Abstract
Purpose
Osteoarthritis is a common disease with a prevalence of approximately 8.9% among the average population. One treatment option is low-dose radiotherapy. Some authors mention that they apply a second or third course of radiation for recurrent pain or partial or no response to the initial course. As the results of re-irradiation have not been analysed systematically, the aim of this study was to document the results of repeated radiation treatment and to identify those patients who will benefit.
Methods and materials
The analysis was performed on patients of three German radiotherapy institutions and included 217 re-irradiated joints. Pain was documented with the numeric rating scale (NRS). Evaluation of the NRS was done before and directly after each radiation therapy as well as at the follow-up of 24 months.
The median age of the patients was 67 years, with 40% male and 60% female patients. Re-irradiation was indicated because the initial radiotherapy resulted in no response in 21.2%, in partial response in 41.5%, and in recurrent pain in 37.3%.
Results
We found a significant response to re-irradiation. For the whole sample, the median pain was 6 before re-irradiation, 4 after 6 weeks, and 3 after 12 weeks, 6 months, 12 months, and 24 months. The percentage of patients being free of pain or with very little pain was approximately 25% 12 months after re-irradiation. All subgroups, notably those with no response to the first course versus partial response to the first course versus recurrent pain, had significant reduction of pain.
Conclusion
Re-irradiation of osteoarthritis is an effective and safe treatment. All subgroups showed a good response to re-irradiation for at least 24 months.
Zusammenfassung
Hintergrund
Die Arthrose ist mit einer Prävalenz von 8,9 % unter der erwachsenen Bevölkerung eine häufige Erkrankung. Die Strahlentherapie stellt eine wichtige Therapieoption dar. Dabei beschreiben einige Autoren die Durchführung einer Rebestrahlung bei rezidivierten Schmerzen bzw. unzureichendem oder keinem Ansprechen auf die initiale Bestrahlungsserie. Eine strukturierte Auswertung der Rebestrahlung existiert allerdings nicht. Ziel dieser Arbeit ist die strukturierte Auswertung der Rebestrahlung bei Arthrose.
Material und Methode
Ausgewertet wurden Patienten aus drei strahlentherapeutischen Institutionen. Insgesamt konnten 217 rebestrahlte Gelenke analysiert werden. Die Schmerzintensität wurde mit Hilfe der numerischen Rating-Skala (NRS) quantifiziert und zu den Zeitpunkten vor Bestrahlungsbeginn, direkt nach Radiatio, 6 und 12 Wochen, 6, 12 und 24 Monate nach Bestrahlung erfasst. Die Patienten waren im Median 67 Jahre alt, 40 % davon waren männlich und 60 % weiblich. Grund der Rebestrahlung war bei 21,2 % der Patienten kein Ansprechen und bei 41,5 % ein unzureichendes Ansprechen auf die erste Bestrahlungsserie sowie bei 37,3 % rezidivierte Schmerzen.
Ergebnisse
Für das Gesamtkollektiv zeigte sich eine signifikante Schmerzreduktion. Die mediane Schmerzintensität war 6 vor der Rebestrahlung, 4 nach 6 Wochen und 3 nach 12 Wochen, 6, 12 und 24 Monaten. Nach 12 Monaten waren ungefähr 25 % der Patienten schmerzfrei oder nahezu schmerzfrei. Alle Subgruppen, insbesondere Patienten ohne Ansprechen und Patienten mit unzureichendem Ansprechen auf die initiale Bestrahlung bzw. Patienten mit rezidivierten Schmerzen zeigten eine signifikante Schmerzreduktion.
Schlussfolgerung
Zusammenfassend zeigt diese Arbeit, dass die Rebestrahlung bei der Arthrose eine effektive Therapie darstellt und dass alle analysierten Subgruppen von der Therapie profitieren.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis is a common disease, especially in elderly people. The prevalence of symptomatic osteoarthritis is approximately 8.9% and that of asymptomatic osteoarthritis approximately 20.3% among the adult population [1,2,3]. Most frequently the knee is affected, with about 6% symptomatic knee arthritis [1, 4]. For the population older than 70 years, the prevalence of knee arthritis is about 40% [2, 4]. The prevalence of rhizarthritis is approximately 7% for men and 15% for women among a population over 30 years [5]. As life expectancy and the prevalence of risk factors for osteoarthritis, such as overweight and inactivity, are rising, an increasing prevalence of osteoarthritis can be expected in the future [2].
Several therapeutic options for treatment of osteoarthritis are in use [2, 4]. There is good evidence for arthroplasty for advanced osteoarthritis [2, 3, 6, 7]. For joint-conserving therapies, there is not a high level of evidence [2]. Besides ice, heat, ultrasound treatment, splinting, and physiotherapy, many patients get drug therapy. The drug therapy can be systemic, for example with nonsteroidal anti-inflammatory drugs, or can consist of local injections of anaesthetics or steroids [8,9,10,11].
One noninvasive treatment for osteoarthritis is low-dose radiotherapy [12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33]. As for several other bone and joint disorders, low-dose radiation has shown an anti-inflammatory effect [12, 15, 34,35,36,37,38,39,40,41,42,43,44,45]. There are several retrospective studies and some prospective nonrandomised trials with about 2100 published patients in total that strongly suggest its effectiveness [17, 24, 46]. For example, in Germany about 4500 patients receive low-dose radiation therapy for knee arthritis per year [16].
Some authors mention that they apply a second or third course of radiotherapy [16, 23, 24, 47]. A second or third radiation course was usually given because of recurrent pain or partial or no response after the initial radiation course [16, 23, 24, 34, 47]. In some institutions, two courses of radiation are included in the primary treatment concept [37].
To our best knowledge, there is no study existing that analyses the results of re-irradiation systematically. The aim of this survey is to document the results of re-irradiation for osteoarthritis and to help identify those patients who will benefit from re-irradiation.
Patients and methods
The study was approved by the Ethics Committee of the University of Regensburg.
The retrospective analysis was performed on data from patients at three German radiotherapy institutions. All patients who underwent more than one course of low-dose radiotherapy for osteoarthritis on the same joint or joint region were identified.
For diagnosis of osteoarthritis, appropriate findings on radiological imaging and distinct clinical findings were mandatory. The patients’ data from the regular follow-up visits were analysed. Additionally, the patients were questioned about their current status and were clinically examined. The aetiology of their pain was identified, the reason for re-irradiation was assessed, and the time between initial radiotherapy and re-irradiation was documented. Possible risk factors for the result of radiation were registered and correlated with the response.
Pain was documented using the numeric rating scale (NRS). Evaluation of the NRS was done before and directly after each radiation therapy course as well as for the follow up. Follow-up was done 6 weeks, 12 weeks, 6 months, 12 months, and 24 months after treatment.
Descriptive statistics were done. For NRS and all time periods, the median, range, and interquartile range (IQR) were calculated. To analyse significant differences in the chronological sequence of NRS, the paired Wilcoxon test for dependent variables was used. The Mann–Whitney U test for independent variables was used for subgroup analyses, and the Fisher–Yates test was used for binomial variables. It was postulated that p < 0.05 was significant. Statistics were done with SPSS Statistics 23.0 (IBM Corporation, Armonk, NY, USA).
For some small joints such as osteoarthritis of the finger, the finger joints of each hand were subsumed to one joint region, as patients were not able to score the pain for each single joint.
Finger and toes were categorised as small joints, while the hip, knee, shoulder, and ankle were classified as large joints.
Results
A total of 140 patients could be identified, questioned, and clinically examined, and 217 joint or joint regions were treated since some patients were irradiated on more than one joint.
The median age of the patients was 67 years, with a range of 38–88 years and an IQR of 59–73 years. Eighty-four patients were female, and 56 were male. The right limb was treated 115 times and the left limb 99 times. Most often, an arthritis of the knee (78 joints), rhizarthritis [38], a Heberden or Bouchard arthritis [24], or an arthritis of the hip [22] was treated. The median follow-up was 25 months, with an IQR from 13 months to 37 months (Table 1).
Low-dose radiotherapy was performed with a linear accelerator using 6 MV or 15 MV photons in opposing fields or as a single field. Dose calculation was done to the isocentre or middle of the joint. Re-irradiation was given a median of 14 weeks after the initial radiation (range 6 weeks to 133 months, IQR 11–26 weeks). The reason for re-irradiation was no response after the initial radiation in 21.2%, partial response in 41.5%, and recurrent pain in 37.3%.
One hundred twenty-three (56.7%) joints were re-irradiated with a fractionated dose of 0.5 Gy to a total dose of 3.0 Gy (120 joints) or 1.5 or 2.0 Gy (three joints), and 94 (43.3%) joints were re-irradiated with a fractionated dose of 1.0 Gy to a total dose of 6.0 Gy. Treatment time was usually 2 or 3 weeks (two or three times per week). Seventy joints (33.7%) were re-irradiated over 2 weeks, and 138 joints (66.3%) were re-irradiated over 3 weeks.
Acute or long-term side effects did not occur in our sample.
The median pain before the initial irradiation was 7 on the NRS (IQR 6–8). Before the re-irradiation, the median was 6 (IQR 4–8), and on the last day of the re-irradiation the median was 5 (IQR 3–7). Six weeks after re-irradiation, it was 4 (IQR 2–5). After 12 weeks and after 6 months it was 3 (IQR 1–5 respectively 6), and after 12 months and 24 months it was also 3 (IQR 2–6 respectively 7) (Fig. 1). At the last follow-up, the median pain was 4 (IQR 2–7).
Pain reduction compared to the pain level before re-irradiation was significant (p < 0.0001) for the entire follow-up.
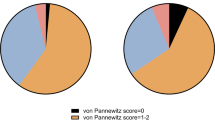
The percentage of patients being free of pain (NRS 0) or scoring pain as 1 on the NRS increased with time (Fig. 2).
Six weeks after the re-irradiation, 22.3% of the joints had pain reduction of three grades or more on the NRS. After 12 weeks it was 30.3%, after 6 months 30.8%, after 12 months 30.6%, and after 24 months 29.1%. The general response rate (reduction of one grade or more on the NRS) was 53.0% after 6 weeks, 58.7% after 12 weeks, 57.6% after 6 months, 50.6% after 12 months, and 47.0% after 24 months.
Male and female patients older or younger than 67 years had a significant reduction of pain (p < 0.0001 for all categories and the entire follow-up). There was no significant difference in the remaining pain level for gender or age (patients older or younger than 67 years) for the entire follow-up.
There was no significant difference between the right and the left limbs. Both groups had a significant reduction of pain.
There was no significant difference in pain reduction or absence of pain whether large joints or small joints were re-irradiated. Both subgroups had a significant reduction of pain (p < 0.0001).
Patients with knee arthritis (p < 0.01 for the entire follow-up), rhizarthritis (p < 0.001 for the entire follow-up), finger arthritis (p < 0.01 for the entire follow-up except at 24 months), and hip arthritis (p < 0.05 for the entire follow-up) had a significant reduction of pain.
Patients were analysed separately based on the reason for re-irradiation. For the joints with no response after the initial radiation, the median NRS score was 7 (IQR 5.75–8) pre-re-irradiation, 3 (IQR 1–4) 6 weeks after re-irradiation, 3 (IQR 1–3) for the 12-week follow-up, 2 (IQR 2–4) for the 6‑month follow-up, and 3 (IQR 2–5 and 2–6, respectively) for the 12-month and 24-month follow-ups.
There was a significant response for the entire follow-up (p < 0.0001).
Nonresponders after the initial radiation had a significantly better response to re-irradiation than patients with partial response or recurrent pain for the entire follow-up (p < 0.0001). Nonresponders had a significant lower remaining NRS pain level at 6 weeks and 12 weeks after re-irradiation than the other patients mentioned above (p < 0.02).
The joints with partial response after the initial radiation had a median NRS pain score of 7 (IQR 5–8) before the re-irradiation, 5.5 (IQR 4–8) after 6 weeks, and 5 (IQR 3–8) after 12 weeks. After 6 months and 12 months it was 5.5 (IQR 2.75–8), and after 24 months it was 6 (IQR 2–8).
There was a significant response (p < 0.0001) for the entire follow-up.
Response was significantly worse for the patients with partial response after the initial radiation compared with patients with no response or recurrent pain (p < 0.0001 for the entire follow-up). Patients with partial response also had a significantly higher remaining pain level compared to the other patients for the entire follow-up (p < 0.0001 for 6 weeks and 12 weeks as well as for 6 months and 12 months, and p < 0.001 for 24 months).
For those joints with recurrent pain, the median NRS score was 5 (IQR 4–6) before re-irradiation and 3 (IQR 2–4) 6 weeks after re-irradiation. After 12 weeks it was 2 (IQR 1–3), after 6 months and 12 months it was 2 (IQR 1–4), and after 24 months it was 3 (IQR 1–4).
Pain reduction was significant (p < 0.0001) for the entire follow-up (Fig. 3).
Except for 24 months after re-irradiation, there was no significant difference for patients with recurrent pain compared to the other patients. Twenty-four months after re-irradiation, response was worse for patients with recurrent pain (p = 0.021). There was a significantly lower NRS level for the entire follow up (p < 0.001) but also for the baseline before re-irradiation.
There was no significant difference in pain reduction whether joints were irradiated twice or three times weekly, as well as whether re-irradiation took place 6–9 weeks or 10–16 weeks after the initial course. Joints in all those categories had a significant reduction of pain for the entire follow-up (p < 0.01).
Patients re-irradiated with 0.5 Gy single dose to a total dose of 3.0 Gy as well as those re-irradiated with 1.0 Gy single dose to a total dose of 6.0 Gy had a significant response from treatment (p < 0.0001) for the entire follow-up. There was a significantly better reduction in pain using six times 0.5 Gy compared with six times 1.0 Gy (p < 0.01 for the 6‑week, 12-week, 6‑month, and 12-month follow-ups). The rate of patients being free of pain or scoring pain as 1 on the NRS was not significantly different between these subgroups.
Seventeen joints were re-irradiated a second time (third radiation course). In most cases it was because of no response to the initial radiotherapy or to the first re-irradiation. The median pain on the NRS was 8 before re-irradiation, 4 after 6 weeks, 3 after 12 weeks, 2 after 6 months, 3 after 12 months. There was a significant reduction of pain for the entire follow-up (p < 0.01).
Discussion
Although some recently published randomised trials did not show a significant benefit for radiotherapy of osteoarthritis of the knee and fingers, radiotherapy for osteoarthritis is well established [48, 49]. The weakness of these trials was discussed by Ott et al. in detail [50]. There are several retrospective studies and some nonrandomised prospective trials that strongly suggest the effectiveness of low-dose radiotherapy for osteoarthritis [17, 46]. In addition, prospective nonrandomised trials with objective response criteria have shown a beneficial effect of low-dose radiotherapy [45, 51].
Our sample is the first one examining re-irradiation of osteoarthritis systematically. Other authors did note re-irradiation, and some presented information such as descriptive statistics, but most authors simply stated that patients were re-irradiated. No specific major subgroup analysis had been done until now. The mentioned samples are small or mostly unstructured [17, 24, 32, 34, 37, 47]. For some manuscripts with mixed collectives of patients suffering from different diseases, data on re-irradiation of osteoarthritis have been mentioned [32].
Our sample of only re-irradiated patients seems to be comparable to samples of primary radiated patients. For example, the median age of 67 years seems to be comparable to that of the samples of Kaltenborn et al. (median age 61 years) [47], Ruppert et al. (average age 62 years) [37], Valtonen et al. (average age 59 years) [13], and Schertel and Roos (mean age 65 years) [17, 34] The proportion of male to female patients varies, but the percentage of male patients for radiotherapy of osteoarthritis is mostly between 19.5% and 36.9% [13, 17, 34, 47]. The ratio of 2:3 in our study seems at least to be comparable. Knee arthritis and finger arthritis belong to the most common types of osteoarthritis [2, 3].
The radiation technique and dose concept are equivalent to the recommended concept of the German Cooperative Group on Radiotherapy for Benign Diseases. Most of the recently published samples were treated in that way [52]. Re-irradiation has proven beneficial to our sample. Most of the patients had a response to re-irradiation, and approximately 25% of the patients were free of pain or scored low pain (NRS 1) for the long-term follow-up of at least 2 years.
For the collectives receiving low-dose radiotherapy for osteoarthritis, the overall response rate varies between 19% and 76% [17, 37, 47]. The long-term response rate of approximately 50% in our re-irradiated sample is at least comparable to those data.
Looking at the few and unstructured data for re-irradiation published so far, some information may be derived from the German patterns-of-care study [16] and Keller et al. [23]. They mention re-irradiation in approximately 30% of the collective. Detailed information concerning the results is missing.
Kaltenborn et al., for example, presented data of nine patients re-irradiated because of rhizarthritis [47]. Five out of eight patients had a partial response after re-irradiation. Schertel et al. presented data of 14 re-irradiated patients, with a slight further improvement in six of the patients [34].
For samples in which two courses of radiation separated by 6 weeks were generally used for osteoarthritis, most of them with a total dose of two times 3.0 Gy, no separate analysis of the second course had been described [37].
For reasons of radiation protection, a general application of two series of radiotherapy for osteoarthritis has to be carefully evaluated as to its risk. In most of the published samples, the majority of patients can be treated with sufficient results using just one course of low-dose radiotherapy [34, 47]. In summary, a general application of two series of radiotherapy should not be recommended.
As is recommended for the initial series of radiation, a single dose of 0.5–1.0 Gy and a total dose of 3.0–6.0 Gy, twice or three times weekly, should be used for re-irradiation of osteoarthritis [52]. Because we performed no randomised trial, a definitive suggestion for the exact dose concept cannot be made based on our analysis. A single dose of 0.5 Gy and a total dose of 3.0 Gy over 2–3 weeks seems to be recommendable for reasons of radiation protection, based on the data of Ott et al. for radiotherapy of other benign diseases [53,54,55]. Above all, we found a better response of patients in favour of a single dose of 0.5 Gy and a total dose of 3.0 Gy.
No relevant risk factors for treatment failure of re-irradiated patients could be found in our sample. All patients—male and female in all age categories; left and right limb; patients with knee, hip, and finger arthritis—showed positive responses to re-irradiation, mainly without significant differences among these subgroups. There was also no significant difference for the patients re-irradiated over a 2- or 3‑week period.
Independent of the reason for re-irradiation (no response, partial response to initial radiation, or recurrent pain), patients had significant pain reduction. The patients with partial response to the initial radiation retained a higher level of pain during the entire follow-up. In addition, they had a worse response to re-irradiation. Nevertheless, these patients also had significant pain reduction with re-irradiation.
The reasons for this worse response can only be assumed. One reason might be that inflammation causes just part of the pain. There might be pain simply due to degeneration. Maybe just the part of the pain related to intraarticular inflammation can be successfully treated with irradiation, and for the patients with partial response after the initial radiotherapy, most of the remaining pain is not related to inflammation [56, 57].
Some authors mention a third or even fourth radiation series for osteoarthritis [47]. A separate analysis of this subgroup has not been performed so far. We found a significant reduction in pain even with a third radiation course in our survey. Regarding these results, further re-irradiation (at least a third course of radiotherapy) seems to be an option for patients with osteoarthritis.
Conclusion
Re-irradiation of osteoarthritis is an effective and safe treatment. All subgroups, notably those with no response, partial response, or recurrent pain, showed a good response to re-irradiation for at least 24 months.
References
Andrianakos AA, Kontelis LK, Karamitsos DG et al (2006) Prevalence of symptomatic knee, hand, and hip osteoarthritis in Greece. The ESORDIG study. J Rheumatol 33(12):2507–2513
Rabenberg M (2013) Arthrose. Gesundheitsberichterstattung des Bundes vol 54. Robert Koch-Inst, Berlin
Arnold I (2016) Arthrose. Was gibt es Neues? Dtsch Ärztebl 113(44):1976–1982
Michael JW-P, Schlüter-Brust KU, Eysel P (2010) The epidemiology, etiology, diagnosis, and treatment of osteoarthritis of the knee. Dtsch Arztebl Int 107(9):152–162
Haara MM, Heliövaara M, Kröger H et al (2004) Osteoarthritis in the carpometacarpal joint of the thumb. Prevalence and associations with disability and mortality. J Bone Joint Surg 86(7):1452–1457
Grayson CW, Decker RC (2012) Total joint arthroplasty for persons with osteoarthritis. J Inj Funct Rehabil 4(5 Suppl):97–103
Gutowski CJ, Parvizi J, Purtill JJ (2015) Protocol-based arthroplasty. Less is more. Orthopedics 38(10):631–638
Taruc-Uy RL, Lynch SA (2013) Diagnosis and treatment of osteoarthritis. Prim Care 40(4):821–836, vii
Smelter E, Hochberg MC (2013) New treatments for osteoarthritis. Curr Opin Rheumatol 25(3):310–316
Schuh A, Jezussek D, Fabijani R et al (2007) Bleiben Sie kritisch bei der Wahl Ihrer Therapie! MMW Fortschr Med 149(25-26):31–32
Rehart S, Arnold I, Fürst M (2007) Die konservative Lokaltherapie des entzündeten Gelenks. Lokal-invasive Therapieformen. Z Rheumatol 66(5):382–387
Trott KR, Parker R, Seed MP (1995) Die Wirkung von Röntgenstrahlen auf die experimentelle Arthritis der Ratte. Strahlenther Onkol 171(9):534–538
Valtonen EJ, Lilius HG, Malmio K (1975) The value of roentgen irradiation in the treatment of painful degenerative and inflammatory musculoskeletal conditions. A double-blind study. Scand J Rheumatol 4(4):247–249
Stech H (1954) Zur Frage der Röntgen-Ganzkörper-Abschnittsbestrahlung (RöGKAB.) bei gutartigen Erkrankungen (chronische Ekzeme, Heuschnupfen, Akne vulgaris, Psoriasis, endogen bedingte Arthrosen und Depressionen). Wien Klin Wochenschr 66(43):829–832
Seegenschmiedt MH, Micke O (2012) Strahlentherapie nichtmaligner Erkrankungen. Vergangenheit, Gegenwart und Zukunft. Strahlenther Onkol 188(Suppl 3):272–290
Mücke R, Seegenschmiedt MH, Heyd R et al (2010) Strahlentherapie bei schmerzhafter Kniegelenkarthrose (Gonarthrose). Ergebnisse einer deutschen Patterns-of-Care-Studie. Strahlenther Onkol 186(1):7–17
Minten MJM, Mahler E, den Broeder AA et al (2016) The efficacy and safety of low-dose radiotherapy on pain and functioning in patients with osteoarthritis. A systematic review. Rheumatol Int 36(1):133–142
Merte H, Pfab R (1995) Strahlentherapie degenerativ-entzündlicher Gelenkerkrankungen im Alter. Eine lohnende Therapiemassnahme. Fortschr Med 113(22):323–324
Fischer U, Kamprad F, Koch F et al (1998) Effekte einer niedrig dosierten Co-60-Bestrahlung auf den Verlauf einer aseptischen Arthritis am Kniegelenk des Kaninchens. Strahlenther Onkol 174(12):633–639
Lindner H, Freislederer R (1982) Langzeitergebnisse der Bestrahlung von degenerativen Gelenkerkrankungen. Strahlentherapie 158(4):217–223
Krautzun K, Elingshausen HP (1955) Beitrag zur Röntgentherapie der Kniegelenkarthrosen. Strahlentherapie 96(1):82–85
Kern PM (2013) Wie Strahlen gegen Entzündung wirken. MMW Fortschr Med 155(1):47–48
Keller S, Müller K, Kortmann R‑D et al (2013) Efficacy of low-dose radiotherapy in painful gonarthritis. Experiences from a retrospective East German bicenter study. Radiat Oncol 8:29
Keller HL (1974) Röntgenbestrahlung bei Arthrosis deformans. Medizinische Klin 69(20):930
Kapatkin AS, Nordquist B, Garcia TC et al (2016) Effect of single dose radiation therapy on weight-bearing lameness in dogs with elbow osteoarthritis. Veterinary and comparative orthopaedics and traumatology. Vet Comp Orthopaed 29(4):338–343
Hess P, Bonmann KH (1955) Die Röntgentherapie der Arthrosen, Spondylosen, der Periarthritis humeroscapularis und der Epikondylitis. Strahlentherapie 96(1):75–81
Grosu AL (2001) Radiotherapie ausserhalb der Onkologie. Wann ist sie sinnvoll? MMW Fortschr Med 143(48):16 (interview by Waltraud Paukstadt)
Gibson TJ, Winter PJ, Grahame R (1972) Radiotherapy in the treatment of osteoarthrosis of the knee. Ann Rheum Dis 31(5):423–424
Fuchs G (1951) Zur Strahlenbehandlung der Arthrosis deformans. Wien Klin Wochenschr 63(16):295–296
Keim H (1965) Mitteilung über die Durchführung der Entzündungsbestrahlung mit dem Telekobaltgerät. Strahlentherapie 127:49–52
Weitmann HD, Niewald M (2013) Nicht nur bei Arthrosen erfolgversprechend. MMW Fortschr Med 155(1):43–46
Wieland C, Kuttig H (1965) Hochvolttherapie bei Arthrosen und Entzündungen. Strahlentherapie 127:44–48
Thurmayr R, Bohmert H (1966) Zur konservativen Behandlung der Arthrosis deformans. Vergleichende Untersuchungen über die therapeutische Wirksamkeit von Eleparon und Röntgenbestrahlungen. Munchener Medizinische Wochenschrift 108(4):213–216
Schertel L, Roos A (1968) Strahlenbehandlung bei degenerativen Skeletterkrankungen? Medizinische Klin 63(28):1112–1115
Schäfer U, Micke O, Seegenschmiedt HM et al (2010) Low-dose radiotherapy. Dtsch Arztebl Int 107(34-35):603–604
Schäfer U, Micke O, Willich N (1996) Schmerzbestrahlung bei degenerativ bedingten Skeletterkrankungen. Rontgenpraxis 49(10):251–254
Ruppert R, Seegenschmiedt MH, Sauer R (2004) Radiotherapie von Arthrosen. Indikation, Technik, klinische Ergebnisse. Orthopäde 33(1):56–62
Rossi F, Cancedda S, Leone VF et al (2018) Megavoltage radiotherapy for the treatment of degenerative joint disease in dogs. Results of a preliminary experience in an Italian radiotherapy centre. Front Vet Sci 5:74
Robson PN, van Miert PJ (1962) Treatment of osteo-arthritis of the hip by interstitial cobalt 60 irradiation. Br J Surg 49:624–636
Prokein B, Holtmann H, Hautmann MG et al (2017) Strahlentherapie des Fersensporns mit 2 Fraktionierungsschemata. Ergebnisse einer randomisierten Multizenterstudie nach 48 Wochen Follow-up. Strahlenther Onkol 193(6):483–490
Dietzel CT, Schäfer C, Vordermark D (2017) Erfolgreiche Behandlung der chronisch rekurrierenden multifokalen Osteomyelitis mit niedrigdosierter Radiotherapie. Ein Fallbericht. Strahlenther Onkol 193(3):229–233
von Pannewitz G (1970) Strahlentherapie der Arthrosis deformans. Technik und Ergebnisse. Radiologe 10(2):51–54
Keilholz L, Seegenschmiedt H, Sauer R (1998) Radiotherapie bei schmerzhaften degenerativ-entzündlichen Gelenkerkrankungen. Indikation, Technik und klinische Ergebniss. Strahlenther Onkol 174(5):243–250
Hautmann MG, Beyer LP, Süß C et al (2019) Strahlentherapie der Epicondylitis humeri. Analyse von 138 mit Linearbeschleuniger bestrahlten Ellenbogen. Strahlenther Onkol 195(4):343–351
Hautmann MG, Jung E‑M, Beyer LP et al (2019) Ist die Strahlentherapie eine effektive Behandlungsoption der Bakerzyste? Strahlenther Onkol 195(1):69–76
Micke O, Ugrak E, Bartmann S et al (2018) Radiotherapy for calcaneodynia, achillodynia, painful gonarthrosis, bursitis trochanterica, and painful shoulder syndrome—early and late results of a prospective clinical quality assessment. Radiat Oncol 13(1):71
Kaltenborn A, Bulling E, Nitsche M et al (2016) Relevanz der Feldgröße in der Reizbestrahlung bei Rhizarthrose. Relevanz der Feldgröße. Strahlenther Onkol 192(8):582–588
Minten MJM, Leseman-Hoogenboom MM, Kloppenburg M et al (2018) Lack of beneficial effects of low-dose radiation therapy on hand osteoarthritis symptoms and inflammation. A randomised, blinded, sham-controlled trial. Osteoarthr Cartil 26(10):1283–1290
Mahler EAM, Minten MJ, Leseman-Hoogenboom MM et al (2019) Effectiveness of low-dose radiation therapy on symptoms in patients with knee osteoarthritis. A randomised, double-blinded, sham-controlled trial. Ann Rheum Dis 78(1):83–90
Ott OJ, Micke O, Mücke R et al (2019) Low-dose radiotherapy. Mayday, mayday. We’ve been hit! Strahlenther Onkol 195(4):285–288
Riesterer O, Eberle B, Rogers S, Vogt DR (2019) Schmerz- und Funktionsverbesserung durch analgetische, entzündungshemmende Radiotherapie bei Patienten mit Fingerarthrosen, Epicondylitis radialis/ulnaris oder mit Fasziitis plantaris – Ergebnisse einer prospektiven single center Studie. Strahlenther Onkol 195(Suppl 1):49
Ott OJ, Niewald M, Weitmann H‑D et al (2015) DEGRO guidelines for the radiotherapy of non-malignant disorders. Part II. Painful degenerative skeletal disorders. Strahlenther Onkol 191(1):1–6
Ott OJ, Hertel S, Gaipl US et al (2014) The Erlangen Dose Optimization Trial for radiotherapy of benign painful shoulder syndrome. Long-term results. Strahlenther Onkol 190(4):394–398
Ott OJ, Jeremias C, Gaipl US et al (2015) Radiotherapy for benign achillodynia. Long-term results of the Erlangen Dose Optimization Trial. Strahlenther Onkol 191(12):979–984
Ott OJ, Hertel S, Gaipl US et al (2014) The Erlangen Dose Optimization trial for low-dose radiotherapy of benign painful elbow syndrome. Long-term results. Strahlenther Onkol 190(3):293–297
Arenas M, Sabater S, Hernández V et al (2012) Anti-inflammatory effects of low-dose radiotherapy. Indications, dose, and radiobiological mechanisms involved. Strahlenther Onkol 188(11):975–981
Hildebrandt G, Jahns J, Hindemith M et al (2000) Effects of low dose radiation therapy on adjuvant induced arthritis in rats. Int J Radiat Biol 76(8):1143–1153
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M.G. Hautmann, P. Rechner, M. Hipp, U. Neumaier, F. Steger, F. Pohl, M. Weber, O. Kölbl, and C. Süß declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Hautmann, M.G., Rechner, P., Hipp, M. et al. Re-irradiation for osteoarthritis—retrospective analysis of 217 joints. Strahlenther Onkol 195, 1060–1067 (2019). https://doi.org/10.1007/s00066-019-01500-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-019-01500-2