Abstract
Objectives
We examined changes in sleep-onset difficulties over time and associations with physical activity and screen time behavior among adolescents.
Methods
We used data from last four survey waves of the Health Behavior in School-Aged Children (HBSC) study (2002–2006–2010–2014). Multilevel logistic regression analyses were conducted to explore associations between regular sleeping difficulties, excessive screen time exposure and being insufficiently physically active (i.e., < 60 min daily) among 33 European and non-European countries.
Results
Findings indicate an increase in the prevalence of sleep-onset difficulties and in excessive screen time exposure and a small but significant increase in physical activity levels. Additionally, adolescents exceeding 2-h daily screen time had 20% higher odds of reporting sleep-onset difficulties, while no association was found for physical activity. The strength of the association between screen time and sleep-onset difficulties increased over time, which may reflect a change in type of screen time use (e.g., the increased use of easy accessible screens such as smartphones and tablets).
Conclusions
Effective strategies to reduce screen time are key to reverse the detrimental trend in sleep-onset difficulties among adolescents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescents, defined as young people between the age of 10 and 19 years old, have often been considered as having a low burden of disease and relatively good physical and mental health compared with other stages of the life course (Gore et al. 2011). Nevertheless, the period of adolescence is characterized by many changes, such as physical changes in weight, height and muscle mass, as well as changes in lifestyle behaviors (Christie and Viner 2005). A number of health-related behaviors (e.g., physical activity, sedentary behavior and nutrition and sleep) are shaped during adolescence and impact health during adolescence, but also have profound consequences for cardio-metabolic health during adulthood (Ekelund et al. 2012).
In 2014, Canadian researchers emphasized the importance of using a 24-h approach to study the link between several health behaviors and actual health status (Irish et al. 2014). This 24-h approach stresses the importance of all health behaviors performed in a day, including sleep, physical activity and sedentary behavior, to explain health outcomes. Sleep is an important health behavior as humans sleep approximately one third of a day (Irish et al. 2014), it impacts the circadian metabolic effects and allows the brain to rest and consolidate day experiences (Brand and Kirov 2011). Furthermore, insufficient sleep has been associated with bad mood, high blood pressure, increased risk of type II diabetes, higher engagement in risky behavior and drowsy driving and lower academic performances (Hysing et al. 2016; Owens 2014; Short et al. 2013).
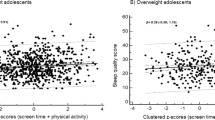
However, sleep has been largely neglected in the past as an important health behavior. The 24-h approach also emphasizes the need to better understand how waking behaviors such as physical activity and sedentary behavior are associated with sleep, as it is hypothesized that these behaviors are interrelated (Irish et al. 2014). For example, an association between screen time (a highly prevalent type of sedentary behavior) and sleep difficulties can partly be explained by the exposure to blue light, which increases the alertness of the individual and may induce difficulties in falling asleep (Boniel-Nissim et al. 2015; Nuutinen et al. 2013). The association between sleep and physical activity has been hypothesized to be bidirectional, i.e., engagement in physical activity is associated with better sleep, but evidence is also accumulating that poor sleep may also lead to lower physical activity levels (Kline 2014). The association between physical activity and sedentary behavior is not univocal, with some studies reporting an inverse association (Pearson et al. 2014; Tanaka et al. 2017), while others reported no association (Borraccino et al. 2009; Serrano-Sanchez et al. 2011). Recently, the interrelation between sleep, screen time and physical activity was tested within a large sample of English adults and showed that low physical activity levels, high screen time levels and poor sleep duration tend to cluster. The clustering of these three behaviors was much more prevalent in overweight or obese adults compared to a normal weight group, showing that these health behaviors are linked with obesity Cassidy et al. (2017). One recent U.S. study found that more daily screen time was associated with worse sleep quality, while lower physical activity was associated with more awakenings at night and higher sleep fragmentation among girls aged 7 to 12 years with a low socioeconomic status (Greever et al. 2017). Also, Chilean girls aged 12 years with low screen time and high physical activity levels reported lower prevalence of sleeping difficulties, compared to those with high screen time and low physical activity levels (Aguilar et al. 2015). Finally, a study among Chinese college students showed a positive association between screen time and sleeping difficulties, but no association was found between physical activity and prevalence of sleeping difficulties (Wu et al. 2015). However, large scale studies examining the association between these three behaviors in an international context are currently lacking. Additionally, no studies have explored this association among adolescents in a European context.
International trend analyses showed a strong increase in screen time among adolescents during the past decade, while physical activity levels generally remain low and efforts to increase physical activity seem to have small but positive effects on the prevalence of adolescents being sufficiently physically active (Bucksch et al. 2016; Inchley et al. 2017; Kalman et al. 2015; Nelson et al. 2006). Only limited information is available on how the prevalence of sleeping difficulties has changed during the past decade (Kronholm et al. 2015; Pallesen et al. 2008b). Since physical activity and screen time have been shown to be related to sleeping difficulties, it would be informative to describe the trends in sleeping difficulties together with the trends in physical activity and screen time.
Sleeping difficulties is a term which has been used in a wide range of contexts and can cover many problems related to bad sleep. The current study focusses on difficulties in falling asleep. Limited information is available on the prevalence of difficulties of falling asleep among adolescents. To the authors’ knowledge, there is only one paper which describes the changes in difficulties on falling asleep among a sample of Norwegian adolescents and found that prevalence increased significantly between 1983 and 2005 (Pallesen et al. 2008a). No evidence is available on how this prevalence might have changed during the last decade, how this might differ across countries, and limited information is available on factors associated with these problems with falling asleep. Therefore, the aim of the current study was twofold. First, we aimed to describe the prevalence of sleep-onset difficulties, insufficient physical activity and excessive screen time in 33 European countries between 2002 and 2014. Second, the aim was to examine the associations of physical activity and screen time with sleep-onset difficulties and whether these associations have changed over time and differ between countries.
Methods
Data from the four most recent waves of the Health Behavior in School-Aged Children (HBSC) (2002–2006–2010–2014) were used for the current analysis. The HBSC study is a large international study developed by an international network of researchers, in collaboration with the World Health Organization (WHO) Regional Office for Europe. The study aims to obtain insights into health behaviors and well-being among school children via a self-reported questionnaire which is repeated every 4 years (HBSC 2018).
The current study includes only those 33 countries/regions which participated in the four waves (Belgium—Flemish and French part; UK—Scotland, Wales and England). Sample selection protocols were described previously (HBSC 2018). Questionnaires, which were in the national language of the participating areas, were completed in schools by adolescents aged 11, 13 and 15 years. For the purposes of the current study, questions regarding physical activity, screen time and sleep-onset difficulties were included in the analyses, along with age, gender and material socioeconomic position, measured using the Family Affluence Scale (Currie et al. 2008). Physical activity was self-reported by the adolescents as the number of days of being physically active at moderate-to-vigorous intensity for 60 min in the past 7 days (range: 0–7) (Prochaska et al. 2001). Screen time behavior was measured by responses on three different questions (“How many hours a day, in your free time, do you usually spend watching TV, videos, DVDs, and other entertainment on a screen?”; “How many hours a day, in your free time, do you usually spend playing games on a computer, games console, tablet (like iPad), smartphone or other electronic device (not including moving or fitness games)?”; and “How many hours a day, in your free time, do you usually spend using electronic devices such as computers, tablets (like iPad) or smart phones for other purposes, for example, homework, emailing, tweeting, Facebook, chatting, surfing the internet?”) separately for week and weekend days. Nine response categories were possible, ranging from none at all to up to more than 7 h daily. These responses were treated as continuous and were thus recoded as follows: none at all = 0, half an hour a day = 0.5, about an hour a day = 1.0, etc. Average daily screen time was calculated by summing these three behaviors for week and weekend days separately, which were used to create a weighted average mean (= (5 × weekday + 2 × weekend day)/7 days) (Rey-López et al. 2010). Sleep-onset difficulties were assessed by a single item: “how often in the past six months did you have difficulties in falling asleep?” Response categories were “about every day,” “more than once a week,” “about every week,” “about every month” and “rarely or never.” The three behaviors were dichotomized to conform with the current international health guidelines for physical activity and screen time, i.e., being physically active for 7 days (1) or not (0) (World Health Organization 2011), exceeding 2-h daily screen time (1) or not (0) (American Academy of Pediatrics: Children, adolescents, and television 2001) and having difficulties in falling asleep “about every day/more than once a week” (1) or less (0) (Irish et al. 2014).
Analysis
First, prevalence (%) was calculated for each country/region (n = 33) for each survey year (2002, 2006, 2010, 2014) for not meeting the physical activity guidelines (= less than 7 days physically active for at least 60 min in last 7 days), exceeding screen time guidelines (= more than 2 h per day) and having regular sleep-onset difficulties (= about every day and more than once a week). Twelve-year differences were calculated (prevalence of behavior in 2014 − prevalence in 2002) and mapped on geographical areas (i.e., countries) to illustrate geographical differences in the changes over time, with the use of Tableau Software. A mean score was calculated per country if region information was available (i.e., Belgium and UK). Positive trends were marked green, while detrimental (unfavorable) changes were marked red. Second, a multilevel logistic regression model was fitted in R studio, using the lme4 package, in order to assess whether sleep-onset difficulties could be explained by exceeding the screen time guidelines and not reaching the physical activity guidelines. Adolescents were clustered within year by country units, which in turn were clustered within countries [i.e., three-level model (Fairbrother 2013)]. A stepwise model fitting approach was used, by first fitting a time effect model (model 1), and then age, gender and FAS were added (model 2). Age and FAS were centered around their mean. In order to be able to assess the relative rank within the socioeconomic hierarchy across different time points and cross-national contexts, FAS scores were transformed to ridits corrected for survey year, country, gender and age. A ridit is a proportional rank score that represents the proportion (P) of observations with lower scores plus one-half the proportion with equal scores \(\left( {{\text{Ridit}}_{j = } \sum\nolimits_{n = 1}^{j - 1} {P_{2n} } + \frac{{P_{2j} }}{2}} \right)\). Physical activity was added to model 2 (model 3a), followed by screen time (model 3b), and physical activity and screen time simultaneously (model 3c). In model 4a and model 4b, a random slope over country was allowed to test whether associations differed across countries, for physical activity and screen time, respectively. Finally, interactions between physical activity and time (model 5a), and screen time and time (model 5b) were tested to examine whether associations of physical activity and screen time with sleep-onset difficulties have changed over time. Model fit was compared using Akaike information criterion and Bayesian information criterion (AIC and BIC, respectively) values. Log-likelihood ratio tests were conducted to examine significant improvements/deteriorations in model fits. Significance was set at α < 0.05.
Results
Sample descriptives
Table 1 shows an overview of the sample descriptives across the 4 years. Age and sex distributions are comparable across survey years. Prevalence of sleep-onset difficulties and excessive screen time increased over time, while a small increase in the prevalence of sufficient physical activity can be observed. Additionally, an increase in mean daily screen time can be observed.
Descriptive trends in sleep-onset difficulties, physical activity and screen time
Different time trends can be observed across countries (see Table 2). Figures 1, 2 and 3 geographically illustrate the magnitude of the 12-year changes in sleep-onset difficulties, screen time and physical activity. In most countries, an increase in the prevalence of sleep-onset difficulties was observed over 12 years, except for Greece (− 4.3%), Spain (− 4.1%), Norway (− 2.0%), England (− 1.7%) and Portugal (− 1.3%). In 2014, on average around 20% of the adolescents had regular difficulties in falling asleep, but prevalence ranged from 9.6% in Ukraine to 37.4% in France.
Twelve-year change in the prevalence of insufficient physical activity, the Health Behavior in School-Aged Children (HBSC) survey, 2002–2014. Red color indicates detrimental evolutions. Green color indicates positive evolutions. The darker the color, the larger the 12-year change (color figure online)
For physical activity, 19 out of 33 countries (58%) showed a positive change over 12 years, i.e., decreases in the proportion of adolescents not being moderately or vigorously physically active every day (see Fig. 2). However, prevalence of insufficient physical activity was still very high across all countries with, on average, 80% of adolescents being insufficiently physically active in 2014 ranging from 89.9% (Italy) to 72.2% (Finland). It can also be observed that most countries improved their physical activity levels from 2002 to 2006, followed by a small decrease in physical activity in 2010 and again small increases in physical activity levels from 2010 to 2014.
Prevalence of exceeding the 2-h screen time/day has increased in almost all countries, except for Israel (− 1.6%) and Lithuania (− 27.7%) (see Fig. 3). Around 90% of the adolescents in the participating countries exceeded the guidelines of 2 h of daily screen time in 2014, ranging from 56.7% in Lithuania to 95.4% in the Netherlands. It can also be observed that countries with lower prevalence in 2002 had larger increases in their prevalence for excessive screen time (and vice versa, e.g., Israel), and differences between countries decreased over time. In 2014, prevalence of excessive ST was over 90% in 12 out of 33 countries.
Change in sleep-onset difficulties over time and the association with screen time and physical activity
Results of the multilevel logistic regression models are shown in Table 3. Model 1 shows a significant time trend for the odds of having regular sleep-onset difficulties. No differences were observed between 2002 and 2006, but a significant increase in odds was found for 2010 (OR = 1.102, 95% CI: 1.043–1.164) and 2014 (OR = 1.208, 95% CI: 1.145–1.275) compared to 2002. Adding sociodemographic variables to the model increased the model fit (model 2), i.e., age, gender and FAS were significantly associated with the odds of having regular sleep-onset difficulties. Adolescents aged 1 year older had 2.3% higher odds (95% CI: 1.019–1.027) of having sleep-onset difficulties. Higher affluent groups had 3.3% (95% CI: 0.964–0.970) lower odds of having sleep-onset difficulties compared to the lower affluent groups. Girls had 44.0% (95% CI: 1.421–1.458) higher odds to report sleep-onset difficulties. Adding conformity to the physical activity guidelines into the model (3a) only slightly improved the model fit, and physical activity was not significantly associated with sleep-onset difficulties. Adding conformity to the screen time guidelines to model 2 increased the model fit and illustrated a positive association between excessive screen time and the odds of sleep-onset difficulties (model 3b). Adolescents exceeding the guidelines for screen time had 20.1% (95% CI: 1.178–1.225) higher odds of reporting regular sleep-onset difficulties. In model 3c, both conformity to the physical activity and screen time guidelines were added simultaneously to the model and showed a slightly better model fit compared to model 3b in which only screen time was added. This model confirms that adolescents who exceeded the screen time guidelines had higher odds of reporting regular sleep-onset difficulties even after adjustment for physical activity. In model 4a and model 4b, a random country slope was added for physical activity and screen time, respectively, and each showed a significant increase in model fit [model 4a vs 3a Chi2 (2df) = 72.777, p < 0.001; model 4b vs 3b Chi2 (2df) = 54.22, p < 0.001]. This implies that the strength of the association between physical activity and screen time with sleep-onset difficulties differs significantly between countries. Finally, an interaction term for physical activity (model 5a) and screen time (model 5b) by time was added to the model. Model 5a showed a significant interaction between physical activity and time showing that the magnitude of the association between physical activity and sleep-onset changes over time, although in none of the years, the magnitude differed significantly from 1. The association between physical activity and sleep-onset difficulties was significantly larger in 2014 compared to 2002 (OR 2002 = 0.992, 95% CI: 0.976–1.010; OR 2006 = 0.991, 95% CI: 0.958–1.026; OR 2010 = 1.015, 95% CI: 0.981–1.095; OR 2014 = 0.971, 95% CI: 0.939–1.004). Model 5b illustrates that the association between screen time and sleep-onset difficulties got stronger over time (OR 2002 = 1.201, 95% CI: 1.178–1.225; OR 2006 = 1.163, 95% CI: 1.118–1.211; OR 2010 = 1.219, 95% CI: 1.170–1.270, OR 2014 = 1.419, 95% CI: 1.360–1.480). The magnitude of the association between screen time and sleep-onset difficulties increased each wave, and all waves did significantly differ from 2002 (see Table 3, model 5b).
Discussion
The current study was the first to describe co-occurrence of trends in sleep-onset difficulties, physical activity and screen time, and to examine the association between sleep-onset difficulties, physical activity and screen time among a large sample of mainly European adolescents.
Across the majority of countries, unfavorable changes were observed for screen time and sleep-onset difficulties, while physical activity levels slightly increased over time. Results indicated increases in the prevalence of sleep-onset difficulties over time [odds ranged between 1.208 (model 1) and 1.279 (model 4a)]. The prevalence of sleep-onset difficulties differed across gender (girls had 44% higher odds of reporting sleep-onset difficulties), socioeconomic groups (lower SES was associated with more sleep-onset difficulties) and age groups (older adolescents reported more sleep-onset difficulties). These differences in sleep-onset difficulties between sociodemographic groups were found in some previous studies (Lundqvist 2014; Wiklund et al. 2012). However, the existence of these differences needs further investigation. As sleep-onset difficulties may lead to the development of more serious sleeping disorders (e.g., impairment of sleep onset, sleep maintenance, premature final morning awakening and non-restorative sleep) and delayed sleep time disorders, it is important to identify appropriate strategies to decrease the prevalence of sleep-onset difficulties. For example, adolescent could be stimulated to develop consistent sleep schedules, given that adolescents with a schedule on both weekdays and weekends experience less difficulties in falling asleep than their counterparts with inconsistent sleep schedules (Mindell and Owens 2010).
Excessive screen time gets more prevalent over time, and in many countries, more than 90% of the adolescents exceeded the recommendations of 2-h screen time daily. This increase in excessive screen time was recently described in the HBSC International report 2014 (Inchley et al. 2017) and can be attributed to a rapid increase in computer/tablet/smartphone use for both gaming and non-gaming purposes. Although not investigated within the current study, it can be hypothesized that this increase is mainly explained by the increased use of smartphones among adolescents during the past few years (Škařupová et al. 2016). Smartphones are portable and accessible screen time devices, and especially when used before going to bed, they negatively influence sleep quality and quantity (Christensen et al. 2016). This shift in content of screen time may explain our finding that the strength of the association between screen time and sleep-onset difficulties increased over time.
The prevalence of sleep-onset difficulties was related to the prevalence of excessive screen time, but no association was found with physical activity, which is in contrast to findings of a previous study conducted in Switzerland, which found that high physical activity groups had less sleep-onset difficulties compared to low physical activity group (Lang et al. 2013). It might be that no association was found in our study due to our crude measure of physical activity. In-depth analyses illustrated that in some countries significant associations were found, with most of them being negatively associated with sleep-onset difficulties, but in some regions also positive associations were found (results not shown). More research including more detailed assessment of physical activity (e.g., time of the day, intensity and duration of physical activity) is needed to explore the association between physical activity and sleep-onset difficulties. It could be hypothesized that sleep quality or sleep quantity improves the night following the physical activity session, if it is not performed just before sleeping time (Kline 2014). However, such information is not available within the HBSC study. Similarly, no information was available on the timing of screen time, although it could be hypothesized that screen time right before bedtime may have the largest implications on difficulties in falling asleep (Hale and Guan 2015). In the current study, only difficulties in falling asleep were examined, while other elements related to sleep such as sleep duration, sleep quality, differences in sleep duration between week and weekend days, sleep hygiene and other sleep problems are also important to examine in future studies. Furthermore, more insights are needed in how associations might differ across countries and regions, as no overall association between physical activity and sleep-onset difficulties was found, but sub-analyses showed significant associations in some regions. Therefore, there is need for more in-depth study on physical activity and sleep, in order to prevent careless made conclusions that physical activity is not related to sleep/sleep problems.
Strengths and limitations
This study pioneered to present an international overview of trends over time in sleep-onset difficulties in a large international sample, highlighting an emerging health problem which has often been neglected in past health behavior studies. This study was limited to mainly European countries, and future studies should explore whether these trends are also observed in other regions such as the U.S. and Australia, and how associations may differ for in, for example, regions which are characterized by high mobile device use. Additionally, more insights are needed in the relationship between physical activity, screen time and other sleep-related health behaviors or outcomes, as this information was not available in the current study. A second limitation was the use of self-reported measures, which are prone to social desirability and recall bias. Also, screen time levels may have been somewhat overestimated in the current study, due to the co-occurrence of screen time activities. The use of objective measures which can assess both physical activity, screen time or sedentary behavior in general and sleep would overcome these limitations and allow researchers to further examine the 24-h approach. This may generate better understanding of the associations between these three behaviors as information on the specific moment of the day, intensity and duration of the activities can be obtained.
Conclusions
To conclude, findings of the current study indicate that sleep-onset difficulties are an emerging health problem. Additionally, findings suggest that interventions are needed to lower the prevalence of excessive screen time, which could lead to less difficulties in falling asleep among adolescents. However, more insights into the determinants of sleep-onset difficulties (and sleep in general) are needed, as screen time is only one pathway associated with sleep-onset difficulties, and little is known on other potential influencing factors.
References
Aguilar MM, Vergara FA, Velasquez EJA, Garcia-Hermoso A (2015) Physical activity, screen time and sleep patterns in Chilean girls. An Pediatr 83:304–310. https://doi.org/10.1016/j.anpedi.2014.12.006
American Academy of Pediatrics: children, adolescents, and television (2001) Pediatrics 107:423–426
Boniel-Nissim M et al (2015) International trends in electronic media communication among 11- to 15-year-olds in 30 countries from 2002 to 2010: association with ease of communication with friends of the opposite sex. Eur J Pub Health 25:41–45. https://doi.org/10.1093/eurpub/ckv025
Borraccino A et al (2009) Socioeconomic effects on meeting physical activity guidelines: comparisons among 32 countries. Med Sci Sports Exerc 41:749–756. https://doi.org/10.1249/MSS.0b013e3181917722
Brand S, Kirov R (2011) Sleep and its importance in adolescence and in common adolescent somatic and psychiatric conditions. Int J Gen Med 4:425–442. https://doi.org/10.2147/IJGM.S11557
Bucksch J et al (2016) International trends in adolescent screen-time behaviors from 2002 to 2010. J Adolesc Health 58:417–425. https://doi.org/10.1016/j.jadohealth.2015.11.014
Cassidy S, Chau JY, Catt M, Bauman A, Trenell MI (2017) Low physical activity, high television viewing and poor sleep duration cluster in overweight and obese adults; a cross-sectional study of 398,984 participants from the UK Biobank. Int J Behav Nutr Phys Act 14:57. https://doi.org/10.1186/s12966-017-0514-y
Christensen MA et al (2016) Direct measurements of smartphone screen-time: relationships with demographics and sleep. PLoS ONE 11:e0165331. https://doi.org/10.1371/journal.pone.0165331
Christie D, Viner R (2005) Adolescent development. BMJ: Br Med J 330:301–304
Currie C, Molcho M, Boyce W, Holstein B, Torsheim T, Richter M (2008) Researching health inequalities in adolescents: the development of the Health Behaviour in School-Aged Children (HBSC) family affluence scale. Soc Sci Med (1982) 66:1429–1436. https://doi.org/10.1016/j.socscimed.2007.11.024
Ekelund U, Luan J, Sherar LB, Esliger DW, Griew P, Cooper A (2012) Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. JAMA 307:704–712. https://doi.org/10.1001/jama.2012.156
Fairbrother M (2013) Two multilevel modeling techniques for analyzing comparative longitudinal survey datasets. Political Sci Res Methods 2:119–140. https://doi.org/10.1017/psrm.2013.24
Gore FM et al (2011) Global burden of disease in young people aged 10–24 years: a systematic analysis. The Lancet 377:2093–2102. https://doi.org/10.1016/S0140-6736(11)60512-6
Greever CJ, Ahmadi M, Sirard J, Alhassan S (2017) Associations among physical activity, screen time, and sleep in low socioeconomic status urban girls. Prev Med Rep 5:275–278. https://doi.org/10.1016/j.pmedr.2017.01.014
Hale L, Guan S (2015) Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep Med Rev 21:50–58. https://doi.org/10.1016/j.smrv.2014.07.007
Hysing M, Harvey AG, Linton SJ, Askeland KG, Sivertsen B (2016) Sleep and academic performance in later adolescence: results from a large population-based study. J Sleep Res 25:318–324. https://doi.org/10.1111/jsr.12373
Inchley J, Currie D, Jewell J, Breda J, Barnekow V (2017) Adolescent obesity and related behaviours: trends and inequalities in the WHO European Region, 2002–2014. World Health Organization Europe, Copenhagen
Irish LA et al (2014) A 24-hour approach to the study of health behaviors: temporal relationships between waking health behaviors and sleep. Ann Behav Med 47:189–197. https://doi.org/10.1007/s12160-013-9533-3
Kalman M et al (2015) Secular trends in moderate-to-vigorous physical activity in 32 countries from 2002 to 2010: a cross-national perspective. Eur J Public Health 25(Suppl 2):37–40. https://doi.org/10.1093/eurpub/ckv024
Kline CE (2014) The bidirectional relationship between exercise and sleep: implications for exercise adherence and sleep improvement. Am J lifestyle Med 8:375–379. https://doi.org/10.1177/1559827614544437
Kronholm E et al (2015) Trends in self-reported sleep problems, tiredness and related school performance among Finnish adolescents from 1984 to 2011. J Sleep Res 24:3–10. https://doi.org/10.1111/jsr.12258
Lang C, Brand S, Feldmeth AK, Holsboer-Trachsler E, Pühse U, Gerber M (2013) Increased self-reported and objectively assessed physical activity predict sleep quality among adolescents. Physiol Behav 120:46–53. https://doi.org/10.1016/j.physbeh.2013.07.001
Lundqvist L (2014) Socio-demographic variation in sleep difficulties among adolescents in Sweden. Stockholm, Stockholm University, Faculty of Social Sciences, Centre for Health Equity Studies (CHESS)
Mindell JA, Owens JA (2010) A clinical guide to pediatric sleep: diagnosis and management of sleep problems. Lippincott Williams & Wilkins, Philadelphia
Nelson MC, Neumark-Stzainer D, Hannan PJ, Sirard JR, Story M (2006) Longitudinal and secular trends in physical activity and sedentary behavior during adolescence. Pediatrics 118:e1627–e1634. https://doi.org/10.1542/peds.2006-0926
Nuutinen T, Ray C, Roos E (2013) Do computer use, TV viewing, and the presence of the media in the bedroom predict school-aged children’s sleep habits in a longitudinal study? BMC Public Health 13:684. https://doi.org/10.1186/1471-2458-13-684
Owens J (2014) Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics 134:e921–e932. https://doi.org/10.1542/peds.2014-1696
Pallesen S, Hetland J, Sivertsen B, Samdal O, Torsheim T, Nordhus IH (2008a) Time trends in sleep-onset difficulties among Norwegian adolescents: 1983–2005. Scand J Public Health 36:889–895. https://doi.org/10.1177/1403494808095953
Pallesen S, Hetland J, Sivertsen B, Samdal O, Torsheim T, Nordhus IH (2008b) Time trends in sleep-onset difficulties among Norwegian adolescents: 1983–2005. Scand J Public Health 36:889–895. https://doi.org/10.1177/1403494808095953
Pearson N, Braithwaite RE, Biddle SJ (2014) Associations between sedentary behaviour and physical activity in children and adolescents: a meta-analysis. Obes Rev 15:666–675. https://doi.org/10.1111/obr.12188
Prochaska JJ, Sallis JF, Long B (2001) A physical activity screening measure for use with adolescents in primary care. Arch Pediatr Adolesc Med 155:554–559. https://doi.org/10.1001/archpedi.155.5.554
Rey-López JP et al (2010) Sedentary patterns and media availability in European adolescents: the HELENA study. Prev Med 51:50–55. https://doi.org/10.1016/j.ypmed.2010.03.013
Serrano-Sanchez JA, Martí-Trujillo S, Lera-Navarro A, Dorado-García C, González-Henríquez JJ, Sanchís-Moysi J (2011) Associations between screen time and physical activity among Spanish adolescents. PLoS ONE 6:e24453. https://doi.org/10.1371/journal.pone.0024453
Short MA, Gradisar M, Lack LC, Wright HR (2013) The impact of sleep on adolescent depressed mood, alertness and academic performance. J Adolesc 36:1025–1033. https://doi.org/10.1016/j.adolescence.2013.08.007
Škařupová K, Ólafsson K, Blinka L (2016) The effect of smartphone use on trends in European adolescents’ excessive Internet use. Behav Inf Technol 35:68–74. https://doi.org/10.1080/0144929X.2015.1114144
Tanaka C, Tanaka M, Okuda M, Inoue S, Aoyama T, Tanaka S (2017) Association between objectively evaluated physical activity and sedentary behavior and screen time in primary school children. BMC Res Notes 10:175. https://doi.org/10.1186/s13104-017-2495-y
Wiklund M, Malmgren-Olsson E-B, Öhman A, Bergström E, Fjellman-Wiklund A (2012) Subjective health complaints in older adolescents are related to perceived stress, anxiety and gender—a cross-sectional school study in Northern Sweden. BMC Public Health 12:993. https://doi.org/10.1186/1471-2458-12-993
Health Behaviour in School-aged Children (HBSC) study (2018) About HBSC. http://www.hbsc.org/about/index.html. Accessed 15 Jan 2018
World Health Organization (2011) Global recommendations on physical activity for health 5–17 years old. World Health Organization, Geneva
Wu XY, Tao SM, Zhang YK, Zhang SC, Tao FB (2015) Low physical activity and high screen time can increase the risks of mental health problems and poor sleep quality among chinese college students. PLoS ONE 10:10. https://doi.org/10.1371/journal.pone.0119607
Acknowledgements
The International Coordinator of the 2002–2014 HBSC surveys was Candace Currie. Data Bank Manager was Oddrun Samdal.
Funding
The study was funded by the government of Flanders (Grant No. GEO-1GDD2A-WT) and the Research Foundation Flanders (Grant No. 12I1117N).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. HBSC is a WHO collaborative study and as such fulfills all WHO ethical requirements. The study is approved in each country separately by national or ministry ethical committees. The Flemish study was approved by the ethical committee of the University Hospital of Ghent (Project EC/2013/1145).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ghekiere, A., Van Cauwenberg, J., Vandendriessche, A. et al. Trends in sleeping difficulties among European adolescents: Are these associated with physical inactivity and excessive screen time?. Int J Public Health 64, 487–498 (2019). https://doi.org/10.1007/s00038-018-1188-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00038-018-1188-1