Abstract
Objective
The Mashhad stroke and heart atherosclerotic disorder (MASHAD) study is a 10-year cohort study that aims to evaluate the impact of various genetic, environmental, nutritional and psychosocial risk factors on the incidence of cardiovascular events among an urban population in eastern Iran.
Methods
The MASHAD study comprises a cohort of 9704 individuals aged 35–65 years using a stratified cluster random sampling design. This cohort will be followed up until 2020, with follow-up examinations being undertaken every 3 years. Ten-year cardiovascular disease (CVD) risk estimation was determined using NCEP ATP III criteria.
Results
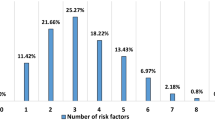
Overall, 88.4 % of women and 79.2 % of men (P < 0.001) had at least one lipid abnormality. The 10-year risk for CVD of <10, 10–20 and >20 % were observed to be 86.6, 11 and 2.5 %, respectively. Predicted risk of CVD > 10 % using the Framingham algorithm was considerably higher in men compared to women. Overall, 9.5 % [95 % confidence interval (CI) 8.9–10.1 %] of our subjects had prevalent CAD.
Conclusion
The prevalence of CVD risk factors within our population is high compared to Western countries, indicating the necessity for interventional risk modifications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease (CVD) is a major cause of morbidity and mortality globally (Husten et al. 1998; Dawber et al. 1957). The early identification of individuals at high risk of CVD allows timely intervention and is an important part of health policy in many countries. For example in the United Kingdom vascular risk screening has recently been introduced for individuals over 40 years of age (updated: The Handbook for Vascular Risk Assessment, Risk Reduction and Risk Management, 2012). It is now well recognized that cardiovascular disease has a complex, multi-factorial basis (Kuulasmaa et al. 2000; Smith et al. 2010; Uthoff et al. 2010; Schweigman et al. 2006). In recent years the global prevalence of CVD has changed significantly. Although it has been well documented that the mortality attributable to stroke and ischemic or coronary heart disease has declined in Western countries (Sytkowski et al. 1996; Beaglehole et al. 1997; Lloyd 1994; Ornish et al. 1998), its prevalence in many developing countries has increased substantially over the same period (Azarpazhooh et al. 2010; Monge and Beita 2000; Beaglehole 1993; Najeeb 1993). CVD now accounts for 47.3 % of all-cause mortality in Iran (Sarraf-Zadegan et al. 1999). Whilst there has been a decline in mortality related to infectious diseases as a result of improvement in health services, as in many other Asian countries, there has been an increase in CVD burden in Iran (Esteghamati et al. 2008; Kelishadi et al. 2008; Delavari et al. 2009; Harati et al. 2009; Hajian-Tilaki and Heidari 2007; Sarrafzadegan et al. 2010).
Few well-designed prospective studies have investigated risk factors of cardiovascular diseases in populations of developing countries such as those of the Middle East. An analysis of the clinical impact of the traditional and emerging CVD risk factors in a developing country would have implications for the global management of this chronic disease, and may provide insights into the risk of CVD among ethnic minorities living in the West. Data from the Mashhad Stroke Incidence Study (MSIS), a 1-year community-based incidence stroke study conducted in Mashhad (2006–2007), provided evidence for a relatively high incidence of stroke, which was also found to occur at a younger age, in Iran compared to those reported in Western countries (Azarpazhooh et al. 2010). However, the reason for these patterns of variations in our population is unclear. Genetic, ethnic and social differences, differences in the pattern of prevalent cardiovascular risk factors, and the systems that exist for managing them, may account for these variations. Furthermore, there has been no systematic attempt to examine genetic susceptibility and gene–environment interaction in a cohort from the Middle East. On this basis, we planned to conduct a large longitudinal cohort study, the Mashhad stroke and heart atherosclerotic disorder (MASHAD) study, the aim of which was to investigate the determinants and other risk markers of CAD and stroke in our population. The clinical endpoints for follow-up are CAD and stroke and participants will be followed for a period of at least 10 years. The specific aims of the project were to: (1) determine the prevalence of stroke and coronary disease and their biological, environmental, social, and behavior-related risk factors in a defined geographic area in north-western Iran; (2) identify characteristics related to the development of clinically evident CAD and stroke; (3) identify the association between various genetic and environmental risk indicators and cardiovascular and cerebrovascular disease endpoints; and (4) track the changes in CAD and stroke risk indicators during a period of at least 10 years.
The objective of the present paper is to describe the rationale, design and cross-sectional baseline characteristics of the cohort, as well as providing an estimate of 10-year CVD risk in this population.
Methods
The MASHAD study started in 2010 and will continue until 2020. The total population in the city of Mashhad was estimated using the national Iranian census in 2006. Participants were drawn from three regions in Mashhad, located in the north-eastern Iran, using a stratified cluster random sampling technique. Each region was divided into nine sites centered upon Mashhad Healthcare Center divisions. Households with individuals of eligible age between 35 and 65 years were identified and the local population authorities provided families with an information brochure of the study. Community leaders who were familiar with the families in the community also assisted with the identification and recruitment of potential participants. After identifying eligible participants, they were contacted to arrange an appointment for the formal physical examination. Eighty-two percent of subjects responded and agreed to enroll in the study. The non-responders (n = 2035) were contacted and information was sought regarding their demographic and socioeconomic profile and self-reported diabetes and hypertension status. Our primary analysis showed no significant differences in age and gender distribution of responders and non-responders.
The demographic, anthropometric and lifestyle data were collected and recorded by two certified health care professionals and a nurse. Our health-related questionnaires included (a) demographic data, physical exercise, tobacco and alcohol use, food frequency questionnaire (FFQ) and 24-h food record (b) anthropometric measurements, cardiovascular risk-related questionnaire and (c) anxiety and depression tests.
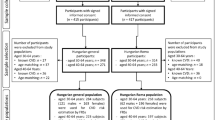
Study phases
Results from this cohort will be reported in two phases. In the first phase, we will report the cross-sectional data for all participants recruited into the study including those with and without history of CVD. In the second phase, after exclusion of prevalent cases of CAD, stroke and peripheral arterial disease, subjects will be followed for 10 years to determine the incidence rates of these disorders in our cohort of healthy individuals (Fig. 1). Individuals with medium and high risk will be given counseling about healthy diet, physical activity and smoking cessation. Those with elevated blood pressure, serum cholesterol, or other findings will be sent for medical follow-up. Any “alert” findings of conditions that should be medically evaluated on an urgent basis will be reported to the participant and his or her physician by telephone as soon as they were identified. In this present paper, we report the cross-sectional data for the prevalence of classic risk factors in our total participants based on a survey in 2010–2011.
Baseline examinations
Blood and mid-stream urine samples were collected from participants. Blood samples were taken between 8 and 10 a.m. by venepuncture of an antecubital vein after 14 h overnight fasting. The samples were collected in vacuum tubes (20 ml) from subjects in a sitting position, according to a standard protocol. All blood specimens were centrifuged at room temperature within 30–45 min of collection to separate the serum and plasma into six aliquots (0.5 ml), which were then sent to the Bu Ali Research Institute, Mashhad. Aliquots of serum were also kept frozen at −80 °C for future analysis. Low-density lipoprotein cholesterol (LDL-C) was calculated from the serum total cholesterol (TC), triglycerides (TGs), and high-density lipoprotein cholesterol (HDL-C) concentrations expressed in mg/dl using Friedewald formula (Castelli et al. 1986) if serum TGs concentrations were lower than 400 mg/dl. A baseline 12-lead electrocardiogram (ECG) was undertaken for each participant. All ECGs were scored blindly using the Minnesota codes, and were stored digitally for subsequent analysis. Dyslipidemia was defined as TC ≥ 200 mg/dl (5.18 mmol/l), LDL-C ≥ 130 mg/dl (3.36 mmol/l), or TG ≥ 150 mg/dl (1.69 mmol/l), or HDL-C < 40 mg/dl (1.03 mmol/l) in men and <50 mg/dl (1.30 mmol/l) in women (2002).
Diabetes mellitus was defined as a FBG ≥ 126 mg/dl or being treated with existing oral hypoglycemic agents or insulin treatment. According to the World Health Organization recommendations for obesity, (25 ≥ BMI > 25 kg/m2) was defined as overweight and (BMI ≥ 30 kg/m2) was considered as obese. Truncal obesity was defined as a WHR ≥ 0.95 in men and a WHR ≥ 0.8 in women. Based on International Diabetes Federation (IDF) cut-off points, WC ≥ 94 cm in men and ≥80 cm in women were considered high. Hypertension was diagnosed in individuals with systolic blood pressure at or above 140 mmHg and/or diastolic blood pressure at or above 90 mmHg, and in persons who were on anti-hypertension medication.
According to the World Health Organization (WHO) definition, stroke is defined as “rapidly developing signs of focal or global disturbance of cerebral function lasting >24 h with no apparent cause other than of vascular origin (Hatano 1976). The presence of coronary heart disease was established by a history of myocardial infarction or angina pectoris or electrocardiographic evidence for a definite Q wave using the Minnesota Code. A current smoker was defined as smoking cigarettes at least once a day. An ex-smoker was formerly a daily smoker, but someone who currently did not smoke. Data for non-cigarette smoking were also obtained. Psychometric tests were performed using the Beck’s anxiety inventory (BAI) to calculate an anxiety score that is explained as follows: a 0–7, minimal level of anxiety; 8–15, mild anxiety; 16–25, moderate anxiety and 26–63, severe anxiety. The Beck’s depression inventory II (BDI-II) was also used to evaluate depression. The cut-offs used were as follows: 0–13, minimal depression; 14–19, mild depression; 20–28, moderate depression; and 29–63, severe depression.
Statistical analysis
Data collected at the field centers were transmitted to the data bank using Microsoft visual studio.NET software which is exclusively designed for data management in MASHAD study. Descriptive analysis was used to process the outcomes in tables and graphs. Values were expressed as mean ± SD for normally distributed variables. Baseline demographics and clinical characteristics were compared between groups using independent samples t test, Chi-square and/or Fisher’s exact test, as appropriate. Prevalence rates are reported as the crude and age-standardized rates using WHO population data. Sex-specific estimates for determining the 10-year risk for developing CVD was carried out using a modified Framingham risk scoring according to the NCEP ATP III for participants without self-reported CVD or CVD equivalent (heart attack and angina pectoris, stroke, peripheral vascular disease and diabetes). Risk scores were calculated to determine the 10-year absolute risk. Three levels of risk were defined as <10, 10–20, and >20 %. Patients with CVD or a CVD risk equivalent were considered to be at very high risk for sustaining an acute cardiovascular event. SPSS software (version 15, Chicago, IL, USA) was used for statistical analysis. For all analyses, statistical significance was assessed at a level of 0.05 (two-tailed) and P value less than 0.05 was considered significant.
Follow-up
It is intended that the subjects recruited into the MASHAD study will be monitored for at least 10 years and will be contacted at 3-yearly intervals to reduce the risk of losing contact. They will be asked to complete the follow-up questionnaire to identify any changes in their state of health and lifestyle. A follow-up analysis will be performed every 3 years. However, certain data will be collected more frequently as required for the particular sub-projects. Morbidity and mortality data and myocardial infarction (MI) and stroke rates are being collected regularly from the reference community.
Ethics
Documents explaining the study were provided to the participants before enrollment. Moreover, a 10-min face-to-face explanation was provided for groups of individuals. Each item for agreement was explained individually to obtain a written consent for those who agreed to participate in the study. The study was approved by the Ethic Committee of Mashhad University of Medical Sciences.
Results
There were a total of 9761 participants, of whom approximately 40 % were males and 60 % females. Table 1 shows the age distribution of our participants by gender.
Sociodemographic findings
The mean age was 48.1 years in the total population, while men were slightly older than women (48.9 vs 47.6 years). Table 2 shows the socioeconomic status of the participants. Overall, 61 were single, 9083 were married, 135 were divorced and 474 were widowed.
Among participants, 305 (7.8 %) of men and 1027 (17.5 %) of women were illiterate.
Of the male population, 2866 (73.4 %) were employed and 700 (17.9 %) were retired. Among the female population, 706 (12 %) were employed and 252 (4.3 %) were retired. Smoking was more prevalent among males. Approximately, 28.5 % of men and 18 % of women were current smokers and 13.9 % of men and 6.3 % of women were ex-smokers. While 75.7 % of women were never-smokers, only 57.5 % of men had never been smokers in the past.
Blood biochemistry
Baseline biochemical values of participants are shown in Table 3. Overall, 23.7 % of our total population had elevated blood pressure (SBP ≥ 140 and/or DBP ≥ 90 mmHg). The prevalence of raised BP was higher among men compared to women (24.4 vs 23.3 %) (Table 4). The higher prevalence of HTN among men as compared to women was more pronounced for the two extremes of age groups (35–39 and 60–65 age group) (Table 4). Fourteen point one percent of the total population sample were diabetics; the prevalence of DM was higher in women as compared to men (14.5 vs 13.5 %). We observed an increasing prevalence of DM across age groups and women 60–65 years old had the highest prevalence of DM (27.3 %). Lipid profile disturbances were also significantly higher in women. Overall, 88.4 % of women and 79.2 % of men (P < 0.001) had at least one lipid abnormality to be categorized as dyslipidemic. The mean level of serum TC was 186.4 ± 38.1 in men and 194 ± 40.3 mg/dl in women. At-risk values of serum TC (>200 mg/dl) were significantly more prevalent in women than in men (41.5 vs 34 %, P < 0.001). Serum TG levels were significantly higher in men than in women (124.03 vs 117 mg/dl, P < 0.001). A high serum TG level (>150 mg/dl) was present in 36.9 % of men and 31.8 % of women (P < 0.001). The mean level of serum LDL-C was 113.5 ± 35.5 mg/dl in men and 118.1 ± 36.1 mg/dl in women (P < 0.001). Ten point five percent of our total population sample had an elevated serum LDL-C (>160 mg/dl), whilst the prevalence of an elevated serum LDL-C was significantly higher in women than in men (11.8 vs 8.6 %, P < 0.001). Women in 60–65 age group had the highest levels of serum LDL-C among the participants. Mean serum HDL-C concentrations was higher in women than in men (44.9 ± 10.1 vs 39.9 ± 9.3 mg/dl, P < 0.001). Overall, the prevalence of low serum HDL-C (<35 mg/dl) was 21.3 % in our total population and low serum HDL-C was found to be significantly more common in men than in women (32.1 vs 14 %, P < 0.001).
Age-standardized prevalence rates (using WHO population data) were 13.8 % for DM, 14.47 % for low serum HDL, 11.74 % for high cholesterol 11.34 % for high serum LDL and 22.06 % for HTN in our total population (Table 5).
Ten-year absolute CAD risk
Among participants without CVD or a CVD equivalent, the 10-year risk for CAD of <10, 10–20 and >20 % were estimated to be 86.6, 11 and 2.5 %, respectively (Table 6). Women constituted a larger proportion of individuals in <10 % risk category than men (98.9 vs 68.1 %), a greater percentage of men had 10–20 and >20 % risk for CAD development compared with women (25.7 and 6.1 vs 1.1 and 0 %, respectively). Based on these findings, approximately 300 men and 270 women without CVD or CVD risk equivalent are predicted to develop an event over 10 years, with approximately 57 new cases/year in these individuals.
Discussion
Since the landmark studies on CVD risk, such as the Framingham Study (Dawber et al. 1957), considerable efforts have been made to investigate factors associated with the progression of CVD in a large number of geographically or ethnically diverse populations. Such efforts have provided important information, increased the awareness of cardiovascular risk factors, and helped to develop strategies for lipid, hypertension, and diabetes control, exercise, and smoking prevention (Luepker et al. 1994; Ornish et al. 1998; Smith et al. 2010; Wilson et al. 1980). Nevertheless, there is still scant population-based information for populations from developing countries (Ergör et al. 2012) and this is an important omission as the WHO has predicted that non-communicable diseases, and particularly cardiovascular disease will exert the greatest disease burden in this region.
A high prevalence of CVD risk factors among Iranian middle-aged adults is probably now associated with the current high levels of CVD mortality and morbidity observed in Iran (Azizi et al. 2002; Esteghamati et al. 2008; Hadaegh et al. 2010). At baseline, a considerable proportion of our adult population aged 35–65 had hypertension, DM and hyperlipidemia that is markedly higher than reports from Western countries (Geiss et al. 2006). For example, based on the latest heart disease and stroke statistics for 2013, 8.3 % of adults in the USA had DM while the prevalence of DM was 14 % in our cohort of middle-aged individuals. Mean serum HDL levels were also lower in our subjects compared to the mean USA HDL levels (40 vs 51 mg/dl). The high prevalence of CVD risk factors among the women is another interesting feature of this population compared to others derived from the Western world. For instance, the prevalence of DM and hyperlipidemia was considerably higher in women compared to men amongst the population of subjects we have sampled. This finding is in contrast with reports from Western population (Slavenka et al. 2014) and China. However, these studies have also reported a tendency for these risk factors to cluster among overweight/obese women. This requires more detailed follow-up and analysis. Will these risk factors impact on future cardiovascular events in this population? In a recent 1-year incidence study of stroke in Mashhad, we observed relatively low crude rates of stroke, but very high age-standardized incidence rates after adjustment to European or WHO population, higher than all previous ideal incidence stroke studies around the world that can be explained by the young structure of our population (Azarpazhooh et al. 2010). Hence a high rate of CVD may be anticipated during the aging transition of our population. In the present study, our estimated risk for future CAD was in line with findings from the USA population. Data from the NHANES III in the USA have indicated that among participants without CVD, 81.7 % had a 10-year risk for CAD of <10 %, 15.5% of 10–20 % and 2.9 % of >20 %. Data from a previous cohort in Iran, the Tehran Lipid Glucose Study (TLGS), estimated the 10-year risk for CAD of <10 %, 10–20 % and >20 % to be 86.0, 12.0 and 2.0 % among participants with two or more risk factors and without CVD or a CVD risk equivalent, respectively. These comparisons indicate that along with rapid westernization in developing countries including Iran, the risk of CAD may increase to levels similar to, or indeed exceeding those within many developed countries.
The various aspects of socioeconomic status (SES) have a complex impact on cardiovascular health, and this may differ in men and women in various communities. In a previous cohort of an Iranian population from Isfahan, the authors found no independent association between the SES and incident CVD (Masoudkabir et al. 2012). It is anticipated that our cohort will provide additional data for exploring the association between SES and cardiovascular disease among men and women in our population.
Furthermore, the genetic susceptibility loci for CAD, stroke and atrial fibrillation are largely unknown in the Middle-Eastern populations. Our bank of blood and DNA samples will enable us to study the role and the contribution of genetic and environmental factors to CVDs in this population.
Our project also has the potential to influence the implementation of community interventions to target smoking, unhealthy diet, and physical inactivity. We will also have potential for other interventions throughout the course of the project targeting the community in general. The design of our study will enable us to reach individuals who would not normally seek medical help, and therefore has the potential to reduce the inequalities in utilization of services. This will enable us not only to determine CVD risks, but also to evaluate the impact of community interventions for disease prevention and risk reduction.
Whilst the participation rate was high in our study, there is still the possibility for non-participation bias and differential misclassification of CVD risk factors among different SES, gender or age groups. A random sample of non-respondents did not show significant difference regarding age and gender. Therefore, we can assume that non-respondent bias in the study was small and the respondents were generally representative of the target population. However, our data could result in spuriously high estimates of risk factor and disease prevalence if the non-response rate and/or the baseline differences had been considerably larger. This is mainly because individuals with known disease conditions are more likely to seek free medical evaluations. Also, our sample is mainly from urban population that may limit generalizability of our findings to rural populations.
Finally, it has been demonstrated that more locally based risk engines such as QRISK in the UK, may perform better in predicting clinical outcomes (Hippisley-Cox et al. 2007). In addition, most of these CVD risk algorithms are based on a limited set of variables that do not include factors such as obesity, physical activity, psychosocial status, family history of CVD, genetic susceptibility, etc. Additional emerging risk factors for CVD, for example hs-CRP and inflammatory biomarkers and plasma fatty acid concentrations may also need to be considered for inclusion to improve these algorithms. We have also developed a comprehensive model for quality assurance and several validated instruments that will allow comparisons with the results of other epidemiological studies that provides a basis for international collaboration. In conclusion, our 10-year follow-up results would provide a useful resource to help address the above-mentioned epidemiologic and public health issues in anticipation of a significant increase of persons at risk for CAD and stroke in our young but aging population.
References
Azarpazhooh MR, Etemadi MM, Donnan GA, Mokhber N, Majdi MR, Ghayour-Mobarhan M, Ghandehary K, Farzadfard MT, Kiani R, Panahandeh M, Thrift AG (2010) Excessive incidence of stroke in Iran: evidence from the Mashhad Stroke Incidence Study (MSIS), a population-based study of stroke in the Middle East. Stroke 41:e3–e10
Azizi F, Rahmani M, Emami H, Mirmiran P, Hajipour R, Madjid M, Ghanbili J, Ghanbarian A, Mehrabi Y, Saadat N, Salehi P, Mortazavi N, Heydarian P, Sarbazi N, Allahverdian S, Saadati N, Ainy E, Moeini S (2002) Cardiovascular risk factors in an Iranian urban population: Tehran lipid and glucose study (phase 1). Soz Praventivmed 47:408–426
Beaglehole R (1993) Cardiovascular disease in developing countries. BMJ 306:395
Beaglehole R, Stewart AW, Jackson R, Dobson AJ, McElduff P, D’Este K, Heller RF, Jamrozik KD, Hobbs MS, Parsons R, Broadhurst R (1997) Declining rates of coronary heart disease in New Zealand and Australia, 1983–1993. Am J Epidemiol 145:707–713
Castelli WP, Garrison RJ, Wilson PW, Abbott RD, Kalousdian S, Kannel WB (1986) Incidence of coronary heart disease and lipoprotein cholesterol levels. The Framingham study. JAMA 256:2835–2838
Dawber TR, Moore FE, Mann GV (1957) Coronary heart disease in the Framingham study. Am J Public Health Nations Health 47:4–24
Delavari A, Forouzanfar MH, Alikhani S, Sharifian A, Kelishadi R (2009) First nationwide study of the prevalence of the metabolic syndrome and optimal cutoff points of waist circumference in the Middle East: the national survey of risk factors for noncommunicable diseases of Iran. Diabetes Care 32:1092–1097
Ergör G, Soysal A, Sözmen K, Ünal B, Uçku R, Kılıç B, Günay T, Ergör A, Demiral Y, Saatlı G, Meseri R, Baydur H, Simşek H, Budak R, Arık H, Karakuş N (2012) Balcova heart study: rationale and methodology of the Turkish cohort. Int J Public Health 57:535–542
Esteghamati A, Abbasi M, Alikhani S, Gouya MM, Delavari A, Shishehbor MH, Forouzanfar M, Hodjatzadeh A, Ramezani RD (2008) Prevalence, awareness, treatment, and risk factors associated with hypertension in the Iranian population: the national survey of risk factors for noncommunicable diseases of Iran. Am J Hypertens 21:620–626
Geiss LS, Pan L, Cadwell B, Gregg EW, Benjamin SM, Engelgau MM (2006) Changes in incidence of diabetes in US adults, 1997–2003. Am J Prev Med 30:371–377
Hadaegh F, Hatami M, Tohidi M, Sarbakhsh P, Saadat N, Azizi F (2010) Lipid ratios and appropriate cut off values for prediction of diabetes: a cohort of Iranian men and women. Lipids Health Dis 9:85
Hajian-Tilaki KO, Heidari B (2007) Prevalence of obesity, central obesity and the associated factors in urban population aged 20–70 years, in the north of Iran: a population-based study and regression approach. Obes Rev 8:3–10
Harati H, Hadaegh F, Saadat N, Azizi F (2009) Population-based incidence of Type 2 diabetes and its associated risk factors: results from a 6-year cohort study in Iran. BMC Public Health 9:186
Hatano S (1976) Experience from a multicentre stroke register: a preliminary report. Bull World Health Organ 54:541–553
Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, May M, Brindle P (2007) Derivation and validation of QRISK, a new cardiovascular disease risk score for the United Kingdom: prospective open cohort study. BMJ 335:136
Husten L (1998) Global epidemic of cardiovascular disease predicted. Lancet 352:1530
Kelishadi R, Alikhani S, Delavari A, Alaedini F, Safaie A, Hojatzadeh E (2008) Obesity and associated lifestyle behaviours in Iran: findings from the First National Non-communicable Disease Risk Factor Surveillance Survey. Public Health Nutr 11:246–251
Kuulasmaa K, Tunstall-Pedoe H, Dobson A, Fortmann S, Sans S, Tolonen H, Evans A, Ferrario M, Tuomilehto J (2000) Estimation of contribution of changes in classic risk factors to trends in coronary-event rates across the WHO MONICA Project populations. Lancet 355:675–687
Lloyd BL (1994) Declining cardiovascular disease incidence and environmental components. Aust N Z J Med 24:124–132
Luepker RV, Murray DM, Jacobs DR Jr, Mittelmark MB, Bracht N, Carlaw R, Crow R, Elmer P, Finnegan J, Folsom AR (1994) Community education for cardiovascular disease prevention: risk factor changes in the Minnesota Heart Health Program. Am J Public Health 84:1383–1393
Masoudkabir F, Toghianifar N, Talaie M, Sadeghi M, Sarrafzadegan N, Mohammadifard N, Marshall T, Thomas GN (2012) Socioeconomic status and incident cardiovascular disease in a developing country: findings from the Isfahan cohort study (ICS). Int J Public Health 57:561–568
Monge R, Beita O (2000) Prevalence of coronary heart disease risk factors in Costa Rican adolescents. J Adolesc Health 27:210–217
Najeeb MA (1993) Cardiovascular disease in developing countries. BMJ 306:927
Ornish D, Scherwitz LW, Billings JH, Brown SE, Gould KL, Merritt TA, Sparler S, Armstrong WT, Ports TA, Kirkeeide RL, Hogeboom C, Brand RJ (1998) Intensive lifestyle changes for reversal of coronary heart disease. JAMA 280:2001–2007
Sarrafzadegan N, Talaei M, Sadeghi M, Kelishadi R, Oveisgharan S, Mohammadifard N, Sajjadieh AR, Kabiri P, Marshall T, Thomas GN, Tavasoli A (2010) The Isfahan cohort study: rationale, methods and main findings. J Hum Hypertens 25:545–553
Sarraf-Zadegan N, Boshtam M, Malekafzali H, Bashardoost N, Sayed-Tabatabaei FA, Rafiei M, Khalili A, Mostafavi S, Khami M, Hassanvand R (1999) Secular trends in cardiovascular mortality in Iran, with special reference to Isfahan. Acta Cardiol 54:327–333
Schweigman K, Eichner J, Welty TK, Zhang Y (2006) Cardiovascular disease risk factor awareness in American Indian communities: the strong heart study. Ethn Dis 16:647–652
Slavenka J, Dragana S, Janko J, Miloš E, Jelena M (2014) Status of cardiovascular health in a transition European country: findings from a population-based cross-sectional study. Int J Public Health. 59:769–778
Smith EN, Chen W, Kahonen M, Kettunen J, Lehtimaki T, Peltonen L, Raitakari OT, Salem RM, Schork NJ, Shaw M, Srinivasan SR, Topol EJ, Viikari JS, Berenson GS, Murray SS (2010) Longitudinal genome-wide association of cardiovascular disease risk factors in the Bogalusa heart study. PLoS Genet 6:e1001094
Sytkowski PA, D’Agostino RB, Belanger A, Kannel WB (1996) Sex and time trends in cardiovascular disease incidence and mortality: the Framingham Heart Study, 1950–1989. Am J Epidemiol 143:338–350
Uthoff H, Staub D, Socrates T, Meyerhans A, Bundi B, Schmid HP, Frauchiger B (2010) PROCAM-, FRAMINGHAM-, SCORE- and SMART-risk score for predicting cardiovascular morbidity and mortality in patients with overt atherosclerosis. Vasa 39:325–333
Wilson PW, Garrison RJ, Castelli WP, Feinleib M, McNamara PM, Kannel WB (1980) Prevalence of coronary heart disease in the Framingham Offspring Study: role of lipoprotein cholesterols. Am J Cardiol 46:649–654
Conflict of interest
Authors have no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ghayour-Mobarhan, M., Moohebati, M., Esmaily, H. et al. Mashhad stroke and heart atherosclerotic disorder (MASHAD) study: design, baseline characteristics and 10-year cardiovascular risk estimation. Int J Public Health 60, 561–572 (2015). https://doi.org/10.1007/s00038-015-0679-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00038-015-0679-6