Abstract
Development of therapies aimed at inhibiting the angiogenesis, in combination with classical anti-cancer therapies, is among the most intensively studied approaches to the treatment of cancer. As a continuation of the efforts to discover and develop “4-aryl-4H-chromenes” as novel anti-cancer agents, in this study, we have been synthesizing (and examining) these compounds that appear to inhibit metastasis and, in particular, angiogenesis by using successful approaches such as three-dimensional capillary tube formation as well as matrix metalloproteinase (MMP) gelatinase assay in the endothelial cell-based experimental system. Anti-angiogenic and anti-proliferative effects of chromene compound 1 were especially checked on three-dimensional culture of human umbilical vein endothelial cells (HUVECs) in collagen matrix and HUVECs proliferation assay, respectively. Compound 1 was identified to be a highly potent anti-angiogenic agent at well-tolerated concentrations. In mechanistic studies, baseline MMP activities were inhibited in the presence of compound 1, in a dose-dependent manner. Based on our data, there is this possibility that chromene compounds (especially 1) are useful in treatment of some cancers because of their ability to both induce cancer cell apoptosis and reduce the stimulatory factors involved in HUVEC cell proliferation and angiogenesis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cancer cells are characterized by unlimited replicative potential, altered transcription of cell cycle genes, self-sufficiency in growth signals, insensitivity to antigrowth signals, sustained angiogenesis, abnormal vasculature, metastasis, and evasion of apoptosis (Hanahan and Weinberg, 2000; Plank and Sleeman, 2003). Since many tumor cells exhibit abnormality in cell cycle and apoptosis, there is a strong motivation for discovery and development of apoptosis inducers as potential anti-cancer drugs (Ribatti et al., 1999; Kemnitzer et al., 2007), although the emergence of drug-resistant tumor cells as well as dose-limiting levels of neurologic and bone marrow toxicity are two important limitations for their widespread use (Kasibhatla et al., 2004). Angiogenesis, the endothelial cell division/migration to form new capillaries, takes place primarily during development of the embryo and also, locally/transiently, is essential in many physiological processes such as ovulation, menstruation, and wound healing (Deplanque and Harris, 2000). This multi-step process is tightly controlled by a balance of angiogenesis inducers and inhibitors. Disregulated angiogenesis is seen in many pathological conditions such as diabetic retinopathy, rheumatoid arthritis, and psoriasis (Deplanque and Harris, 2000; Ribatti et al., 1999; Arenberg, and Strieter, 1999). Also, growth of solid tumors is not only angiogenesis-dependent but also uncontrolled (excessive) angiogenesis provide cancer cells a gateway through which they enter the circulation and metastasize to distant sites (Kuwano et al., 2001). However, in the malignant state, the growth rate of endothelial cells is considerably fast with doubling times as low as 7–10 days (Shepherd, 2001). Malignant angiogenesis depends on a switch in the tumor to the “angiogenic phenotype,” and this abnormal neovascularization is mediated via changing the balance of angiogenesis inducers and inhibitors by tumor cells (Kuwano et al., 2001; Folkman, 2003; Hanahan and Folkman, 1996). Angiogenesis inducers (such as VEGF, FGFs) may be paracrine from adjacent tumor/stromal cells or autocrine from endothelial cells themselves and increased level of them is often accompanied by decreased expression of endogenous inhibitors such as β-interferon (Singh et al., 1995; Volpert et al., 1998). The VEGF/bFGF-induced “angiogenesis switch” not only allows the growth of tumors but also favors metastatic dissemination (Deplanque and Harris, 2000; Kuwano et al., 2001). Since angiogenesis is a key process in the promotion of cancer and its metastasis (most common cause of cancer death in human), inhibition of angiogenesis is one of the promising approaches for treatment of tumor growth and metastasis. To date, major advances have been made to blocking malignant angiogenesis and encouraging clinical results, also, have been obtained (Nakao et al., 2008; Duncton et al., 2009; Yamashita et al., 2009; Gangjee et al., 2008; Chandrappa et al., 2010). The growing list of angiogenic inhibitors including natural and synthetic compounds (directed against VEGFs and their receptors), enzyme inhibitors and endogenous proteins have been approved and applied as effective agents for treating malignancy. However, according to the successful history of the identification of new, safe, and more effective drugs, there is room for improvement in this area (Deplanque and Harris, 2000; Nakao et al., 2008; Duncton et al., 2009). Furthermore, several anti-angiogenic agents have entered clinical trials, and there is a possibility that they will be applied as an alternate therapeutic weapon (Deplanque and Harris, 2000).
Recently, the anti-tumor efficacy of 4-aryl-4H-chromenes (Fig. 1), as effective apoptosis inducers, has been characterized (Kemnitzer et al., 2004, 2005, 2007). They were found to induce tubulin destabilization as well as to arrest cells at the G2/M stage (Kasibhatla et al., 2004; Kemnitzer et al., 2005) with high selectivity against proliferating versus resting cells. This series of compounds, also, were found as tumor vasculature targeting agents (Kasibhatla et al., 2004). By applying appropriate assays, we have reported that synthesized chromene compounds (especially compound 1, see Fig. 1) have potent anti-angiogenic activity. This study on the effects of chromenes (and chromanones) on human umbilical vein endothelial cell (HUVEC) angiogenesis behavior, is particularly novel and significant because to the best of our knowledge, no previous similar studies have been reported in this field. We found that compound 1 suppress HUVEC proliferation and formation of blood vessels at concentrations well below the cytotoxic dose.
Materials and methods
Chemicals, reagents, and materials
The chemical structure of test compounds, chromenes and chromanones, are summarized in Fig. 1 and Table 1, respectively.
Chemistry
2-Amino-3-cyano-7-(dimethylamino)-4-(2-methoxyphenyl)-4H-chromene (compound 1, see Fig. 1) was synthesized by the condensation of 3-(dimethylamino)phenol (a), 2-methoxybenzaldehyde (b) and malonitrile in ethanol in the presence of piperidine (Scheme 1). The structure of compound 1 was characterized by IR, 1H NMR, mass spectral data, and elemental analysis. The melting point was taken on a Kofler hot stage apparatus and is uncorrected. IR spectrum was recorded on a Shimadzu 470 spectrophotometer (KBr disk). 1H NMR spectrum was recorded on a Bruker FT-80 NMR spectrophotometer using CDCl3 as solvent and TMS as an internal standard. The purity of the compound was monitored by thin layer chromatography.
2-Amino-3-cyano-7-(dimethylamino)-4-(2-methoxyphenyl)-4H-chromene (compound 1)
Piperidine (10 mmol) was added to a mixture of 3-dimethylaminophenol (a, 5 mmol), 2-methoxybenzaldehyde (b, 5 mmol), and malonitrile (5 mmol) in ethanol (20 ml). The reaction mixture was stirred at 35°C for 12 h. After cooling, the precipitated solid was filtered, washed with cold ethanol, and crystallized from ethanol to give a yellow solid (yield = 44%); m.p. 196–197°C; IR (KBr) ν: 3420, 3290 (NH2), 2192 cm−1 (CN); 1H NMR (CDCl3): 7.20–7.18 (m, 1H, aromatic), 7.05–6.80 (m, 4H, aromatic), 6.45–6.24 (m, 2H, aromatic), 5.16 (s, 1H, 4H-chromene), 4.50 (br s, 2H, NH2), 3.84 (s, 3H, OMe), 2.90 (s, 6H, NMe2). Ms (m/z, %): 321 (M+, 75), 320 (74), 290 (36), 214 (100), 198 (35), 160 (16). Anal. (C19H19N3O2) C, H, N.
2-Amino-3-cyano-7-(dimethylamino)-4-(3-nitrophenyl)-4H-chromene (compound 2)
2-Amino-3-cyano-7-(dimethylamino)-4-(3-nitrophenyl)-4H-chromene (compound 2) was prepared by procedure similar to that described in literature (Kemnitzer et al., 2005, 2007).
2-Amino-3-cyano-7-(dimethylamino)-4-(3-trifluoromethylphenyl)-4H-chromene (compound 3)
2-Amino-3-cyano-7-(dimethylamino)-4-(3-trifluoromethylphenyl)-4H-chromene (compound 3) was also synthesized according to general method described previously (Kemnitzer et al., 2004; Foroumadi et al., 2007a, b).
The substituted 3-benzylidene-7-alkoxychroman-4-ones (compounds 4–14, Table 1) were synthesized as described by Foroumadi et al. (2007a, b). The test compounds were dissolved in DMSO, diluted with media and stored as the stock solutions with a concentration of 200 μg/ml at −20°C. The stocks of various compounds were diluted with medium to the desired concentrations. Rat tail collagen type I (at 2 mg/ml in 0.02 M acetic acid), MCD131 medium, DMEM, RPMI1640, and ConA were from Sigma chemical company (USA), fetal bovine serum (FBS), and 10× minimum essential medium (10× MEM) were purchased from Gibco. A dextran-coated cytodex-3 microcarrier was from Amersham Pharmacia Biotech. 1.4% (W/V) Sodium bicarbonate solution and NaOH (1 M sterile solution) were from Merck. Lactate dehydrogenase (LDH) cytotoxicity assay kit was from Roche chemical company. Gel reagents and all other chemicals were the highest analytical grade of purity available and were used without further purifications. All solutions were prepared with steriled double distilled water. Appropriate vehicle controls were run in all experiments.
Cell isolation/culture
Human umbilical vein endothelial cells were obtained from human umbilical vein of newborns using actinidin digestion method according to Mostafaie et al. (2008). In this way, written informed consent was obtained from all participating parents after careful explanation of the study. The isolated endothelial cells were started from frozen stock and grown on tissue culture-treated plastic in endothelial cell basal medium supplemented with 10% heat-inactivated FBS and maintained at 37°C with 5% CO2 until 90% confluent.
Preparation of collagen gels
Type I collagen from rat tail tendons was solubilized by stirring for 48 h at 4°C in a sterile 0.02 M acetic acid solution (Hata-Sugi et al., 2002). For collagen gel formation, seven volumes of cold collagen solution with one volume of 10× minimal essential medium and two volume of sodium bicarbonate solution (11.76 mg/ml) were mixed in a sterile flask kept on ice to prevent immediate gelation.
Cytotoxicity assay
To determine maximum non-toxic (and cytotoxic) concentrations of each test compound, several concentrations of compounds 1–14 (Fig. 1, Table 1) were added to medium containing confluent HUVECs. After 48 h of incubation, the effect of compounds on cell viability was determined by trypan blue exclusion and LDH assays (Gorman et al., 1996; Decker and Lohmann-Matthes, 1988). The absorbance of converted dye in LDH assay was measured at wavelength of 490 nm with background subtraction at 630 nm. The absorbance of treated cells was compared with the absorbance of the controls, which cells were exposed only to the vehicle (DMSO) and were considered as 100% viability value. The final concentration of DMSO in the test medium and controls was less than 1% throughout this investigation. Each concentration was tested in three independent experiments.
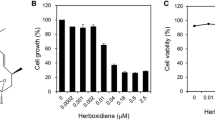
Anti-proliferation assay
Anti-proliferation assay was performed on HUVEC, as representative of microvascular endothelial cells, in MCDB131 medium (Sigma) supplemented with 10% FBS. Exponentially, growing cells were seeded in round-bottomed plates and allowed to attach overnight. After 24 h incubation at 37°C and 5% CO2, different amounts of the test compounds (1–14) were added, and the cells were exposed to drugs for additional 3 days. The cells were then harvested by trypsinization and counted against control wells by a coulter counter (KX-21 Sysmex Co). The IC50 values were calculated and represent the concentration of drug causing 50% inhibition in cell proliferation. Each point represents the mean value of triplicate.
HUVEC capillary tube formation in three-dimensional collagen gel and evaluation of angiogenesis in vitro
HUVEC cells were grown in MCDB131 medium supplemented with 10% FBS at 37°C and 5% CO2 and after 3–5 passages were used for this experiment. The cells were mixed with dextran-coated cytodex-3 microcarriers at a ratio of 30 HUVEC cells per bead in 1 ml of MCDB131 medium supplemented with 10% heat-inactivated FBS. Beads with cells were shaken gently every 20 min for 4 h at 37°C and 5% CO2. The mixture were transferred to four wells of a 24-well tissue culture plate and left for 12–16 h in 1 ml of MCDB131 at 37°C and 5% CO2. The following day, cell-coated beads were re-suspended (cultured) in type I collagen matrix and, for gel formation, were placed in 37°C/5% CO2 incubator, as described above. About 50 μl of collagen-bead mixture was added to each well of a 96-well tissue culture plate and allowed to clot for 20 min at 37°C and 5% CO2. About 250 μl of MCDB131 medium containing 10% FBS was added to each well, and HUVECs attached to cytodex were incubated with different concentrations of the test compounds. The plates were incubated at above conditions, and (for 3 days) anti-angiogenic effects of the test compounds were monitored daily, as demonstrated by the formation of microtubule structures, which were observed (counted) under a light microscope.
Gelatin zymography assay
The matrix metalloproteinase-2 (MMP-2) and MMP-9 gelatinolytic activities of conditioned media from HUVECs were assayed by electrophoresis (Toth and Fridman, 2001). Confluent HUVECs were isolated and immediately incubated in the absence of FBS with different concentrations of the test compounds for 16 h. Equal protein samples concentrated serum free culture medium of HUVECs treated with 1–16 μg/ml of test compounds, measured by the method of Bradford, were separated on 7.5% SDS-polyacrylamide gels containing 2 mg/ml (0.2%) gelatin under nonreducing conditions at 4°C (Bradford, 1976). PAGE gels were run at 120 V, renatured by exchanging SDS with 2.5% Triton X-100 for 1 h at room temperature, and then incubated for 16 h at 37°C in the activation buffer (50 mM Tris–HCl, pH 7.5, 10 mM CaCl2) for development of active bands. After staining with Coomasie brilliant blue R-250 (10% glacial acetic acid, 30% methanol, and 1.5% dye) for 2–3 h, the gel was destained with a solution of 10% glacial acetic acid, and 30% methanol for 1 h. The gelatinolytic activities were detected as transparent bands against the background of coomasie-stained gelatin. Positive control wells contained ConA, while negative controls contained tetracycline, as an angiogenesis inhibitor. Protein standards were run concurrently for determining the molecular weight of MMP bands. In a series of independent experiments, different concentrations of the test compound were added at (SDS to Triton) exchanging step for evaluating their direct inhibitory effects on MMP gelatinase activity.
Results and discussion
When well-developed tumors are treated with appropriate dose of a suitable angiogenesis inhibitor (e.g., Endostatin or Avastin), the tumors shrank dramatically (Scheme 2). It not only halt the development of new vessels, but may be also caused the destruction of blood vessels that had been formed earlier by the tumor. The cycle of tumor shrinkage (after administration of anti-angiogenesis agent) and expansion (due to treatment suspension) can be repeated several times, demonstrating that, unlike anti-proliferative chemotherapy, the tumor do not become resistant to renewed drug application. In addition, angiogenesis inhibitors target normal (and genetically stable) endothelial cells, not abnormal tumor cells, so it is not surprising that the involved individual fail to develop resistance to such agents. After a number of cycles of successful anti-angiogenic treatment, the tumor stops growing and remains as dormant microscopic cell clusters (Karp, 2002).
Schematic representation of the response of a solid tumor to treatment with angiogenesis inhibitor and chemotherapy (Karp, 2002)
The emergence of drug-resistant tumor cells (Scheme 2), as well as dose-limiting neurologic and bone marrow toxicity, however, has limited the use of chemotherapeutic (tubulin targeting) agents, such as Taxol and Vincristine (Kemnitzer et al., 2005). In contrast, the chromene compounds that induce apoptosis in cancer cells by targeting tubulin/microtubule system while retaining activity in multi-drug resistant tumors, have the potential to offer new treatment options in the field of oncology (Kemnitzer et al., 2004, 2005, 2007). According to data presented previously, 4-aryl-4H-chromenes with hydrophobic dimethylamino group at the 7-position and without substitutions at 5- and 6-positions (see structure of compounds 1–3) are potent apoptosis inducer agents (Kemnitzer et al., 2005). In addition, a subclass of substituted 4-aryl-4H-chromenes, as “vascular targeting agents,” was shown to preferentially disrupt preexisting tumor vasculature by targeting endothelial cells (Kasibhatla et al., 2004). As stated earlier, angiogenesis is a physiological process of new capillary formation, therefore, there is gross difference between “anti-angiogenesis” and “vascular targeting” activities. In this frame, with deciphering the many biological processes involved in cancer, development of therapies aimed at inhibiting both the tumor angiogenesis (vasculature) and apoptosis of malignant cells appears worthwhile. Based on the earlier reports on vascular targeting potency of 4-aryl-4H-chromenes, and to determine whether modification with different substitutes affects/improves the anti-angiogenic activity of chromenes, we decided to concentrate our exploration efforts on the 4-position (of 4-aryl-4H-chromenes) with different substituents on the phenyl ring and 2-OMe (1), 3-Nitro (2), and 3-CF3 (3) groups (Fig. 1) were selected to explore different aryls at the 4-position (Kemnitzer et al., 2004, 2005, 2007).
Reactive oxygen species (ROS) and free radicals, on the other hand, not only are required in many physiological processes such as phagocytosis, cell division, and collagen synthesis but also are involved in development of a wide spectrum of serious human diseases such as diabetes, neurodegenerative disorders, and cancer (Foroumadi et al., 2007a, b). In this way, there are several reports that agents with ROS neutralizing capability may be therapeutically useful in the prevention/control of these diseases. For instance, some 2-amino-4-aryl-3-cyano-7-(dimethylamino)-4H-chromenes have been shown to exhibit antioxidant activity. Also, the antioxidant activities of homoisoflavonoids (3-benzylidenechroman-4-ones) occur as natural products, as well as synthetic substituted 3-benzylidene-7-alkoxychroman-4-ones (4–14) has been well characterized (Foroumadi et al., 2007a, b). Although chromene and chromanone compounds have shown (potent apoptosis-inducing activity and) antioxidant effects, to date and to the best of our knowledge, there have been no reported studies on their anti-proliferative/anti-angiogenic activity on blood vessel’s endothelial cells (Foroumadi et al., 2007a, b). The aim of this study was to evaluate anti-angiogenic (and anti-proliferative) activities of synthetic chromene/chromanone compounds on HUVECs attached to cytodex microcarrier beads, in a quantitative in vitro assay of angiogenesis.
The maximum non-toxic concentrations of the test compounds varied in a wide range of concentrations. Addition of compounds 2–14 to culture medium containing confluent HUVECs, also, resulted in dose-dependent cytotoxicity (data not shown). The results also indicated that compound 1 was not cytotoxic up to 40 μg/ml as assessed by trypan blue and LDH cytotoxicity assays. Since ideal anti-angiogenesis drugs are expected to have effect against pathogenic angiogenesis without producing cytotoxicity in the target cells (HUVEC), and because, among chromene/chromanone compounds, only compound 1 had significant anti-angiogenic (and anti-proliferative) effect on HUVECs at non-toxic concentrations (1–40 μg/ml or 3.11–124 μM), it was selected to study in details and the other compounds (which were not only highly cytotoxic at 1–40 μg/ml concentration range but also had no anti-proliferative/angiogenic activity at their non-toxic concentration ranges) were excluded from further studies.
Proliferation of endothelial cells is an absolute requirement for angiogenesis. The compound 1 induced significant decrease in the proliferation of HUVEC in a dose-dependent manner (Fig. 2). Furthermore, this inhibitory effect did not result of cytotoxic effect, as assessed by trypan blue exclusion and LDH cytotoxicity assays, compared with controls (data not shown). Taking the results (Fig. 2) into account, it can be concluded that endothelial cell proliferation, as major prerequisite of angiogenesis, was suppressed in the presence of less than 10 μg/ml of compound 1. In addition, this compound was able to inhibit completely angiogenesis in HUVEC capillary tube formation model (Fig. 3f) at ~1 μg/ml concentration.
Anti-angiogenic activity of selected 4-aryl-4H-chromene (1) on in vitro HUVEC capillary tube formation. Spontaneous formation of capillary-like structures by HUVECs on “dextran-coated cytodex-3 microcarriers” was used to assess anti-angiogenic potential. a Angiogenesis of endothelial cells in the untreated wells (negative control). The endothelial cell attached to particles has been migrated through the collagen matrix. b–f Inhibition of angiogenesis of the endothelial cells treated by different (0.1, 0.2, 0.4, 0.8, and 1 μg/ml) concentrations of compound 1. Photomicrographs (×10 magnification) shown are representative example of three independent experiments. Further details are given in experimental procedures
The ability for endothelial cells to form tubular structures (on cytodex matrix) offers an in vitro model of angiogenesis. Within ~3 days of being seeded on carrier, HUVECs flattened into a reticular network and then form a mesh of capillary-like vessels (untreated controlled cells, Fig. 3a). In order to evaluate the possible effect of selected 4-aryl-4H-chromene (1) as angiogenesis inhibitor, increasing concentrations of compound 1 were added to endothelial cells. A dose-dependent anti-angiogenic behavior was observed and representative results are shown in Fig. 3a–f. As it is evident from figure, compound 1 was quite potent causing angiogenesis inhibition with complete suppression at 1 μg/ml.
Angiogenesis is tightly regulated by complex system of pro- and anti-angiogenic factors including growth factors and MMPs (Kappert et al., 2009; Göoz et al., 2009; Verma and Hansch, 2007). It is initiated by the release of proteases that allow degradation of the basement membrane and followed by proliferation/migration of endothelial cells. Once a tumor is established, interactions between stromal, tumor, and endothelial cells will trigger secretion/activation of various MMPs followed by degradation and invasion of the extracellular matrix (ECM) which permits tumor cell motility (within ECM) and metastases as well as facilitates budding of new blood vessels. To date, at least 26 human MMPs are known (Verma and Hansch, 2007). These MMPs are classified into collagenases, gelatinases, stromelysins, matrilysins, and membrane-type MMPs (Verma and Hansch, 2007). Metalloproteinases have attracted significant interest not only because they degrade the ECM molecules but because they also regulate growth factor signaling, cell adhesion, and release pro- and anti-angiogenic fragments of ECM proteins (Kappert et al., 2009; Göoz et al., 2009). Furthermore, most MMPs are secreted as zymogenes upon cytokine stimulation and require extracellular proteolytic activation. MMP-2 (gelatinase A, EC 3.4.24.24) and MMP-9 (gelatinase B, EC 3.4.24.35) have been extensively studied owing to their consistent association with tumor invasion and metastasis (Toth and Fridman, 2001; Verma and Hansch, 2007). In this way inhibition of expression, conversion and/or biological (enzymatic) function of these proteases may block angiogenesis both in vivo and in vitro (Kappert et al., 2009; Verma and Hansch, 2007). There is a possibility that compound 1 exerts its angiogenic activity (Fig. 3) via inhibition of MMP function. In this frame and to test this possibility, we examined the expression, conversion, or enzymatic function of MMPs in the presence or the absence of this chromene compound.
As shown by Fig. 4 (lanes 2–5), The MMP-9 activity was decreased in a dose-dependent manner, with an increase of compound 1 concentration. In addition, complete suppression of MMP-9 expression/activity was obtained in the presence of compound 1 at 8 μg/ml (24.88 μM) concentration. Also, at higher concentrations (12 μg/ml) of this chromene compound, abolished MMP-2 activity/expression was evident. These results suggested that the tested inhibitor is involved in the expression/activity of both MMP-9 and MMP-2. It is noteworthy that the same observations were made when compound 1 was added to the PAGE gel at renaturing step, confirming MMP-inhibitory property of this compound (data not shown). Taking the MMP-inhibitory data into account, it can be concluded that compound 1 act as a more potent MMP-9 inhibitor, compared to MMP-2. Also, there is about tenfold reduction in MMP-inhibitory/anti-angiogenic potency of compound, when compared to its caspase/apoptosis-inducing power (Kemnitzer et al., 2004). Further studies on subject including (study of MMP expression under the effect of compound, using RT-PCR technique) structure–activity relationship studies, are in process. In addition, it has been previously observed that proteolytic activity of some MMPs (MMP-2 and MMP-9) decreases cancer cell apoptosis via different mechanisms (Verma and Hansch, 2007). Then, inhibition of MMPs, in this context, may also have an additional apoptosis-inducing effect regarding to abnormal inhibition of apoptosis by cancer cells. Taking the results into account, anti-angiogenic activity of compound 1 is not only associated with a decrease in endothelial cell proliferation but also can be attributed to inhibition of MMP activity and/or interference of cytoskeleton organization (Scheme 3), which are known to play important roles in cell locomotion and capillary tube formation (Kemnitzer et al., 2005; Keshavarz et al., 2009, 2010). Furthermore, there is this possibility that chromene compound 1 both induces apoptosis in cancer cells and inhibits EC angiogenesis via targeting tubulin/cytoskeleton (as well as MMPs) system. In order to test this possibility, extensive experimental works are needed. Finally, it is worthwhile to differentiate whether compound 1 (2-amino-4-(2-methoxyphenyl)-3-cyano-7-(dimethylamino)-4H-chromene, see Fig. 1) is only an anti-angiogenesis factor or it has either vascular disrupting activity. It is noteworthy that 4-aryl-chromenes with methoxy substitution(s) at 4-position, have been identified as potent vascular disrupting agents (Cai et al., 2009; Kasibhatla et al., 2004). Vascular disrupting agents, which are a new class of potential anti-cancer drugs, disrupt preformed endothelial cell capillary tubules (Cai et al., 2009). Taking results of the current article and literature into account, it may be inspired that “methoxyphenyl” substitutes on the 4-position improve the anti-angiogenic activity of chromenes or there is this possibility that “methoxyphenyl”-containing 4-aryl-4H-chromenes display both vascular targeting and anti-angiogenesis activities. Further studies on this subject may provide deeper insights to screening for more effective anti-angiogenesis chromenes.
Gelatin zymography assay of extracellular MMP activity of HUVECs treated with increasing concentrations of compound 1, 3.11 (lane 2), 6.22 (lane 3) 12.44 (lane 4), 24.88 (lane 5), 37.32 (lane 6), and 49.76 (lane 7) μM. Lanes 1 and 8 represent the ConA (as positive control, note the relative induction of MMP-2 in response to ConA, at 5 μg/ml, compared to other lanes) and tetracycline (as negative control) effects on MMP activity, respectively (Toth and Fridman, 2001). Note the partial inhibition of MMP-2 (62–72 kDa) and complete suppression of MMP-9 (100 kDa), at 2 μg/ml of tetracycline (Kappert et al., 2009). MMP-9 was inhibited by moderate concentrations (between 4 and 8 μg/ml, see lanes 4 and 5) of compound 1. Complete inhibition of MMP-2 is shown with an excess amount (12–16 μg/ml, lane 6) of it. Unreduced molecular weight standards are not shown. Data shown are the representative zymogram from three independent experiments
The angiogenesis process includes endothelial cells migration, cell division, proliferation, and maturation which lead to vessel formation. Enzyme production, involved in extra cellular matrix modifying, is also a key process enabling endothelial cells to bud from extra cellular matrix. Chromene compounds (especially 1, see Fig. 1) are proposed to inhibit cancer development via different mechanisms a induction of cancer cell apoptosis, b inhibition of MMPs and extracellular matrix digestion which is an obligate prerequisite for migration of endothelial cells, and c suppress proliferation of endothelial cells (Ribatti et al., 1999)
Conclusions
The most common cause of cancer death in humans is metastasis of the primary tumor to distant sites, not growth of the primary tumor. The process of metastasis is aided by many features shared by tumors, including their ability to form new blood vessels, known as angiogenesis, to enhance their access to necessary nutrients from the host as well as to facilitate their spread into and through the vascular system (Kuwano et al., 2001). Thus, angiogenesis is a key process in the promotion of cancer and its metastasis. In this way, inhibition of angiogenesis is one of the promising approaches for treatment of tumor growth and metastasis. This study demonstrates that the test chromene (1), as multi-functional chemotherapeutic candidates, inhibits angiogenesis via its effect on EC proliferation and MMP activity, in addition to apoptosis-inducing behavior on malignant cells (Kemnitzer et al., 2005). We may also propose 4-aryl-2-amino-3-cyano-4H-chromenes, with one or more methoxy substitution(s) at 4-position, as potential anti-cancer agents with both apoptosis-inducing and also potent anti-angiogenic activity. With further in vivo studies, these (multi-functional anti-cancer) compounds may prove to be useful for not only palliative or curative treatment but also in the prevention of diseases in which the inhibition of angiogenesis could be beneficial (Zhang et al., 2007; Fife et al., 2000; Göoz et al., 2009).
Abbreviations
- PMSF:
-
Phenyl methyl sulphonyl fluoride
- MMP:
-
Matrix metalloproteinase
- VEGF:
-
Vascular endothelial growth factor
- bFGF:
-
Basic fibroblast growth factor
- EC:
-
Endothelial cell
- HUVEC:
-
Human umbilical vein endothelial cell
- FBS:
-
Fetal bovine serum
- DMSO:
-
Dimethyl sulphoxide
- ECM:
-
Extracellular matrix
- ConA:
-
Concanavalin A
- DMEM:
-
Dulbeccos modified minimum essential medium
- LDH:
-
Lactate dehydrogenase
- EC:
-
Endothelial cell
- VDA:
-
Vascular disrupting agent
- SAR:
-
Structure–activity relationship
- RT-PCR:
-
Reverse-transcriptase polymerase chain reaction
- SDS:
-
Sodium dodecyl sulfate
- MNTCS:
-
Maximum non-toxic concentrations
References
Arenberg DA, Strieter RM (1999) Angiogenesis. In: Serhan CN, Ward PA (eds) Molecular and cellular basis of inflammation. Humana Press, Totowa, pp 29–49
Bradford M (1976) A rapid and sensitive method for the quantification of microgram quantities of protein utilizing the principle of protein–dye binding. Anal Biochem 72:248–254
Cai XS, Drewe J, Kemnitzer W (2009) Discovery of 4-aryl-4H-chromenes as potent apoptosis inducers using a cell- and caspase-based anti-cancer screening apoptosis program (ASAP): SAR studies and the identification of novel vascular disrupting agents. Anticancer Agents Med Chem 9:437–456
Chandrappa S, Chandru H, Sharada AC, Vinaya K, Ananda Kumar CS, Thimmegowda NR, Nagegowda P, Karuna Kumar M, Rangappa KS (2010) Synthesis and in vivo anticancer and antiangiogenic effects of novel thioxothiazolidin-4-one derivatives against transplantable mouse tumor. Med Chem Res 19:236–249
Decker T, Lohmann-Matthes ML (1988) A quick and simple method for the quantitation of lactate dehydrogenase release in measurements of cellular cytotoxicity and tumor necrosis factor (TNF) activity. J Immunol Methods 115:61–69
Deplanque G, Harris AL (2000) Anti-angiogenic agents: clinical trial design and therapies in development. Eur J Cancer 36:1713–1724
Duncton MA, Piatnitski Chekler EL, Katoch-Rouse R, Sherman D, Wong WC, Smith LM II et al (2009) Arylphthalazines as potent, and orally bioavailable inhibitors of VEGFR-2. Bioorg Med Chem 17:731–740
Fife RS, Sledge GW Jr, Sissons S, Zerler B (2000) Effects of tetracyclines on angiogenesis in vitro. Cancer Lett 153:75–78
Folkman J (2003) Angiogenesis and apoptosis. Semin Cancer Biol 13:159–167
Foroumadi A, Dehghan G, Samzadeh-Kermani A, Arabsorkhi F, Sorkhi M, Shafiee A et al (2007a) Synthesis and antioxiodant activity of some novel 2-amino-4-aryl-3-cyano-7-(dimethylamino)-4H-chromenes. Asian J Chem 19:1391–1396
Foroumadi A, Samzadeh-Kermani A, Emami S, Dehghan G, Sorkhi M, Arabsorkhi F et al (2007b) Synthesis and antioxidant properties of substituted 3-benzylidene-7-alkoxychromsanon-4-ones. Bioorg Med Chem Lett 17:6764–6769
Gangjee A, Namjoshi OA, Yu J, Ihnat MA, Thorpe JE, Warnke LA (2008) Design, synthesis and biological evaluation of substituted pyrrolo [2, 3-d] pyrimidines as multiple receptor tyrosine kinase inhibitors and antiangiogenic agents. Bioorg Med Chem 16:5514–5528
Göoz P, Göoz M, Baldys A, Hoffman S (2009) ADAM-17 regulates endothelial cell morphology, proliferation, and in vitro angiogenesis. Biochem Biophys Res Commun 380:33–38
Gorman A, McCarthy J, Finucane D, Reville W, Gotter T (1996) Morphological assessment of apoptosis. In: Gotter TG, Martin ST (eds) Techniques in apoptosis. A user’s guide. Portland Press Ltd, London, pp 6–7
Hanahan D, Folkman J (1996) Patterns and emerging mechanisms of the angiogenic switch during tumorigenesis. Cell 86:353–364
Hanahan D, Weinberg RA (2000) The hallmarks of cancer. Cell 100:57–70
Hata-Sugi N, Kawase-Kageyama R, Wakabayashi T (2002) Characterization of rat aortic fragment within collagen gel as an angiogenesis model; capillary morphology may reflect the action mechanisms of angiogenesis inhibitors. Biol Pharm Bull 25:446–451
Kappert K, Meyborg H, Baumann B, Furundzija V, Kaufmann J, Graf K et al (2009) Integrin cleavage facilitates cell surface-associated proteolysis required for vascular smooth muscle cell invasion. Int J Biochem Cell Biol 41:1511–1517
Karp G (2002) Cellular and molecular biology, concepts and experiments. Wiley, New York, pp 671–702
Kasibhatla S, Gourdeau H, Meerovitch K, Drewe J, Reddy S, Qiu L, Zhang H, Bergeron F, Bouffard D, Yang Q, Herich J, Lamothe S, Xiong Cai S, Tseng B (2004) Discovery and mechanism of action of a novel series of apoptosis inducers with potential vascular targeting activity. Mol Cancer Ther 3:1365–1373
Kemnitzer W, Drewe J, Jiang S, Zhang H, Wang Y, Zhao J et al (2004) Discovery of 4-aryl-4H-chromenes as a new series of apoptosis inducers using a cell- and caspase-based high-throughput screening assay. 1. Structure–activity relationships of the 4-aryl group. J Med Chem 47:6299–6310
Kemnitzer W, Kasibhatla S, Jiang S, Zhang H, Wang Y, Zhao J et al (2005) 4-Aryl-4H-chromenes as a new series of apoptosis inducers using a cell- and caspase-based high throughput screening assay, structure–activity relationships of the 7,8-positions. Bioorg Med Chem Lett 15:4745–4751
Kemnitzer W, Drewe J, Jiang S, Zhang H, Wang Y, Zhao J et al (2007) Discovery of 4-aryl-4H-chromenes as a new series of apoptosis inducers using a cell- and caspase-based high-throughput screening assay. 3. Structure–activity relationships of fused rings at the 7, 8-positions. J Med Chem 50:2858–2864
Keshavarz M, Mostafaie A, Mansouri K, Shakiba Y, Mohamadi Motlagh HR (2009) Inhibition of corneal neovascularization with propolis extract. Arch Med Res 40:59–61
Keshavarz M, Mostafaie A, Mansouri K, Bidmeshkipour A, Mohammadi Motlagh HR, Parvaneh S (2010) In vitro and ex vivo anti-angiogenic activity of Salvia officinalis. Phytother Res (in press)
Kuwano M, Fukushi J, Okamoto M, Nishie A, Goto H, Ishibashi T et al (2001) Angiogenesis factors. Intern Med 40:565–572
Mostafaie A, Bidmeshkipour A, Shirvani Z, Mansouri K, Chalabi M (2008) A proper new collagenase for isolation of cells from different tissues. Appl Biochem Biotechnol 144:123–131
Nakao Y, Narazaki G, Hoshino T, Maeda S, Yoshida M, Maejima H et al (2008) Evaluating of antiangiogenic activity of azumamides by the in vitro vascular organization model using mouse induced pluripotent stem (iPS) cells. Bioorg Med Chem Lett 18:2982–2984
Plank MJ, Sleeman BDJ (2003) Tumour-induced angiogenesis: a review. J Theor Med 5:137–153
Ribatti D, Vacca A, Dammacco F (1999) The role of the vascular phase in solid tumor growth: a historical review. Neoplasia 4:293–302
Shepherd FA (2001) Angiogenesis inhibitors in the treatment of lung cancer. Lung Cancer 34:S81–S89
Singh RK, Gutman M, Bucana CD, Sanchez R, Llansa N, Fidler IJ (1995) Interferons alpha and beta down-regulate the expression of basic fibroblast growth factor in human carcinomas. Proc Natl Acad Sci USA 92:4562–4568
Toth M, Fridman R (2001) Assessment of gelatinases (MMP-2 and MMP-9) by gelatin zymography. Methods Mol Med 57:163–174
Verma RP, Hansch C (2007) Matrix metalloproteinases (MMPs): chemical–biological functions and (Q) SARs. Bioorg Med Chem 15:2223–2268
Volpert OV, Dameron KM, Bouck N (1998) A human fibrosarcoma inhibits systemic angiogenesis and the growth of experimental metastases via thrombospondin-1. Oncogene 14:1495–1498
Yamashita T, Nakao Y, Matsunaga S, Oikawa T, Imahara Y, Fusetani N (2009) A new antiangiogenic C24 oxylipin from the soft coral Sinularia numerosa. Bioorg Med Chem 17:2181–2184
Zhang S, Zhang D, Sun B (2007) Vasculogenic mimicry: current status and future prospects. Cancer Lett 254:157–164
Acknowledgments
The authors appreciate the joint financial support of this investigation by the research council of the Kermanshah University of Medical Sciences, Kermanshah, Iran and Tehran University of Medical Sciences, Pharmaceutical Sciences Research Center, Tehran, Iran. R. K. would like to acknowledge scientific help provided by Dr. H. Adibi (Department of Medicinal Chemistry, Faculty of Pharmacy, Kermanshah University of Medical Sciences).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Mansouri, K., Khodarahmi, R., Foroumadi, A. et al. Anti-angiogenic/proliferative behavior of a “4-aryl-4H-chromene” on blood vessel’s endothelial cells: A possible evidence on dual “anti-tumor” activity. Med Chem Res 20, 920–929 (2011). https://doi.org/10.1007/s00044-010-9418-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00044-010-9418-y