Abstract
Multiple treatment options and risk assessment in cerebrovascular diseases are the actual challenges in diagnostic as well as in interventional neuroradiology.
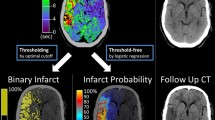
Acute ischemic stroke essentially requires rapid detection of the location and extent of infarction and tissue at risk for making treatment decisions. In the acute setting, modern multiparametric perfusion imaging protocols help to determine infarct core and adjacent penumbral tissue, and they enable the estimation of collateral flow of intra- and extracranial arteries. In subacute delayed cerebral ischemia (DCI) after subarachnoid hemorrhage (SAH) or chronic occlusive neurovascular diseases estimation of residual and collateral flow may be even more difficult.
Prediction of sufficient or insufficient supply of brain tissue may be essential to balance conservative against interventional therapies. However, so far no established reliable thresholds are available for determining tissue at acute, subacute, chronic progressive, or chronic risk.
Reliable and reproducible thresholds require quantitative perfusion measurements with a calibrated instrument. But the measurement instrument is not at all defined-a variety of parameter settings, different algorithms based on multiple assumptions and a wide variety of published normal and pathologic values for perfusion parameters indicate the problem. In the following text, we explain how deep the problem may be enrooted within techniques and algorithms impeding broad use of perfusion for many clinical issues.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Structural imaging in computed tomography (CT) and magnetic resonance imaging (MRI) is a standard and reproducible technique. Nevertheless, the imaging of anatomic structures does not reflect the dynamic function of the cerebrovascular system. Registration of irreversible structural damage in parenchymal imaging marks the endpoint of ongoing cerebrovascular decompensation. Optimal diagnostics should be able to detect the shift of the vascular dynamics to a defined threshold to prevent the onset of irreversible damage. Diagnostics of a dynamic system must be able to acquire and to measure dynamics.
The first technique giving temporal information of cerebral blood flow was intra-arterial catheter angiography. Dynamic information like circulation time, slope of arterial inflow, intensity of parenchymal blush over time, time of wash-out, and venous outflow can be obtained.
In 1956, Greitz [1] analyzed brain perfusion based on cerebral angiography. However catheter angiography is an invasive method with potentially severe complications (i.e., stroke, local complications at the puncture site, etc.).
Despite the possibility of CT or MRI to obtain fascinating structural insights into the human anatomy, initially there was a lack of visualization of in vivo function and dynamics. With faster CT and MRI imaging-techniques it was feasible to obtain dynamic information. While circulation time in angiography is well defined, results of mean transit time (MTT) in CT or MR-perfusion depend on the different acquisition methods (Table 1).
Under physiological conditions, normal brain perfusion is maintained within a narrow range by autoregulation of the cerebral vasculature. Normal cerebral blood flow (CBF) in human gray matter is about 50–60 ml/100 g per minute [2]. In cases of ischemic stroke due to vessel occlusion, the survival of brain tissue depends on the minimum necessary collateral supply from leptomeningeal anastomoses. Animal studies have shown that at a CBF below 35 ml/100 g per minute protein synthesis within neurons ceases completely [3]. In this oligemic stage, brain tissue can survive as long as CBF is not further reduced. If CBF further decreases below 20 ml/100 g per minute, normal neuronal interaction via synaptic transmission is no longer possible [4]. However, these neurons are still viable and the ischemic brain tissue that is “living” under these conditions adjacent to already irreversibly damaged tissue is defined as tissue at risk. If CBF decreases below 10 ml/100 g per minute, irreversible cell death occurs [4]. Thus an instrument is needed to measure those values in an individual patient. CT and MRI depict changes in density or signal-intensity caused by the passage of a contrast bolus. The resulting time-density curves allow to calculate perfusion parameters.
Dynamic CT scanning after intravenous injection of iodine contrast medium (CM) was already proposed in the early days of CT. The goal was to characterize tissue by extracting information from the temporal course of enhancement. In 1980, Axel [5] described a modelling algorithm to determine CBF by rapid-sequence CT; this was a milestone on the way to modern perfusion-studies. The actual techniques are still based on the idea of fast repetitive image acquisition during the first passage of a contrast bolus through the analysed organ [6, 7].
Comparing CT and MRI there is a fundamental physical difference: While the relation between tissue density/contrast-concentration and X-ray attenuation in CT is linear, the attenuation of signal intensity due to the paramagnetic effect of gadolinium in MRI follows a logarithmic curve. Consequently, the temporal change in MRI signal differs depending on the starting point on that logarithmic function: While the slope of the MRI signal intensity curve changes, the slope in CT imaging is constant. Thus, absolute quantification in MR-perfusion beside simple time determination results to be impossible. MR-Perfusion allows a relative intra-individual mapping of perfusion, but does not define interindividual thresholds for normal, reduced, critical, or insufficient perfusion. Moreover, MR signal intensity values are not absolute values as the Hounsfield units in CT. For that reason we focus on CT-Perfusion.
Technics of Perfusion-Data Acquisition
For CT-Perfusion, a temporal sequence of CT-slices renders the underlying necessary information (Fig. 1).
Sequence of computed tomography (CT) images (interslice time gap: 1 s). (a) The corresponding time–density curves show arrival of the contrast bolus in the arteries (red = arterial input function AIF), in the brain parenchyma (grey = tissue function TF), and in the veins (blue = venous outflow function VOF). (b) The schematic drawing top right shows a contrast-bolus (yellow) passing the vascular compartments from arteries (red) to veins (blue). The well-defined bolus seen in the arteries (red) becomes less defined (less contrast, wider) passing through the capillaries. When it reaches the veins (VOF) it is better visible but wider than in the arteries (AIF). (c) In the case of acute stroke, a perfusion deficit can be detected: In the posterior part of left middle cerebral artery territory TF arrival is later and broader. All curves show a second peak starting at 40 to 45 s due to recirculating contrast
In a typical and reproducible setting, time-density curves of the contrast-bolus passing the brain vascular structures from arteries via parenchyma to veins will be obtained depending on initial bolus definition and patient’s cardiovascular and cerebrovascular conditions. Using these data, the physical principle of fluid dynamics (Fick principle) and the dilution theory, the parameters defining brain perfusion may be calculated.
Later on, dedicated software were developed to analyze the time–density curves obtained from sequential CT scanning. A good understanding of the basic concept of perfusion analysis is essential to prevent dangerous mistakes.
Theory of CT-Perfusion
The underlying idea of visualizing cerebral perfusion is to evaluate the distribution of a visible substance over the brain parenchyma. Homogeneity and intensity (concentration) of this substance are surrogate factors that provide information about cerebral perfusion and potential perfusion deficits. The mathematical algorithms for delivering colored images encoding perfusion information are based on the indicator dilution theory [5, 8]. Common to all approaches that aim at the determination of cerebral blood flow is the intravenous injection of a usually short and compact bolus of contrast media (Fig. 2), the rapid sequential scanning of one representative slice or volume of the brain with appropriate temporal resolution and the application of a tracer kinetic model to either region-of-interest (ROI)-based or pixel-based time attenuation curves (TAC).
Indicator dilution theory is based on the assumption that the contrast bolus reaches maximal contrast within zero time (dotted green line = optimal bolus). The real bolus (green curve, injection volume: 30 ml contrast, rate 5 ml/s—injection time 6 s) deviates from that optimal bolus—but within a certain range a broader bolus may be used for calculations based on indicator dilution theory resulting in an acceptable error. After venous administration of the contrast bolus, the cardiopulmonary passage, arterial input function (AIF), and the further dilution of the contrast in parenchymal capillaries leads to flattening and widening of the curve resulting in a reduced signal to noise ratio of the curve compared with inhomogeneous signal of brain parenchyma. Only if the tissue curve (TF) exceeds the basal noise (BN) a reliable analysis is possible
The schematic model of a vascular structure (Fig. 1) illustrates the arteriovenous passage of an intra-arterial contrast-bolus and the corresponding time dependent intensity/density curves.
Depending on the vascular compartment analyzed, the same bolus shows different shapes starting with a well-defined short arterial bolus with a high slope of the curve. First changes of bolus curve result from dilution and deceleration in arterioles and capillaries (pictured as broadening of the total vessel diameter). The corresponding density curve is broadened and flattened compared to the initial arterial curve. In some parts of the parenchyma the bolus curve might even be more flattened and broader due to indirect collateral flow.
In order to meet the assumptions of the indicator dilution theory both the injection rate and the concentration of the contrast media should be as high as reasonably achievable. Using a total of 30 ml contrast volume at an injection rate of 5 ml/s and contrast medium with an iodine content of 350–400 mg/ml (preheated to body temperature) is an acceptable compromise clinical practice to achieve a high iodine flux and subsequently high quality CT Perfusion images.
In human brain perfusion not all parameters can be as exactly defined as in a physical experiment. To get the complex physiological system of brain perfusion close to the conditions defined in the principles mentioned above some assumptions have to be made. Either we presume that the contrast is diluted in a defined volume neglecting venous outflow, or we presume that the vascular compartment is completely separated from the extravascular compartment. Under assumption of a system without venous outflow the “maximum slope algorithm” is suitable; under assumption of a hermetically sealed system the “deconvolution algorithm” can be applied. Taking the blood–brain barrier into account and regarding only the first pass of contrast the assumption of a sealed system may not be too far from reality. Both algorithms result in a mathematically correct way to approximate both cerebral blood flow and cerebral blood volume. Hence, the resulting values are only approximate ones, because based on assumptions, and therefore different algorithms will result in different calculated values. As long as different algorithms leading to different results for cerebral blood flow and cerebral blood volume are used for CT Perfusion analysis, it will not be possible to define general thresholds for pathologic changes in cerebral perfusion.
The clinical users of perfusion software should decide concertedly which approximation to reality should be used in CT Perfusion. Otherwise the majority of our colleagues will call the fundamental added value of CT Perfusion into question.
Motion Artifacts
Especially in severely ill or disorientated patients, motion artifacts can result in unusable data. A pixel first located in the brain tissue may shift by movement to a location in an artery, resulting in a mixture of tissue and arterial function. Therefore, it is crucial to identify and correct motion artifacts.
Technical Parameters and Radiation Exposure
As mentioned above, perfusion CT consists of repetitive scanning of a specific volume. The examined volume depends on the width of the CT detector and usually is limited to a partial volume of the brain. Usually temporal sampling is 1 scan/s with 80 kV and 120 m as for a total scanning time of 40–45 s. In our setting of a single slice perfusion CT of patients after subarachnoid hemorrhage a 35 s acquisition time is sufficient. Radiation exposure under these conditions is 1.35 mSv (calculation: CT-Perfusion is based on two slices of 1 cm thickness. Based on an interscan interval of 1 s and scan duration of 35 s the total current-time-product is 4200 mAs). With a scan-distance of 20 mm (collimation 4 × 5 mm) the dose-length product is 588 mGy × cm with a Computed Tomography Dose Index (CTDIw) of 294 mGy. The effective dose is the result of multiplication with the weighting factor for the supraorbital head (“European Guidelines on Quality Criteria for Computed Tomography” (http://www.drs.dk/guidelines/ct/quality/htmlindex.htm Appendix I table 2) of 0.0023: 1.35 mSv).
For comparison, the diagnostic reference levels for diagnostic CT-scans of the neurocranium (http://www.bfs.de/SharedDocs/Downloads/BfS/DE/fachinfo/ion/drw-roentgen.pdf;jsessionid=B798D68703E2CE0BA77BE674FDDD3106.1_cid349?__blob=publicationFile&v=1) published by the German “Bundesamt für Strahlenschutz” give a CTDIvol of 65 mGy, resulting in a dose length product of 950 mGy × cm compared to 588 mGy × cm for CT-Perfusion in a 2 cm field. With the advent of CT scanners capable of continuously imaging almost the entire brain with repetitive low dose spiral scans (up to 14.4 cm z-axis coverage, leading to the term “volume perfusion CT” (VPCT)), a huge amount of anatomic vascular information is obtained with every VPCT scan (Fig. 3). Increasing the z-axis coverage of perfusion CT scans can improve the diagnostic sensitivity for detecting ischemic lesions [9, 10]. So far, diagnostic evaluation of VPCT examinations typically focused on functional abnormalities detected on perfusion parameter maps (i.e., cerebral blood volume, cerebral blood flow, mean transit time, and time to peak) whereas vascular reconstructions are not routinely obtained. With the advent of CT scanners allowing volumetric perfusion CT examinations of almost the entire brain, time-resolved 4-dimensional CT angiography (4D CTA) of the cerebral vasculature can be obtained in the same setting from the same data, to noninvasively study cerebral hemodynamics. Thus, occlusion of intracranial vessels, thrombus burden, and collateral blood flow can be visualized from the same VPCT source data that are used for perfusion parameter map analysis [11–14].
Usually, VPCT data are acquired using a periodic spiral approach consisting of 30 consecutive spiral scans of the brain (96 mm in z-axis, 1.5 s mean temporal resolution) for a total examination time of 45 s after injection of a short contrast bolus. For VPCT, we typically use 80 kV, 200 mAs, rotation time 0.3 s, maximum pitch 0.5, collimation 2 × 64 × 0.6 mm, 36 ml of highly iodinated contrast media at a flow rate of 6 ml/s followed by a 30 ml saline chaser at 6 ml/s. VPCT data are routinely reconstructed with a slice width of 5 mm every 3 mm for perfusion analysis and with a slice width of 1.5 mm every 1 mm for 4D CTA analysis. For VPCT, radiation exposure under the abovementioned conditions is approximately 5.2 mSv.
Volume perfusion computed tomography (VPCT) of a patient with an acute large right hemispheric infarction: area of reduced cerebral blood flow (CBF) (a); areas of prolongation of the time to peak (TTP) (b) time–density curves resulting from 3D-maximum intensity projection (MIP) (c) possible visualization of a penumbra (d-f) whereas nonviable tissue is coded red, brain parenchyma with reduced CBF but not yet severely reduced cerebral blood volume (CBV) is coded yellow. The threshold values for the color coding, however, can be set manually. (g) The non-enhanced computed tomography (CT) from the following day shows the demarcated infarct
Quantification of CT-Perfusion Maps
In acute stroke, of course, there are more than only temporal aspects that predict patient’s clinical outcome. Standardized quantitative perfusion might be a promising way to depict nonviable tissue and tissue at risk of irreversible infarction more precisely and therefore to predict clinical outcome after thrombectomy better than rigid time frames alone [15]. Today, successful neurointerventional recanalization of occluded vessels is not the question in acute stroke, but indication for recanalization might be better defined with the help of universal thresholds of perfusion parameters [16].
In subacute or more chronic cerebrovascular diseases (like cerebral perfusion disturbancies after subarachnoid hemorrhage (SAH)) definition of threshold may be even more important. In a retrospective analysis of 319 patients after SAH over a 4 year period [17], an excellent correlation between the long-term outcome of patients with SAH and the perfusion parameter MTT was shown [18]. More recently, data from another study showed that the perfusion parameter time to drain (TTD) is extremely helpful to recognize early perfusion changes in cerebral vasospasm and strongly correlates with spastic stenosis according to 4D CTA and conventional angiography [19]. Thus, the results of CT-Perfusion should be taken into account for decisions regarding further treatment (i.e., endovascular spasmolysis) in patients diagnosed with delayed cerebral ischemia (DCI).
Conclusion
CT-Perfusion is a diagnostic technique widely used in acute ischemic stroke and gaining more importance for other clinical settings as DCI after SAH or in neuro-oncology. Depicting cerebral perfusion changes using CT Perfusion increases diagnostic and therapeutic certainty in the acute setting. Similar to stroke MRI, CT-Perfusion enables the identification of tissue at risk by the mismatch between infarct core and a potentially larger area of critical hypoperfusion [20, 21]. Use of CT-Perfusion in the setting of subacute or chronic neurovascular diseases gains increasing relevance.
The clinical application remains far below the potential of CT-Perfusion could have as a reliable measurement instrument. A clear definition of X-ray parameters and bolus application is a requirement. As usual quality and reliability are the result of optimized conditions (contrast bolus with high injection rate and high iodine concentration). An accurate data handling including identification of artifacts and using motion correction (if necessary) is crucial. Radiation exposure may be minimized by using dose reduction protocols and confinement to absolute necessary number of slices.
Up to today different algorithms for estimation of perfusion parameters are applied based on completely different assumptions. Maximum slope model and deconvolution model are the most used algorithms. The underlying assumptions behind these algorithms induce different results from different software tools. One solution of that problem would be to define only one algorithm to calculate perfusion parameters based on clearly defined X-ray parameters and bolus-dynamics. A more practical or realistic solution is conversion formulas between the different algorithms.
In the future, better standardization techniques for absolute values in CT-Perfusion are necessary, due to the rising number of patients undergoing intra-arterial thrombectomy in acute ischemic stroke [22–24].
Conflict of Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
References
Greitz T. A radiologic study of the brain circulation by rapid serial angiography of the carotid artery. Acta Radiol Suppl. 1956;140:1–123.
Heiss WD. Ischemic penumbra: evidence from functional imaging in man. J Cereb Blood Flow Metab. 2000;20:1276–93.
Mies G, Ishimaru S, Xie Y, Seo K, Hossmann KA. Ischemic thresholds of cerebral protein synthesis and energy state following middle cerebral artery occlusion in rat. J Cereb Blood Flow Metab. 1991;11:753–61.
Astrup J, Siesjo BK, Symon L. Thresholds in cerebral ischemia—the ischemic penumbra. Stroke. 1981;12:723–5.
Axel L. Cerebral blood flow determination by rapid-sequence computed tomography. Radiology. 1980;137:679–86.
Klotz E, König M. Perfusion measurements of the brain: using dynamic CT for the quantitative assessment of cerebral ischemia in acute stroke. Eur J Radiol. 1999;30:170–84.
Wintermark M, Thiran JP, Maeder P, Schnyder P, Meuli R. Simultaneous measurement of regional cerebral blood flow by perfusion CT and stable xenon CT: a validation study. AJNR Am J Neuroradiol. 2001;22:905–14.
Meier P, Zierler KL. On the theory of the indicator-dilution method for measurement of blood flow and volume. J Appl Physiol. 1954;6:731–44.
Morhard D, Wirth CD, Fesl G, Schmidt C, Reiser MF, Becker CR, Ertl-Wagner B. Advantages of extended brain perfusion computed tomography: 9.6 cm coverage with time resolved computed tomography-angiography in comparison to standard stroke-computed tomography. Invest Radiol. 2010;45:363–9.
Page M, Nandurkar D, Crossett MP, Stuckey SL, Lau KP, Kenning N, Troupis JM. Comparison of 4 cm Z-axis and 16 cm Z-axis multidetector CT-Perfusion. Eur Radiol. 2010;20:1508–14.
Frölich AM, Psychogios MN, Klotz E, Schramm R, Knauth M, Schramm P. Angiographic reconstructions from whole-brain perfusion CT for the detection of large vessel occlusion in acute stroke. Stroke. 2012;43:97–102.
Frölich AM, Schrader D, Klotz E, Schramm R, Wasser K, Knauth M, Schramm P. 4D CT angiography more closely defines intracranial thrombus burden than single-phase CT angiography. AJNR Am J Neuroradiol. 2013;34:1908–13.
Frölich AM, Wolff SL, Psychogios MN, Klotz E, Schramm R, Wasser K, Knauth M, Schramm P. Time-resolved assessment of collateral flow using 4D CT angiography in large-vessel occlusion stroke. Eur Radiol. 2014;24:390–6.
Kaschka IN, Kloska SP, Struffert T, Engelhorn T, Gölitz P, Kurka N, Köhrmann M, Schwab S, Doerfler A. Clot burden and collaterals in anterior circulation stroke: Differences between single-phase CTA and multi-phase 4D-CTA. Clin Neuroradiol. 2014 Nov 20. [Epub ahead of print]
Psychogios MN, Schramm P, Frölich AM, Kallenberg K, Wasser K, Reinhardt L, Kreusch AS, Jung K, Knauth M. Alberta Stroke Program Early CT Scale evaluation of multimodal computed tomography in predicting clinical outcomes of stroke patients treated with aspiration thrombectomy. Stroke. 2013;44:2188–93.
Turowski B, Haenggi D, Wittsack HJ, Beck A, Aurich V. [Computerized analysis of brain perfusion parameter images]. Rofo. 2007;179:525–9.
Mathys C, Martens D, Reichelt DC, Caspers J, Aissa J, May R, Hänggi D, Antoch G, Turowski B. Long-term impact of perfusion CT data after subarachnoid hemorrhage. Neuroradiology. 2013;55:1323–31.
Caspers J, Rubbert C, Turowski B, Martens D, Reichelt DC, May R, Aissa J, Hänggi D, Etminan N, Mathys C. Timing of mean transit time maximization is associated with neurological outcome after subarachnoid hemorrhage. Clin Neuroradiol. 2015 May 5. [Epub ahead of print]
Dolatowski K, Malinova V, Frölich AM, Schramm R, Haberland U, Klotz E, Mielke D, Knauth M, Schramm P. Volume perfusion CT (VPCT) for the differential diagnosis of patients with suspected cerebral vasospasm: qualitative and quantitative analysis of 3D parameter maps. Eur J Radiol. 2014;83:1881–9.
Schramm P, Schellinger PD, Klotz E, Kallenberg K, Fiebach JB, Külkens S, Heiland S, Knauth M, Sartor K. Comparison of perfusion computed tomography and computed tomography angiography source images with perfusion weighted imaging and diffusion weighted imaging in patients with acute stroke of less than 6 hours duration. Stroke. 2004;35:1652–8.
Wintermark M, Rowley HA, Lev MH. Acute stroke triage to intravenous thrombolysis and other therapies with advanced CT or MR imaging: pro CT. Radiology. 2009;251:619–26.
Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, Schonewille WJ, Vos JA, Nederkoorn PJ, Wermer MJ, van Walderveen MA, Staals J, Hofmeijer J, van Oostayen JA, Lycklama à Nijeholt GJ, Boiten J, Brouwer PA, Emmer BJ, de Bruijn SF, van Dijk LC, Kappelle LJ, Lo RH, van Dijk EJ, de Vries J, de Kort PL, van Rooij WJ, van den Berg JS, van Hasselt BA, Aerden LA, Dallinga RJ, Visser MC, Bot JC, Vroomen PC, Eshghi O, Schreuder TH, Heijboer RJ, Keizer K, Tielbeek AV, den Hertog HM, Gerrits DG, van den Berg-Vos RM, Karas GB, Steyerberg EW, Flach HZ, Marquering HA, Sprengers ME, Jenniskens SF, Beenen LF, van den Berg R, Koudstaal PJ, van Zwam WH, Roos YB, van der Lugt A, van Oostenbrugge RJ, Majoie CB, Dippel DW; MR CLEAN Investigators. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372:11–20.
Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, Roy D, Jovin TG, Willinsky RA, Sapkota BL, Dowlatshahi D, Frei DF, Kamal NR, Montanera WJ, Poppe AY, Ryckborst KJ, Silver FL, Shuaib A, Tampieri D, Williams D, Bang OY, Baxter BW, Burns PA, Choe H, Heo JH, Holmstedt CA, Jankowitz B, Kelly M, Linares G, Mandzia JL, Shankar J, Sohn SI, Swartz RH, Barber PA, Coutts SB, Smith EE, Morrish WF, Weill A, Subramaniam S, Mitha AP, Wong JH, Lowerison MW, Sajobi TT, Hill MD; ESCAPE Trial Investigators Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372:1019–30.
Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, Yan B, Dowling RJ, Parsons MW, Oxley TJ, Wu TY, Brooks M, Simpson MA, Miteff F, Levi CR, Krause M, Harrington TJ, Faulder KC, Steinfort BS, Priglinger M, Ang T, Scroop R, Barber PA, McGuinness B, Wijeratne T, Phan TG, Chong W, Chandra RV, Bladin CF, Badve M, Rice H, de Villiers L, Ma H, Desmond PM, Donnan GA, Davis SM; EXTEND-IA Investigators. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372:1009–18.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Turowski, B., Schramm, P. An Appeal to Standardize CT- and MR-Perfusion. Clin Neuroradiol 25 (Suppl 2), 205–210 (2015). https://doi.org/10.1007/s00062-015-0444-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-015-0444-5