Abstract
Indomethacin is an indol derivative, non-steroidal, anti-inflammatory drug with anti-inflammatory, analgesic, and antipyretic effects. Indomethacin became the first-choice drug to produce an experimental ulcer model as a result of having a higher ulcerogenic potential than other non-steroidal anti-inflammatory drugs (NSAIDs). There have been several conflicting reports about the ulcerogenic mechanism of indomethacin; the mechanism is still unclear. It has been suggested that indomethacin induces gastric damage via inhibiting the release of protective factors like cyclooxygenase-1 (COX-1), prostaglandin E2 (PGE2), bicarbonate, and mucus; increasing aggressive factors like acid; and increasing oxidant parameters while decreasing antioxidant parameters. Classic antiulcer drugs are known to produce antiulcer effects by activating against indomethacin (increasing PGE2, mucus, and bicarbonate production; inhibiting acid secretion; decreasing oxidant parameters; and increasing antioxidants). However, some antiulcer drugs have been shown to inhibit indomethacin-induced ulcers without affecting acid and mucus secretion or oxidant parameters, as well as to inhibit the production of protective factors like COX-1, PGE2, and bicarbonate, and to reduce antioxidant parameters. In order to resolve the contradictions in the abovementioned data, this review hypothesized a relationship between indomethacin-induced ulcers and α 2 adrenergic receptors. It is suggested that blockage of α 2 adrenergic receptors may be responsible for the increase in the aggressive factors induced by indomethacin, and stimulation of α 2 adrenergic receptors may be responsible for the increase of protective factors induced by antiulcer drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Indomethacin is an indol derivative, non-steroidal, anti-inflammatory drug with anti-inflammatory, analgesic, and antipyretic effects [1]. It is used in the treatment of ankylosing spondilitis, osteoarthritis, rheumatoid arthritis, gout arthritis, bursitis, tendonitis, sinovitis, and other inflammatory diseases because of its effective suppression of pain, fever, color, and edema [2–4]. It is known that the inhibition potencies of non-steroidal anti-inflammatory drugs (NSAIDs) on cyclooxygenase-1 (COX-1) and cyclooxygenase-2 (COX-2) enzymes are different [5]. It is believed that while inhibition of COX-1 by NSAIDs causes side effects as a result of reduced prostaglandin (PG) synthesis, inhibition of COX-2 is related to their anti-inflammatory effect [5–7]. Indomethacin potently damages PG synthesis by inhibiting both the COX-1 and COX-2 enzymes [1, 8]. Inhibition of the COX-1 and COX-2 enzymes is necessary for gastric damage to occur [9]. Indomethacin and similar NSAIDs, which inhibit both isoforms of the COX enzyme, produce more severe damage in gastric tissue, even gastrointestinal bleeding when combined with antithrombotic agents [10]. Inhibition of the COX-2 enzyme is thought to be responsible for indomethacin’s anti-inflammatory effect, while inhibition of COX-1 is responsible for its gastrointestinal system (GIS) side effects [10, 11].
Indomethacin became the first-choice drug to produce an experimental ulcer model as a result of having a higher ulcerogenic potential than other NSAIDs [12]. The fact that nimesulide, which is less selective for COX-2, is able to inhibit NSAID-induced gastric damage [13, 14], while celecoxib and rofecoxib, which are more selective for COX-2 (350 to 800 times as selective), are unable to inhibit these ulcers [15], reveals that it is impossible to attribute the GIS side effects of indomethacin and other NSAIDs to the inhibition of only the COX-1 enzyme.
Inhibition of Prostaglandin Synthesis
Prostaglandins are derived from arachidonic acid by phospholipase A2 and cyclooxygenase isoenzymes. Under basal conditions, prostaglandins are synthesized by constitutive cyclooxygenase (COX-1), which is expressed in most cell types [16]. For a better understanding of PG inhibition by indomethacin and other NSAIDs, it is necessary to give a detailed explanation of the COX enzyme system. COX enzyme catalyses the first step in the synthesis of arachidonic acid (AA) metabolites (PG, thromboxane A2, leukotrienes, prostacyclin) [16]. The COX enzyme was first discovered in 1971; later, COX-1, COX-2 (in humans), and COX-3 (in dogs) isoforms were found [17–19]. COX-1 is involved in the synthesis of PGs, which are responsible for platelet aggregation and gastric mucosal protection [20]. However, COX-2 is an inducible protein included in inflammatory reactions [21]. Gastric ulcers and other side effects related to NSAID usage occur as a result of COX-1 inhibition [10, 22]. It has been shown that indomethacin produces gastric damage by reducing PGE2 levels via COX-1 inhibition [23]. Ding et al. reported that indomethacin causes gastric damage by reducing PGE2 levels in stomach tissue [24]. Also, the exogenous administration of PGE2 prevented indomethacin-induced gastric mucosal damage [24, 25]. PGE2 and PGI2 are believed to expose gastroprotective effects by decreasing stomach acid secretion, increasing the thickness of mucus layers, and improving the blood flow of mucosa [26]. However, aspirin, which inhibits cytoprotective PGE2, was shown not to cause gastric damage, even in the case of preventing indomethacin-induced ulcers by intraperitoneal administration [27]. Aspirin may produce gastroprotection due to its effect on 15 epi-lipoxins. Lipoxins are potent anti-inflammatory lipid mediators [28]; their most interesting synthetic pathway is that associated with the acetylation of COX-2 by aspirin. Aspirin acetylates serine residues in both COX-1 and COX-2, leading to conformational changes in the enzyme that alters their ability to metabolize arachidonic acid [29–31]. With both isozymes, acetylation by aspirin leads to a complete blockade of the generation of PGH2. However, aspirin-acetylated COX-2 is still able to convert arachidonic acid to 15-R-Hydroxyeicosatetraenoic acid (15-RHETE), which can subsequently be metabolized via 5-lipoxygenase to 15-R-lipoxin A4 [30]. Lipoxins prevent further neutrophilic infiltration and stimulate local nitric oxide production. Wallace and colleagues have demonstrated this in several reports and have provided evidence for aspirin-triggered lipoxins in the protection of mucosal lesions [32]. However, lipoxin A4 generation is not observed following the administration of non-aspirin NSAIDs such as indomethacin. Moreover, the lipoxin generation is completely inhibited by co-administration of a selective COX-2 inhibitor [33]. Wallace and coworkers had also previously demonstrated [34] that NSAID-induced gastric damage required the inhibition of both COX-1 and COX-2; that is, the selective suppression of either isoform alone did not result in significant gastric damage in otherwise healthy animals. This observation was confirmed by other investigators [35, 36]. Furthermore, recent studies have demonstrated that the acetylation of the COX-1 dimer alters the substrate’s specificity for the second dimer: COX-2 [37]. These data demonstrated that it is difficult to attribute the gastrotoxic effects of indomethacin to only one factor, specifically the inhibition of COX-1. In another study, naloxone could not improve indomethacin-induced PGE2 inhibition, despite increasing the mucosal PGE2 level [38], although morphine could not prevent indomethacin-induced mucosal lesions while it did inhibit aspirin-induced mucosal lesions [39]. Even so, morphine has been reported to increase indomethacin-induced ulcers [40]. This case shows that the ulcerogenic mechanisms of indomethacin and aspirin, which inhibit COX-1 enzymes, are different. Ketotifen, an anti-allergic agent, was found to exert an anti-ulcer effect by reducing the PGE2 level in rats [41]. Lansoprazole, an anti-ulcer agent, does not affect gastric PG production [42]. Although the chronic administration of NSAIDs significantly inhibited PGE2 production, reduction in mucosal lesions (cytoprotection) was observed [43]. These data indicate that there is no direct parallelism between NSAID-induced GIS damage and the degree of COX and/or PG inhibition. Glucocorticoids are also known to suppress the production of arachidonic acid and its metabolites by blocking the induction of the phospholipase A2 enzyme [44, 45]. Thus, stomach damage occurring as a result of inhibited PG synthesis is one of the most prevalent side effects of glucocorticoids [46]. However, the fact that glucocorticoids are ulcerogenic in intact rats while being anti-ulcerogenic in adrenalectomized rats [47] clearly shows that there is no direct relationship between PG inhibition and GIS damage.
In addition to its effects on PG production, indomethacin has been shown to be a prostaglandin D2 (DP) receptor agonist [48, 49], and activation of these receptors promotes chemotaxis of Th2 cells, eosinophils, and basophils, as well as the degranulation of eosinophils and cytokine release from Th2 cells [50–53]. In addition, PGD2 has been demonstrated to be involved in indomethacin-induced gastric ulcer formation; specifically, PGD2 application reduced indomethacin-induced ulcer formation in experimental models [54]. It is unclear why indomethacin both induces ulcers via PGD2 inhibition and behaves like a PGD2 receptor agonist. The literature also suggests that the arachidonic acid pathway cannot be the sole factor in indomethacin-induced ulcers.
Increase of Acid Secretion
The importance of increased gastric acid secretion in the occurrence of severe indomethacin-induced stomach damage has previously been shown [55]. It has been suggested that increased gastric acid secretion results from the inhibition of PG synthesis via indomethacin [23]. Cytoprotective PGs exert their protective effect on GIS mucosa by reducing gastric acid secretion [1, 56]. Most of the anti-ulcer drugs presently used are produced with the aim of reducing gastric acid secretion. Treatment of gastric ulcers by proton pump inhibitors, H2 receptor antagonists, and anticholinergic and anti-acid drugs as a result of gastric acid inhibition can be exemplified [1, 57].
Stimulation of muscarinic receptors (M) in stomach parietal cells increases gastric acid secretion [1]. Anisodamine, an atropine analogue that antagonizes M receptors, has been reported to prevent indomethacin-induced gastric mucosal damage by inhibiting gastric acid secretion [58]. Also, the anti-ulcer effect of diltiazem has been seen in the inhibition of gastric acid secretion [59]. A common property of the drugs used in ulcer treatment is that they are intended for the inhibition of gastric acid [1, 60]. However, morphine could not prevent indomethacin-induced ulcers despite reducing gastric acid secretion [39]. This indicates that the relationship between inhibition of acid secretion and gastroprotection is not convincing. The inability of morphine to prevent indomethacin-induced ulcers despite reducing acid secretion and the inhibition of this effect by naloxone [39, 40] indicate that gastric acid is not an aggressive factor. Atropine, known to be a muscarinic receptor antagonist, reduces gastric acid secretion by blocking M receptors in parietal cells [1]. Atropine significantly prevents indomethacin-induced mucosal ulceration where the cytoprotective effect has decreased after bilateral surgical vagotomy. This proves that atropine produces a gastroprotective effect without reducing gastric acid secretion [61]. Both oral and intraperitoneal (IP) administration of butoxamin reduced indomethacin ulcers; however, oral administration increased PGE2 levels, while IP administration did not affect PGE2 levels [62]. These data expose that there is no relation between either PG and acid secretion or PG-acid secretion and gastric damage.
Increase of Gastric Mucus Production
Prostaglandins are found to produce a gastroprotective effect not only via decreasing acid secretion, but also by increasing the gastric mucus level [63]. The importance of protecting the gastric mucosal barrier in gastroprotection has been shown [64]. In addition to mucosal PG and bicarbonate, reduction of mucus secretion is responsible for indomethacin-induced gastric ulcers [65]. It has also been determined that clonidine produces an anti-ulcer effect by decreasing gastric acid and pepsin secretion and increasing mucus secretion [66]. In an experimental study on rats, Guzel et al. showed that fish oil protects stomach tissue from indomethacin-induced ulcers by increasing the mucus secretion of stomach mucosa [67]. Propranolol protects stomach tissue from indomethacin, ethanol, and stress-induced ulcers by preventing the reduction in mucus levels [68]. In addition, rebamipide, a new anti-ulcer drug, has been reported to increase the gastric levels of PGE2 and PGI2, which can increase gastric mucus concentration [69]. Omeprazole, a classic anti-ulcer drug, is known as not only a proton pump inhibitor, but also as a stimulator of gastric mucus secretion [70]. However, some herbal alkaloids (Rhizoma coptis chinensis) were shown to produce a gastroprotective effect without affecting gastric mucus secretion [71]. These data demonstrate that the relationship between the increase of mucus secretion and gastroprotection is not considerable.
Effects on Bicarbonate Secretion
Gastroprotective PGs (PGE2) are known to increase gastric bicarbonate content [72]. Classic drugs used in peptic ulcer treatment are thought to increase the production of gastrocytoprotective PGs [1, 73]. This information demonstrates the importance of the PG-HCO3 relation in gastroprotection. An example of this is the decrease in bicarbonate secretion in parallel with the reduction in PG amounts in indomethacin-induced ulcers [66, 74]. Drugs with a gastroprotective effect, as well as classic anti-ulcer drugs, increase the basal bicarbonate production of the stomach and the pH of the gastric content [1, 58]. However, Nimacih et al. demonstrated experimentally that nizatidine and ranitidine, classic anti-ulcer drugs, increase HCO3 secretion, while famotidine does not [75]. These data indicate that the relationship between the inhibition of HCO3 secretion and ulcers and/or the stimulation of HCO3 secretion and gastroprotection is not remarkable (Table 1). Thus, we can conclude that it is impossible to associate gastric ulcer formation and cytoprotection with only one factor.
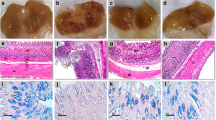
Effects on Oxidant and Antioxidant parameters
The role of toxic oxygen radicals in the etiopathogenesis of indomethacin-induced gastric damage has been shown [76]. Research studies show that antioxidant parameters reduced in gastric tissue with indomethacin-induced damage [77–80]. Indomethacin produces gastric damage via increasing mucosal myeloperoxidase (MPO) and malondialdehyde (MDA) levels [81]. Two hours after indomethacin administration, an acute increase occurs in the production of toxic oxygen radicals (superoxide and hydrogen peroxide) in the gastric mucosa [82]. This shows that gastric damage results from toxic radicals. MPO, present in phagocytic cells (PNL), catalyses toxic hypochlorous acid (HOCl) production from hydrogen peroxide (H2O2) [83]. PNLs cause the excessive uncontrolled production of reactive oxygen species such as superoxide anions (O2-) and hydroxyl radicals (OH-) [84]. Excessive production of MPO and other reactive radicals bring about oxidative damage. Measurement of lipid peroxidation levels is used to determine oxidative damage [85]. Lipid peroxidation is an important reason for cell membrane damage; MDA is the end product of lipid peroxidation and used to indicate the level of lipid peroxidation [86]. Indomethacin-induced increases in mucosal MPO and MDA levels have been improved by classic anti-ulcer drugs like omeprazole and lansoprazole [81]. Diltiazem, a calcium channel blocker, produced an anti-ulcer effect via inhibiting the increase in mucosal MDA [59]. Taurine prevented the gastric damage that occurred as a result of the activation, numerical increase, and adhesion of PNLs after indomethacin administration [87]. This effect shows the importance of MPO and MDA inhibition in preventing indomethacin-induced gastric damage. These neutrophil derivative reactive oxygen species are involved in the formation of indomethacin-induced ulcers [88]. The anti-ulcer and gastroprotective effects of proton pump inhibitors are related to the mechanisms that are not dependent on acidity, such as the prevention of oxidative tissue damage and neutrophil infiltration [70, 81]. This group of drugs decreases various neutrophil functions, like the adhesion of neutrophils to endothelial cells and the acidification of phagocytes and phagolysosomes [89–91]. These data introduce the role of toxic oxygen radicals in ulcer formation. Furthermore, these data show the importance of the reduction of toxic oxygen products in the anti-ulcer activity of drugs, and indicates that the relationship between antioxidant activity and the anti-ulcer effect is more important. Cimetidine, a classic anti-ulcer drug, prevented indomethacin-induced ulcers, although it did not inhibit granulocyte elastase secretion, which depends on leukocyte activation, and it did not decrease the high MPO activity [92]. In another study, diethyl dithiocarbamate (DDC), a superoxide dismutase (SOD) enzyme inhibitor, was determined to prevent indomethacin-induced mucosal damage while inhibiting SOD activity, suggesting that the suppression of gastric motility is more important than antioxidant activity in ulcer healing [93]. While MPO and MDA levels increased in indomethacin administered to rat stomach tissue, enzymatic and nonenzymatic antioxidant parameters decreased, including GSH, glutathione S-transferase (GST), SOD, catalase (CAT), and glutathione peroxidase (GPX) [82, 94–96]. In addition, the inhibition of indomethacin-induced gastric lesions is thought to be related to the antioxidant effect [97]. Pantoprazole produces an anti-ulcer effect via preventing the decrease in GSH levels in indomethacin or other NSAIDs administered to animal gastric tissue [98]. Lansoprazole was shown to produce similar effects to those of pantoprazole by Blandizzi et al. [94]. However, Robert et al. reported that DEM, a sulfhydryl blocker, produces gastroprotection via reducing GSH in gastric mucosa, and that gastric glutathione alone is not protective against stomach damage [99]. This particular study demonstrates that there is no significant relationship between GSH levels and ulcers.
After indomethacin administration, a decrease occurred in the GST and SOD activities in gastric mucosal tissue [95, 96]. However, ranitidine significantly prevented indomethacin-induced ulcers, despite decreasing GST levels more than indomethacin did [96]. The same study demonstrated that an herbal extract that increases GST levels significantly when compared to the control (intact) and indomethacin groups, exerted lower anti-ulcer effects than ranitidine. The prevention or reduction of the increase in SOD activity exacerbates gastric mucosal damage and increasing lipid peroxidation [100]. Improvement of gastric damage using ozonized sunflower oil (OSO) was a treatment found to be related to a significant increase in SOD activity in rat gastric tissue [101]. However, as mentioned above, DDC, which inhibits SOD activity, prevented indomethacin-induced ulcers [93]. This suggests that there are more important factors than antioxidant activity involved in ulcer healing. The CAT and GPX levels decreased in gastric tissue with indomethacin-induced damage [82, 95]. Some literature contradicts these data; specifically, while indomethacin produced ulcers by increasing the CAT level in rat gastric tissue, ranitidine showed an anti-ulcer effect via decreasing CAT and GST activity [96]. Nevertheless, in another study, the effects of ranitidine on CAT and GST activities were found to be insignificant [102]. Ranitidine significantly increased GPX activity, which was decreased by indomethacin [103]. Some research reported that ethanol, known as an ulcerogen agent, increases GPX activity [104]. In addition, in a study performed by Berenguer et al., the anti-ulcer activity of a herbal extract was found to have less of an anti-ulcer effect at the dose that increases GPX activity more [105]. These data show that there is no direct relationship between GPX activity and ulcers.
Indomethacin was found to produce ulcers via increasing gastric acid secretion and decreasing nitric oxide (NO) synthesis [106]. NO is known to regulate acid and gastric mucus secretion and blood flow in stomach tissue [107]. In addition, NO was reported to prevent peroxidation of membrane lipids [108]. A significant decrease was observed in the damaged stomach tissue when compared to healthy tissue; ranitidine produced an anti-ulcer effect by increasing the NO level significantly when compared to the control [102]. There are also data representing reduced NO levels in damaged stomach tissue [109]. Nevertheless, Morsy et al. demonstrated that indomethacin increased the NO level and that eugenol produced an anti-ulcer effect via reducing the NO level (Fig. 1) [110]. The abovementioned contradictory studies also demonstrate that oxidative stress and the antioxidant mechanism are directly responsible for indomethacin-induced ulcers.
a Effects of indomethacin on oxidant and antioxidant parameters in gastric tissue (↑ increases, ↓ decreases, ↑↓ both increases and decreases). b Effects of anti-ulcer drugs on oxidant and antioxidant parameters in gastric tissue of indomethacin given rats (↑ increases, ↓ decreases). c Effects of anti-ulcer drugs on oxidant and antioxidant parameters in gastric tissue of indomethacin given rats (↓ decreases, | not effect). RAN: ranitidine, CIM: cimetidine.
Effects on Other Parameters and Systems
Mukarami et al. indicated the benefits of inhibiting granulocyte elastase, which is released from activated leukocytes, in preventing NSAID-induced gastric lesions; in this study, rebamipide, an anti-ulcer drug, and ONO-5046, an inhibitor of granulocyte elastase, was shown to inhibit indomethacin-induced ulcers, while cimetidine inhibited indomethacin-induced ulcers without inhibiting granulocyte elastase [92].
The prevention of indomethacin-induced ulcers has also been related to the opening of K (ATP) channels. While the K (ATP) channel opener diazoxide prevented indomethacin-induced ulcers, the K (ATP) channel antagonist glibenclamide ameliorated the gastric ulcer [111]. In another study, hydralazine was reported to have no effect on indomethacin-induced ulcers [112]. Hydralazine was reported to be a potassium channel opener [113]. These data cannot completely clarify the role of potassium channel activation in anti-ulcer activity.
Indomethacin produces gastric mucosal lesions with the reduction in the PGE2 level following neutrophil infiltration and an increase in the TNF-α levels in gastric mucosa; exogenous administration of PGE2 produced an anti-ulcer effect by preventing the indomethacin-induced TNF-α increase. In the same study, while pentoxifylline and PGE2 produced an anti-ulcer effect by preventing the increase in TNF-α levels, methotrexate produced an anti-ulcer effect without affecting TNF-α [24].
Indomethacin produces gastric mucosal damage by increasing the cAMP level in gastric mucosal tissue [73]. Also, naloxone was seen to improve indomethacin-induced ulcers by increasing the mucosal cAMP level [38]. These data also fail to explain the formation mechanism of indomethacin-induced ulcers.
A New Hypothesis to Explain Indomethacin-induced Gastric Ulcers: Blockage of α 2 Adrenergic Receptors
Presynaptic α 2 receptors have previously been reported to play a role in the inhibition of indomethacin-, aspirin-, ethanol-, stress-, and pyloric-ligation-induced ulcers [114–116]. α 2 adrenoreceptors have subtypes such as α 2A, α 2B, and α 2C. α 2A receptors have been shown to be responsible for the inhibition of gastric emptying and increased motor activity, while the α 2B and α 2C receptor subtypes are responsible for gastroprotection [117, 118]. α 2 Receptors produce gastroprotective effects through multiple mechanisms [117] that involve the stimulation of α 2 receptors to inhibit gastric acid secretion and motility. These effects occur with the activation of presynaptic α 2 receptors in the vagus nerve and the inhibition of acetylcholine release [118].
In previous studies, nimesulide, an anti-inflammatory drug, was surprisingly shown to prevent indomethacin-induced ulcers in intact rats [13]. However, nimesulide ameliorated indomethacin-induced ulcers in adrenalectomized rats and even produced gastric ulcers when used alone [119]. This situation made researchers hypothesize that there is an adrenal gland–derived factor that has a role in ulcer formation. Then, the authors exhibited the role of cortisol, an adrenal cortex hormone, and adrenaline, an adrenal medulla hormone, in the anti-ulcer effect mechanism of nimesulide [47]. In addition, Filaretova et al. showed that in adrenalectomized rat stomach, corticosterone can antagonize the gastric damage produced by celecoxib, an NSAID [120]. In light of the discovery that glucocorticoids can be gastroprotective in adrenalectomized rats, Suleyman et al. determined that in adrenalectomized rats, the anti-ulcer effect of prednisolone, a glucocorticoid, is antagonized by yohimbine, an α-2 adrenergic receptor blocker [47], suggesting a possible role of α-2 adrenergic receptors in the gastroprotective effects of glucocorticoids. This study also demonstrated that adrenalin prevented indomethacin-induced ulcers in both intact and adrenalectomized rats; however, prednisolone increased indomethacin-induced ulcers in intact rats and decreased indomethacin-induced ulcers in adrenalectomized and/or intact rats whose adrenalin level was decreased via metyrosine [47, 121]. These data demonstrate that increasing glucocorticoid levels when adrenalin presents in the body (at normal levels) produces gastric damage. Additionally, glucocorticoids may produce an anti-ulcer effect by binding α 2 adrenergic receptors in the absence or scarcity of adrenalin [47]. As we mentioned above, the α 2 adrenergic (α 2B, 2C) receptors have been reported to take roles in gastroprotection [117]. Suleyman et al. reported that nimesulide prevents indomethacin-induced ulcers by reducing adrenalin levels [47]. Because of the inhibition of indomethacin-induced ulcers via clonidine, an α 2 adrenergic receptor antagonist [122], we suggest that indomethacin produces gastric damage by blocking α 2 adrenergic receptors. Metyrosine, a thyroxine hydroxylase inhibitor, decreases cathecolamine synthesis by 35% to 80% [123, 124]. Prednisolone, a glucocorticoid, prevented indomethacin-induced ulcers in rats given metyrosine [47]. Furthermore, these data suggest that prednisolone produces an anti-ulcer effect via α 2 adrenergic receptors. L-dopa prevented indomethacin-induced ulcers; while haloperidol, a dopamine antagonist, failed to inhibit the gastroprotective effect of L-dopa, yohimbine successfully inhibited the effects of L-dopa [122]. When we reevaluate these latest data in combination with previous results, we can suggest that there is an extremely significant relationship between indomethacin-induced ulcers and α 2 adrenergic receptors.
Conclusion
In conclusion, this review argued that blockage of α 2 adrenergic receptors may be responsible for the increase of the mentioned aggressive factors induced by indomethacin, and stimulation of α 2 adrenergic receptors may be responsible for the increase of the mentioned protective factors of antiulcer drugs.
References
Botting, R.M. 2006. Inhibitors of cyclooxygenases: mechanisms, selectivity and uses. Journal of Physiology and Pharmacology 57(Suppl 5): 113–124.
Amadio Jr., P., D.M. Cummings, and P. Amadio. 1993. Nonsteroidal anti-inflammatory drugs. Tailoring therapy to achieve results and avoid toxicity. Postgraduate Medicine 93: 73–76. 79–81, 85–8 passim.
Brandman, S., M.J. Vandenburg, R. Jenkins, and W.J. Currie. 1985. The effect of non-steroidal anti-inflammatory therapy on plasma neuropeptide concentrations in patients with osteoarthritis. British Journal of Rheumatology 24: 46–52.
Mitchell, J.A., and T.D. Warner. 1999. Cyclo-oxygenase-2: pharmacology, physiology, biochemistry and relevance to NSAID therapy. British Journal of Pharmacology 128: 1121–1132.
Simon, L.S. 1999. Role and regulation of cyclooxygenase-2 during inflammation. American Journal of Medicine 106: 37S–42S.
Suleyman, H., Z. Halici, E. Cadirci, A. Hacimuftuoglu, and H. Bilen. 2008. Indirect role of beta2-adrenergic receptors in the mechanism of anti-inflammatory action of NSAIDS. Journal of Physiology and Pharmacology 59: 661–672.
Wright, J.M. 2002. The double-edged sword of COX-2 selective NSAIDs. CMAJ 167: 1131–1137.
Patrignani, P. 2000. Nonsteroidal anti-inflammatory drugs, COX-2 and colorectal cancer. Toxicology Letters 112–113: 493–498.
Peskar, B.M., N. Maricic, B. Gretzera, R. Schuligoi, and A. Schmassmann. 2001. Role of cyclooxygenase-2 in gastric mucosal defense. Life Sciences 69: 2993–3003.
Delaney, J.A., L. Opatrny, J.M. Brophy, and S. Suissa. 2007. Drug drug interactions between antithrombotic medications and the risk of gastrointestinal bleeding. Canadian Medical Association Journal 177: 347–351.
Rainsford, K.D. 2007. Anti-inflammatory drugs in the 21st century. Sub-Cellular Biochemistry 42: 3–27.
Sigthorsson, G., R. Crane, T. Simon, M. Hoover, H. Quan, J. Bolognese, et al. 2000. COX-2 inhibition with rofecoxib does not increase intestinal permeability in healthy subjects: a double blind crossover study comparing rofecoxib with placebo and indomethacin. Gut 47: 527–532.
Suleyman, H., F. Akcay, and K. Altinkaynak. 2002. The effect of nimesulide on the indomethacin- and ethanol-induced gastric ulcer in rats. Pharmacological Research 45: 155–158.
Suleyman, H., E. Salamci, E. Cadirci, and Z. Halici. 2007. Beneficial interaction of nimesulide with NSAIDs. Medicinal Chemistry Research 16: 78–87.
Suleyman, H., L.O. Demirezer, and A. Kuruuzum-Uz. 2004. Effects of Rumex patientia root extract on indomethacine and ethanol induced gastric damage in rats. Pharmazie 59: 147–149.
Thuresson, E.D., K.M. Lakkides, C.J. Rieke, Y. Sun, B.A. Wingerd, R. Micielli, et al. 2001. Prostaglandin endoperoxide H synthase-1: the functions of cyclooxygenase active site residues in the binding, positioning, and oxygenation of arachidonic acid. Journal of Biological Chemistry 276: 10347–10357.
Xie, W.L., J.G. Chipman, D.L. Robertson, R.L. Erikson, and D.L. Simmons. 1991. Expression of a mitogen-responsive gene encoding prostaglandin synthase is regulated by mRNA splicing. Proceedings of the National Academy of Sciences of the United States of America 88: 2692–2696.
Chandrasekharan, N.V., H. Dai, K.L. Roos, N.K. Evanson, J. Tomsik, T.S. Elton, et al. 2002. COX-3, a cyclooxygenase-1 variant inhibited by acetaminophen and other analgesic/antipyretic drugs: cloning, structure, and expression. Proceedings of the National Academy of Sciences of the United States of America 99: 13926–13931.
Kujubu, D.A., B.S. Fletcher, B.C. Varnum, R.W. Lim, and H.R. Herschman. 1991. TIS10, a phorbol ester tumor promoter-inducible mRNA from Swiss 3T3 cells, encodes a novel prostaglandin synthase/cyclooxygenase homologue. Journal of Biological Chemistry 266: 12866–12872.
Meade, E.A., W.L. Smith, and D.L. DeWitt. 1993. Differential inhibition of prostaglandin endoperoxide synthase (cyclooxygenase) isozymes by aspirin and other non-steroidal anti-inflammatory drugs. Journal of Biological Chemistry 268: 6610–6614.
Schuschke, D.A., A.S. Adeagbo, P.K. Patibandla, U. Egbuhuzo, R. Fernandez-Botran, and W.T. Johnson. 2009. Cyclooxygenase-2 is upregulated in copper-deficient rats. Inflammation 32: 333–339.
Willoughby, D.A., A.R. Moore, and P.R. Colville-Nash. 2000. COX-1, COX-2, and COX-3 and the future treatment of chronic inflammatory disease. Lancet 355: 646–648.
Kataoka, H., Y. Horie, R. Koyama, S. Nakatsugi, and M. Furukawa. 2000. Interaction between NSAIDs and steroid in rat stomach: safety of nimesulide as a preferential COX-2 inhibitor in the stomach. Digestive Diseases and Sciences 45: 1366–1375.
Ding, S.Z., S.K. Lam, S.T. Yuen, B.C. Wong, W.M. Hui, J. Ho, et al. 1998. Prostaglandin, tumor necrosis factor alpha and neutrophils: causative relationship in indomethacin-induced stomach injuries. European Journal of Pharmacology 348: 257–263.
Appleyard, C.B., D.M. McCafferty, A.W. Tigley, M.G. Swain, and J.L. Wallace. 1996. Tumor necrosis factor mediation of NSAID-induced gastric damage: role of leukocyte adherence. American Journal of Physiology 270: G42–G48.
Buttgereit, F., G.R. Burmester, and L.S. Simon. 2001. Gastrointestinal toxic side effects of nonsteroidal anti-inflammatory drugs and cyclooxygenase-2-specific inhibitors. American Journal of Medicine 110(Suppl 3A): 13S–19S.
Komoike, Y., M. Takeeda, A. Tanaka, S. Kato, and K. Takeuchi. 2002. Prevention by parenteral aspirin of indomethacin-induced gastric lesions in rats: mediation by salicylic acid. Digestive Diseases and Sciences 47: 1538–1545.
Serhan, C.N. 1994. Lipoxin biosynthesis and its impact in inflammatory and vascular events. Biochimica et Biophysica Acta 1212: 1–25.
Mancini, J.A., G.P. O’Neill, C. Bayly, and P.J. Vickers. 1994. Mutation of serine-516 in human prostaglandin G/H synthase-2 to methionine or aspirin acetylation of this residue stimulates 15-R-HETE synthesis. FEBS Letters 342: 33–37.
Claria, J., and C.N. Serhan. 1995. Aspirin triggers previously undescribed bioactive eicosanoids by human endothelial cell-leukocyte interactions. Proceedings of the National Academy of Sciences of the United States of America 92: 9475–9479.
Serhan, C.N., and E. Oliw. 2001. Unorthodox routes to prostanoid formation: new twists in cyclooxygenase-initiated pathways. Journal of Clinical Investigation 107: 1481–1489.
Wallace, J.L., O.M. De Lima Jr., and S. Fiorucci. 2005. Lipoxins in gastric mucosal health and disease. Prostaglandins Leukotrienes and Essential Fatty Acids 73: 251–255.
Fiorucci, S., O.M. De Lima Jr., A. Mencarelli, B. Palazzetti, E. Distrutti, W. McKnight, et al. 2002. Cyclooxygenase-2-derived lipoxin A4 increases gastric resistance to aspirin-induced damage. Gastroenterology 123: 1598–1606.
Wallace, J.L., W. McKnight, B.K. Reuter, and N. Vergnolle. 2000. NSAID-induced gastric damage in rats: requirement for inhibition of both cyclooxygenase 1 and 2. Gastroenterology 119: 706–714.
Gretzer, B., N. Maricic, M. Respondek, R. Schuligoi, and B.M. Peskar. 2001. Effects of specific inhibition of cyclo-oxygenase-1 and cyclo-oxygenase-2 in the rat stomach with normal mucosa and after acid challenge. British Journal of Pharmacology 132: 1565–1573.
Tanaka, A., H. Araki, Y. Komoike, S. Hase, and K. Takeuchi. 2001. Inhibition of both COX-1 and COX-2 is required for development of gastric damage in response to nonsteroidal antiinflammatory drugs. Journal of Physiology Paris 95: 21–27.
Yuan, C., R.S. Sidhu, D.V. Kuklev, Y. Kado, M. Wada, I. Song, et al. 2009. Cyclooxygenase Allosterism, Fatty Acid-mediated Cross-talk between Monomers of Cyclooxygenase Homodimers. Journal of Biological Chemistry 284: 10046–10055.
Waisman, Y., G. Dinari, H. Marcus, M. Ligumsky, Y. Rosenbach, I. Zahavi, et al. 1985. Naloxone is protective against indomethacin-induced intestinal ulceration in the rat. Gastroenterology 89: 86–91.
Tazi-Saad, K., J. Chariot, J. Vatier, M. Del Tacca, and C. Roze. 1991. Antisecretory and anti-ulcer effects of morphine in rats after gastric mucosal aggression. European Journal of Pharmacology 192: 271–277.
Gyires, K., S. Furst, E. Farczadi, and A. Marton. 1985. Morphine potentiates the gastroulcerogenic effect of indometacin in rats. Pharmacology 30: 25–31.
Zahavi, I., T. Weizen, H. Marcus, F. Karmeli, and G. Dinari. 1996. Ketotifen is protective against indomethacin-induced intestinal ulceration in the rat. Israel Journal of Medical Sciences 32: 312–315.
Fukuda, T., T. Arakawa, Y. Shimizu, K. Ohtani, K. Higuchi, and K. Kobayashi. 1995. Effects of lansoprazole on ethanol-induced injury and PG synthetic activity in rat gastric mucosa. Journal of Clinical Gastroenterology 20(Suppl 2): S5–S7.
Brzozowski, T., P.C. Konturek, S.J. Konturek, I. Brzozowska, and T. Pawlik. 2005. Role of prostaglandins in gastroprotection and gastric adaptation. Journal of Physiology and Pharmacology 56(Suppl 5): 33–55.
Dennis, E.A. 2000. Phospholipase A2 in eicosanoid generation. American Journal of Respiratory and Critical Care Medicine 161: S32–S35.
Schimmer, B.P., and K.L. Parker. 1996. Adrenocorticotropin hormone. In Goodman & Gilman’s the pharmacological basis of therapeutics. Vol. 9, ed. L.S. Goodman, L.E. Limbird, P.B. Milinoff, and R.W. Ruddon, 1458–1485. New York: Mc Graw-Hill.
Bailey, J.M. 1991. New mechanisms for effects of anti-inflammatory glucocorticoids. Biofactors 3: 97–102.
Suleyman, H., Z. Halici, E. Cadirci, A. Hacimuftuoglu, S. Keles, and F. Gocer. 2007. Indirect role of alpha2-adrenoreceptors in anti-ulcer effect mechanism of nimesulide in rats. Naunyn-Schmiedebergs Archives of Pharmacology 375: 189–198.
Hirai, H., K. Tanaka, S. Takano, M. Ichimasa, M. Nakamura, and K. Nagata. 2002. Cutting edge: agonistic effect of indomethacin on a prostaglandin D2 receptor, CRTH2. Journal of Immunology 168: 981–985.
Stubbs, V.E., P. Schratl, A. Hartnell, T.J. Williams, B.A. Peskar, A. Heinemann, et al. 2002. Indomethacin causes prostaglandin D(2)-like and eotaxin-like selective responses in eosinophils and basophils. Journal of Biological Chemistry 277: 26012–26020.
Hirai, H., K. Tanaka, O. Yoshie, K. Ogawa, K. Kenmotsu, Y. Takamori, et al. 2001. Prostaglandin D2 selectively induces chemotaxis in T helper type 2 cells, eosinophils, and basophils via seven-transmembrane receptor CRTH2. Journal of Experimental Medicine 193: 255–261.
Monneret, G., S. Gravel, M. Diamond, J. Rokach, and W.S. Powell. 2001. Prostaglandin D2 is a potent chemoattractant for human eosinophils that acts via a novel DP receptor. Blood 98: 1942–1948.
Gervais, F.G., R.P. Cruz, A. Chateauneuf, S. Gale, N. Sawyer, F. Nantel, et al. 2001. Selective modulation of chemokinesis, degranulation, and apoptosis in eosinophils through the PGD2 receptors CRTH2 and DP. Journal of Allergy and Clinical Immunology 108: 982–988.
Tanaka, K., H. Hirai, S. Takano, M. Nakamura, and K. Nagata. 2004. Effects of prostaglandin D2 on helper T cell functions. Biochemical and Biophysical Research Communications 316: 1009–1014.
Goto, H., S. Nakazawa, K. Segawa, Y. Tsukamoto, S. Hase, T. Arisawa, et al. 1989. The role of prostaglandin D2 in the genesis of indomethacin-induced gastric lesions in rats. Scandinavian Journal of Gastroenterology Supplement 162: 91–94.
Filaretova, L., A. Tanaka, T. Miyazawa, S. Kato, and K. Takeuchi. 2002. Mechanisms by which endogenous glucocorticoid protects against indomethacin-induced gastric injury in rats. American Journal of Physiology Gastrointestinal and Liver Physiology 283: G1082–G1089.
Isakson, P. C., K. M. Verburg, T. J. Maziasz, G. S. Geis. 1999. Selective inhibitors of COX-2. Gastroenterology, 12.
Zanatta, F., R.B. Gandolfi, M. Lemos, J.C. Ticona, A. Gimenez, B.K. Clasen, et al. 2009. Gastroprotective activity of alkaloid extract and 2-phenylquinoline obtained from the bark of Galipea longiflora Krause (Rutaceae). Chemico-Biological Interactions 180: 312–317.
Yong, D.G., B.Q. Geng, G.G. Gu, F.M. Zhong, and W.H. Yu. 1991. Anti-ulcer effect of anisodamine in rats. Zhongguo Yao Li Xue Bao 12: 522–525.
Yong, D.G., B.Q. Geng, Y. Li, and S. Bi. 1995. Antiulcer effect of diltiazem in rats. Zhongguo Yao Li Xue Bao 16: 517–520.
Welage, L.S. 2003. Pharmacologic properties of proton pump inhibitors. Pharmacotherapy 23: 74S–80S.
Karadi, O., Z. Nagy, B. Bodis, and G. Mozsik. 2001. Atropine-induced gastrointestinal cytoprotection dependences to the intact of vagal nerve against indomethacin-induced gastrointestinal mucosal and microvascular damage in rats. Journsl of Physiol Paris 95: 29–33.
Kaan, S.K., and C.H. Cho. 1997. Effects of selective beta-adrenoceptor antagonists on gastric ulceration in the rat. Journal of Pharmacy and Pharmacology 49: 200–205.
Ruppin, H., B. Person, A. Robert, and W. Domschke. 1981. Gastric cytoprotection in man by prostaglandin E2. Scandinavian Journal of Gastroenterology 16: 647–652.
Gu, G.G., D.G. Yong, and B.Q. Geng. 1990. Anti-gastric ulcer activity of zinc sulfadiazine in rats. Zhongguo Yao Li Xue Bao 11: 460–462.
Luo, G.Y., Y. He, and L.B. Tu. 1990. Effects of clonidine on experimental stomach ulcer in rats. Zhongguo Yao Li Xue Bao 11: 457–459.
Kapui, Z., K. Boer, I. Rozsa, G. Blasko, and I. Hermecz. 1993. Investigations of indomethacin-induced gastric ulcer in rats. Arzneimittel-Forschung 43: 767–771.
Guzel, C., G. Ulak, A. Sermet, R. Cicek, and M. Ulak. 1995. Effect of fish oil on indometacin-induced gastric lesions in rats. Arzneimittel-Forschung 45: 1172–1173.
Kaan, S.K., and C.H. Cho. 1996. A study of the antiulcer mechanisms of propranolol in rats. Inflammation Research 45: 370–375.
Kleine, A., S. Kluge, and B.M. Peskar. 1993. Stimulation of prostaglandin biosynthesis mediates gastroprotective effect of rebamipide in rats. Digestive Diseases and Sciences 38: 1441–1449.
Kobayashi, T., Y. Ohta, K. Inui, J. Yoshino, and S. Nakazawa. 2002. Protective effect of omeprazole against acute gastric mucosal lesions induced by compound 48/80, a mast cell degranulator, in rats. Pharmacological Research 46: 75–84.
Li, B., H.R. Liu, Y.Q. Pan, Q.S. Jiang, J.C. Shang, X.H. Wan, et al. 2006. Protective effects of total alkaloids from rhizoma Coptis chinensis on alcohol-induced gastric lesion in rats. Zhongguo Zhong Yao Za Zhi 31: 51–54.
Takeuchi, K., E. Aihara, Y. Sasaki, Y. Nomura, and F. Ise. 2006. Involvement of cyclooxygenase-1, prostaglandin E2 and EP1 receptors in acid-induced HCO3- secretion in stomach. Journal of Physiology and Pharmacology 57: 661–676.
Waisman, Y., I. Zahavi, H. Marcus, M. Ligumsky, Y. Rosenbach, and G. Dinari. 1988. Sucralfate is protective against indomethacin-induced intestinal ulceration in the rat. Digestion 41: 78–82.
Ueki, S., K. Takeuchi, and S. Okabe. 1988. Gastric motility is an important factor in the pathogenesis of indomethacin-induced gastric mucosal lesions in rats. Digestive Diseases and Sciences 33: 209–216.
Mimaki, H., S. Kawauchi, S. Kagawa, S. Ueki, and K. Takeuchi. 2001. Bicarbonate stimulatory action of nizatidine, a histamine H(2)-receptor antagonist, in rat duodenums. Journal of Physiology Paris 95: 165–171.
Naito, Y., T. Yoshikawa, N. Yoshida, and M. Kondo. 1998. Role of oxygen radical and lipid peroxidation in indomethacin-induced gastric mucosal injury. Digestive Diseases and Sciences 43: 30S–34S.
Dengiz, G.O., F. Odabasoglu, Z. Halici, E. Cadirci, and H. Suleyman. 2007. Gastroprotective and antioxidant effects of montelukast on indomethacin-induced gastric ulcer in rats. Journal of Pharmacological Sciences 105: 94–102.
Dengiz, G.O., F. Odabasoglu, Z. Halici, H. Suleyman, E. Cadirci, and Y. Bayir. 2007. Gastroprotective and antioxidant effects of amiodarone on indomethacin-induced gastric ulcers in rats. Archives of Pharmacal Research 30: 1426–1434.
El-Missiry, M.A., I.H. El-Sayed, and A.I. Othman. 2001. Protection by metal complexes with SOD-mimetic activity against oxidative gastric injury induced by indomethacin and ethanol in rats. Annals of Clinical Biochemistry 38: 694–700.
Suleyman, H., E. Cadirci, A. Albayrak, B. Polat, Z. Halici, F. Koc, et al. 2009. Comparative study on the gastroprotective potential of some antidepressants in indomethacin-induced ulcer in rats. Chemico-Biological Interactions 180: 318–324.
Pozzoli, C., A. Menozzi, D. Grandi, E. Solenghi, M.C. Ossiprandi, C. Zullian, et al. 2007. Protective effects of proton pump inhibitors against indomethacin-induced lesions in the rat small intestine. Naunyn-Schmiedebergs Archives of Pharmacology 374: 283–291.
Hassan, A., E. Martin, and P. Puig-Parellada. 1998. Role of antioxidants in gastric mucosal damage induced by indomethacin in rats. Methods and Findings in Experimental and Clinical Pharmacology 20: 849–854.
Hiraishi, H., A. Terano, S. Ota, H. Mutoh, T. Sugimoto, T. Harada, et al. 1994. Protection of cultured rat gastric cells against oxidant-induced damage by exogenous glutathione. Gastroenterology 106: 1199–1207.
Suzuki, M., M. Mori, S. Miura, M. Suematsu, D. Fukumura, H. Kimura, et al. 1996. Omeprazole attenuates oxygen-derived free radical production from human neutrophils. Free Radical Biology and Medicine 21: 727–731.
Peralta, C., R. Rull, A. Rimola, R. Deulofeu, J. Rosello-Catafau, E. Gelpi, et al. 2001. Endogenous nitric oxide and exogenous nitric oxide supplementation in hepatic ischemia-reperfusion injury in the rat. Transplantation 71: 529–536.
Nielsen, F., B.B. Mikkelsen, J.B. Nielsen, H.R. Andersen, and P. Grandjean. 1997. Plasma malondialdehyde as biomarker for oxidative stress: reference interval and effects of life-style factors. Clinical Chemistry 43: 1209–1214.
Son, M., H.K. Kim, W.B. Kim, J. Yang, and B.K. Kim. 1996. Protective effect of taurine on indomethacin-induced gastric mucosal injury. Advances in Experimental Medicine and Biology 403: 147–155.
Vaananen, P.M., J.B. Meddings, and J.L. Wallace. 1991. Role of oxygen-derived free radicals in indomethacin-induced gastric injury. American Journal of Physiology 261: G470–G475.
Agastya, G., B.C. West, and J.M. Callahan. 2000. Omeprazole inhibits phagocytosis and acidification of phagolysosomes of normal human neutrophils in vitro. Immunopharmacology and Immunotoxicology 22: 357–372.
Suzuki, M., M. Mori, D. Fukumura, H. Suzuki, S. Miura, and H. Ishii. 1999. Omeprazole attenuates neutrophil-endothelial cell adhesive interaction induced by extracts of Helicobacter pylori. Journal of Gastroenterology and Hepatology 14: 27–31.
Wandall, J.H. 1992. Effects of omeprazole on neutrophil chemotaxis, super oxide production, degranulation, and translocation of cytochrome b-245. Gut 33: 617–621.
Murakami, K., K. Okajima, M. Uchiba, N. Harada, M. Johno, H. Okabe, et al. 1997. Rebamipide attenuates indomethacin-induced gastric mucosal lesion formation by inhibiting activation of leukocytes in rats. Digestive Diseases and Sciences 42: 319–325.
Takeuchi, K., K. Takehara, and T. Ohuchi. 1996. Diethyldithiocarbamate, a superoxide dismutase inhibitor, reduces indomethacin-induced gastric lesions in rats. Digestion 57: 201–209.
Blandizzi, C., M. Fornai, R. Colucci, G. Natale, V. Lubrano, C. Vassalle, et al. 2005. Lansoprazole prevents experimental gastric injury induced by non-steroidal anti-inflammatory drugs through a reduction of mucosal oxidative damage. World Journal of Gastroenterology 11: 4052–4060.
Tanaka, J., and Y. Yuda. 1996. Lipid peroxidation in gastric mucosal lesions induced by indomethacin in rat. Biological and Pharmaceutical Bulletin 19: 716–720.
Halici, M., F. Odabasoglu, H. Suleyman, A. Cakir, A. Aslan, and Y. Bayir. 2005. Effects of water extract of Usnea longissima on antioxidant enzyme activity and mucosal damage caused by indomethacin in rats. Phytomedicine 12: 656–662.
Erkin, B., D. Dokmeci, S. Altaner, and F.N. Turan. 2006. Gastroprotective effect of L-carnitine on indomethacin-induced gastric mucosal injury in rats: a preliminary study. Folia Medica (Plovdiv) 48: 86–89.
Fornai, M., G. Natale, R. Colucci, M. Tuccori, G. Carazzina, L. Antonioli, et al. 2005. Mechanisms of protection by pantoprazole against NSAID-induced gastric mucosal damage. Naunyn-Schmiedebergs Archives of Pharmacology 372: 79–87.
Robert, A., C. Lancaster, J.P. Davis, S.O. Field, A.J. Sinha, and B.A. Thornburgh. 1985. Cytoprotection by prostaglandin occurs in spite of penetration of absolute ethanol into the gastric mucosa. Gastroenterology 88: 328–333.
van der Vliet, A., and A. Bast. 1992. Role of reactive oxygen species in intestinal diseases. Free Radical Biology and Medicine 12: 499–513.
Zamora, Z., R. Gonzalez, D. Guanche, N. Merino, S. Menendez, F. Hernandez, et al. 2008. Ozonized sunflower oil reduces oxidative damage induced by indomethacin in rat gastric mucosa. Inflammation Research 57: 39–43.
Bayir, Y., F. Odabasoglu, A. Cakir, A. Aslan, H. Suleyman, M. Halici, et al. 2006. The inhibition of gastric mucosal lesion, oxidative stress and neutrophil-infiltration in rats by the lichen constituent diffractaic acid. Phytomedicine 13: 584–590.
Fields, M., C.G. Lewis, and M.D. Lure. 1996. Antioxidant defense system in lung of male and female rats: interactions with alcohol, copper, and type of dietary carbohydrate. Metabolism 45: 49–56.
Cadirci, E., H. Suleyman, H. Aksoy, Z. Halici, U. Ozgen, A. Koc, et al. 2007. Effects of Onosma armeniacum root extract on ethanol-induced oxidative stress in stomach tissue of rats. Chemico-Biological Interactions 170: 40–48.
Berenguer, B., L.M. Sanchez, A. Quilez, M. Lopez-Barreiro, O. de Haro, J. Galvez, et al. 2006. Protective and antioxidant effects of Rhizophora mangle L. against NSAID-induced gastric ulcers. Journal of Ethnopharmacology 103: 194–200.
Lanas, A., E. Bajador, P. Serrano, J. Fuentes, S. Carreno, J. Guardia, et al. 2000. Nitrovasodilators, low-dose aspirin, other nonsteroidal antiinflammatory drugs, and the risk of upper gastrointestinal bleeding. New England Journal of Medicine 343: 834–839.
Martin, M.J., M.D. Jimenez, and V. Motilva. 2001. New issues about nitric oxide and its effects on the gastrointestinal tract. Current Pharmceutical Design 7: 881–908.
Hogg, N., and B. Kalyanaraman. 1999. Nitric oxide and lipid peroxidation. Biochimica et Biophysica Acta 1411: 378–384.
Fan, T.Y., Q.Q. Feng, C.R. Jia, Q. Fan, C.A. Li, and X.L. Bai. 2005. Protective effect of Weikang decoction and partial ingredients on model rat with gastric mucosa ulcer. World Journal of Gastroenterology 11: 1204–1209.
Morsy, M.A., and A.A. Fouad. 2008. Mechanisms of gastroprotective effect of eugenol in indomethacin-induced ulcer in rats. Phytotherapy Research 22: 1361–1366.
Toroudi, H.P., M. Rahgozar, A. Bakhtiarian, and B. Djahanguiri. 1999. Potassium channel modulators and indomethacin-induced gastric ulceration in rats. Scandinavian Journal of Gastroenterology 34: 962–966.
al-Bekairi, A.M., A.M. al-Rajhi, and M. Tariq. 1994. Effect of (+/−)-verapamil and hydralazine on stress- and chemically-induced gastric ulcers in rats. Pharmacological Research 29: 225–236.
Bang, L., J.E. Nielsen-Kudsk, N. Gruhn, S. Trautner, S.A. Theilgaard, S.P. Olesen, et al. 1998. Hydralazine-induced vasodilation involves opening of high conductance Ca2+-activated K+ channels. European Journal of Pharmacology 361: 43–49.
Del Soldato, P. 1986. Gastric lesion-preventing or -potentiating activity of clonidine in rats. Japanese Journal of Pharmacology 41: 257–259.
DiJoseph, J.F., J.R. Eash, and G.N. Mir. 1987. Gastric antisecretory and antiulcer effects of WHR1582A, a compound exerting alpha-2 adrenoceptor agonist activity. Journal of Pharmacology and Experimental Therapeutics 241: 97–102.
Kunchandy, J., S. Khanna, and S.K. Kulkarni. 1985. Effect of alpha2 agonists clonidine, guanfacine and B-HT 920 on gastric acid secretion and ulcers in rats. Archives Internationales de Pharmacodynamie et de Therapie 275: 123–138.
Gyires, K., K. Mullner, S. Furst, and A.Z. Ronai. 2000. Alpha-2 adrenergic and opioid receptor-mediated gastroprotection. Journal of Physiology Paris 94: 117–121.
Fulop, K., Z. Zadori, A.Z. Ronai, and K. Gyires. 2005. Characterisation of alpha2-adrenoceptor subtypes involved in gastric emptying, gastric motility and gastric mucosal defence. European Journal of Pharmacology 528: 150–157.
Suleyman, H., B. Demircan, F. Gocer, Z. Halici, and A. Hacimuftuoglu. 2004. Role of adrenal gland hormones in the mechanism of antiulcer action of nimesulide and ranitidine. Polish Journal of Pharmacology 56: 799–804.
Filaretova, L., A. Tanaka, Y. Komoike, and K. Takeuchi. 2002. Selective cyclooxygenase-2 inhibitor induces gastric mucosal damage in adrenalectomized rats. Inflammopharmacology 10: 413–422.
Suleyman, H., E. Cadirci, A. Albayrak, and Z. Halici. 2008. Nimesulide is a selective COX-2 inhibitory, atypical non-steroidal anti-inflammatory drug. Current Medecinal Chemistry 15: 278–283.
Kiro, A., I. Zahavi, H. Marcus, and G. Dinari. 1992. L-dopa is protective against indomethacin-induced small intestinal ulceration in the rat: possible role of an alpha-2-adrenergic mechanism. Life Sciences 51: 1151–1156.
Hoffman, B.B. 2006. Therapy of hypertension. In Godman and Gilman’s the pharmacological basis of therapeutics, ed. L.L. Brunton, 845–897. New-York: Mc Graw-Hill.
Reams, G.P., and J.H. Bauer. 1999. Atlas of diseases of the kidney, 28–30. Philadelphia: Blackwell Science.
Acknowledgment
We would like to express our thanks to Research Assistant Mss. Beyzagul Polat for her contribution to this work.
Disclosure
None of the authors has any conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Suleyman, H., Albayrak, A., Bilici, M. et al. Different Mechanisms in Formation and Prevention of Indomethacin-induced Gastric Ulcers. Inflammation 33, 224–234 (2010). https://doi.org/10.1007/s10753-009-9176-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-009-9176-5