Abstract
Membrane endoglin (Eng, CD105) is a transmembrane glycoprotein essential for the proper function of vascular endothelium. It might be cleaved by matrix metalloproteinases to form soluble endoglin (sEng), which is released into the circulation. Metabolic syndrome comprises conditions/symptoms that usually coincide (endothelial dysfunction, arterial hypertension, hyperglycemia, obesity-related insulin resistance, and hypercholesterolemia), and are considered risk factors for cardiometabolic disorders such as atherosclerosis, type II diabetes mellitus, and liver disorders. The purpose of this review is to highlight current knowledge about the role of Eng and sEng in the disorders mentioned above, in vivo and in vitro extent, where we can find a wide range of contradictory results. We propose that reduced Eng expression is a hallmark of endothelial dysfunction development in chronic pathologies related to metabolic syndrome. Eng expression is also essential for leukocyte transmigration and acute inflammation, suggesting that Eng is crucial for the regulation of endothelial function during the acute phase of vascular defense reaction to harmful conditions. sEng was shown to be a circulating biomarker of preeclampsia, and we propose that it might be a biomarker of metabolic syndrome-related symptoms and pathologies, including hypercholesterolemia, hyperglycemia, arterial hypertension, and diabetes mellitus as well, despite the fact that some contradictory findings have been reported. Besides, sEng can participate in the development of endothelial dysfunction and promote the development of arterial hypertension, suggesting that high levels of sEng promote metabolic syndrome symptoms and complications. Therefore, we suggest that the treatment of metabolic syndrome should take into account the importance of Eng in the endothelial function and levels of sEng as a biomarker and risk factor of related pathologies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endoglin (Eng, CD105) is a 180 kDa transmembrane glycoprotein considered a co-receptor for ligands of the Transforming Growth Factor β (TGFβ) superfamily, with an increasing research interest and currently over 2800 citations in PubMed. Eng is involved in the physiological function of the endothelium, but also plays an essential role in various pathological conditions. There are two different isoforms of membrane Eng expressed by various cells and soluble endoglin (sEng) circulating in plasma or cell culture medium [1].
Eng is expressed by endothelial cells, vascular smooth muscle cells [2], fibroblasts [3], hepatic stellate cells [4], and activated monocytes and macrophages [5]. Changes in Eng expression and function are predominantly associated with several pathological conditions, including Hereditary hemorrhagic telangiectasia (HHT) [6], cancer, angiogenesis [7], heart development [8], fibrosis [9], endothelial dysfunction [10], and inflammation [11].
sEng is the N-terminal cleavage product of the extracellular domain of Eng formed by the activity of matrix metalloproteinases [12,13,14] that is released into the circulation. sEng can be detected and used as a biomarker in patients with various cardiovascular and metabolic disorders such as familial hypercholesterolemia [15, 16], arterial hypertension [17], preeclampsia [18], and diabetes mellitus [19].
The role of the membrane and soluble endoglin in cardiovascular diseases, atherosclerosis, and endothelial dysfunction, were reviewed previously [20, 21]. Furthermore, an excellent review focusing on the role of Eng in angiogenesis, cancer, and immune cells, was recently published by Schoonderwoerd et al. [22]. Indeed, sEng was demonstrated to be a circulating biomarker of development and progression of preeclampsia [18]. However, the elaborate summary of the Eng and sEng role in cardiovascular disorders associated with altered glucose and lipid metabolism was not summarized yet. Metabolic syndrome comprises conditions/symptoms that usually co-occur (endothelial dysfunction, arterial hypertension, hyperglycemia, obesity-related insulin resistance, and hypercholesterolemia or hypertriglyceridemia) and are considered as the risk factors for cardiometabolic disorders such as atherosclerosis, type II diabetes mellitus, and liver disorders. This review aims to critically evaluate recent results and update some information in the light of recent papers regarding membrane and soluble endoglin with respect to metabolic syndrome-related pathologies.
Membrane endoglin structure and signaling
Eng is composed of two disulfide-linked transmembrane monomers, as shown in Fig. 1. According to its structure, Eng belongs to the family of proteins containing the zona pellucida domain [23]. Eng contains an extracellular part, hydrophobic intramembrane part, and short serine/threonine-rich cytoplasmic region. The extracellular part of Eng contains the orphan domain (which does not show any homology with other protein families) and the zona pellucida (ZP) part (responsible for protein–protein interaction). Part of the ZP domain is arginyl-glycyl-aspartic acid (RGD), a fundamental recognition structure for the binding with integrins and other RGD receptors [24, 25].
Schematic of Eng and its cleavage product sEng. The extracellular part of Eng consists of the orphan domain and the ZP domain. ZP domain contains the RGD motif, which is a crucial recognition structure for the binding with integrins and other RGD receptors. Matrix metalloproteinases can cleave the whole extracellular part of Eng and produce sEng, which is released into the circulation or cell culture media. Up to date, both soluble forms of endoglin, including monomer and dimer, were proposed to be detected in the circulation
Two alternatively spliced isoforms of Eng have been identified [26]. Their structure differs in the number of amino acids in the cytoplasmatic tail, level of phosphorylation, and affinity to receptors (Fig. 2) [27].
Role of different Eng isoforms in the endothelium. S-Eng participates in TGFβRII/ALK5-mediated signaling, where it promotes SMAD2/3 phosphorylation. Phosphorylated SMAD2/3 (pSMAD2/3) binds with common mediator SMAD4 (co-SMAD4) and creates an active complex. This complex translocates to the nucleus and induces transcription of genes related to the quiescent endothelial cell phenotype. On the other hand, L-Eng participates in BMP9 and in both TGFβRII/ALK1 and TGFβRII/ALK5-mediated signaling, as well. L-Eng promotes TGFβRII/ALK1—SMAD1/5/8 pathway and inhibits TGFβRII/ALK5–SMAD 2/3 pathway. Binding of phosphorylated SMAD1/5/8 (pSMAD1/5/8) with co-SMAD4 creates an active complex. Translocation of this complex to the nucleus induces transcription of genes related to activated endothelial cells phenotype
Long endoglin (L-Eng) is a predominantly expressed Eng isoform. L-Eng contains a cytoplasmatic chain with 47 amino acids, and it is known to stimulate endothelial cell migration, proliferation, and angiogenesis through Eng/ALK1/SMAD1/5/8 pathway. Short endoglin (S-Eng) is a minor isoform of Eng with a cytoplasmatic chain composed of 14 amino acids. S-Eng expression seems to inhibit endothelial cell proliferation, migration, and it was shown to induce endothelial cell senescence through Eng/ALK5/SMAD2/3 pathway [27]. However, the exact role of S-Eng was not widely explored [22, 26].
L-Eng isoform is the predominantly expressed isoform and plays a crucial role in pathological conditions. This review mainly focuses on L-Eng, which is mentioned as Eng in this paper.
Membrane endoglin expression and function in cardiometabolic disorders in vivo and in vitro
Eng expression is predominant in the cells found in the vessel wall, including endothelial cells, monocytes/macrophages, fibroblasts, and vascular smooth muscle cells (SMCs) [28]. It is also expressed, in lesser amounts, in other cell types, for instance, in hepatic stellate cells [4]. We reviewed the role of Eng in atherosclerosis and endothelial dysfunction, where we suggested the importance of proper Eng expression and signaling in healthy endothelium and its potential involvement in the development/progression of atherogenesis [21]. In the current review, we significantly extend that information and try to highlight novel findings in the field, regarding the importance of Eng expression and function in metabolic syndrome-related pathologies.
Membrane endoglin, hypercholesterolemia, endothelial nitric oxide synthase, endothelial dysfunction, and inflammation
Endothelial nitric oxide synthase (eNOS) is a crucial enzyme maintaining the proper function of vascular endothelium. For instance, when the activity of eNOS is reduced by hypercholesterolemia and/or inflammation, it may result in the development of endothelial dysfunction [29].
Several studies showed a mutual relationship between Eng, eNOS, and the proper function of the endothelium. It was demonstrated that changes in Eng levels result in the alteration of blood vessels function and possibly to the development of endothelial dysfunction [10, 30].
For instance, decreased expression of eNOS in Eng haploinsufficient mice (Eng±) resulted in impaired endothelium-dependent vasodilation in mice [30]. In addition, Toporsian et al. found that Eng is an essential component of the eNOS activation complex and that it stabilizes eNOS protein, which indicates the crucial role of Eng in the regulation of local vascular tone [31]. Another in vitro study, published by Santibanez et al., showed that Eng increases SMAD2 protein levels, phosphorylation status, and stability, which results in an increased eNOS expression in either absence or presence of exogenous TGF-β1 in endothelial cells [32]. Last but not least, reduced Eng/eNOS expression was also demonstrated in vitro in human umbilical vein endothelial cells (HUVECs) after the simulation of inflammation by the treatment with TNF-α [33].
Also, Jerkic et al. used mouse endothelial cells derived from the yolk sac of Eng homozygous Eng−/−, heterozygous Eng± and control Eng+/+ mice during embryonic day 8.5 to demonstrate the role of Eng in endothelial function [34]. In Eng± deficient cells, they showed decreased levels of protein stabilizing factors VEGFR2, PAK-1, VE-cadherin, and Rac-2 and increased levels of endothelial barrier destabilizing factors TSP-1 and CD148. Destabilization of the endothelial barrier was related to increased RhoA activation and increased permeability of neutrophils through the endothelial barrier. They suggested that reduced Eng expression results in increased endothelial permeability and impairment of endothelial barrier function, which are general hallmarks of endothelial dysfunction [34]. Similarly, Anderberg et al. showed significantly weakened endothelial cell barrier to tumor cell intravasation and extravasation enhanced ALK5 signaling and increased endothelial-to-mesenchymal transition in endoglin deficient mice suggesting the importance of Eng for the proper barrier function of the endothelium [35]. Supporting that, Rossi et al. nicely demonstrated the role of Eng in adhesion of mural and endothelial cells (human aortic endothelial cells (HAECs), HUVECs, and umbilical artery smooth muscle cells) [36]. In general, they showed that adhesion of mural cells with endothelial cells depends at least partially on Eng. Once Eng expression was reduced (by siRNA of Eng) or blocked by sEng treatment, integrin-mediated adhesion of mural cells was altered. In line with that, reduced expression of Eng resulted in increased endothelial permeability, suggesting a critical role of Eng in endothelial function [36].
In another experiment, Rossi et al. used rat myoblast transfectants expressing human Eng and corresponding mock transfectants to demonstrate the role of Eng in the adhesion and transmigration of leukocytes through cell monolayer [11]. For the first time, they demonstrated the interaction of leukocyte integrin α5β and platelet αIIbβ3 with Eng expressed on endothelial cells via RGD motif, suggesting that Eng might be considered as an adhesion molecule that promotes the development of endothelial dysfunction. They also showed that reduced Eng expression resulted in a decreased inflammation-induced transendothelial migration of leukocytes, suggesting the crucial role of Eng in leukocyte transmigration, which is the hallmark of endothelial dysfunction [11]. Moreover, Ojeda-Fernandez demonstrated an essential role of Eng for the immune system function in mice macrophages. They compared the immune response of Eng myeloid lineage-specific knock out mice (Eng KO mice) with the immune response of wild-type mice. Eng KO mice developed spontaneous infections in soft tissues, impaired leukocyte transmigration, phagocytosis, and altered gene expression in macrophages, suggesting the important role of Eng in macrophage function and inflammation [37]. Altogether, these studies might suggest the potential proinflammatory role of Eng.
However, it is interesting to mention that these in vitro experiments show the effect of Eng in macrophages in the microvasculature, not in large arteries, where we usually study endothelial dysfunction and atherosclerosis. Thus, we propose the different roles of Eng in various parts of the macrovasculature and microvasculature.
Interestingly, we found that exposure to similar stimuli results in opposite outcomes in vitro and in in vivo experiments with respect to Eng. Our study focused on how hypercholesterolemia in vivo or its simulation in vitro can affect the expression and function of Eng. We explored the differences between the acute effect of 7-ketocholesterol (7 K) [simulating oxidized LDL (oxLDL) effects in atherogenesis] in HAECs and the chronic effect of hypercholesterolemia in apolipoprotein E-deficient/LDL receptor-deficient (ApoE−/−/LDLR−/−) mice [10]. It was demonstrated that 7 K induces Eng expression in HAECs via simultaneous activation of transcription factors regulating Eng expression, including Krüppel like factor 6 (KLF6) [38, 39] nuclear factor kappa B p65—hypoxia-inducible factor 1 (RELA-HIF-1) [40, 41] and liver X receptor (LXR) nuclear receptor subfamily 1 group H member 3 (NR1H3) [14, 42]. Increased expression of Eng was associated with increased expression of eNOS and phosphorylated form of eNOS (p-eNOS) protein levels, which may suggest activation of potential protective mechanisms of Eng after oxidized cholesterol treatment in HAECs. On the other hand, significantly increased protein levels of Eng after 7 K treatment were associated with significantly increased levels of cell adhesion proinflammatory molecules (E/P-selectins, VCAM-1, and ICAM-1). Consequent increased adhesion and transmigration of monocytes through 7 K pre-treated endothelial monolayer confirmed the development of endothelial dysfunction. After the silencing of Eng, induction of adhesion and transmigration were prevented [10], suggesting a crucial role of Eng in endothelial dysfunction in acute (12 h) hypercholesterolemic condition in vitro.
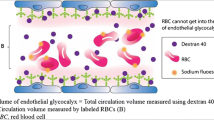
In vivo part of the study was focused on the chronic effect of hypercholesterolemia in ApoE−/−/LDLR−/− mouse model of spontaneous hypercholesterolemia, endothelial dysfunction, and atherogenesis [43]. Hypercholesterolemia (in the time frame of two months) resulted in the development of vascular and endothelial dysfunction in the aorta, with reduced Eng/eNOS/pSMAD2/3 expression in the aorta and decreased nitric oxide (NO) production, induction of inflammation, and increase of sEng levels in plasma. These results show that reduced Eng expression is related to the alteration of NO production and vascular function (endothelial dysfunction) even before the formation of atherosclerotic lesions, which suggests that proper Eng expression is crucial for the prevention of endothelial dysfunction. This is in line with our previous papers, showing that the progression of atherogenesis (increased size of atherosclerotic lesions) is accompanied by reduced Eng expression in the aorta and increased levels of sEng in blood [44,45,46]. Thus, we suggest that reduced Eng expression and increased levels of sEng are hallmarks of endothelial dysfunction development and atherogenesis, as shown in Fig. 3.
To summarize, acute exposure to oxLDL in vitro results in the development of endothelial dysfunction, which is strongly supported by increased expression Eng. In contrast, chronic exposure to cholesterol in vivo shows reduced Eng expression during the development of endothelial dysfunction and atherogenesis.
Membrane endoglin, hyperglycemia, diabetes mellitus, and arterial hypertension
Hyperglycemia is one of the metabolic syndrome-related symptoms and a hallmark of diabetes mellitus. Even though the role of Eng in hyperglycemia and diabetes is not widely investigated, some studies have attempted to establish a possible relationship between them.
Alvarez-Munoz et al. evaluated Eng expression in cultured skin fibroblasts from patients with Type 1 diabetes mellitus (DM1) with and without diabetic nephropathy, because skin fibroblast behaviors in these patients are related to diabetic nephropathy risk. They showed increased Eng mRNA expression and protein levels in fibroblasts isolated from patients with DM1 with a lower risk of nephropathy development (“slow-track”) when compared to the patients with a higher risk of nephropathy development (“fast-track”). Therefore, they suggested a potential protective role of Eng in patients with DM1 for the development of diabetic nephropathy (fibrotic changes). However, there might be some limitations of that study, related to the fact that only four subjects from each group were tested for Eng protein expression studies, and no representative Western blots were shown in the article [47].
Another in vitro study performed on HUVECs treated with high glucose (25 mmol/l) or oscillating glucose (5–25 mmol/l) resulted in increased mRNA expression of Eng, HIF-1α, and KLF6, which could be prevented by antioxidant alpha-lipoic acid [48]. However, no significant changes in Eng protein levels were found by Wang et al. when studying human blood outgrowth endothelial cells exposed to high glucose levels (25 mmol/l) [49].
Systemic arterial hypertension represents another symptom of metabolic syndrome, affecting blood vessels, and promoting endothelial dysfunction, suggesting that it may affect Eng expression and function. Nonetheless, to the best of our knowledge, no studies are focusing on the role of Eng in the systemic arterial hypertension up to date.
Membrane endoglin, liver alteration, and obesity-related to metabolic syndrome
Profibrotic changes in the liver are a part of the pathophysiology of diseases such as nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH). NAFLD is often recognized as a hepatic manifestation of metabolic syndrome-related to obesity and fat accumulation in the liver. Some NAFLD patients may develop a more severe form termed NASH, which may progress to cirrhosis and permanent liver damage [50].
Eng is known to play an important role in fibrosis development in the liver [51, 52]. Meurer et al. reported high protein expression of Eng in isolated liver hepatic stellate cells, myofibroblast-like cells, liver macrophages (Kupffer cells), and liver sinusoidal endothelial cells; however, no expression of Eng in hepatocytes neither in HepG2 cell line was found. Up-regulation of Eng expression was observed during hepatic stellate cell activation and transdifferentiation to myofibroblast-like cells in cell culture and both mice and rat experimental models of liver injury (CCl4 application or bile duct ligation) [53] [54]. However, it is of interest to mention that role of endoglin in liver fibrosis is still not well documented and lacks in-depth studies; thus, it might be too early to review these findings now to provide any meaningful insights.
Obesity (visceral) represents an essential step for the development of insulin resistance, and it plays a crucial role in the pathophysiology of type II diabetes mellitus and metabolic syndrome [55]. Kurki et al. focused on the expression profile of adipose tissue cytokines and angiogenesis-related proteins in obese and lean mice. They found significantly increased expression of Eng in adipose tissue of obese mice when compared to lean mice [56]. When exposed to calorie restriction for 50 days, the expression of Eng in obese mice did not decrease, even though they lost approximately 15.6% of their weight. On the contrary, energy restriction further increased the expression of Eng in obese mice. Surprisingly, the protein expression of Eng induced by energy restriction in lean mice was superior to the Eng expression in obese mice without energy restriction [56]. These data suggest that stress and catabolic processes during fast weight reduction can increase Eng expression as well as chronic inflammation during obesity [56].
Jilkova et al. further investigated the expression of Eng in white adipose tissue (WAT) in obese mice focusing on the relation between obesity, inflammation, and Eng expression in mice. Diet-induced low-grade inflammation in C57BL/6 J obese male mice (fed by corn oil-based high-fat diet) resulted in increased expression of Eng, suggesting promotion of the angiogenesis during the early stages of WAT inflammation. To prove these results, long-chain polyunsaturated fatty acids or rosiglitazone were added to the diet to inhibit inflammation. Significantly reduced VCAM-1 and Eng expression was found in obese mice fed with a combination of long-chain polyunsaturated fatty acids and rosiglitazone when compared to mice fed high-fat diet [57]. The authors suggested the potential involvement of Eng in WAT inflammation and remodeling of adipose tissue (probably via promoting inflammation-related angiogenesis), which can be prevented by long-chain polyunsaturated fatty acids or rosiglitazone.
Taken together, the increase of Eng expression in adipose tissue during obesity is probably related to angiogenesis, inflammation, and/or adipogenesis. Despite that, there is no direct evidence of Eng playing a crucial role in the inflammation induced by visceral obesity development.
Soluble endoglin generation and the role of matrix metalloproteinases
Matrix metalloproteinases (MMPs) are zinc-dependent endopeptidases with various and often opposing effects in the organism. They can cleave many non-matrix targets such as Eng, chemokines, cytokines, cell adhesion molecules, and other proteinases [58]. MMPs may be divided according to the structure in the four main groups. Gelatinases (MMP2, MMP9), matrilysins (MMP7, MMP26), archetypal MMPs (MMP1, MMP8, MMP13, MMP3, MMP10, MMP12, MMP19, MMP20, MMP27), and furin-activable MMPs (MMP11, MMP21, MMP28, MMP14, MMP15, MMP16, MMP24, MMP17, MMP25, MMP23) [59]. Moreover, MMPs may also be divided into soluble forms circulating in the blood or cultured medium in experiments (MMP1, MMP2, MMP3, MMP7, MMP8, MMP9, MMP10, MMP11, MMP12, MMP13, MMP26) and membrane-bound forms expressed in various tissues (MMP14, MMP15, MMP16, MMP17, MMP24, MMP25) [60].
Up to date, only two MMPs demonstrated to be able to cleave Eng to release sEng, namely MMP12 [12] and MMP14 [13]. Interestingly, both MMP12 [61] and MMP14 [62] are known to be involved in the development of vascular diseases such as atherosclerosis.
Several papers were published in recent years concerning the role of sEng as a biomarker of various cardiometabolic disorders. Besides, some studies pointed out the possible role of sEng in the pathophysiology of cardiometabolic disorders/metabolic syndrome, which will be discussed below.
Soluble endoglin as a biomarker of cardiometabolic disorders
Our last review was focused on the importance of sEng as a biomarker of various cardiometabolic disorders [63]. Briefly, sEng levels are increased in patients with hypercholesterolemia [16] and Familial hypercholesterolemia [15]. In addition, sEng levels were also increased in the experimental mouse model of atherosclerosis with hypercholesterolemia, before the formation of visible atherosclerosis in aorta, and during the formation of advanced lesions [10, 45, 46]. Moreover, a correlation of sEng levels with cholesterol levels in hypercholesterolemic mice was demonstrated [63].
Hypercholesterolemia is a crucial risk factor for the development of atherosclerosis, and oxidative modification of cholesterol (oxLDL) plays an important role in the pathogenesis. It was demonstrated that sEng levels are higher in mice with more prominent atherosclerotic lesions [45, 46]. However, no correlation between atherosclerotic plaque size and sEng levels was confirmed [63]. Interestingly, sEng showed a positive linear correlation with carotid intima-media thickness in 978 patients, suggesting that sEng might be an interesting biomarker of subclinical carotid atherosclerosis [64].
Li et al. showed an association between sEng concentration and atherosclerotic cardiovascular disease risk [64]. On the other hand, Saita et al. found an inverse association of sEng concentration and severity of coronary atherosclerosis in patients with coronary artery disease [65]. Finally, Charytan et al. did not find a significant correlation between sEng levels and atherosclerotic burden in 122 patients’ study [66]. According to these data, sEng could be considered a biomarker related to hypercholesterolemia, but there is no conclusive evidence that sEng reflects the development of atherosclerotic lesions.
Soluble endoglin, diabetes mellitus, and obesity
Hyperglycemia is considered as a risk factor for the development of cardiometabolic disorders, especially type II diabetes mellitus (DM). Plasma concentration of sEng was increased in patients with advanced DM, and the concentration of sEng positively correlates with the severity of diabetic vascular alterations such as retinopathy [67], diabetic peripheral neuropathy [68], and nephropathy [19, 69]. Ceriello et al. showed that both hypoglycemia and hyperglycemia increased sEng and MMP14 levels, and this effect could be reversed with glucagon like peptid-1 (GLP-1) in patients with type I diabetes mellitus. They suggested that an increase of sEng and MMP14 is related to oxidative stress development both in hypoglycemia and hyperglycemia [70].
Cawyer et al. focused on the effects of high glucose in the human extravillous cytotrophoblast cell line Sw.71 to evaluate the effects of high glucose on angiogenic (VEGF, PIGF) and antiangiogenic (sEng, sFLT-1) factors. They showed that high glucose levels ≥ 8.3 mmol/l significantly decreased the concentration of angiogenic and increased concentration of antiangiogenic factors, including sEng. This effect of high glucose could be reversed using a p-38 inhibitor (SB203580) or rosiglitazone [71, 72].
Lappas et al. investigated the role of sEng in gestational diabetes mellitus (GDM) and maternal obesity. They focused on the expression of sEng, Eng, and adhesion molecules in the placenta and adipose tissue. They examined healthy women, women with obesity, women with GDM, and women with a combination of obesity and GDM. Interestingly, no changes in the placenta were found, except significantly increased sEng and cell adhesion molecules in samples of adipose tissue of women with GDM [73]. However, Vieira et al. found the opposite trend of sEng concentration changes in obese women. They found a significantly decreased blood plasma concentration of sEng in the group of 834 obese women compared to the group of 3106 non-obese women [74].
These data demonstrate that sEng levels reflect hyperglycemia, and we might propose that sEng could be considered an important biomarker of developing diabetic changes; however, its relation to obesity (especially visceral obesity) must be further investigated.
Soluble endoglin as a biomarker of arterial hypertension
As mentioned above, sEng levels are increased in hypercholesterolemia and hyperglycemia, both risk factors for the development of systemic arterial hypertension. The only paper describing the sEng levels and systemic arterial hypertension showed that sEng levels correlated with systolic blood pressure, left-ventricular hypertrophy, and endothelial dysfunction [67]. In addition, several papers described the relation between sEng and Pulmonary arterial hypertension (PAH). Indeed, PAH is not a subtype of arterial hypertension, and PAH etiopathogenesis is very different from systemic arterial hypertension. Increased sEng concentration in the blood plasma of patients correlated with the New York Heart Association (NYHA) classification of PAH. High sEng concentrations were significantly increased in patients with idiopathic or hereditary PAH, PAH associated with connective tissue disease, drug, or toxin-related PAH, but not with PAH related to congenital heart disease [17]. Also, Coral-Alvarado et al. found significantly increased sEng levels in the plasma of patients with systemic sclerosis combined with PAH compared to the healthy controls [75]. Moreover, Bakouboula et al. tested peripheral venous blood from healthy donors, blood from the jugular vein, and occluded pulmonary artery blood from patients with PAH. They found a significantly increased concentration of sEng in circulating procoagulant microparticles from patients with PAH compared to healthy donors. The concentration of sEng in occluded artery blood was even higher than the concentration of sEng in microparticles from the jugular vein of patients with PAH, suggesting the production of sEng in impaired pulmonary endothelial cells [76]. These data suggest that sEng might be associated with the changes of blood pressure; however, the precise mechanism remains to be elucidated.
Soluble endoglin as an inducer of cardiometabolic disorders
Venkatesha et al. showed that placenta-derived sEng from pregnant preeclamptic women is able to inhibit capillary tube formation in vitro and increase vascular permeability and induce arterial hypertension in vivo. sEng was able to inhibit TGFβ1 binding and signaling in endothelial cells, which resulted in decreased activation of eNOS and impaired vasodilatation in isolated rat renal microvessels and mesenteric vessels. Authors concluded that sEng plays an essential role in the pathogenesis of arterial hypertension, proteinuria, glomerular endotheliosis, and HELLP syndrome [77]. Walshe et al. demonstrated that sEng (using adenovirus expression of sEng) increased the expression of P-selectin, promoted leukocyte rolling on endothelium, and elevated levels of soluble E-selectin, soluble VCAM-1, and impaired endothelial dependence vasodilation [78]. Besides, in an experimental model of preeclampsia, transgenic mice overexpressing human sEng (sEng levels higher than 2000 ng/ml) had higher systolic blood pressure when compared to wild-type littermates [14]. Furthermore, we showed that sEng treatment induced inflammation (represented by increased NF-κB and IL6) in HUVECs, suggesting that sEng has a proinflammatory potential, as well [79].
Based on these studies, we might propose that sEng promotes the development of endothelial dysfunction, which might contribute to an increase of systemic blood pressure, suggesting that high levels of sEng promote metabolic syndrome (Fig. 3). However, how exactly sEng contributes to the development of metabolic syndrome is still unknown.
Some studies are showing that sEng might have beneficial effects on fibrosis development. Kapur et al. showed that sEng was able to prevent cardiac fibrosis by decreasing collagen synthesis in human cardiac fibroblasts. They demonstrated in vivo the ability of sEng injection to decrease cardiac fibrosis via pSmad 2/3 inhibition in mice after thoracic aortic constriction [80]. However, it is of interest to mention that fibrotic process with respect to ALK1/Smad 1/5 and ALK5/Smad 2/3 pathways is controversial. Most studies suggest the protective antifibrotic role of ALK1/Smad 1/5 pathway, which counteracts the profibrotic ALK5/Smad 2/3 pathway [81].
On the other hand, Pannu et al. demonstrated the profibrotic response of systemic sclerosis fibroblasts on the persistent activation of SMAD1 and Erk-1/2 pathway [82]. Also, in hepatic stellate cells, renal fibroblasts, and mesangial cells, increased activation of Smad 1/5 resulted in increased production of extracellular matrix proteins and progression of fibrosis [83]. Indeed, this topic was nicely revised by Múñoz-Félix et al. [81] and Dituri et al. [84] recently.
In addition, it is of interest to mention that dimeric sEng has been considered to be an inhibitory ligand trap for BMP9. Moreover, Breitkopf-Heinlein et al. showed profibrogenic actions of BMP9, suggesting that BMP9 promotes liver fibrogenesis under damage, whereas the absence or inhibition of BMP9 promotes wound healing and liver repairment. This might suggest sEng involvement in liver fibrosis and/or regeneration [85]. On the contrary, Lawera et al. demonstrated that majority of sEng in blood plasma is in monomeric form, and this one does not act as an inhibitory ligand trap for BMP9 signaling [86]. Thus, the interaction of sEng and BMP9 with respect to fibrosis remains to be elucidated.
Reduced inflammatory response after proinflammatory stimuli (LPS, Carrageenan) and ischemia in vivo was demonstrated in transgenic mice model expressing human sEng (high sEng mice) by Ruiz-Remolina et al. In addition, they showed that morphological changes after ischemia–reperfusion of lung and kidney were decreased, as well as leukocyte recruitment in high sEng mice [87]. Moreover, it was shown that decreased leukocyte recruitment in high sEng mice might suggest binding of leukocytes integrin α5β1 with sEng RGD motif. This should result in limited availability of leukocyte integrins for the binding of Eng, thus resulting in decreased transmigration of these cells through endothelium in high sEng mice [11]. Thus, these data show the potential anti-inflammatory effects of sEng. However, it is of interest to mention that the above-mentioned studies were performed in various experimental conditions, which most likely contribute to these contradictory results with respect to sEng.
Our experimental group focused on the role of sEng effects in the aorta, a blood vessel prone to the development of endothelial dysfunction and atherosclerosis, which is part of metabolic syndrome.
It was demonstrated that high levels of sEng did not affect aortic endothelial function either at the protein or at the functional level, suggesting possibly no contribution to endothelial dysfunction when sEng is operating as a single factor [88]. In general, it is accepted that endothelial dysfunction and atherosclerosis “requires” hypercholesterolemia. Thus, we combined high sEng levels with high-fat diet (HFD) administration for 3 months. The results showed that this combination induced proinflammatory (increased expression of P-selectin, ICAM-1, phosphorylated NF-κB and COX-2) and oxidative stress (increased expression of HO-1, NOX-1, and NOX-2) phenotype in aortic endothelium (without any visible atherosclerosis). Surprisingly, endothelium-dependent vasodilatation induced by acetylcholine was preserved better in mice with high sEng levels, suggesting activation of a compensatory mechanism in endothelium [89]. Once we increased the exposure to sEng and HFD to 6 months, we showed significant aggravation of endothelial dysfunction characterized by reduced Eng, p-eNOS/eNOS, pSMAD2/3/SMAD2/3 signaling pathway only in mice with high sEng levels.
Thus, we might suggest that sEng, especially combined with other risk factors of metabolic syndrome, might be considered as a risk factor for the development of endothelial dysfunction/inflammation and possibly atherosclerosis (Fig. 3).
Recently, Gallardo-Vara et al. demonstrated that sEng induces the expression of BMP4 in endothelial cells in various organs, suggesting BMP4 is a downstream mediator of sEng, responsible for the development of systemic arterial hypertension in these mice [90] (Fig. 3).
Hypercholesterolemia-induced endothelial dysfunction and atherogenesis reduce Eng expression, which is related to the development of endothelial dysfunction. Risk factors that determine the development of metabolic syndrome are associated with increased levels of sEng levels, which might be considered as biomarkers of metabolic syndrome-related pathological disorders. In addition, sEng was shown to aggravate existing endothelial dysfunction and induce the development of systemic arterial hypertension. Adapted from [10, 14, 15, 21, 30, 31, 63, 67, 77, 90, 91]
During this review, we noticed that sEng levels are increased in metabolic syndrome, mostly related to hypercholesterolemia. As the liver plays an important role in cholesterol metabolism in vivo, it became interesting to explore the potential impact of high sEng levels on cholesterol and bile acid metabolism in the liver [92].
An experiment in healthy mice showed that the presence of high levels of sEng resulted in increased cholesterol content in the liver due to increased hepatic import of LDL and total cholesterol in these mice. Despite that, it is important to mention that this modulation occurred within physiological levels, since all mice were normocholesterolemic. The presence of sEng also resulted in increased conversion of cholesterol into bile acids via upregulation of Cyp7a1, increased Mdr1 expression, and additionally increased biliary elimination of bile acids coupled with choleretic activity [92].
Taken together, we may speculate that the potential impact of sEng on bile acid metabolism should be considered in patients with metabolic syndrome when they are treated with pharmaceuticals that require hepatic metabolism.
Membrane and soluble endoglin changes after the treatment
So far, we focused on the possible role of Eng and sEng in the pathological conditions related to metabolic syndrome. We showed that both Eng and sEng are involved in the process, so now we would like to focus only on studies mentioning drugs that are used for the treatment of metabolic syndrome-related pathologies such as hypercholesterolemia, diabetes mellitus, and arterial hypertension with respect to Eng and sEng. The summary of all papers is demonstrated in Table 1.
Conclusion
In conclusion, we propose that reduced Eng expression is a hallmark of endothelial dysfunction development in chronic disorders associated with metabolic syndrome. On the other hand, Eng also plays an essential role in leukocyte transmigration and acute inflammation, suggesting that Eng is crucial for the regulation of endothelial function during the acute phase of vascular defense reaction to harmful conditions. sEng is a circulating biomarker of metabolic syndrome-related symptoms and pathologies, including hypercholesterolemia, hyperglycemia, diabetes mellitus, arterial hypertension, and liver damage. In addition, sEng is able to participate in the aggravation of endothelial dysfunction and promote the development of arterial hypertension, suggesting that high levels of sEng promote metabolic syndrome symptoms and its complications. Therefore, we suggest that the treatment of metabolic syndrome should take into account the importance of Eng in the endothelial function and levels of sEng as a biomarker and risk factor of related pathologies.
References
Oujo B, Perez-Barriocanal F, Bernabeu C, Lopez-Novoa JM (2013) Membrane and soluble forms of endoglin in preeclampsia. Curr Mol Med 13(8):1345–1357
Bot PT, Hoefer IE, Sluijter JP, van Vliet P, Smits AM, Lebrin F, Moll F, de Vries JP, Doevendans P, Piek JJ, Pasterkamp G, Goumans MJ (2009) Increased expression of the transforming growth factor-beta signaling pathway, endoglin, and early growth response-1 in stable plaques. Stroke 40(2):439–447. https://doi.org/10.1161/STROKEAHA.108.522284
St-Jacques S, Forte M, Lye SJ, Letarte M (1994) Localization of endoglin, a transforming growth factor-beta binding protein, and of CD44 and integrins in placenta during the first trimester of pregnancy. Biol Reprod 51(3):405–413
Meurer S, Wimmer AE, Leur EV, Weiskirchen R (2019) Endoglin trafficking/exosomal targeting in liver cells depends on n-glycosylation. Cells. https://doi.org/10.3390/cells8090997
Lastres P, Bellon T, Cabanas C, Sanchez-Madrid F, Acevedo A, Gougos A, Letarte M, Bernabeu C (1992) Regulated expression on human macrophages of endoglin, an Arg-Gly-Asp-containing surface antigen. Eur J Immunol 22(2):393–397
McAllister KA, Grogg KM, Johnson DW, Gallione CJ, Baldwin MA, Jackson CE, Helmbold EA, Markel DS, McKinnon WC, Murrell J et al (1994) Endoglin, a TGF-beta binding protein of endothelial cells, is the gene for hereditary haemorrhagic telangiectasia type 1. Nat Genet 8(4):345–351. https://doi.org/10.1038/ng1294-345
Kapur NK, Morine KJ, Letarte M (2013) Endoglin: a critical mediator of cardiovascular health. Vasc Health Risk Manag 9:195–206. https://doi.org/10.2147/VHRM.S29144
Qu R, Silver MM, Letarte M (1998) Distribution of endoglin in early human development reveals high levels on endocardial cushion tissue mesenchyme during valve formation. Cell Tissue Res 292(2):333–343
Alsamman M, Sterzer V, Meurer SK, Sahin H, Schaeper U, Kuscuoglu D, Strnad P, Weiskirchen R, Trautwein C, Scholten D (2018) Endoglin in human liver disease and murine models of liver fibrosis-A protective factor against liver fibrosis. Liver Int 38(5):858–867. https://doi.org/10.1111/liv.13595
Vicen M, Vitverova B, Havelek R, Blazickova K, Machacek M, Rathouska J, Najmanova I, Dolezelova E, Prasnicka A, Sternak M, Bernabeu C, Nachtigal P (2019) Regulation and role of endoglin in cholesterol-induced endothelial and vascular dysfunction in vivo and in vitro. FASEB J 33(5):6099–6114. https://doi.org/10.1096/fj.201802245R
Rossi E, Sanz-Rodriguez F, Eleno N, Duwell A, Blanco FJ, Langa C, Botella LM, Cabanas C, Lopez-Novoa JM, Bernabeu C (2013) Endothelial endoglin is involved in inflammation: role in leukocyte adhesion and transmigration. Blood 121(2):403–415. https://doi.org/10.1182/blood-2012-06-435347
Aristorena M, Gallardo-Vara E, Vicen M, de Las C-E, Ojeda-Fernandez L, Nieto C, Blanco FJ, Valbuena-Diez AC, Botella LM, Nachtigal P, Corbi AL, Colmenares M, Bernabeu C (2019) MMP-12, Secreted by pro-inflammatory macrophages, targets endoglin in human macrophages and endothelial cells. Int J Mol Sci. https://doi.org/10.3390/ijms20123107
Hawinkels LJ, Kuiper P, Wiercinska E, Verspaget HW, Liu Z, Pardali E, Sier CF, ten Dijke P (2010) Matrix metalloproteinase-14 (MT1-MMP)-mediated endoglin shedding inhibits tumor angiogenesis. Cancer Res 70(10):4141–4150. https://doi.org/10.1158/0008-5472.CAN-09-4466
Valbuena-Diez AC, Blanco FJ, Oujo B, Langa C, Gonzalez-Nunez M, Llano E, Pendas AM, Diaz M, Castrillo A, Lopez-Novoa JM, Bernabeu C (2012) Oxysterol-induced soluble endoglin release and its involvement in hypertension. Circulation 126(22):2612–2624. https://doi.org/10.1161/CIRCULATIONAHA.112.101261
Blaha M, Cermanova M, Blaha V, Jarolim P, Andrys C, Blazek M, Maly J, Smolej L, Zajic J, Masin V, Zimova R, Rehacek V (2008) Elevated serum soluble endoglin (sCD105) decreased during extracorporeal elimination therapy for familial hypercholesterolemia. Atherosclerosis 197(1):264–270. https://doi.org/10.1016/j.atherosclerosis.2007.04.022
Blann AD, Wang JM, Wilson PB, Kumar S (1996) Serum levels of the TGF-beta receptor are increased in atherosclerosis. Atherosclerosis 120(1–2):221–226
Malhotra R, Paskin-Flerlage S, Zamanian RT, Zimmerman P, Schmidt JW, Deng DY, Southwood M, Spencer R, Lai CS, Parker W, Channick RN, Morrell NW, Elliott CG, Yu PB (2013) Circulating angiogenic modulatory factors predict survival and functional class in pulmonary arterial hypertension. Pulm Circ 3(2):369–380. https://doi.org/10.4103/2045-8932.110445
Leanos-Miranda A, Navarro-Romero CS, Sillas-Pardo LJ, Ramirez-Valenzuela KL, Isordia-Salas I, Jimenez-Trejo LM (2019) Soluble endoglin as a marker for preeclampsia, its severity, and the occurrence of adverse outcomes. Hypertension 74(4):991–997. https://doi.org/10.1161/HYPERTENSIONAHA.119.13348
Doghish AS, Bassyouni AA, Mahfouz MH, Abd El-Aziz HG, Zakaria RY (2019) Plasma endoglin in Type2 diabetic patients with nephropathy. Diabetes Metab Syndr 13(1):764–768. https://doi.org/10.1016/j.dsx.2018.11.058
Rathouska J, Nemeckova I, Zemankova L, Strasky Z, Jezkova K, Varejckova M, Nachtigal P (2015) Cell adhesion molecules and eNOS expression in aorta of normocholesterolemic mice with different predispositions to atherosclerosis. Heart Vessels 30(2):241–248. https://doi.org/10.1007/s00380-014-0493-8
Nachtigal P, Zemankova Vecerova L, Rathouska J, Strasky Z (2012) The role of endoglin in atherosclerosis. Atherosclerosis 224(1):4–11. https://doi.org/10.1016/j.atherosclerosis.2012.03.001
Schoonderwoerd MJA, Goumans MTH, Hawinkels L (2020) Endoglin: beyond the endothelium. Biomolecules. https://doi.org/10.3390/biom10020289
Xu G, Barrios-Rodiles M, Jerkic M, Turinsky AL, Nadon R, Vera S, Voulgaraki D, Wrana JL, Toporsian M, Letarte M (2014) Novel protein interactions with endoglin and activin receptor-like kinase 1: potential role in vascular networks. Mol Cell Proteom: MCP 13(2):489–502. https://doi.org/10.1074/mcp.M113.033464
Gougos A, Letarte M (1990) Primary structure of endoglin, an RGD-containing glycoprotein of human endothelial cells. J Biol Chem 265(15):8361–8364
Llorca O, Trujillo A, Blanco FJ, Bernabeu C (2007) Structural model of human endoglin, a transmembrane receptor responsible for hereditary hemorrhagic telangiectasia. J Mol Biol 365(3):694–705
Velasco S, Alvarez-Munoz P, Pericacho M, Dijke PT, Bernabeu C, Lopez-Novoa JM, Rodriguez-Barbero A (2008) L- and S-endoglin differentially modulate TGFbeta1 signaling mediated by ALK1 and ALK5 in L6E9 myoblasts. J Cell Sci 121(Pt 6):913–919. https://doi.org/10.1242/jcs.023283
Blanco FJ, Grande MT, Langa C, Oujo B, Velasco S, Rodriguez-Barbero A, Perez-Gomez E, Quintanilla M, Lopez-Novoa JM, Bernabeu C (2008) S-endoglin expression is induced in senescent endothelial cells and contributes to vascular pathology. Circ Res 103(12):1383–1392. https://doi.org/10.1161/CIRCRESAHA.108.176552
Conley BA, Smith JD, Guerrero-Esteo M, Bernabeu C, Vary CP (2000) Endoglin, a TGF-beta receptor-associated protein, is expressed by smooth muscle cells in human atherosclerotic plaques. Atherosclerosis 153(2):323–335 (S0021915000004226 [pii])
Davignon J, Ganz P (2004) Role of endothelial dysfunction in atherosclerosis. Circulation 109(23 Suppl 1):III27-32
Jerkic M, Rivas-Elena JV, Prieto M, Carron R, Sanz-Rodriguez F, Perez-Barriocanal F, Rodriguez-Barbero A, Bernabeu C, Lopez-Novoa JM (2004) Endoglin regulates nitric oxide-dependent vasodilatation. FASEB J 18(3):609–611. https://doi.org/10.1096/fj.03-0197fje03-0197fje[pii]
Toporsian M, Gros R, Kabir MG, Vera S, Govindaraju K, Eidelman DH, Husain M, Letarte M (2005) A role for endoglin in coupling eNOS activity and regulating vascular tone revealed in hereditary hemorrhagic telangiectasia. Circ Res 96(6):684–692. https://doi.org/10.1161/01.RES.0000159936.38601.22
Santibanez JF, Letamendia A, Perez-Barriocanal F, Silvestri C, Saura M, Vary CP, Lopez-Novoa JM, Attisano L, Bernabeu C (2007) Endoglin increases eNOS expression by modulating Smad2 protein levels and Smad2-dependent TGF-beta signaling. J Cell Physiol 210(2):456–468
Zemankova L, Varejckova M, Dolezalova E, Fikrova P, Jezkova K, Rathouska J, Cerveny L, Botella LM, Bernabeu C, Nemeckova I, Nachtigal P (2015) Atorvastatin-induced endothelial nitric oxide synthase expression in endothelial cells is mediated by endoglin. J Physiol Pharmacol 66(3):403–413
Jerkic M, Letarte M (2015) Increased endothelial cell permeability in endoglin-deficient cells. FASEB J 29(9):3678–3688. https://doi.org/10.1096/fj.14-269258
Anderberg C, Cunha SI, Zhai Z, Cortez E, Pardali E, Johnson JR, Franco M, Paez-Ribes M, Cordiner R, Fuxe J, Johansson BR, Goumans MJ, Casanovas O, ten Dijke P, Arthur HM, Pietras K (2013) Deficiency for endoglin in tumor vasculature weakens the endothelial barrier to metastatic dissemination. J Exp Med 210(3):563–579. https://doi.org/10.1084/jem.20120662
Rossini R, Capodanno D, Ferrero P, Gargiulo G, Capranzano P (2016) Management issues of chronic therapy with non-vitamin K oral anticoagulants or antiplatelet agents: different or alike? Int J Cardiol 221:695–696. https://doi.org/10.1016/j.ijcard.2016.07.008
Ojeda-Fernandez L, Recio-Poveda L, Aristorena M, Lastres P, Blanco FJ, Sanz-Rodriguez F, Gallardo-Vara E, de las Casas-Engel M, Corbi A, Arthur HM, Bernabeu C, Botella LM (2016) Mice lacking endoglin in macrophages show an impaired immune response. PLoS Genet 12(3):e1005935. https://doi.org/10.1371/journal.pgen.1005935
Botella LM, Sanchez-Elsner T, Sanz-Rodriguez F, Kojima S, Shimada J, Guerrero-Esteo M, Cooreman MP, Ratziu V, Langa C, Vary CP, Ramirez JR, Friedman S, Bernabeu C (2002) Transcriptional activation of endoglin and transforming growth factor-beta signaling components by cooperative interaction between Sp1 and KLF6: their potential role in the response to vascular injury. Blood 100(12):4001–4010. https://doi.org/10.1182/blood.V100.12.4001100/12/4001[pii]
Gallardo-Vara E, Blanco FJ, Roque M, Friedman SL, Suzuki T, Botella LM, Bernabeu C (2016) Transcription factor KLF6 upregulates expression of metalloprotease MMP14 and subsequent release of soluble endoglin during vascular injury. Angiogenesis 19(2):155–171. https://doi.org/10.1007/s10456-016-9495-8
Sanchez-Elsner T, Botella LM, Velasco B, Langa C, Bernabeu C (2002) Endoglin expression is regulated by transcriptional cooperation between the hypoxia and transforming growth factor-beta pathways. J Biol Chem 277(46):43799–43808. https://doi.org/10.1074/jbc.M207160200M207160200[pii]
van Uden P, Kenneth NS, Rocha S (2008) Regulation of hypoxia-inducible factor-1alpha by NF-kappaB. Biochem J 412(3):477–484. https://doi.org/10.1042/BJ20080476
Henry-Berger J, Mouzat K, Baron S, Bernabeu C, Marceau G, Saru JP, Sapin V, Lobaccaro JM, Caira F (2008) Endoglin (CD105) expression is regulated by the liver X receptor alpha (NR1H3) in human trophoblast cell line JAR. Biol Reprod 78(6):968–975. https://doi.org/10.1095/biolreprod.107.066498
Csanyi G, Gajda M, Franczyk-Zarow M, Kostogrys R, Gwozdz P, Mateuszuk L, Sternak M, Wojcik L, Zalewska T, Walski M, Chlopicki S (2012) Functional alterations in endothelial NO, PGI(2) and EDHF pathways in aorta in ApoE/LDLR-/- mice. Prostaglandins Other Lipid Mediat 98(3–4):107–115. https://doi.org/10.1016/j.prostaglandins.2012.02.002
Vecerova L, Strasky Z, Rathouska J, Slanarova M, Brcakova E, Micuda S, Nachtigal P (2012) Activation of TGF-beta receptors and Smad proteins by atorvastatin is related to reduced atherogenesis in ApoE/LDLR double knockout mice. J Atheroscler Thromb 19(2):115–126
Strasky Z, Vecerova L, Rathouska J, Slanarova M, Brcakova E, Kudlackova Z, Andrys C, Micuda S, Nachtigal P (2011) Cholesterol effects on endoglin and its downstream pathways in ApoE/LDLR double knockout mice. Circ J 75(7):1747–1755
Rathouska J, Vecerova L, Strasky Z, Slanarova M, Brcakova E, Mullerova Z, Andrys C, Micuda S, Nachtigal P (2011) Endoglin as a possible marker of atorvastatin treatment benefit in atherosclerosis. Pharmacol Res 64(1):53–59. https://doi.org/10.1016/j.phrs.2011.03.008
Alvarez-Munoz P, Mauer M, Kim Y, Rich SS, Miller ME, Russell GB, Lopez-Novoa JM, Caramori ML (2010) Cellular basis of diabetic nephropathy: V. Endoglin expression levels and diabetic nephropathy risk in patients with type 1 diabetes. J Diabetes Complicat 24(4):242–249. https://doi.org/10.1016/j.jdiacomp.2009.03.004
La Sala L, Pujadas G, De Nigris V, Canivell S, Novials A, Genovese S, Ceriello A (2015) Oscillating glucose and constant high glucose induce endoglin expression in endothelial cells: the role of oxidative stress. Acta Diabetol 52(3):505–512. https://doi.org/10.1007/s00592-014-0670-3
Wang S, Hirschberg R (2009) Diabetes-relevant regulation of cultured blood outgrowth endothelial cells. Microvasc Res 78(2):174–179. https://doi.org/10.1016/j.mvr.2009.06.002
Rinella ME (2015) Nonalcoholic fatty liver disease: a systematic review. JAMA 313(22):2263–2273. https://doi.org/10.1001/jama.2015.5370
Finnson KW, Philip A (2012) Endoglin in liver fibrosis. J Cell Commun Signal 6(1):1–4. https://doi.org/10.1007/s12079-011-0154-y
Garcia-Pozo L, Miquilena-Colina ME, Lozano-Rodriguez T, Garcia-Monzon C (2008) Endoglin: structure, biological functions, and role in fibrogenesis. Rev Esp Enferm Dig 100(6):355–360. https://doi.org/10.4321/s1130-01082008000600008
Meurer SK, Tihaa L, Borkham-Kamphorst E, Weiskirchen R (2011) Expression and functional analysis of endoglin in isolated liver cells and its involvement in fibrogenic Smad signalling. Cell Signal 23(4):683–699. https://doi.org/10.1016/j.cellsig.2010.12.002
Meurer SK, Alsamman M, Scholten D, Weiskirchen R (2014) Endoglin in liver fibrogenesis: bridging basic science and clinical practice. World J Biol Chem 5(2):180–203. https://doi.org/10.4331/wjbc.v5.i2.180
Chan DC, Barrett HP, Watts GF (2004) Dyslipidemia in visceral obesity: mechanisms, implications, and therapy. Am J Cardiovasc Drugs 4(4):227–246
Kurki E, Shi J, Martonen E, Finckenberg P, Mervaala E (2012) Distinct effects of calorie restriction on adipose tissue cytokine and angiogenesis profiles in obese and lean mice. Nutr Metab (Lond) 9(1):64. https://doi.org/10.1186/1743-7075-9-64
Jilkova ZM, Hensler M, Medrikova D, Janovska P, Horakova O, Rossmeisl M, Flachs P, Sell H, Eckel J, Kopecky J (2014) Adipose tissue-related proteins locally associated with resolution of inflammation in obese mice. Int J Obes (Lond) 38(2):216–223. https://doi.org/10.1038/ijo.2013.108
Vanlaere I, Libert C (2009) Matrix metalloproteinases as drug targets in infections caused by gram-negative bacteria and in septic shock. Clin Microbiol Rev 22(2):224–239. https://doi.org/10.1128/CMR.00047-08 (Table of contents)
Vandenbroucke RE, Libert C (2014) Is there new hope for therapeutic matrix metalloproteinase inhibition? Nat Rev Drug Discov 13(12):904–927. https://doi.org/10.1038/nrd4390
Klein T, Bischoff R (2011) Physiology and pathophysiology of matrix metalloproteases. Amino Acids 41(2):271–290. https://doi.org/10.1007/s00726-010-0689-x
Feinberg MW, Jain MK, Werner F, Sibinga NE, Wiesel P, Wang H, Topper JN, Perrella MA, Lee ME (2000) Transforming growth factor-beta 1 inhibits cytokine-mediated induction of human metalloelastase in macrophages. J Biol Chem 275(33):25766–25773. https://doi.org/10.1074/jbc.M002664200
Rajavashisth TB, Xu XP, Jovinge S, Meisel S, Xu XO, Chai NN, Fishbein MC, Kaul S, Cercek B, Sharifi B, Shah PK (1999) Membrane type 1 matrix metalloproteinase expression in human atherosclerotic plaques: evidence for activation by proinflammatory mediators. Circulation 99(24):3103–3109. https://doi.org/10.1161/01.cir.99.24.3103
Rathouska J, Jezkova K, Nemeckova I, Nachtigal P (2015) Soluble endoglin, hypercholesterolemia and endothelial dysfunction. Atherosclerosis 243(2):383–388. https://doi.org/10.1016/j.atherosclerosis.2015.10.003
Li Q, Lin F, Ke D, Cheng Q, Gui Y, Zhou Y, Wu Y, Wang Y, Zhu P (2020) Combination of endoglin and ASCVD risk assessment improves carotid subclinical atherosclerosis recognition. J Atheroscler Thromb 27(4):331–341. https://doi.org/10.5551/jat.50898
Saita E, Miura K, Suzuki-Sugihara N, Miyata K, Ikemura N, Ohmori R, Ikegami Y, Kishimoto Y, Kondo K, Momiyama Y (2017) Plasma soluble endoglin levels are inversely associated with the severity of coronary atherosclerosis-brief report. Arterioscler Thromb Vasc Biol 37(1):49–52. https://doi.org/10.1161/ATVBAHA.116.308494
Charytan DM, Cinelli A, Zeisberg EM (2015) Association of circulating angiogenesis inhibitors and asymmetric dimethyl arginine with coronary plaque burden. Fibrogenesis Tissue Repair 8:13. https://doi.org/10.1186/s13069-015-0029-6
Blazquez-Medela AM, Garcia-Ortiz L, Gomez-Marcos MA, Recio-Rodriguez JI, Sanchez-Rodriguez A, Lopez-Novoa JM, Martinez-Salgado C (2010) Increased plasma soluble endoglin levels as an indicator of cardiovascular alterations in hypertensive and diabetic patients. BMC Med 8:86. https://doi.org/10.1186/1741-7015-8-86
Bilir B, Ekiz Bilir B, Yilmaz I, Soysal Atile N, Yildirim T, Kara SP, Gumustas SA, Orhan AE, Aydin M (2016) Association of apelin, endoglin and endocan with diabetic peripheral neuropathy in type 2 diabetic patients. Eur Rev Med Pharmacol Sci 20(5):892–898
Ekiz-Bilir B, Bilir B, Aydin M, Soysal-Atile N (2019) Evaluation of endocan and endoglin levels in chronic kidney disease due to diabetes mellitus. Arch Med Sci 15(1):86–91. https://doi.org/10.5114/aoms.2018.79488
Ceriello A, La Sala L, De Nigris V, Pujadas G, Testa R, Uccellatore A, Genovese S (2015) GLP-1 reduces metalloproteinase-14 and soluble endoglin induced by both hyperglycemia and hypoglycemia in type 1 diabetes. Endocrine 50(2):508–511. https://doi.org/10.1007/s12020-015-0565-2
Cawyer C, Afroze SH, Drever N, Allen S, Jones R, Zawieja DC, Kuehl T, Uddin MN (2016) Attenuation of hyperglycemia-induced apoptotic signaling and anti-angiogenic milieu in cultured cytotrophoblast cells. Hypertens Pregnancy 35(2):159–169. https://doi.org/10.3109/10641955.2015.1122035
Cawyer CR, Horvat D, Leonard D, Allen SR, Jones RO, Zawieja DC, Kuehl TJ, Uddin MN (2014) Hyperglycemia impairs cytotrophoblast function via stress signaling. Am J Obstet Gynecol 211(5):e541-548. https://doi.org/10.1016/j.ajog.2014.04.033
Lappas M (2014) Markers of endothelial cell dysfunction are increased in human omental adipose tissue from women with pre-existing maternal obesity and gestational diabetes. Metab Clin Exp 63(6):860–873. https://doi.org/10.1016/j.metabol.2014.03.007
Vieira MC, Poston L, Fyfe E, Gillett A, Kenny LC, Roberts CT, Baker PN, Myers JE, Walker JJ, McCowan LM, North RA, Pasupathy D, Consortium S (2017) Clinical and biochemical factors associated with preeclampsia in women with obesity. Obesity (Silver Spring) 25(2):460–467. https://doi.org/10.1002/oby.21715
Coral-Alvarado PX, Garces MF, Caminos JE, Iglesias-Gamarra A, Restrepo JF, Quintana G (2010) Serum endoglin levels in patients suffering from systemic sclerosis and elevated systolic pulmonary arterial pressure. Int J Rheumatol. https://doi.org/10.1155/2010/969383
Bakouboula B, Morel O, Faure A, Zobairi F, Jesel L, Trinh A, Zupan M, Canuet M, Grunebaum L, Brunette A, Desprez D, Chabot F, Weitzenblum E, Freyssinet JM, Chaouat A, Toti F (2008) Procoagulant membrane microparticles correlate with the severity of pulmonary arterial hypertension. Am J Respir Crit Care Med 177(5):536–543. https://doi.org/10.1164/rccm.200706-840OC
Venkatesha S, Toporsian M, Lam C, Hanai J, Mammoto T, Kim YM, Bdolah Y, Lim KH, Yuan HT, Libermann TA, Stillman IE, Roberts D, D’Amore PA, Epstein FH, Sellke FW, Romero R, Sukhatme VP, Letarte M, Karumanchi SA (2006) Soluble endoglin contributes to the pathogenesis of preeclampsia. Nat Med 12(6):642–649. https://doi.org/10.1038/nm1429
Walshe TE, Dole VS, Maharaj AS, Patten IS, Wagner DD, D’Amore PA (2009) Inhibition of VEGF or TGF-{beta} signaling activates endothelium and increases leukocyte rolling. Arterioscler Thromb Vasc Biol 29(8):1185–1192. https://doi.org/10.1161/ATVBAHA.109.186742
Varejckova M, Gallardo-Vara E, Vicen M, Vitverova B, Fikrova P, Dolezelova E, Rathouska J, Prasnicka A, Blazickova K, Micuda S, Bernabeu C, Nemeckova I, Nachtigal P (2017) Soluble endoglin modulates the pro-inflammatory mediators NF-kappaB and IL-6 in cultured human endothelial cells. Life Sci 175:52–60. https://doi.org/10.1016/j.lfs.2017.03.014
Kapur NK, Wilson S, Yunis AA, Qiao X, Mackey E, Paruchuri V, Baker C, Aronovitz MJ, Karumanchi SA, Letarte M, Kass DA, Mendelsohn ME, Karas RH (2012) Reduced endoglin activity limits cardiac fibrosis and improves survival in heart failure. Circulation 125(22):2728–2738. https://doi.org/10.1161/CIRCULATIONAHA.111.080002
Munoz-Felix JM, Gonzalez-Nunez M, Lopez-Novoa JM (2013) ALK1-Smad1/5 signaling pathway in fibrosis development: friend or foe? Cytokine Growth Factor Rev 24(6):523–537. https://doi.org/10.1016/j.cytogfr.2013.08.002
Pannu J, Nakerakanti S, Smith E, ten Dijke P, Trojanowska M (2007) Transforming growth factor-beta receptor type I-dependent fibrogenic gene program is mediated via activation of Smad1 and ERK1/2 pathways. J Biol Chem 282(14):10405–10413. https://doi.org/10.1074/jbc.M611742200
Wiercinska E, Wickert L, Denecke B, Said HM, Hamzavi J, Gressner AM, Thorikay M, ten Dijke P, Mertens PR, Breitkopf K, Dooley S (2006) Id1 is a critical mediator in TGF-beta-induced transdifferentiation of rat hepatic stellate cells. Hepatology 43(5):1032–1041. https://doi.org/10.1002/hep.21135
Dituri F, Cossu C, Mancarella S, Giannelli G (2019) The interactivity between TGFbeta and BMP signaling in organogenesis, fibrosis, and cancer. Cells. https://doi.org/10.3390/cells8101130
Breitkopf-Heinlein K, Meyer C, Konig C, Gaitantzi H, Addante A, Thomas M, Wiercinska E, Cai C, Li Q, Wan F, Hellerbrand C, Valous NA, Hahnel M, Ehlting C, Bode JG, Muller-Bohl S, Klingmuller U, Altenoder J, Ilkavets I, Goumans MJ, Hawinkels LJ, Lee SJ, Wieland M, Mogler C, Ebert MP, Herrera B, Augustin H, Sanchez A, Dooley S, Ten Dijke P (2017) BMP-9 interferes with liver regeneration and promotes liver fibrosis. Gut 66(5):939–954. https://doi.org/10.1136/gutjnl-2016-313314
Lawera A, Tong Z, Thorikay M, Redgrave RE, Cai J, van Dinther M, Morrell NW, Afink GB, Charnock-Jones DS, Arthur HM, Ten Dijke P, Li W (2019) Role of soluble endoglin in BMP9 signaling. Proc Natl Acad Sci U S A 116(36):17800–17808. https://doi.org/10.1073/pnas.1816661116
Ruiz-Remolina L, Ollauri-Ibanez C, Perez-Roque L, Nunez-Gomez E, Perez-Barriocanal F, Lopez-Novoa JM, Pericacho M, Rodriguez-Barbero A (2017) Circulating soluble endoglin modifies the inflammatory response in mice. PLoS ONE 12(11):e0188204. https://doi.org/10.1371/journal.pone.0188204
Nemeckova I, Serwadczak A, Oujo B, Jezkova K, Rathouska J, Fikrova P, Varejckova M, Bernabeu C, Lopez-Novoa JM, Chlopicki S, Nachtigal P (2015) High soluble endoglin levels do not induce endothelial dysfunction in mouse aorta. PLoS ONE 10(3):e0119665. https://doi.org/10.1371/journal.pone.0119665
Jezkova K, Rathouska J, Nemeckova I, Fikrova P, Dolezelova E, Varejckova M, Vitverova B, Tysonova K, Serwadczak A, Buczek E, Bernabeu C, Lopez-Novoa JM, Chlopicki S, Nachtigal P (2016) High levels of soluble endoglin induce a proinflammatory and oxidative-stress phenotype associated with preserved NO-dependent vasodilatation in aortas from mice fed a high-fat diet. J Vasc Res 53(3–4):149–162. https://doi.org/10.1159/000448996
Gallardo-Vara E, Gamella-Pozuelo L, Perez-Roque L, Bartha JL, Garcia-Palmero I, Casal JI, Lopez-Novoa JM, Pericacho M, Bernabeu C (2020) Potential role of circulating endoglin in hypertension via the upregulated expression of BMP4. Cells. https://doi.org/10.3390/cells9040988
Vitverova B, Blazickova K, Najmanova I, Vicen M, Hyspler R, Dolezelova E, Nemeckova I, Tebbens JD, Bernabeu C, Pericacho M, Nachtigal P (2018) Soluble endoglin and hypercholesterolemia aggravate endothelial and vessel wall dysfunction in mouse aorta. Atherosclerosis 271:15–25. https://doi.org/10.1016/j.atherosclerosis.2018.02.008
Dolezelova E, Sa ICI, Prasnicka A, Hroch M, Hyspler R, Ticha A, Lastuvkova H, Cermanova J, Pericacho M, Visek J, Lasticova M, Micuda S, Nachtigal P (2019) High soluble endoglin levels regulate cholesterol homeostasis and bile acids turnover in the liver of transgenic mice. Life Sci 232:116643. https://doi.org/10.1016/j.lfs.2019.116643
Nachtigal P, Pospisilova N, Vecerova L, Micuda S, Brcakova E, Pospechova K, Semecky V (2009) Atorvastatin increases endoglin, SMAD2, phosphorylated SMAD2/3 and eNOS expression in ApoE/LDLR double knockout mice. J Atheroscler Thromb 16(3):265–274
Giordano A, Romano S, Monaco M, Sorrentino A, Corcione N, Di Pace AL, Ferraro P, Nappo G, Polimeno M, Romano MF (2012) Differential effect of atorvastatin and tacrolimus on proliferation of vascular smooth muscle and endothelial cells. Am J Physiol Heart Circ Physiol 302(1):H135-142. https://doi.org/10.1152/ajpheart.00490.2011
Zemankova L, Varejckova M, Dolezelova E, Fikrova P, Jezkova K, Rathouska J, Cerveny L, Botella LM, Bernabeu C, Nemeckova I, Nachtigal P (2015) Atorvastatin-induced endothelial nitric oxide synthase expression in endothelial cells is mediated by endoglin. J Physiol Pharmacol 66(3):403-413
Shyu KG, Wang BW, Chen WJ, Kuan P, Hung CR (2010) Mechanism of the inhibitory effect of atorvastatin on endoglin expression induced by transforming growth factor-beta1 in cultured cardiac fibroblasts. Eur J Heart Fail 12(3):219–226. https://doi.org/10.1093/eurjhf/hfq011
Brownfoot FC, Tong S, Hannan NJ, Hastie R, Cannon P, Kaitu’u-Lino TJ (2016) Effects of simvastatin, rosuvastatin and pravastatin on soluble fms-like tyrosine kinase 1 (sFlt-1) and soluble endoglin (sENG) secretion from human umbilical vein endothelial cells, primary trophoblast cells and placenta. BMC Pregnancy Childbirth 16:117. https://doi.org/10.1186/s12884-016-0902-3
Romero R, Erez O, Huttemann M, Maymon E, Panaitescu B, Conde-Agudelo A, Pacora P, Yoon BH, Grossman LI (2017) Metformin, the aspirin of the 21st century: its role in gestational diabetes mellitus, prevention of preeclampsia and cancer, and the promotion of longevity. Am J Obstet Gynecol 217(3):282–302. https://doi.org/10.1016/j.ajog.2017.06.003
Buda V, Andor M, Baibata DE, Cozlac R, Radu G, Coricovac D, Danciu C, Ledeti I, Cheveresan A, Nica C, Tuduce P, Tomescu MC (2019) Decreased sEng plasma levels in hypertensive patients with endothelial dysfunction under chronic treatment with Perindopril. Drug Des Devel Ther 13:1915–1925. https://doi.org/10.2147/DDDT.S186378
Hannan NJ, Brownfoot FC, Cannon P, Deo M, Beard S, Nguyen TV, Palmer KR, Tong S, Kaitu’u-Lino TJ (2017) Resveratrol inhibits release of soluble fms-like tyrosine kinase (sFlt-1) and soluble endoglin and improves vascular dysfunction—implications as a preeclampsia treatment. Scientific Reports 7(1):1819. https://doi.org/10.1038/s41598-017-01993-w
Liu Y, Tian H, Blobe GC, Theuer CP, Hurwitz HI, Nixon AB (2014) Effects of the combination of TRC105 and bevacizumab on endothelial cell biology. Invest New Drugs 32(5):851–859. https://doi.org/10.1007/s10637-014-0129-y
Kumar S, Pan CC, Bloodworth JC, Nixon AB, Theuer C, Hoyt DG, Lee NY (2014) Antibody-directed coupling of endoglin and MMP-14 is a key mechanism for endoglin shedding and deregulation of TGF-beta signaling. Oncogene 33(30):3970–3979. https://doi.org/10.1038/onc.2013.386
Funding
This work was supported by project EFSA-CDN (No. CZ.02.1.01/0.0/0.0/16_019/0000841) co-funded by ERDF, Specific University Research (SVV 260 549), Charles University Grant Agency, GAUK 1130120/C, GAUK 1166119/C, and AZV CZ No. 17-31754A.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest, financial or otherwise, are declared by the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vicen, M., Igreja Sá, I.C., Tripská, K. et al. Membrane and soluble endoglin role in cardiovascular and metabolic disorders related to metabolic syndrome. Cell. Mol. Life Sci. 78, 2405–2418 (2021). https://doi.org/10.1007/s00018-020-03701-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00018-020-03701-w