting and interpretation of the functional outcomes after the surgical treatment of disruptions of the pelvic ring: a systematic review. J Bone Joint Surg Br. 2012;94(4):549–55.
Wilson JTL, et al. Reliability of postal questionnaires for the Glasgow Outcome Scale. J Neurotrauma. 2002;19(9):999–1005.
Swiontkowski MF, et al. Short musculoskeletal function assessment questionnaire: validity, reliability, and responsiveness. J Bone Joint Surg Am. 1999;81(9):1245–60.
Wanner JP, et al. Development of a trauma-specific quality-of-life measurement. J Trauma Acute Care Surg. 2015;79(2):275–81.
Ogollah R, et al. Responsiveness and minimal important change for pain and disability outcome measures in pregnancy-related low back and pelvic girdle pain. Phys Ther. 2019;99(11):1551–61.
Copay AG, Cher DJ. Is the oswestry disability index a valid measure of response to sacroiliac joint treatment? Qual Life Res. 2016;25(2):283–92.
Gerbershagen HJ, et al. Chronic pain and disability after pelvic and acetabular fractures–assessment with the Mainz Pain Staging System. J Trauma. 2010;69(1):128–36.
Zeckey C, et al. Head injury in polytrauma-Is there an effect on outcome more than 10 years after the injury? Brain Inj. 2011;25(6):551–9.
Falkenberg L et al. Long-term outcome in 324 polytrauma patients: What factors are associated with posttraumatic stress disorder and depressive disorder symptoms? Eur J Med Res 2017;22(1):44
Koller M et al. Outcome after polytrauma in a certified trauma network: comparing standard vs. maximum care facilities concept of the study and study protocol (POLYQUALY). BMC Health Services Res 2016;16:242.
Roy B (2018) PROMS 2.0 Lecture. in UK PROMS Summit 2018. De Vere Conference Centre:London;2018.
Holch P, et al. Development of an integrated electronic platform for patient self-report and management of adverse events during cancer treatment. Ann Oncol. 2017;28(9):2305–11.
Hsu C, et al. Healing in primary care: a vision shared by patients, physicians, nurses, and clinical staff. Ann Fam Med. 2008;6(4):307–14.
Porter I, et al. Framework and guidance for implementing patient-reported outcomes in clinical practice: evidence, challenges and opportunities. J Comp Eff Res. 2016;5(5):507–19.
Barkham M, et al. Suitability and utility of the CORE-OM and CORE-A for assessing severity of presenting problems in psychological therapy services based in primary and secondary care settings. Br J Psychiatry. 2005;186:239–46.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this paper.
Rights and permissions
About this article
Cite this article
Andrzejowski, P., Holch, P. & Giannoudis, P.V. Measuring functional outcomes in major trauma: can we do better?. Eur J Trauma Emerg Surg 48, 1683–1698 (2022). https://doi.org/10.1007/s00068-021-01720-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-021-01720-1