Abstract
Objective
To determine immigrants’ frequency of use of four health services by place of origin and compare it with that of the Spanish population.
Methods
Based on the 2006 National Health Survey in Spain, we estimated the frequency of use of four health services in men and women from: Spain, Western countries, Eastern Europe, Latin America, North Africa, Sub Saharan Africa and Asia/Oceania. These results were compared with the Spanish population by calculating odds ratios adjusted for age, socioeconomic position, health status, and type of health coverage.
Results
Immigrant men generally use health services less frequently than Spanish nationals. The main exceptions are Latin American men, who more often use emergency services (OR 1.68, 95% CI 1.41–1.99) and Sub-Saharan men, who use specialists more frequently (OR 2.93, 1.70–5.05). Immigrant women use health services about as frequently as Spanish women. The main exceptions are North African women, who less frequently use specialists (OR 0.39, 0.22–0.71) and Sub-Saharan women who more frequently use GPs (OR 4.06, 2.21–7.44), specialists (OR 2.29, 1.06–4.95) and emergency services (OR 2.92, 1.49–5.72).
Conclusions
Health services use by the immigrant population in Spain differs by gender and place of origin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One objective of public health systems with universal health coverage is to achieve equal use of health services for equal level of need—what is known as horizontal equity. Numerous studies have evaluated horizontal equity in relation to income level or socioeconomic position (Regidor et al. 2008a; Van Doorslaer 2000; Van Doorslaer et al. 2006). In contrast, the relation between achieving this objective and other individual characteristics has been the object of less investigation. For example, few studies have examined the influence of place of origin of the immigrant population on the use of health services, and those that have been conducted have obtained heterogeneous results (Laroche 2000; Reijneveld 1998; Stronks et al. 2001). The largest amount of heterogeneity has been seen in visits to the general practitioner and in hospitalisation. (Laroche 2000; Reijneveld 1998; Stronks et al. 2001) The results regarding specialist visits are more homogeneous, with immigrants seen to have a similar or lower rate of use than the native population (Laroche 2000; Stronks et al. 2001).
Immigration is a phenomenon that has increased exponentially in Spain in recent decades. The estimated annual rate of change of the migrant stock during the period 2000–2005 was 19.3%, as compared to the annual rate of change of just 2.2% in Europe (United Nations 2009). In 2006, 10.8% of the Spanish population was foreign-born. Of these, 39.3% were born in Latin America, 22,9% in Western countries, 13.7% in North Africa, 5.1% in Asia/Oceania, and 3.7% in Sub-Saharan Africa (Instituto Nacional de Estadística 2007).
In Spain, access to health care for the immigrant population is regulated by Organic Law 4/2000. According to this law, legal immigrants, as well as all illegal immigrants inscribed in a Municipal Register, and all immigrant children and pregnant women have access to health care in the same conditions as the Spanish population. Illegal immigrants, not inscribed in a Municipal Register have access only to emergency care (Law 2000). Only four countries have the same range of services/entitlements to health care for undocumented immigrants and nationals: France, the Netherlands, Portugal and Spain. In all four countries, full access is tied to a variety of pre-conditions including: proof of identity, residence, destitution and minimum duration of stay (Karl-Trummer et al. 2010).
Recent studies have shown that immigrants’ use of GPs and medical specialists is less than or about the same as the Spanish population, whereas their use of hospitalisation and emergency services is higher. These authors suggest that the immigrant population in Spain may have problems accessing the health system (Hernández-Quevedo and Jiménez-Rubio 2009; Jiménez-Rubio and Hernández-Quevedo 2009).
Moreover, various studies reflect gender differences in health services use among ethnic minorities (Balarajan et al. 1989; Dunlop et al. 2002; Gillam et al. 1989; Song et al. 2006), but information regarding the immigrant population is very limited. In Spain, there are no studies that explore the use of health services in the immigrant population stratified by sex, and the reproductive pattern of immigrant women may be biased results of previous studies.
Accordingly, the objective of this work was to measure, stratifying by sex, the frequency of use of health services by the immigrant population in Spain, by place of origin, and to compare it with that of the Spanish population.
Methods
Data source
The data were obtained from the 2006 Spanish National Health Survey targeting the population aged 16 and over. The datafile with microdata was downloaded from the website of the Ministry of Health and Consumer Affairs (Ministerio de Sanidad y Consumo 2006). The sampling frame consisted of all non-institutionalised persons residing in Spain. Multistage stratified sampling was performed. The first-stage units were the census sections, stratified by size of municipality. Within each stratum, census sections were selected with a probability proportional to their size. The second-stage units were the primary family households, selected with equal probability within each section by systematic sampling with random start. Finally, one individual aged 16 years or older was randomly selected from within each household. The information was gathered by a questionnaire that is administered by trained interviewers. In case of communication problems, the information is gathered by a proxy qualified to answer in place of the interviewee. Because an increasing percentage of persons over 74 are institutionalised, and only a small percentage of the immigrant population is older than that of age, the analysis in the present work was restricted to the population aged 16–74 years.
The four health services studied were visits to general practitioners, visits to specialists, use of emergency services, and hospitalisation. The reference period was the previous 4 weeks for the first two services and the previous year for the latter two. Persons interviewed in the health survey were asked when they had last visited a physician for a health problem or disease, and those who had visited a physician in the previous 4 weeks were asked if the physician consulted at the last visit was a general practitioner or specialist. Respondents were also asked if they had used any emergency service for a health problem or disease and if they had been hospitalised for at least one night during the year before the interview. Those who had been hospitalised were asked the reason for the last admission. Cases in which the last admission was to give birth were excluded.
Place of origin—the main independent variable—was derived from the respondent’s country of birth, which was grouped into seven categories. (a) Spain; (b) Western countries (Western Europe, United States of America and Canada); (c) Eastern Europe; (d) Latin America; (e) Sub-Saharan Africa; (f) North Africa; and (g) Asia and Oceania. To define these categories, we considered criteria of geographical proximity, cultural proximity and size of the categories.
The potential confounding variables used were age, highest educational level completed by the respondent, social class of household reference person, and total household income. Educational level was grouped into the following categories: no education/does not know how to read or write, primary or equivalent, secondary, and university. Social class was based on the current or most recent occupation of the household reference person, understood as the person who contributes the most income to the household. Social class was grouped into the following categories: I: managers and professions associated with a university degree; II: employees and professionals who support management, self-employed persons, supervisors of manual workers; III: skilled manual workers; IV: semi-skilled manual workers; V: unskilled manual workers. Survey respondents were asked to indicate the total household income by selecting one of eight income ranges. A variable was created grouping this information into four categories, plus an additional category to which the 25% of subjects who did not answer this question were assigned.
The variables selected to reflect the need for health care were self-rated health status and number of chronic diseases suffered by the respondent. Respondents were asked to rate their health status in the last year by choosing one of the following categories: very good, good, fair, poor, or very poor. They were also asked if a physician had ever told them they suffered from any of a list of 27 chronic diseases; respondents had to answer yes or no to each disease on the list. The responses to these 27 questions were grouped into a single variable with the following four categories: no disease, one–two diseases, three–four diseases, more than four diseases.
Finally, health coverage was included as a variable that facilitates health care. Respondents were asked to specify the type of health insurance they had by choosing a maximum of two alternatives from a list of eight. Based on this information, a variable for type of health coverage was created, with three categories: only public, both public and private, and no coverage.
Statistical analysis
Men and women were analysed separately. We first calculated the distribution of the different variables in each category of place of origin. The association between place of origin and use of each health service was then calculated as an indication of the relative differences in the use of each service between the immigrant and Spanish population. The measure of association was the odds ratio (OR) with its 95% confidence interval (95% CI), calculated by logistic regression. The first model was adjusted for age, and successive models were also adjusted for the measures of self-rated health and number of chronic diseases, socioeconomic position, and, finally, type of health coverage. The reference category for all cases was the Spanish-born population. The correlation between the independent variables was studied using the Spearman correlation. Variables with a correlation coefficient >0.6 were not included in the multivariable model. The software used was Statistical Package for the Social Sciences 18.0 and Stata 11.0.
Results
The response rate was 96.11%. During the survey, 156 people were replaced due to inability to answer. Of these, the nationality was known in 75 persons: 36 were Spanish and 39 were foreign.
Tables 1 and 2 show the number of subjects in each population group, the distribution of the study variables, and the frequency of use of each health service according to the place of origin. People born in Western countries have a higher socioeconomic position than the Spanish native population. The groups with lower education levels come from Africa. The health status of the immigrant population is better than that of the Spanish-born population, with some exceptions. Men from Sub-Saharan Africa, North Africa and Asia/Oceania report a worse health status. Conversely, women from Sub-Saharan Africa have good self-rated healths as well as a low percentage of women reporting a chronic disease.
Taking Spanish-born men as the reference category, Table 3 shows the ORs associated with health care use by place of origin. After adjusting for age, measures of socioeconomic position, measures of need for health care and health coverage (model 4), all groups of immigrant men visited the GP with about the same frequency as Spanish-born did, except for men from Eastern countries, who visited GPs less frequently: OR 0.49 (95% CI 0.33–0.74). Most immigrant men visited specialists less frequently than Spanish men, except for Eastern Europeans and Asian/Oceanians who visited specialists with the same frequency and Sub-Saharans who visited them more frequently: OR 2.93(95% CI 1.70–5.05).
Most immigrant men used emergency services less frequently than Spanish men, except for North and Sub-Saharan Africans (same frequency) and men from Latin America who used these services more frequently: OR 1.68 (95% CI 1.41–1.99). Most immigrant men were hospitalised about as frequently as Spanish men, except men for men from Western countries (less frequently: OR 0.37 (95% CI 0.18–0.75) and sub-Saharan men (more frequently: OR 2.04 (95% CI 1.05–3.96).
Taking Spanish-born women as the reference category, Table 4 shows the ORs associated with health care use by place of origin. After adjusting for age, measures of socioeconomic position, measures of need for health care, and health coverage (model 4), all groups of immigrant women visited GPs about as often as Spanish women did, except for those Sub-Saharan African, who visited GPs more frequently OR 4.06 (95% CI 2.21–7.44) and women from Asia/Oceania who visited them less frequently OR 0.39 (95% CI 0.20–0.80). Most immigrant women visited specialists with about the same frequency as Spanish did, except for those from Latin America and North Africa [less frequently: OR 0.81 (95% CI 0.67–0.98); OR 0.39 (95% CI 0.22–0.71) respectively], and women from Sub-Saharan Africa who visited specialists more frequently OR 2.29 (95% CI 1.06–4.95).
Most immigrant women used emergency services with the same frequency as Spanish women, except for Sub-Saharan Africans who used them more frequently: OR 2.92 (95% CI 1.49–5.72). Most immigrant women were hospitalised as frequently as Spanish women, except for women from Western countries, who were hospitalised more frequently: OR 1.75 (95% CI 1.15–2.67).
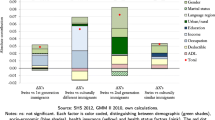
A summary of the principal findings in men and women is shown in Table 5.
Discussion
Although the heterogeneity of the findings in this study do not allow us to define a standard pattern of health services use, some of the most homogeneous results can be highlighted as follows:
-
Immigrant men use health services less frequently than Spanish nationals, with the exception of Latin American men, who more often use emergency services, and Sub-Saharan men, who use specialists more frequently.
-
Immigrant women use health services about as frequently as Spanish women, except for North African women, who visit specialists less frequently, and Asian/Oceanian women, who less often visit GPs. Furthermore, Sub-Saharan women visit GPs and use emergency services more often than Spanish women, and women from Western countries are more frequently hospitalised.
Possible explanations
With regard to the lower use of health services by immigrant men as compared to the native population, it is well documented that immigrants are in better health than the overall native population. This selection bias, known as the healthy migrant bias (Gushulak and MacPherson 2006) could explain the lower use of health services among immigrant men, but not the similar use among immigrant and native women. The lower use of health services by immigrant men as compared to the native population may partly be related to immigrants’ work situation. Although the only information available for this variable was the occupational class of the household reference person, it is often the case that immigrants have greater job insecurity and/or longer workdays than persons in the same occupational class in the native population. These situations have been shown to be related to access to and use of health services (Agudelo-Suárez et al. 2009; García et al. 2009). In contrast, those from the Western countries are more likely to work in highly skilled positions in the primary labour market (Pajares 2007), in which case long workdays, as well as population mobility, could partly be related to their infrequent use of health services. On the other hand, the percentage of male immigrants in rural areas has increased in recent years (Instituto Nacional de Estadística 2007). The limited availability of specialist physicians in these areas may be related to their infrequent use of this resource, as has been seen in other settings (Arcury et al. 2005).
One characteristic not studied, due to the lack of information in the survey, is length of immigrants’ residence in Spain. With increasing time of residence, immigrants may have recourse to different types of resources that permit them to use health services more often. Some studies in Canada and the United States have shown this effect of time of residence of the immigrant population, both on health and on use of health services (Leclere et al. 1994; McDonald and Kennedy 2004). Since immigration is a relatively recent phenomenon in Spain, the limited time of immigrants’ residence in Spain may influence to some degree the lower use of health services observed in some immigrants. However, this does not explain why the use of health services in other immigrants, especially women, is similar to that of the Spanish population.
The influence of cultural reasons in explaining our findings should not be ruled out. Immigrants from Latin America and those from North America used specialist services less than the Spanish population; in contrast, their odds ratios for use of emergency services were higher, although this was significant only in men from Latin America. Cultural proximity due to historic reasons and the common language shared by immigrants from Latin America, may give them more knowledge of the Spanish health system so that they learn to avoid waiting lists for specialist visits using emergency services.
On the other hand, it is possible that immigrants retain the same pattern of behaviour with regard to the health services use in the host country as in their country of origin. In this regard, the lack of universal health coverage in the countries of immigrants from Latin America, Africa and Asia may explain the lower use of health services among male immigrants. It should also be noted that Spain is one of the European countries with the highest frequency of medical visits per inhabitant (World Health Organization/Europe 2009), which may explain why the frequency of health services use is lower in men from Western countries and from Eastern Europe than in Spanish men.
The greater use of health services among the immigrant population from Sub-Saharan Africa could reflect a high frequency of health problems in this population. Several studies show that the burden of disease in this region is very large with respect to other world regions, and that for certain pathologies the disease burden is higher in women than in men (Murray and Lopez 1997; World Health Organization 2004a, b). Also, studies performed in European receiving countries show that immigrants from Sub-Saharan Africa have a worse health profile as compared to other immigrant groups (Venters and Gany 2009).
Likewise, some studies in Spain have shown high mortality from different health problems in immigrants from Sub-Saharan Africa with respect to the Spanish population (Regidor et al. 2008b, 2009).
A recent study showed that African immigrant in Spain use the GP, hospital and hospital emergency services more than the Spanish population (Hernández-Quevedo and Jiménez-Rubio 2009).
In our study, the frequency of negative self-perceived health and of chronic diseases was found to be high in men but low in women from Sub-Saharan Africa. Given the similarity in the pattern of health services use in both sexes, it is possible that the two measures of health used do not adequately reflect the burden of disease in these immigrants.
Although we controlled for variables related to the need for health care in the present study, the subjective value of self-perceived health could be different in different population groups. In fact, the transcultural validity of perceived health has frequently been discussed, and it has been found that the perception of health and its determinants varies among populations (Shetterly et al. 1996).
This situation raises important concerns about the validity of the health measures used as indicators of the need for care. However, it may also indicate that some population groups establish priorities in such a way that health status is not an important determinant of the pattern of health services utilisation; rather, this pattern may be influenced by perceived severity of illness (Torres and Sanz 2000).
Similarly, it is important to note that there may exist a bias in the adjustment for socioeconomic status, since the highest percentage of missing values was seen in the Sub-Saharan African population. This lack of information could be related to use of a proxy to answer in case of communication problems. To try to minimise this bias, the authors included different variables of socio-economic position in the analysis.
In the case of women, the results of the present work show that their use of health services is similar to that of the native population. The fact that immigrant women have less participation in the labour market and dedicate more time to raising children and caring for the extended family could facilitate access to the health system (Pajares 2007). Furthermore, situations related to maternity could increase their knowledge of and contacts with the system.
The similarity between women immigrants and the Spanish population has some exceptions, such as the frequent use of health services by women from Sub-Saharan Africa; as previously discussed. Finally, a surprising result was the high frequency of hospitalisation in women from Western countries, given that their use of the other health services investigated did not differ significantly from that of Spanish women. Although Spain has one of the lowest hospitalisation rates of countries in the Western world (World Health Organization/Europe 2009), this does not seem to be a plausible reason for this finding, since the admission of a patient to hospital is a medical decision depending on the availability of beds at a given moment. Moreover, these results were not seen in men from these countries. Other marked exceptions are the small number of general practitioner visits by women from Asia/Oceania, and of specialist visits by women from North Africa. Future studies on this subject may provide information on the mechanism that explains these findings.
This study has several limitations. A possible limitation of the data source is that the immigrant population might be misrepresented. Specifically, the illegal immigrant population could be under represented. Given that this population may have greater difficulties accessing health care, the association measures may be biased toward the null value. On the other hand, the lack of information on some variables like, time of residence in Spain, occupational status, or administrative situation could partly explain our results (Leclere et al. 1994; McDonald and Kennedy 2004). Finally, the sample size in immigrants from Sub-Saharan Africa and Asia and Oceania was small, which gives rise to wide confidence intervals.
In summary, the heterogeneity found in this study is not new and has been previously documented in the scientific literature. But beyond this, it is important to emphasise the homogeneity and consistency of some of the results: (1) Immigrant men use services less frequently than native men; (2) Immigrant women use them as frequently as native women; (3) Sub-Saharan immigrants, in spite of limitations of the study, seem to constitute a group that uses services more frequently.
It would be desirable to conduct research targeting these groups in order to elucidate if the more frequent use of health services by this group is due to the real health needs or to other factors. Future research on patterns of health services utilisation should incorporate methodological approaches that make it possible to study social, cultural, economic and geographic variables that have not been considered to date, and which may influence these patterns in both immigrants and the native population. Future national surveys in Spain need to consider boosting sample numbers to achieve adequate sample sizes for some groups. In addition, we recommend the use of translators and/or cultural mediators in case of communication problems.
References
Agudelo-Suárez A, Gil-González D, Ronda-Pérez E et al (2009) Discrimination, work and health in immigrant populations in Spain. Soc Sci Med 68:1866–1874
Arcury TA, Gesler WM, Preisser JS, Sherman J, Spencer J, Perin J (2005) The effects of geography and spatial behavior on health care utilization among the residents of a rural region. Health Serv Res 40(1):135–155
Balarajan R, Yuen P, Soni Raleigh V (1989) Ethnic differences in general practitioner consultations. BMJ 299:960
Dunlop DD, Manheim LM, Song J, Chang RW (2002) Gender and ethnic/racial disparities in health care utilization among older adults. J Gerontol B Psychol Sci Soc Sci 57(suppl):S221–S233
García AM, López-Jacob MJ, Agudelo-Suárez AA et al (2009) Condiciones de trabajo y salud en inmigrantes (PROYECTO ITSAL): entrevistas a informantes clave. Gac. Sanit 23(2):91–97
Gillam SJ, Jarman B, White P, Law R (1989) Ethnic differences in consultation rates in urban general practice. BMJ 299:957
Gushulak BD, MacPherson DW (2006) The basic principles of migration health: population mobility and gaps in disease prevalence. Emerg Themes Epidemiol 4(3):3
Hernández-Quevedo C, Jiménez-Rubio D (2009) A comparison of the health status and health care utilization patterns between foreigners and the national population in Spain: new evidence from the Spanish National Health Survey. Soc Sci Med 69(3):370–378
Instituto Nacional de Estadística (2007) Padrón Municipal de Habitantes 2007. http://www.ine.es/inebmenu/mnu_cifraspob.htm. Accessed 24 May 2009
Jiménez-Rubio D, Hernández-Quevedo C (2009) Inequalities in the use of health services between immigrants and the native population in Spain: what is driving the differences?. Eur J Health Econ. doi:10.1007/s10198-010-0220-z
Karl-Trummer U, Novak-Zezula S, Metzler B (2010) Access to health care for undocumented migrants in the EU: a first landscape of NowHereland. Eurohealth 16:13–16
Laroche M (2000) Health status and health services utilization of Canada’s immigrant and non-immigrant population. Can Public Policy 26:51–73
Law 4/2000 (2000) Law 4/2000, in 11th of January, about rights and liberties of foreigners in Spain and their social cohesion. http://www.boe.es/boe/dias/2000/01/12/pdfs/A01139-01150.pdf
Leclere FB, Jensen L, Biddlecom AE (1994) Health care utilization, family context, and adaptation among immigrants in the United States. J Health Soc Behav 35:370–384
McDonald JT, Kennedy S (2004) Insights into the ‘healthy immigrant effect’: health status and health service use of immigrants to Canada. Soc Sci Med 59:1613–1627
Ministerio de Sanidad y Consumo (2006) Encuesta Nacional de Salud de España 2006. http://www.msc.es/estadEstudios/estadisticas/encuestaNacional/encuesta2006.htm. Accessed 4 May 2009
Murray CJL, Lopez AD (1997) Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet 349:1436–1442
Pajares M (2007) Inmigración y Mercado de trabajo. Informe 2007. Análisis de datos de España y Cataluña. Madrid: Subdirección General de Información Administrativa y Publicaciones. Ministerio de Trabajo y Asuntos Sociales
Regidor E, Martínez D, Calle ME, Astasio P, Ortega P, Domínguez V (2008a) Socioeconomic patterns in the use of public and private health services and equity in health care. BMC Health Serv Res 14(8):183
Regidor E, de La Fuente L, Martínez D, Calle ME, Domínguez V (2008b) Heterogeneity in cause-specific mortality according to birthplace in immigrant men residing in Madrid, Spain. Ann Epidemiol 18:605–615
Regidor E, Ronda E, Pascual C, Martínez D, Elisa Calle M, Domínguez V (2009) Mortalidad por enfermedades cardiovasculares en inmigrantes residentes en la Comunidad de Madrid. Med Clin (Barc) 132:621–624
Reijneveld S (1998) Reported health, lifestyles, and use of health care of first generation immigrants in The Netherlands: do socioeconomic factors explain their adverse position? J Epidemiol Community Health 52:298–304
Shetterly SM, Baxter J, Mason LD, Hamman RF (1996) Self-rated health among Hispanic vs non-Hispanic white adults: the San Luis Valley Health and Aging Study. Am J Public Health 86:1798–1801
Song J, Chang RW, Manheim LM, Dunlop DD (2006) Gender differences across race/ethnicity in use of health care among Medicare-aged Americans. J Women Health (Larchmt) 15:1205–1213
Stronks K, Ravelli A, Reijneveld S (2001) Immigrants in the Netherlands: equal access for equal needs? J Epidemiol Community Health 55:701–707
Torres AM, Sanz B (2000) Health care provision for illegal immigrants: should public health be concerned? J Epidemiol Community Health 54:478–479
United Nations (2009) International Migrant Stock: The 2008 Revision. http://esa.un.org/migration/p2k0data.asp. Accessed 30 Oct 2009
Van Doorslaer E (2000) Equity in the delivery of health care in Europe and the US. J Health Econ 19:553–583
Van Doorslaer E, Masseria C, Koolman X (2006) Inequalities in access to medical care by income in developed countries. CMAJ 174(2):177–183
Venters H, Gany F (2009) African Immigrant Health. J Immigr Minor Health. doi:10.1007/s10903-009-9243-x
World Health Organization (2004a) The world health report 2004. Changing history. Geneva: WHO, 2004. http://www.who.int/whr/2004/en/. Accessed 4 May 2009
World Health Organization (2004b) The global burden of disease: 2004 update. Geneva: WHO, 2004. http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/index.html. Accessed 24 May 2009
World Health Organization/Europe (2009) European Health for all database. http://www.euro.who.int/hfadb. Accessed 4 May 2009
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Additional information
This paper belongs to the special issue “Migrants and ethnic minorities in Europe: new challenges for public health research and practice”.
Rights and permissions
About this article
Cite this article
Sanz, B., Regidor, E., Galindo, S. et al. Pattern of health services use by immigrants from different regions of the world residing in Spain. Int J Public Health 56, 567–576 (2011). https://doi.org/10.1007/s00038-011-0237-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00038-011-0237-9