Abstract
Objectives
The single-item question on self-rated health has been widely used in surveys. This study aims to explore which frames of reference are used by respondents when answering this question, to describe differences in the used frame of reference according to gender, educational background and age, and to determine whether subgroup differences can be explained by differences in prior health experiences.
Methods
Face-to-face interviews were conducted in a sample of 310 adults who were asked to rate their health using a single-item question with closed-ended answering categories and to explain the reasons for the rating they gave with open-ended probes. Different indicators of prior health experiences were taken into account.
Results
Physical health problems were the most utilized referents. However, participants also mentioned reasons that go beyond the physical dimension of health. Subgroup differences were found. Prior health experiences partly explained subgroup differences for some referents, but not for others.
Conclusions
Investigators using the single question on self-rated health for comparing health across different population groups should be aware that the meaning of the question varies across different socio-demographic groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the most frequently used measures of health in health surveys is a single question on self-rated health (SRH). The exact wording of this question and its response choices varies somewhat from one study to another, but respondents are asked to rate their health in general on a five-point scale, for example from ‘excellent’ to ‘poor’, or from ‘very good’ to ‘very bad’.
This question has good test–retest reliability (Cox et al. 2009; Lundberg and Manderbacka 1996; Martikainen et al. 1999), and proved to be a powerful predictor for mortality (Idler and Benyamini 1997; Nielsen et al. 2008) and a range of other health outcomes such as functional decline (Idler and Kasl 1995; Jagger et al. 1993), future morbidity (Moller et al. 1996) and health service use (Fylkesnes 1993), independent of specific health status indicators and other relevant covariates.
Based on its easy administration and its ability to provide a concise way of summarizing the health status, the SRH question has been used extensively. It is also frequently applied as a proxy question for more thorough, complicated and expensive measurements of health status in research where health is a background variable.
It is presumed that SRH combines numerous aspects of health and when respondents answer the SRH question, they give an indication according to their own perceptual framework on health. Hereby, the response option chosen indicates the label they use to summarize their subjective health perceptions (Locker et al. 2009).
Despite the widespread use of SRH as a health indicator, the knowledge of the process underlying people’s evaluation of their general health is limited and the dimensions, frames of reference and meanings that respondents use to answer the SRH question are not well known (Jylha 2009; Kaplan and Baron-Epel 2003; Quesnel-Vallee 2007).
There are essentially two possible approaches to understand what the global SRH item measures (Krause and Jay 1994). A first approach involves correlating the global health rating with other theoretically relevant external criterion measures, as physical and mental health symptoms, longstanding illness, sickness absence, leisure physical activity, body mass index, smoking, etc (Bailis et al. 2003; Singh-Manoux et al. 2006). Although this kind of studies has provided some useful insights, there are important limitations related to this approach. The measures that should be included in the analysis are based on an a priori theory about the factors that may play a role in shaping health perceptions. Most researchers address only selected parameters and thus are likely to yield only partial or confounded information on what SRH determines (Mantzavinis et al. 2005). This approach also fails to provide an indication of the extent to which these factors directly enter people’s perceptual framework when judging their health or are related more outside of people’s awareness. In addition, in these studies a significant proportion of variance in SRH remains unexplained.
A second approach asks people to elaborate on the reasons underlying their rating of health. Some studies take a strictly qualitative approach and identified frames of reference (Abdulrahim and Ajrouch 2010; Manderbacka 1998), while others coded according to these frames of reference and focused on simple quantitative analysis to determine subgroup differences (Krause and Jay 1994; Simon et al. 2005).
It is very relevant to know whether participants from different subgroups consider different frames of reference when they are asked to rate their overall health status. Should the meaning of the SRH question differ substantially between subgroups, then the utility of the SRH question for making subgroup comparisons may be questioned (d’Uva et al. 2008; Dowd and Zajacova 2010; Lang and Delpierre 2009; Singh-Manoux et al. 2007). In spite of this intrinsic importance, the issue of subgroup differences in the frames of reference has not been investigated in-depth. Krause and Jay (1994) reported that people in different age groups have a tendency to use different frames of reference. The same may be true with respect to race and education. Simon et al. (2005) described differences by gender and age.
Differences in the frame of reference by subgroups could be attributed to prior experiences with ill health (Krause and Jay 1994; Simon et al. 2005). For example, because older people are more likely than younger individuals to experience chronic health problems, it may not be surprising that older people think in terms of health problems when answering the SRH question (Krause and Jay 1994). Examining subgroup differences after the effects of prior health experiences, such as physical health status or health care utilization had been controlled statistically, would be valuable (Krause and Jay 1994). Yet, due to a rather small sample size or the absence of other health status measures, the previous studies were not able to provide insight into this question (Krause and Jay 1994; Simon et al. 2005).
The aim of this study is (1) to explore which frames of reference are used by survey respondents when answering a single SRH question, (2) to describe differences in the used frame of reference according to gender, educational background and age, and (3) to determine whether subgroup differences can be explained by differences in prior health experiences.
Methods
Study population and procedure
Respondents were randomly selected from the list of patients of a community health center. This is a clinic staffed by an interdisciplinary group of general practitioners, nurses, social workers and health promotion workers. The center provides accessible and affordable primary health care to the inhabitants of a traditionally deprived neighborhood in Ghent (Belgium) which experienced now an inflow of young, higher educated families. Inclusion criteria were that they should be aged 18 years or over and that they should understand the Dutch language. The staff of the health community center excluded all patients whose medical condition would not allow a face-to-face interview (e.g., because of a severe psychiatric disorder, because the patient had Alzheimer disease, etc). All selected subjects were informed by mail by the community health center regarding the study. Trained interviewers approached and interviewed them face-to-face at home about their health and about their opinion regarding the community health center. The data were collected for the purpose of community-oriented primary care (COPC). COPC combines individual patient and physician practice data with public health data at the community level, leading to a ‘community diagnosis’ (Gavagan 2008).
Measures
Self-rated health
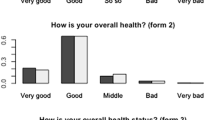
After asking study participants to respond to the question “how is your health in general?” by selecting a closed-ended answer (i.e., very good, good, fair, bad or very bad), subjects were asked to explain why they selected a particular closed-ended response with two open-ended probes: first subject was asked “why did you select that particular answering category and not a better category” followed by “why did you not select a worse category”. To avoid any influence, these questions were asked before other health related questions. The answers were transcribed ‘near verbatim’.
Socio-demographic variables
Date of birth, gender and level of education were recorded. For this study, subgroups were created by grouping the participants by age (‘below 36’, ‘between 36 and 55’ and ‘above 55’) and education (participant had a degree of higher education or not). Participants still studying were categorized into the level of their study.
Prior health experiences
Five indicators of various prior health experiences were taken into account. First, the number of chronic diseases and conditions the respondent had indicated on a list of 30 presented items was used. Also the scales ‘physical functioning’ (10 items), ‘mental health’ (5 items) and ‘vitality’ (4 items) from the Medical Outcomes Study 36-Item Short Form (SF-36) survey were included. The SF-36 is a generic health-related quality of life questionnaire constructed for use in medical outcomes studies (McHorney et al. 1993; Ware and Sherbourne 1992). Finally, contact with a GP past 3 months (yes/no) was used as an indicator for prior health care utilization.
Coding procedure
The transcripts of the open-ended questions were coded according to the following procedure. Two researchers (WP and SW) independently reviewed and coded 20 interviews and independently developed a preliminary categorization scheme based on the answers given by the respondents. The results were compared and discussed to come to a generic categorization scheme. In a second step, both researchers independently applied this categorization scheme to 80 interviews. The results were again compared, the categorization scheme was adapted and discrepancies were resolved. Finally, both researchers coded all other interviews independently, compared results and consensus was found.
The final categorization scheme that was used for coding the answers consists of several domains. For each domain, the distinction was made between aspects and referents with a positive undertone and referents with a more negative connotation. While some answers were simple and referred to a single frame of reference, others were more complex and could not be captured by means of a single category and required the allocation of multiple categories of the categorization scheme.
Data-analysis
In a series of bivariate logistic regression analysis, odds ratios were calculated to see whether the referents mentioned varied by gender, education and age. A separate logistic regression analysis was performed for every category of the categorization scheme that was mentioned at least by 12 respondents. Next, the odds ratios were calculated again, this time adjusted for prior health experiences.
Results
Response rate
In total, 457 patients were invited to participate, 310 (67.8%) were interviewed at home, 45 (9.8%) refused to participate, 23 (5%) were not found at home and from 79 (17.3%) the contact details were inaccurate. Response was higher for female and older respondents. Complete data on all health status measures were available for 299 cases. Their characteristics can be found in Table 1.
Referents used in answering the SRH question
In the answers the respondents gave on the open-ended probes, 10 domains, each with a positive and a negative side, could be identified. Further, in the domain ‘health comparisons’ a distinction between ‘health comparisons with others’ and ‘health comparisons with oneself in the past’ could be made. This resulted in a categorization scheme with 22 categories or referents (see Table 2). In Appendix Table 6 the description of the referents is given and illustrated with quotes.
Any reference to disease or ‘body’-oriented problems or complaints was considered to be an aspect of the categories ‘absence’ or ‘presence of physical health problems’. These categories were the most frequently mentioned categories. References to physical functional abilities or limitations were considered to be an aspect of the domain ‘physical functioning’. For this domain, the category with a positive connotation was mentioned almost thrice more than the category with a negative connotation. The domain ‘medical treatment’ grouped all references to (not) visiting a GP, using medication or passed surgery. The domain ‘mental health’ was used for referents to depression, nervousness or emotional problems. This domain was more frequently used as a referent with a negative connotation. References to feeling (not) tired, fatigued or energetic were considered to be an aspect of the ‘vitality’ domain. For this domain, only answers with a negative undertone were registered. On the contrary, those who compared their health to others did this only with a positive undertone. Any reference to a positive or negative attitude toward health in general or a current illness or having adapted to its limitations is considered to be an aspect of the ‘coping’ domain. The category ‘medical risk factors’ included all references to medical risk factors (i.e., blood pressure, cholesterol, and weight). The ‘health behavior’ domain referred to any answer referring to health behavior, such as smoking and doing sports. References to feelings without any further justification (e.g., ‘I feel good’ or ‘I feel bad’) were classified in the ‘wellbeing’ domain. ‘Feeling good’ was mentioned by more than a quarter of the respondents, ‘feeling bad’ was not very common.
Differences by gender
Table 3 shows the differences in the use of referents by gender. Men were less likely to express referents from the category ‘absence of physical health problems’ and more likely to mention ‘(problems with) physical functioning’. When prior health experiences were taken into account, especially the SF-36 scale physical functioning, the differences were even more pronounced. The largest differences between men and women were found for ‘negative health behavior’ which was the most reported by men. Also the categories ‘medical risk factors with a negative connotation’ and ‘feeling good’ were more mentioned by male subjects. These results remained after adjustment for prior health experiences. No significant gender differences could be observed in the other categories.
Differences by education
The respondents with a higher education were more likely than those without a higher education to include the absence of physical health problems and illnesses in their answer and less likely to refer to the presence of physical health problems (Table 4). The differences decreased when chronic diseases or physical functioning was brought into the analysis. Physical functioning, both with a positive undertone and with a negative connotation, was more referred to by the higher educated. The association enhanced when the SF-36 scale ‘physical functioning’ was taken into account.
The respondents with a degree of higher education more frequently used statements that refer to vitality to describe their health. The differences became even more pronounced when the SF-36 scales ‘mental health’ and ‘vitality’ were brought into the analysis. Participants with lower level of education referred more often to their better health in the past to describe their current health status.
Differences by age
Examining the age variation (Table 5) revealed that older age groups were more likely to mention ‘physical health problems’. This association diminished when chronic diseases or physical functioning were taken into account. ‘Medical treatment’, especially when it was expressed with a negative undertone, was also more used by the older age groups. The oldest age groups were also more inclined to use the category ‘health comparisons with oneself in the past with a negative connotation’ to motivate their answer on the SRH questionnaire. Bringing prior health experiences into the analysis did not change the association.
The data also suggest that the youngest age group was considerably more likely to use ‘negative health behavior’ as a referent. This category was almost exclusively mentioned by the participants from this age group.
Discussion
This study tried to answer three questions. First, it wanted to explore the frames of reference respondents apply to respond to global SRH. As in the previous studies, this study found a wide variation in the aspects playing a role in how respondents assess their health. The physical health dimension was most dominant and proved to be a pivotal factor in the self-assessment of health. Nevertheless, some people thought in terms of more general physical functioning, or made a comparison with others or with their own health in the past, or mentioning just feeling good. The referents identified in this study are in accordance with the categories uncovered in the previous studies (Abdulrahim and Ajrouch 2010; Borawski et al. 1996; Kaplan and Baron-Epel 2003; Krause and Jay 1994; Manderbacka 1998; Simon et al. 2005) notwithstanding the fact that the number and labels of categories differed between studies. Also in line with the previous studies (Krause and Jay 1994; Locker et al. 2009; Simon et al. 2005) is the observation that respondents refer, respectively, to different aspects of the concept of health as well as to points of reference to compare themselves with (age-peers, their earlier health).
The second aim concerned subgroup differences in these frames of reference. The data suggested that the tendency to use a particular referent was associated with socio-demographic factors such as gender, education and age.
This study demonstrated that men were more inclined to mention the physical functioning aspect compared with women. This was also found by Simon et al. (2005). They suggested that men, more than women, have incorporated the functional definition of health as ‘being able to perform the necessary duties’ (Simon et al. 2005).
The results also revealed that people with different educational background had a tendency to use one frame of reference more instead of another. The differences were most pronounced for the dimension physical functioning. Although problems with physical functioning occur more frequently among people with lower level of education, respondents with higher educational attainment were more inclined to consider (problems with) physical functioning as a referent when answering the SRH question.
Also some significant age differences were detected. The observation that older respondents were more inclined to refer to physical health problems, utilization of medical care and a decline of their health when they answered the SRH question is in concordance with the fact that older people are more confronted with health problems, are in fact utilizing more frequent medical care and are confronted with a deterioration of their health. On the other hand, the category negative health behavior was almost exclusively used by younger respondents. Also Krause and Jay (1994) found that younger people tend to use health behavior more often as a referent. An explanation is not available yet. Further research should find out the reason.
The observed subgroup differences are in accordance with other studies that show SRH has a different association with biological risk factors and mortality in different population groups (Benyamini et al. 2003; Deeg and Kriegsman 2003; Dowd and Zajacova 2007, 2010; Franks et al. 2003; Huisman et al. 2007; Singh-Manoux et al. 2007), even though other studies found no significant interactions (e.g., (Burstrom and Fredlund 2001; McFadden et al. 2009).
The third aim of this study was to explore the possibility that was opted by Krause and Jay (1994) who suggested that the subgroup differences in frames of reference reflect underlying differences in the health status or other prior health experiences. The results of this study suggested that for some referents, prior health experiences could partly explain the differences. For example, people with lower lever of education are more confronted with physical health problems. As expected, this category was more used as a referent by the respondents with lower level of education, and when the number of chronic diseases or the SF-36 scale ‘physical functioning’ was taking into account, the association diminished. This observation confirmed that prior health experiences could be an explanation for the differences. However, frequently opposite results could be found. The dimension ‘physical functioning’ was more mentioned by people with higher level of education and this association enhances when adjusted for health status. Clearly, more research is needed to disentangle this issue.
Strengths and limitations
A key strength of this study was the utilization of several indicators of prior health experiences to explain subgroup differences in frames of reference. This was the first study to test the hypothesis that subgroup differences in frames of reference reflect prior health experiences. An important limitation was that only self-reported measures of prior health experiences were available. The possibility exists that the indicators used in the current study do not cover the ill health experienced by the respondents sufficiently. This could potentially be an alternative explanation why the subgroup differences were not fully explained by adjusting for prior health experiences.
Idler et al. (1999) have criticized the practice to use the first responses only, when summarizing and quantitatively analyzing qualitative data, as Krause and Jay (1994) did, because it should lead to a substantial loss of information and masks the complexity and multilayered character of health ratings. The present study included all aspects which participants mentioned (multiple-reference study). In addition, a different approach was used to elicit the referents using two open-ended probes instead of one question to explain the initial response to the SRH question. This approach may be closer to people’s actual decision-making processes and probably produced data that reflect the multilayered character of health ratings in a more valid way. Even though that for some domains the positive or negative side was not very common, or even absent, the procedure to use a positive and a negative side for each of the different domains in the categorization scheme was in accordance with the method to use two open-ended probes. This made it possible to show important subgroup differences that otherwise could not have been detected. As a consequence, this approach facilitated the understanding of the complexity of the meanings that underlie global SRH questions for survey respondents. However, the answers the respondents gave, may still be limited to a shorter list of the most salient factors, and/or to factors that people feel were legitimate to report in such an interview.
Another strength was the large sample size compared with the previous studies (Krause and Jay 1994; Simon et al. 2005), which made it possible to determine subgroup differences in a more valid way. In spite of this, the sample size of this study was still limited, resulting in wide confidence intervals and the interpretation of the results should be done carefully. Some results provide strong evidence of subgroup differences in the used frame of reference while for other aspects, the evidence of subgroup differences is only weak. For some categories no statistical significant subgroup differences were found, but because of limited statistical power, it is not possible to draw a final conclusion for those categories.
There were only seven people who rated their health as bad and no one assessed it very bad. Because the two (out of five) most badly categories of the SRH question are hardly covered, there is the possibility that some aspects related to ill health were missed.
Another potential limitation arises when continuous measures like age are arbitrarily partitioned into ordinal categories. To address this potential problem, the data were reanalyzed using different cut-off points. The results from these additional analyses (not shown) were quite close to those presented in Table 5.
Implications
To conclude, as Mallinson (2002) has stated: “The issue of meaning is absolutely central to understanding subjective views and without more assessment of peoples’ understandings of survey questions it is difficult to see how one can establish their validity as subjective health measures.” The findings of the present study are important for investigators who use SRH as an easy and inexpensive way to compare health across different population groups. Comparisons should be made with caution and researchers should be aware of the different meanings that SRH has in different groups. Using anchoring vignettes to take into account socio-demographic differences in health reporting behavior could be a solution, though further research to develop this method is necessary (d’Uva et al. 2008).
References
Abdulrahim S, Ajrouch K (2010) Social and cultural meanings of self-rated health: Arab immigrants in the United States. Qual Health Res 20(9):1229–1240. doi:10.1177/1049732310371104
Bailis DS, Segall A, Chipperfield JG (2003) Two views of self-rated general health status. Soc Sci Med 56(2):203–217 (pii:S0277-9536(02)00020-5)
Benyamini Y, Blumstein T, Lusky A, Modan B (2003) Gender differences in the self-rated health-mortality association: is it poor self-rated health that predicts mortality or excellent self-rated health that predicts survival? Gerontologist 43(3):396–405
Borawski EA, Kinney JM, Kahana E (1996) The meaning of older adults’ health appraisals: congruence with health status and determinant of mortality. J Gerontol B Psychol 51(3):S157–S170
Burstrom B, Fredlund P (2001) Self rated health: is it as good a predictor of subsequent mortality among adults in lower as well as in higher social classes? J Epidemiol Community Health 55(11):836–840
Cox B et al (2009) The reliability of the Minimum European Health Module. Int J Public Health 54(2):55–60. doi:10.1007/s00038-009-7104-y
D’Uva TB, O’Donnell O, van Doorslaer E (2008) Differential health reporting by education level and its impact on the measurement of health inequalities among older Europeans. Int J Epidemiol 37(6):1375–1383. doi:10.1093/ije/dyn146
Deeg DJH, Kriegsman DMW (2003) Concepts of self-rated health: specifying the gender difference in mortality risk. Gerontologist 43(3):376–386
Dowd JB, Zajacova A (2007) Does the predictive power of self-rated health for subsequent mortality risk vary by socioeconomic status in the US? Int J Epidemiol 36(6):1214–1221. doi:10.1093/Ije/Dym214
Dowd JB, Zajacova A (2010) Does self-rated health mean the same thing across socioeconomic groups? Evidence from biomarker data. Ann Epidemiol 20(10):743–749. doi:10.1016/j.annepidem.2010.06.007
Franks P, Gold MR, Fiscella K (2003) Sociodemographics, self-rated health, and mortality in the US. Soc Sci Med 56(12):2505–2514 (pii:S0277-9536(02)00281-2)
Fylkesnes K (1993) Determinants of health-care utilization—visits and referrals. Scand J Soc Med 21(1):40–50
Gavagan T (2008) A systematic review of COPC: evidence for effectiveness. J Health Care Poor U 19(3):963–980
Huisman M, van Lenthe F, Mackenbach J (2007) The predictive ability of self-assessed health for mortality in different educational groups. Int J Epidemiol 36(6):1207–1213. doi:10.1093/ije/dym095
Idler EL, Benyamini Y (1997) Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav 38(1):21–37
Idler EL, Kasl SV (1995) Self-ratings of health: do they also predict change in functional ability? J Gerontol B Psychol Sci Soc Sci 50(6):S344–S353
Idler EL, Hudson SV, Leventhal H (1999) The meanings of self-ratings of health—a qualitative and quantitative approach. Res Aging 21(3):458–476
Jagger C, Spiers NA, Clarke M (1993) Factors associated with decline in function, institutionalization and mortality of elderly people. Age Ageing 22(3):190–197
Jylha M (2009) What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med 69(3):307–316. doi:10.1016/j.socscimed.2009.05.013
Kaplan G, Baron-Epel O (2003) What lies behind the subjective evaluation of health status? Soc Sci Med 56(8):1669–1676 (pii:S0277-9536(02)00179-X)
Krause NM, Jay GM (1994) What do global self-rated health items measure. Med Care 32(9):930–942
Lang T, Delpierre C (2009) ‘How are you?’ what do you mean? Eur J Public Health 19(4):353. doi:10.1093/eurpub/ckp083
Locker D, Maggirias J, Wexler E (2009) What frames of reference underlie self-ratings of oral health? J Public Health Dent 69(2):78–89. doi:10.1111/j.1752-7325.2008.00103.x
Lundberg O, Manderbacka K (1996) Assessing reliability of a measure of self-rated health. Scand J Soc Med 24(3):218–224
Mallinson S (2002) Listening to respondents: a qualitative assessment of the Short-Form 36 health status questionnaire. Soc Sci Med 54(1):11–21
Manderbacka K (1998) Examining what self-rated health question is understood to mean by respondents. Scand J Soc Med 26(2):145–153
Mantzavinis GD, Pappas N, Dimoliatis LDK, Ioannidis JPA (2005) Multivariate models of self-reported health often neglected essential candidate determinants and methodological issues. J Clin Epidemiol 58(5):436–443. doi:10.1016/j.jclinepi.2004.08.016
Martikainen P et al (1999) Reliability of perceived health by sex and age. Soc Sci Med 48(8):1117–1122
McFadden E, Luben R, Bingham S, Wareham N, Kinmonth AL, Khaw KT (2009) Does the association between self-rated health and mortality vary by social class? Soc Sci Med 68(2):275–280. doi:10.1016/j.socscimed.2008.10.012
McHorney CA, Ware JE Jr, Raczek AE (1993) The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care 31(3):247–263
Moller L, Kristensen TS, Hollnagel H (1996) Self rated health as a predictor of coronary heart disease in Copenhagen, Denmark. J Epidemiol Community Health 50(4):423–428
Nielsen ABS, Siersma V, Hiort LC, Drivsholm T, Kreiner S, Hollnagel H (2008) Self-rated general health among 40-year-old Danes and its association with all-cause mortality at 10-, 20-, and 29 years’ follow-up. Scand J Public Healt 36(1):3–11. doi:10.1177/1403494807085242
Quesnel-Vallee A (2007) Self-rated health: caught in the crossfire of the quest for ‘true’ health? Int J Epidemiol 36(6):1161–1164. doi:10.1093/ije/dym236
Simon JG, De Boer JB, Joung IMA, Bosma H, Mackenbach JP (2005) How is your health in general? A qualitative study on self-assessed health. Eur J Public Health 15(2):200–208. doi:10.1093/eurpub/cki102
Singh-Manoux A, Martikainen P, Ferrie J, Zins M, Marmot M, Goldberg M (2006) What does self rated health measure? Results from the British Whitehall II and French Gazel cohort studies. J Epidemiol Community Health 60(4):364–372. doi:10.1136/jech.2005.039883
Singh-Manoux A et al (2007) The association between self-rated health and mortality in different socioeconomic groups in the GAZEL cohort study. Int J Epidemiol 36(6):1222–1228. doi:10.1093/ije/dym170
Ware JE, Sherbourne CD (1992) The Mos 36-item short-form health survey (sf-36).1. Conceptual-framework and item selection. Med Care 30(6):473–483
Conflict of interest
Authors do not have any conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
See Table 6.
Rights and permissions
About this article
Cite this article
Peersman, W., Cambier, D., De Maeseneer, J. et al. Gender, educational and age differences in meanings that underlie global self-rated health. Int J Public Health 57, 513–523 (2012). https://doi.org/10.1007/s00038-011-0320-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00038-011-0320-2