Abstract
Chronic obstructive pulmonary disease (COPD) primarily affects the lungs; however, cardiovascular conditions are among the most common extrapulmonary comorbidities. Besides shared risk factors such as cigarette smoking, pathophysiological connections between the lung and the heart have been identified as mediators of reduced cardiac output. Recent research has focused on hyperinflation of the lung as a pulmonary cause for heart dysfunction. Hyperinflation is a typical lung abnormality seen in COPD; it is characterized by increased residual volume, intrathoracic gas volume, and total lung capacity while vital capacity is decreased. The degree of hyperinflation with airway obstruction is inversely related to left ventricular filling, stroke volume, and cardiac output. The underlying mechanisms are assumed to be compression of the pulmonary veins and thus reduced preload of the left heart as well as decreased pulmonary microvascular blood flow due to compression of the pulmonary vasculature. Treatment with a dual bronchodilator antagonizes this detrimental lung–heart unbalance effectively: Pulmonary blood flow, left ventricular end-diastolic volume, and stroke volume increase in COPD patients without cardiac abnormalities. Similar effects, yet less pronounced, were reported with single bronchodilator therapy. Future work needs to investigate whether these promising findings can be reproduced in COPD patients with cardiovascular diseases.
Zusammenfassung
Die chronisch obstruktive Lungenkrankheit (COPD) betrifft in erster Linie die Atemwege, kardiovaskuläre Erkrankungen zählen jedoch zu den häufigsten Komorbiditäten. Neben gemeinsamen Risikofaktoren wie dem Rauchen tragen zusätzlich pathophysiologische Wechselwirkungen zwischen Lunge und Herz zu einer verringerten kardialen Auswurfleistung bei. Die aktuelle Forschung konzentriert sich v. a. auf die Lungenüberblähung als Ursache für eine reduzierte Herzleistung bei Patienten mit COPD. Die Überblähung ist eine für die COPD typische pulmonale Funktionsabweichung, die durch ein erhöhtes Residualvolumen, intrathorakales Gasvolumen und eine vergrößerte totale Lungenkapazität bei erniedrigter Vitalkapazität charakterisiert ist. Das Verhältnis zwischen dem Grad der Überblähung und linksventrikulärem enddiastolischem Volumen, Schlagvolumen und Auswurfleistung ist umgekehrt proportional. Dem zugrunde liegen vermutlich erstens eine Kompression der Pulmonalvenen, die zu einer verringerten linksventrikulären Vorlast führt, und zweitens eine Kompression des pulmonalen Kapillarbetts, die einen verminderten pulmonalen mikrovaskulären Blutfluss zur Folge hat. Die Behandlung mit einem dualen Bronchodilatator korrigiert dieses Ungleichgewicht zwischen Lunge und Herz in eine günstige Richtung: Pulmonaler Blutfluss, linksventrikuläres enddiastolisches Volumen und Schlagvolumen erhöhen sich bei überblähten COPD-Patienten ohne kardiale Vorerkrankungen. Ähnliche Effekte, jedoch schwächer ausgeprägt, lassen sich mit einer einfachen bronchienerweiternden Therapie erreichen. Eine zukünftige Forschungsaufgabe liegt darin zu untersuchen, ob sich ähnlich positive Ergebnisse bei COPD-Patienten mit kardiovaskulären Erkrankungen erzielen lassen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
COPD and cardiovascular dysfunction
Chronic obstructive pulmonary disease (COPD) plays a major part in morbidity and mortality worldwide. The burden of disease is high with 384 million cases, corresponding to a prevalence of 11.7% [1]. Moreover, COPD is the third leading cause of death globally [2]. Although COPD primarily affects the lungs, cardiovascular disease is the most common extrapulmonary comorbidity [3]. The mortality of COPD patients due to cardiovascular factors is higher than the mortality related to respiratory insufficiency and failure [4]. These patients have an increased risk for developing ischemic heart disease, heart failure, arrhythmias, peripheral vascular disease, and arterial hypertension, of which the latter is the most common cardiovascular comorbidity [5]. In part, this co-occurrence can be explained by shared risk factors such as cigarette smoking. Synergistically, the pathophysiologic consequences of inflammatory small-airway damage directly affect the cardiovascular system. Among them, exacerbations increase the risk of myocardial infarction in COPD patients with coronary artery disease. Also, they can contribute to the development of atrial fibrillation.
Pulmonary hypertension impairs right ventricular function, leading to dilation, hypertrophy, and the risk of atrial fibrillation. Another factor that adversely modulates the cardiovascular system is the striking neurohumoral activation that has been reported in COPD [6]. The resulting increased sympathetic activity is associated with more frequent hospitalization and premature death [7]. The pathogenesis of this increased sympathetic activity is multifactorial; hypoxia [8], impaired baroreflexes [9], and hyperinflation [10] have been described as triggers. Hyperinflation is thought to increase the wall tension of the left and right ventricle via a more negative pleural pressure [10, 11], thus leading to an increased sympathetic tone. Detrimental consequences include increased breathing frequency, dead-space ventilation and exertional dyspnea [12, 13], impaired endothelial function with decreased exercise-induced vasodilatation in skeletal muscles, a decrease in the number of type 1 slow muscle fibers, cardiomyocyte injury, apoptosis, muscle wasting, and reduced exercise capacity [6, 14, 15].
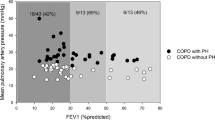
Hyperinflation is a major lung function abnormality characterized by an increased residual volume and intrathoracic gas volume as well as a decreased vital capacity. The resistance and compliance of the lung deteriorate, and gas exchange is compromised. Hyperinflation has been identified as an important factor contributing to the impairment of cardiac function in COPD (Fig. 1) [16]. For example, Barr et al. observed an inverse relationship between emphysema with airflow obstruction and left ventricular filling, stroke volume, and cardiac output [17]. More recently, Alter et al. demonstrated reduced diastolic filling in COPD subjects with emphysema and suggested a decrease in preload to be the underlying mechanism [18]. Substantial benefits are to be gained from investigating the connection between hyperinflation and impaired cardiac function in COPD, and how pharmacotherapy can positively intervene in this devastating relationship. The following section presents previous contributions and the latest insights in this field of COPD research.
Hyperinflation and impaired left heart function
The link between lung hyperinflation and reduced cardiac function has received much attention in recent years. Basically, it has long been acknowledged that in severe COPD with its high pulmonary vascular resistance and intrathoracic pressure exceeding venous pressure, reduced cardiac filling is a logical consequence. Yet Barr et al. demonstrated that airflow obstruction, as measured by spirometry, and extent of emphysema, as measured by computed tomography, are inversely related to left ventricular end-diastolic volumes, stroke volume, and cardiac output. Interestingly, these phenomena are also evident in patients with mild hyperinflation and no cardiac comorbidity [17]. The underlying mechanism is apparently more complex and still not fully understood.
Smith et al. observed that the pulmonary veins were compressed in patients with emphysema and proposed that left ventricular filling is lowered by reduced preload due to pulmonary—not cardiac—causes [19]. Confirming this assumption, Watz et al. described an impaired left ventricular diastolic filling pattern and an impaired global right ventricular function in hyperinflated patients [16]. This supports the concept of reduced preload in patients with emphysema, since left ventricular isovolumetric relaxation time was unaffected by hyperinflation, indicating no connection with left ventricular distensibility. Kohli et al. found that hyperinflated patients have a lower cardiac output, left and right ventricular end-diastolic volume, although the ejection fraction remained unchanged [20]. Another effect of COPD on the heart is decreased chamber sizes. Watz et al. observed that with increasing GOLD (Global Initiative for Chronic Obstructive Lung Disease) stage, all cardiac chamber sizes decrease [16]. The strongest association was seen between parameters of static hyperinflation (inspiratory-to-total lung capacity ratio) and chamber sizes. Another relevant aspect of lung dysfunction in COPD is the reduced pulmonary microvascular blood flow (PMBF). Aron et al. suggested that smoking-related pulmonary vascular changes such as hyperinflation might lead to compression of the pulmonary capillary bed [21]. They found an association between reduced total pulmonary vascular volume (TPVV) and decreased left ventricular end-diastolic volume (LVEDV), stroke volume, and cardiac output. Ventricular relaxation and ejection fraction were not impaired, again hinting at pulmonary causes. Besides hyperinflation-induced pressure increase, further pulmonary causes could be regional hypoxic vasoconstriction resulting in reduced blood flow to the left heart [21].
In summary, the association between COPD and reduced left ventricular function might be due to reduced blood flow caused by pulmonary vasculature damage as well as increased intrathoracic pressure compressing the pulmonary veins that supply the left heart with oxygenated blood from the lungs. Hyperinflation likely plays a major role in this pathophysiological process. These observations lead to the question of whether lung deflation might positively affect left ventricular function.
Impact of deflation
Long-acting bronchodilators, which are recommended as the pharmacological treatment of choice in COPD [5], effectively reduce gas trapping and thus antagonize hyperinflation [22, 23]. The parasympatholytic or sympathomimetic stimulation of muscarinic and beta-adrenergic receptors in the bronchial muscles facilitate relaxation, which stabilizes the bronchioles and prevents collapsing. This results in an improved air flow in the small airways und temporarily reduces hyperinflation for the duration of the drugs’ action. The deflation decreases the compression of the pulmonary microvasculature and consecutively pulmonary perfusion increases. As a consequence, cardiac filling also improves (Fig. 2).
Effect of lung deflation on left ventricular filling and cardiac output in patients with chronic obstructive pulmonary disease and hyperinflation. (© “Lung” from emcurious.com by Michael Macias/CC BY 4.0; © “Heart” from en.wikipedia.org by Drake/CC BY 2.0; Both pictures made transparent from original)
Santus et al. were the first group to examine the effects of single-bronchodilator-mediated deflation on cardiac function [24]. They observed improved right ventricular compliance indexes and a reduced heart rate in association with a decreased residual volume under treatment. Stone et al. added an inhaled corticosteroid (ICS) to the treatment regimen with a single long-acting beta2-agonist [25]. They reported an improved biventricular stroke volume, left atrial function, and pulsatility within the pulmonary circulation. Deflation led to a decompression of the pulmonary vasculature and heart, thus end-diastolic volume and consecutively stroke volume increased. However, Beeh et al. demonstrated, that a combination of a long-acting beta2-agonist (LABA) with a long-acting muscarinic receptor antagonist (LAMA) is superior to a LABA combined with an ICS in improving lung functioning [26]. Hence, Hohlfeld et al. recently investigated the effect of a combined LABA/LAMA treatment on cardiac functioning and hyperinflation in the CLAIM study [27]. Since bronchodilation is more pronounced under a dual treatment, it was assumed that the effects on deflation and consequently cardiac functioning would be more distinct. The study results confirmed this: The once-daily dual bronchodilator treatment for 14 days with indacaterol and glycopyrronium significantly reduced hyperinflation and airflow obstruction in COPD patients. Left ventricular end-diastolic volume increased by approximately 10%. The positive cardiac effects were stronger than previously shown in the aforementioned study by Stone et al.
Complementary to the assessment of lung and heart parameters, Vogel-Claussen et al. evaluated data on pulmonary microvascular blood flow obtained during the CLAIM study [28]. Besides deflation of the lung, the LABA/LAMA combination was able to remarkably improve pulmonary microvascular blood flow (PMBF). This improvement in pulmonary vasculature is significantly linked to the increased left ventricular end-diastolic volume. The authors presumed the positive effects to be mediated by an increased regional ventilation leading to reduced parenchymal hypoxia, improved endothelial function and vasodilation of the pulmonary vasculature. Moreover, the enhanced organ functioning under LABA/LAMA treatment translated into improved patient-reported outcomes as indicated by increases in health status and dyspnea during the CLAIM study. The magnitude of effect on symptoms and quality of life was greater compared with previous studies on indacaterol/glycopyrronium [29, 30]. While all participants suffered mainly from moderate-to-severe COPD, patients in the CLAIM study differed in their degree of hyperinflation because they were selected accordingly and they did not suffer from relevant cardiac abnormalities. Nonetheless, left ventricular end-diastolic volume obtained at baseline was near the lower limit of normal and cardiac function parameters significantly improved after lung deflation. The rise that was achieved with the LABA/LAMA treatment is likely to be beneficial in the long term even for patients with hyperinflation and COPD without distinct cardiovascular dysfunction.
Practical conclusion
Prior work has documented the connection between lung hyperinflation and impaired cardiac function; Watz et al., for example, reported reduced heart chamber sizes, impaired left ventricular diastolic filling pattern, and an impaired global right ventricular function in patients with hyperinflation and COPD . Pharmacological deflation with single-bronchodilator treatment increased left ventricular end-diastolic volume and decompressed the pulmonary vasculature. However, treatment with a dual bronchodilator surpassed the positive effects of a mono-therapy, confirming the substantial benefits of a strong bronchodilation in reducing air trapping and thus reversing hyperinflation. Furthermore, there is compelling evidence that dual bronchodilation improved pulmonary microvascular blood flow, which enhances organ functioning of the heart and lung. Although patient-reported outcomes regarding health status and dyspnea also improved under this therapy regimen, it still remains unclear whether the positive vascular changes are sustained over extended periods of time. Also, future research needs to explore whether these promising results can be extended to COPD patients with comorbid cardiac diseases.
References
Adeloye D, Chua S, Lee C et al (2015) Global and regional estimates of COPD prevalence: Systematic review and meta-analysis. J Glob Health 5(2):020415. https://doi.org/10.7189/jogh.05-020415
World Health Organization (2018) Global health estimates 2016: deaths by cause, age, sex, by country and by region. https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death
Sin DD, Anthonisen NR, Soriano JB et al (2006) Mortality in COPD: role of comorbidities. Eur Respir J 28(6):1245–1257. https://doi.org/10.1183/09031936.00133805
André S, Conde B, Fragoso E et al (2018) COPD and cardiovascular disease. Pulmonology. https://doi.org/10.1016/j.pulmoe.2018.09.006
The Global Initiative for Chronic Obstructive Lung Disease (2019) Global initiative for chronic obstructive lung disease 2019 report. https://goldcopd.org/wp-content/uploads/2018/11/GOLD-2019-v1.7-FINAL-14Nov2018-WMS.pdf
Andreas S, Anker SD, Scanlon PD et al (2005) Neurohumoral activation as a link to systemic manifestations of chronic lung disease. Chest 128(5):3618–3624. https://doi.org/10.1378/chest.128.5.3618
Andreas S, Haarmann H, Klarner S et al (2014) Increased sympathetic nerve activity in COPD is associated with morbidity and mortality. Am J Physiol 192(2):235–241. https://doi.org/10.1007/s00408-013-9544-7
Heindl S, Lehnert M, Criee CP et al (2001) Marked sympathetic activation in patients with chronic respiratory failure. Am J Respir Crit Care Med 164(4):597–601. https://doi.org/10.1164/ajrccm.164.4.2007085
Raupach T, Bahr F, Herrmann P et al (2008) Slow breathing reduces sympathoexcitation in COPD. Eur Respir J 32(2):387–392. https://doi.org/10.1183/09031936.00109607
Forfia PR, Vaidya A, Wiegers SE (2013) Pulmonary heart disease: the heart-lung interaction and its impact on patient phenotypes. Pulm Circ 3(1):5–19. https://doi.org/10.4103/2045-8932.109910
Smith BM, Kawut SM, Bluemke DA et al (2013) Pulmonary hyperinflation and left ventricular mass. Circulation 127(14):1503–1511e6. https://doi.org/10.1161/CIRCULATIONAHA.113.001653
Heistad DD, Abboud FM (1980) Dickinson W. Richards Lecture: Circulatory adjustments to hypoxia. Circulation 61(3):463–470
Coats AJ, Adamopoulos S, Radaelli A et al (1992) Controlled trial of physical training in chronic heart failure. Exercise performance, hemodynamics, ventilation, and autonomic function. Circulation 85(6):2119–2131
Grassi G, Seravalle G, Quarti-Trevano F et al (2009) Sympathetic activation in congestive heart failure: evidence, consequences and therapeutic implications. Curr Vasc Pharmacol 7(2):137–145
Haarmann H, Folle J, Nguyen XP et al (2016) Sympathetic activation is associated with exercise limitation in COPD. COPD 13(5):589–594. https://doi.org/10.3109/15412555.2015.1136272
Watz H, Waschki B, Meyer T et al (2010) Decreasing cardiac chamber sizes and associated heart dysfunction in COPD: role of hyperinflation. Chest 138(1):32–38. https://doi.org/10.1378/chest.09-2810
Barr RG, Bluemke DA, Ahmed FS et al (2010) Percent emphysema, airflow obstruction, and impaired left ventricular filling. N Engl J Med 362(3):217–227. https://doi.org/10.1056/NEJMoa0808836
Alter P, Watz H, Kahnert K et al (2018) Airway obstruction and lung hyperinflation in COPD are linked to an impaired left ventricular diastolic filling. Respir Med 137:14–22. https://doi.org/10.1016/j.rmed.2018.02.011
Smith BM, Prince MR, Hoffman EA et al (2013) Impaired left ventricular filling in COPD and emphysema: is it the heart or the lungs? The Multi-Ethnic Study of Atherosclerosis COPD Study. Chest 144(4):1143–1151. https://doi.org/10.1378/chest.13-0183
Kohli P, Neilan TG, Natarajan P et al (2014) Hyperinflation: a potential effect modifier of cardiovascular performance in individuals with chronic obstructive pulmonary disease and heart disease. Am J Respir Crit Care Med 189:A1125
Aaron CP, Hoffman EA, Lima JAC et al (2017) Pulmonary vascular volume, impaired left ventricular filling and dyspnea: The MESA Lung Study. PLoS ONE 12(4):e176180. https://doi.org/10.1371/journal.pone.0176180
Cazzola M, Mantero A, Santus P et al (2007) Doppler echocardiographic assessment of the effects of inhaled long-acting beta2-agonists on pulmonary artery pressure in COPD patients. Pulm Pharmacol Ther 20(3):258–264. https://doi.org/10.1016/j.pupt.2006.02.002
Beeh KM, Singh D, Di Scala L et al (2012) Once-daily NVA237 improves exercise tolerance from the first dose in patients with COPD: the GLOW3 trial. Int J Chron Obstruct Pulmon Dis 7:503–513. https://doi.org/10.2147/COPD.S32451
Santus P, Radovanovic D, Di Marco S et al (2015) Effect of indacaterol on lung deflation improves cardiac performance in hyperinflated COPD patients: an interventional, randomized, double-blind clinical trial. Int J Chron Obstruct Pulmon Dis 10:1917–1923. https://doi.org/10.2147/COPD.S91684
Stone IS, Barnes NC, James W‑Y et al (2016) Lung deflation and cardiovascular structure and function in chronic obstructive pulmonary disease. A randomized controlled trial. Am J Respir Crit Care Med 193(7):717–726. https://doi.org/10.1164/rccm.201508-1647OC
Beeh K‑M, Derom E, Echave-Sustaeta J et al (2016) The lung function profile of once-daily tiotropium and olodaterol via Respimat® is superior to that of twice-daily salmeterol and fluticasone propionate via Accuhaler® (ENERGITO® study). Int J Chron Obstruct Pulmon Dis 11:193–205. https://doi.org/10.2147/COPD.S95055
Hohlfeld JM, Vogel-Claussen J, Biller H et al (2018) Effect of lung deflation with indacaterol plus glycopyrronium on ventricular filling in patients with hyperinflation and COPD (CLAIM): a double-blind, randomised, crossover, placebo-controlled, single-centre trial. Lancet Respir Med 6(5):368–378. https://doi.org/10.1016/S2213-2600(18)30054-7
Vogel-Claussen J, Schonfeld C‑O, Kaireit TF et al (2019) Effect of Indacaterol/Glycopyrronium on pulmonary perfusion and ventilation in Hyperinflated COPD patients (CLAIM): a double-blind, Randomised, crossover trial. Am J Respir Crit Care Med. https://doi.org/10.1164/rccm.201805-0995OC
Vogelmeier CF, Bateman ED, Pallante J et al (2013) Efficacy and safety of once-daily QVA149 compared with twice-daily salmeterol-fluticasone in patients with chronic obstructive pulmonary disease (ILLUMINATE): a randomised, double-blind, parallel group study. Lancet Respir Med 1(1):51–60. https://doi.org/10.1016/S2213-2600(12)70052-8
Bateman ED, Ferguson GT, Barnes N et al (2013) Dual bronchodilation with QVA149 versus single bronchodilator therapy: the SHINE study. Eur Respir J 42(6):1484–1494. https://doi.org/10.1183/09031936.00200212
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Bauersachs’s, T. Welte’s and J.M. Hohlfeld’s institutions received grant support for conducting clinical studies on the impact of dual bronchodilation in COPD patients by Novartis Pharma GmbH. Moreover, they received personal honoraria for advisory boards and lectures from Novartis Pharma GmbH. N. Struß declares that she has no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies performed were in accordance with the ethical standards indicated in each case.
Rights and permissions
About this article
Cite this article
Struß, N., Bauersachs, J., Welte, T. et al. Left heart function in COPD. Herz 44, 477–482 (2019). https://doi.org/10.1007/s00059-019-4816-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-019-4816-5
Keywords
- Pulmonary disease, chronic obstructive
- Hyperinflation
- Bronchodilator effect
- Left ventricular function
- Cardiovascular disease