Abstract
Introduction
Frailty is a geriatric syndrome, leading to declines in homeostatic reserve and physical resistance. It has been considered as a risk factor for falls, fractures, need of institutionalization, length of stay and mortality. Our aim was to evaluate the relationship between frailty, 30-day postoperative mortality and morbidity, for elderly patients undergoing surgical emergencies.
Material and methods
Prospective, observational cohort Study (September 2017–April 2019), using four different frailty scales (Clinical Frailty Scale, FRAIL scale, TRST and Share-FI) as a risk factor of 30-day postoperative outcomes, for patients older than 70 years undergoing emergency surgery. We analyzed diagnoses, clinical examination at admission, surgical procedures, and postoperative outcomes during the first 30 days or until discharge.
Results
92 patients were included, with a mean age was 78.7 years (SD 6.3). Frailty prevalence varied since 14.1% obtained using FRAIL scale, to 25%, 29.2% and 30.4%, from Clinical Frailty Scale, TRST and Share-FI, respectively. All four frailty scales show statistical differences to predict major complication and mortality in our sample. FRAIL scale showed the highest sensitivity–specificity pair to predict mortality in our sample (AUC = 0.870). TRST and FRAIL scales showed the strongest measure of association (OR 7.69 and 5.92, respectively) for major complications. Regarding need for admission to the ICU, hospital stay or reoperation rate, only FRAIL scale showed a statistically significant association.
Conclusion
Frailty represents a predictive marker of mortality and major complications, in surgical emergencies. FRAIL score, shows the strongest relationship with mortality and complications, compared to other frailty scales.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Frailty is a geriatric syndrome associated with aging, which leads to a decrease in the body’s homeostatic reserve and physical resistance, which leaves the individual vulnerable to health stressors [1].
Frail phenotype has been considered a high-prevalence risk factor in the elderly population [2], which increases the risk of unfavorable health-related outcomes, such as duration of hospitalization, risk of falls, the need for institutionalization and mortality [3]. Frailty is present in approximately 17–30% of patients over 65 years of age [2, 4,5,6,7], reaching up to 50% of those over 75 years.
One of the fundamental problems regarding this syndrome is the absence of standardized terminology, as well as the lack of a valid screening method for persons who may benefit from certain treatments or preventive measures [3]. The most commonly used scales assess frailty according to Fried phenotype criteria, unlike deficit accumulation models, which are more complex and less representative of the original concept of Fried [8].
Although there is a consensus about the frailty criteria defined by Fried (weight loss, exhaustion, low physical activity, slowness and weakness), there is no unanimous agreement to defend a single test, since most offer high sensitivity but lack adequate specificity to be used as a single diagnostic test, specially in the elective setting [9]. On the other hand, the use of brief frailty scales in emergency departments, where comprehensive geriatric assessment can be complex, has increased in recent years [10]. These feasible scales for rapid frail assessment, as Clinical Frailty Scale, FRAIL scale, the Triage Risk Screening Tool (TRST) or Share-FI, have capability enough to evaluate patients’ baseline condition [11, 12].
Different studies have related frailty with adverse clinical outcomes after elective surgery, with longer hospital stays, decrease functional status, and with an increased risk of complications, higher readmission rates and mortality [13, 14].
With respect to emergency procedures, information regarding the influence of frailty on postoperative complications remains scarce [15]. As a result, some elderly patients undergoing surgical procedures may have unacceptable risks of postoperative complications and mortality. On the other hand, some surgeries might be contraindicated based exclusively on criteria of age or inaccurate tools, denying the opportunity for a treatment that could be life-saving or improve the quality of life in this group of patients.
Based on the above, the objective of this study was to determine the relationship between frailty and postoperative outcomes in elderly patients who undergo emergency surgery.
Methods
Prospective, observational cohort study, using four frailty scales as a risk factor of short-term adverse outcomes, for patients older than 70 years, during the postoperative course of emergency surgery, registered at Hospital Universitario Virgen del Rocío (Seville, Spain), between September 2017 and April 2019.
The study was approved by the Clinical Investigations Ethics Committee (CIEC) of Hospital Universitario Virgen del Rocío.
The main objective was to evaluate the relationship between frailty and postoperative mortality, using four different frailty scales. Secondary objectives were to compare the predictive accuracy of the four frailty scales, to detect the best pair sensitivity/specificity and to assess the association between the frailty scales and postoperative complications.
A prior sample size calculation was assessed to estimate the study population necessary to meet the primary objective. As risk of postoperative mortality for frail patients in the emergency departments has not consistently demonstrated, we assumed an estimated OR for postoperative mortality of 3.5 for our sample calculation, based on previous studies reporting and OR for postoperative mortality in the elective setting ranged between 4 and 11.7 [16, 17]. With a study power of 80% and an α-error of 0.05, 90 patients resulted as the required sample size.
Inclusion criteria were patients over 70 years of age, and patients who underwent abdominal surgery. Since age-related physiological decline is widely known, there is no set age at which a person becomes geriatric. Although the typical age for considering an “elderly patient” has been over 65, studies considering age over 70, 75 or 85 years have recently raised. Patients under 70 years, patients with moderate-severe cognitive deterioration and patients with terminal illness, defined as a life expectancy of less than 6 months, were excluded from the study.
Data related to age, sex, BMI, cardiovascular risk factors, comorbidities, polymedication (defined as the use of more than five drugs daily) [18], patients on anticoagulant or antiplatelet medication, and record of falls in the last year [18] were registered for subsequent analysis. Furthermore, variables related to the acute disease at admission, clinical parameters and laboratory tests at admission, as well as the surgical treatment performed, were collected.
Finally, complications that occurred during the first 30 postoperative days or until discharge, as well as their length of hospital stay, were recorded. For measurement of postoperative complications, the internationally accepted Clavien Dindo classification was used to describe their severity [19]. Major complications were defined as those with grade 3 or higher of this classification.
The study was developed in three phases: a recruitment phase, in which patients who met the inclusion criteria were identified, the informed consent form was signed and the baseline frailty assessment of patients was carried out using four validated diagnostic scales (Clinical Frailty Scale, FRAIL score, TRST and Share-FI). All frailty scales measurements were taken by a single physician. The second phase was the period of follow-up, in which a daily record of the patient’s clinical status was made, identifying postoperative complications; and finally a statistical analysis phase to achieve results interpretation.
For the statistical analysis, the qualitative variables are presented with their distribution of frequencies. The chi-squared test or Fisher’s exact test was used to restore differences between the groups.
Quantitative variables are summarized in their mean and standard deviation (SD) and variables that do not follow a normal distribution are expressed with median and interquartile range (IQR). The normality of quantitative variables was evaluated through the graphic inspection of histograms and Q–Q plot graphs (quantile–quantile). They were compared through the Student’s t test and the analysis of variance (ANOVA). When a normal distribution was not present, the continuous variables were expressed as median and range and were compared using the Mann–Whitney U test.
Contingency tables, logistics regression models, multivariate analysis and ROC curve statistical analysis were done to evaluate the prognostic efficacy of the scales. The statistical study was carried out with the SPSS statistical program (IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp).
Results
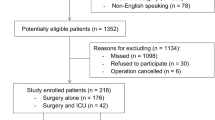
From 722 emergency surgeries between the study period, 113 were considered eligible for inclusion, of whom 92 patients were finally included. During follow-up in the first 30 days after surgery or until discharge, there were no losses. Thus, the sample of 92 patients who underwent urgent surgical procedure with follow-up until hospital discharge or until death was analyzed.
The mean age of the population was 78.71 years (SD 6.26). Women represented 53.3% of the sample, and men represented 46.7%.
Hypertension was the most common disease according to the patients’ personal medical records, followed by heart disease (history of ischemic cardiomyopathy and atrial fibrillation).
Non-perforated acute abdomen (25%), intestinal obstruction (32.6%) and perforation of the hollow viscus (16.3%) were the most common diagnosis for which the patients underwent surgery. Of these, tumor disease represented about 29.34%. Table 1 shows the type of surgical procedures performed.
The overall rate of complications was 50%, with up to 46 patients having some deviation from the normal postoperative course. Table 2 shows the types of complications that occurred in the sample, as well as the grade of complication according to the Clavien-Dindo classification.
The rate of anastomotic dehiscence in the sample was 18.51%. Overall mortality was 10.9%. The median time of admission was 6 days (IQR 3.25–11.65).
With regard to recording of frailty, the prevalence in our population oscillated, according to the four scales used. The FRAIL scale found a smaller sample of frail patients than the rest of the scales (14.1%). The Clinical Frailty Scale, Triage Risk Screening Tool, and Share-Fi scales found a similar prevalence of frailty in the sample, from 25 to 30.4%.
Analyzing the association between the presence of frailty and postoperative complications, the four scales were statistically significant for predicting both major complications and mortality in our sample. The binary logistic regression model demonstrated a greater OR in the FRAIL scale (OR = 16.071 (95% CI 3.646–70.845), p < 0.001), compared to the others. The frail phenotype demonstrated a greater association with the risk of developing major complications considered grade 3 or higher on the Clavien-Dindo scale (Table 3). The TRST and FRAIL scales were the ones that showed the greatest strength of association (OR 7.69 and 5.92, respectively). Use of polymedication was not related individually to major complications or mortality. Patients on anticoagulant or antiplatelet medication were related to postoperative bleeding (OR 1.27, CI 95% 1.05–4.72, p = 0.046), but with no relationship with other adverse events as reoperation rate, need for ICU, other complications, or mortality.
The ROC curve analysis highlighted the FRAIL scale a greater area under the curve (AUC = 0.870) than the others, to relate frailty with post-operative mortality. AUC of CFS, FRAIL scale, Share-FI and TRST are shown in Fig. 1.
When it comes to predicting the need for admission to the ICU, hospital stay or reoperation rate, frailty only showed a statistically significant association when determined using the FRAIL scale. The other scales did not show the relationship between frailty and the presence of any of these adverse events.
Kappa coefficient between four frailty scales and preoperative physical status assessed by the American Society of Anesthesiologists (ASA) classification was also evaluated in our sample. Kappa values of 0.18, 0.15, 0.19 and 0.07 were observed for TRST, Share-FI, Clinical Frailty Scale and FRAIL scale, respectively, indicating a poor agreement between the ASA score, and the four frailty scales.
Finally, binary regression was used to establish the morbimortality variables that were most related to frailty. As shown in Table 4, these complications were respiratory failure, renal failure and organ-space surgical site infection (Table 4). Hospital stay was also longer in the frail group (16.9 days VS 9.1, p = 0.019).
Discussion
Our study found a significant relationship between the presence of frailty and both mortality and major complications, in patients over 70 years requiring emergency surgery.
Frailty has been analyzed in recent years in several epidemiological studies, finding that mortality is the primary adverse event in the emergency setting [5, 7, 13, 20, 21]. It has been defined as a pathology with high prevalence in the population over 65 years, reaching up to 30% in some studies [2, 4]. In our study, most of the scales defined a frail elderly population over 25% of the total sample, although using the FRAIL scale, the prevalence was lower (14%).
Based on the different frailty scales used in our study, the risk of death after undergoing an emergency surgical procedure would be 5–16 times more likely when frailty syndrome is present. Furthermore, this group of patients has an increased risk of suffering complications such as acute renal failure, surgical site infection or acute confusional state. Compared to other studies analyzing frail patients in elective surgeries [13, 21], our results may be interpreted as a significant increase in the risk of complications and death when patients require emergency surgery,
According to our results, frailty could be even more disastrous in the emergency surgery patient than in individuals with other acute diseases. Salinas et al. [22] reported a threefold higher mortality in frail elderly patients who suffered an episode of the acute coronary syndrome, and a 2.7-fold higher risk of bleeding during the first 30 days.
Furthermore, the great variability of diagnostic scales to define frailty does not allow for standardization of use, nor contribute to the use of a single scale, since no scale has demonstrated its superiority over the others [8]. In this respect, the use of frailty scales based on the definition of the phenotype of Fried et al. [3], through short questionnaires that evaluate the patient’s baseline status, is being increasingly used in the emergency departments [23, 24]. Considering the results in our study, we concluded that all four scales used (Clinical Frailty Scale, FRAIL, TRST and Share-Fi) are able to predict the risk of mortality and major complications after emergency surgery. Furthermore, FRAIL scale showed the strongest association with those complications, regardless of other factors. This results might be due to different factors. First, FRAIL scale was also the test obtaining the lower prevalence of frailty (14.1%), which probably increased the specificity as a predictor of adverse events. Other reason could be that four out of five items in the FRAIL scale questionnaire, were related to physical activity, while other scales included comorbidities or social support aspects in their questionnaires.
Our study has the following limitations: the sample size, although calculated to meet the primary objective of the study, may involve a limitation for some secondary objectives, for which few events were registered. In addition, wide confidence intervals might suggest insufficient accuracy due to the number of patients. On the other hand, as a consequence of the exclusion of patients with moderate to severe cognitive impairment, the prevalence of frailty might be lowered in our sample. Inclusion of only surgical patients might be another limitation of the study. Considering the frailty scales assessment was not analyzed on elderly patients with medical processes for which surgical treatment was not performed (e.g., acute cholecystitis with conservative treatment), which may imply a worse baseline situation than those who undergo surgery. Therefore, the absence of selection bias in this sense cannot be guaranteed. Given that this was a single-center study, there might be a potential limitation in the generalizability of the results, as the composition of the study population, and resources or department characteristics cannot be extrapolated to other centers.
Finally, patient follow-up during the first 30 days of admission does not allow for an adequate analysis of the effect of frailty on the subsequent quality of life of patients included in the study, nor the medium- to long-term morbimortality.
Despite the limitations mentioned, from our study it can be concluded that the frailty represents a predictive marker of short-term mortality and major complications in patients over 70 years of age admitted for surgical emergencies, regardless of the other factors. Furthermore, in our sample, these patients had a longer hospital stay.
References
Hogan DB, Maxwell CJ, Afilalo J, Arora RC, Bagshaw SM, Basran J, et al. A scoping review of frailty and acute care in middle-aged and older individuals with recommendations for future research. Can Geriatr J. 2017;20:22.
Rockwood K, Stadnyk K, MacKnight C, McDowell I, Hébert R, Hogan DB. A brief clinical instrument to classify frailty in elderly people. Lancet. 1999;353:205–6.
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–M156156.
Shamliyan T, Talley KMC, Ramakrishnan R, Kane RL. Association of frailty with survival: a systematic literature review. Ageing Res Rev. 2013;12:719–36.
Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol Ser A Biol Sci Med Sci. 2004;59:M255–M263263.
Cigolle CT, Ofstedal MB, Tian Z, Blaum CS. Comparing models of frailty: the health and retirement study. J Am Geriatr Soc. 2009;57:830–9.
Abizanda P, Romero L, Sánchez-Jurado PM, Martínez-Reig M, Gómez-Arnedo L, Alfonso SA. Frailty and mortality, disability and mobility loss in a Spanish cohort of older adults: the FRADEA study. Maturitas. 2013;74:54–60.
Bouillon K, Kivimaki M, Hamer M, Sabia S, Fransson EI, Singh-Manoux A, et al. Measures of frailty in population-based studies: an overview. BMC Geriatr. 2013;13:64.
Woo J, Yu R, Wong M, Yeung F, Wong M, Lum C. Frailty screening in the community using the FRAIL scale. J Am Med Dir Assoc. 2015;16:412–9.
Carpenter CR, Shelton E, Fowler S, et al. Risk factors and screening instruments to predict adverse outcomes for undifferentiated older emergency department patients: a systematic review and meta-analysis. Acad Emerg Med. 2015;22:1–21.
Rodríguez-queraltó O, Formiga F, López-palop R, et al. FRAIL scale also predicts long-term outcomes in older patients with acute coronary syndromes. J Am Med Dir Assoc. 2019.
Kahlon S, Pederson J, Majumdar SR, Belga S, Lau D, Fradette M, et al. Association between frailty and 30-day outcomes after discharge from hospital. Can Med Assoc J. 2015;187:799–804.
Robinson TN, Wu DS, Stiegmann GV, Moss M. Frailty predicts increased hospital and 6-month healthcare cost following colorectal surgery in older adults. Am J Surg. 2011;202:511–4.
Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath F-A. Laparoscopic colorectal surgery confers lower mortality in the elderly: a systematic review and meta-analysis of 66,483 patients. Surg Endosc. 2015;29:322–33.
Goeteyn J, Evans LA, De Cleyn S, et al. Frailty as a predictor of mortality in the elderly emergency general surgery patient. Acta Chir Belg. 2017;117:370–5.
Farhat JS, Velanovich V, Falvo AJ, Horst HM, Swartz A, Patton JH, et al. Are the frail destined to fail? Frailty index as predictor of surgical morbidity and mortality in the elderly. J Trauma Acute Care Surg. 2012;72:1526–31.
Hewitt J, Moug SJ, Middleton M, Chakrabarti M, Stechman MJ, McCarthy K. Prevalence of frailty and its association with mortality in general surgery. Am J Surg. 2015;209:254–9.
Masnoon N, Shakib S, Kalisch-ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17:230.
Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Ethun CG, Bilen MA, Jani AB, Maithel SK, Ogan K, Master VA. Frailty and cancer: implications for oncology surgery, medical oncology, and radiation oncology. CA Cancer J Clin. 2017;67:362–77.
Kojima G. Frailty as a predictor of future falls among community-dwelling older people: a systematic review and meta-analysis. J Am Med Dir Assoc. 2015;16:1027–33.
Salinas GLA, Fernández MS, Izco MP, et al. Frailty predicts major bleeding within 30 days in elderly patients with Acute Coronary Syndrome. Int J Cardiol. 2016;222:590–3.
Carpenter CR, Banerjee J, Keyes D, et al. Accuracy of dementia screening instruments in emergency medicine: a diagnostic meta-analysis. Acad Emerg Med. 2019;26:226–45.
Lewis ET, Dent E, Alkhouri H, Kellett J, Williamson M, Asha S, et al. Which frailty scale for patients admitted via Emergency Department? A cohort study Arch Gerontol Geriatr. 2019;80:104–14.
Funding
The authors declare that no funding was received in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest in relation to this article.
Ethical responsibilities
The study was approved by the Ethics Committee of Hospital Universitario Virgen del Rocío. All participants granted their consent to participate in the study. All of the authors have confirmed the preservation of confidentiality and respect of patients’ rights in the document of author responsibilities, publication agreement and transfer of rights to the European Journal of Trauma and Emergency Surgery.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Arteaga, A.S., Aguilar, L.T., González, J.T. et al. Impact of frailty in surgical emergencies. A comparison of four frailty scales. Eur J Trauma Emerg Surg 47, 1613–1619 (2021). https://doi.org/10.1007/s00068-020-01314-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-020-01314-3