Abstract
The transfer of genes into cells, both in vitro and in vivo, is critical for studying gene function and conducting gene therapy. Methods that utilize viral and nonviral vectors, as well as physical approaches, have been explored. Viral vector-mediated gene transfer employs replication-deficient viruses such as retrovirus, adenovirus, adeno-associated virus and herpes simplex virus. A major advantage of viral vectors is their high gene delivery efficiency. The nonviral vectors developed so far include cationic liposomes, cationic polymers, synthetic peptides and naturally occurring compounds. These nonviral vectors appear to be highly effective in gene delivery to cultured cells in vitro but are significantly less effective in vivo. Physical methods utilize mechanical pressure, electric shock or hydrodynamic force to transiently permeate the cell membrane to transfer DNA into target cells. They are simpler than viral- and nonviral-based systems and highly effective for localized gene delivery. The past decade has seen significant efforts to establish the most desirable method for safe, effective and target-specific gene delivery, and good progress has been made. The objectives of this review are to (i) explain the rationale for the design of viral, nonviral and physical methods for gene delivery; (ii) provide a summary on recent advances in gene transfer technology; (iii) discuss advantages and disadvantages of each of the most commonly used gene delivery methods; and (iv) provide future perspectives.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1. Introduction
Gene delivery is an essential first step for studies that require expression of an exogenous gene in a target cell. Because of its large size and anionic property, DNA carrying the therapeutic gene(s) must cross the membrane barrier and reach the nucleus of the target cells where gene expression takes place. For effective gene delivery in vivo, it is also necessary to overcome nuclease-mediated degradation and DNA uptake by nontargeted cells after systemic administration of the exogenous DNA.
Currently, three categories of gene delivery methods are available: (i) viral vector based; (ii) nonviral vector based; and (iii) physical methods. Viral vectors are mostly replication deficient and genetically modified viruses. Viral vectors have the advantage of high delivery efficiency to a variety of cells and were employed in the first gene therapy clinical trial in 1990.[1] Nonviral vectors, such as synthetic and natural compounds, are less toxic than the viral vectors, offer flexibility in the size of gene they can deliver and have low immunogenicity. The physical methods employ physical force to facilitate gene transfer into cells. Compared with viral vectors, the nonviral and physical methods developed so far exhibit relatively low delivery efficiency, especially for in vivo gene delivery. The following is a brief summary of the recent advances in each of the three gene delivery systems.
2. Virus-Based Gene Delivery Systems
Almost always, virus-based gene delivery is accomplished by using replication-deficient viruses containing the gene of interest, but with the disease-causing sequences deleted from the viral genome.[2] Both RNA and DNA viruses have been utilized.[3] The primary feature of RNA-based viral vectors, such as retroviruses, is that they are capable of long-term transgene expression through gene integration.[4,5] DNA-based viral vectors normally result in transgene expression in episomal form without integration.[6] Major features of the most commonly used viral vectors are summarized in table I.
2.1 Retroviral Vectors
The most commonly used RNA viral vectors are derived from retroviruses. These are enveloped viruses with a diameter of 80–130 nm and a genome size of 8–11 kilobases (kb).[4] The viral genome is encased within the capsid along with integrase and reverse transcriptase. Retroviral vectors are produced simply by replacing replication elements with the gene of interest but retaining all necessary RNA regions, primarily the long terminal repeat (LTR) that plays an important role in packaging, reverse transcription, integration and transcription regulation. The retroviral vectors are produced in packaging cells that provide all essential viral proteins in trans. The vectors themselves have all the viral genes deleted and can accept up to 7–10kb of an exogenous gene sequence.[4,5] A successful gene delivery by retroviral vectors involves interaction of viral envelope proteins with appropriate receptors of the host cells, and fusion of lipid membrane between the viral particles and the host cells. Entry of the viral core into the cell allows the reverse transcriptase to convert the viral genome to a double-stranded DNA provirus, which is then inserted into a host chromosome with the help of integrase.[3,4] To date, retroviral vectors have been used more than any other gene transfer vehicle for gene therapy of severe combined immunodeficiency (SCID) using the ex vivo approach.[1,7–9] RNA viral vectors under development include oncoretroviruses encoding structural genes of gag, pol and env, and lentiviruses and spumaviruses, which contain additional viral proteins.[4,5]
2.1.1 Oncoretroviral Vectors
The first generation of retroviral vectors was developed from the murine leukaemia virus. The vectors themselves had all the viral genes deleted and were fully replication deficient. However, a significant overlap existed between the vector and the packaging components, which represented a high risk of recombination to yield replication-competent retroviruses (RCRs). To minimize RCR production, an early improvement was to split the packaging components, placing the gag, pol and env genes into two separate plasmids.[10] The risk of LTR overlap-based creation of RCRs was reduced by the use of heterologous promoters and polyA signal in the packaging construct.[11] Improvement was made in the titre (number of colony-forming units per mL) by establishing stable packaging cells and by the development of transient expression systems that were capable of producing high titres.[12]
The major advantage of retroviral vectors is that they integrate into the host genome, but this is a double-edged sword. [13] On the one hand, it allows for the possibility of stable and long-term gene expression that can be passed to the daughter cells but, on the other hand, the possibility of insertion into pre-oncogene or the site for inactivation of tumour suppressor genes renders the risk of subsequent tumour development. Indeed, five of twenty patients who received ex-vivo transduced, autologous CD34+ haematopoietic progenitor cells for the treatment of X-linked SCID, developed T-cell leukaemia between 23 and 68 months after treatment.[14] The disease was fatal for one patient and was cured in four others. All five cases featured an uncontrolled proliferation of a specific subtype of T cells caused by the deregulated expression of oncogene (LMO2) as a result of the integration of provirus.[15] The enhancer activity of the viral LTR (used to drive therapeutic gene expression) had transactivated the oncogene.[16] Detailed analysis has revealed that the retroviral vectors inserted their sequence into actively transcribed genes in a semirandom manner (including both promoter and gene coding region). On the basis of these observations, the LTR enhancer element in the vectors was removed and the internal promoter added for a safer gene transfer.[17]
Recently, Aiuti et al.[8] reported the clinical outcome of gene therapy for adenosine deaminase deficiency (ADA) SCID. In this trial, ADA-expressing retroviral vectors were transfused into CD34+ bone marrow cells ex vivo and eight often patients have essentially been treated. Their blood continues to show ADA after the median follow up of 4.0 years (range 1.8–8.0 years), and the patients are no longer in need of enzyme-replacement therapy. No leukaemia developed in any of these patients, suggesting that both vectors and the transgene played the important roles in causing adverse effects in patients.
2.1.2 Lentiviral Vectors
Lentiviral vectors have been the most studied retroviral vectors for gene delivery in recent years. It is molecularly modified lentiviruses that belong to a subclass of retroviruses that have three to six additional accessory viral proteins that regulate viral gene expression and infectivity, in addition to three essential gag, pol and env gene products.[18] These viral proteins facilitate an active transport of the pre-integration complex through the nucleopore; thus, lentiviral vectors do not require the breakdown of the nuclear membrane[19] and are able to transduce nondividing cells. [20,21] Lentiviruses favour transgene integration near active transcription sites, while oncoretroviruses preferentially integrate at the transcription start site. [11,22] Without any accessory genes, current lentiviral vectors are considered reasonably safe, because the replication of the vectors is highly inhibited and the possibility of recombination is reduced.[22,23] Recent work showed successful gene transfer by lentiviral vectors into quiescent T and B lymphocytes for immunotherapy of several genetic dysfunctions of the haematopoietic system.[24–27]
Results from an ongoing lentivirus-based gene therapy trial in France for b-thalassaemia showed that one patient had not required blood transfusions for the past 16 months. [28] Another successful use of lentiviral vector in a clinical trial was reported for the treatment of X-linked adrenoleukodystrophy due to a deficiency of the ABCD1 gene.[29] In this trial, progressive cerebral demyelination in two patients was successfully blocked for 14–16 months after lentiviral delivery of wild-type ABCD1 to CD34+ cells ex vivo.[29] These results encourage more clinical investigation into the use of lentiviral vectors for human gene therapy.
2.1.3 Foamy Viral Vectors
Recently developed foamy viral vectors are modified foamy viruses (FVs), which are the largest retroviruses with a genome size over 13 kb and are capable of packaging 9.2 kb of nucleic sequences.[30–32] FVs infect dividing cells, can also form a stable transduction intermediate in nondividing cells, do not require entry of the core for reverse transcription and have no preference for integrating into the genome.[33] Recent work demonstrated the therapeutic potential of FV vectors in haematopoietic stem cell gene therapy. [34,35] FV vector-based delivery of the Fanconi anemia complementation group C gene in a murine Fanconi anaemia model showed functional correction of haematopoietic stem cells.[35] Bauer et al.[34] reported the successful gene therapy to the canine leukocyte adhesion deficiency (CLAD) model by administrating the FV vectors expressing canine CD 18. Four of the five dogs treated showed complete reversal of the CLAD phenotype, which was sustained for more than 2 years. Clinical trials of FV vector-based human gene therapy have not been reported.
2.2 DNA Viral Vectors
2.2.1 Adenoviral Vectors
The most studied DNA viral vectors are modified adeno-viruses that were discovered in 1953 as the causative agents of the common cold.[36] In 1977, Graham et al.[37] developed a cell line enabling the first production of recombinant adenoviruses in a helper-free environment. Since that time, adenoviral vectors have received much attention as gene transfer agents.[6] There are over 100 adenoviral serotypes identified that can infect and replicate in a wide range of organs, including 51 classified into six subgroups (A-F).[38,39] Of these, serotypes 2 and 5 in subgroup B are the most characterized viruses.
Adenovirions are icosahedral in shape, 70–90 nm in diameter and not enveloped. The viral genome is large, consisting of a double-stranded DNA molecule of 36–38 kb in size. Viral DNA replication and transcription is complex, and the viral replication and assembly occur only in the nucleus of the infected cells. There are nine major complex transcription units divided into early (E1A, E1B, E2-E4) and late (L1-L5) transcripts flanked by inverted terminal repeat (ITR). As the E1 A region encodes the principal protein that activates the expression of other adenoviral transcription units’ genes, and E1 proteins play essential roles in viral replication,[40] the E1 gene was replaced with the transgene in the first generation of adenoviral vectors.[41,42] Combining the E1 and nonessential region of E3, the cloning capacity of adenoviral vectors can be increased up to 8.3 kb.[43]
Adenoviral infection is a highly complex process and is independent of cell cycle. Viral fibre proteins bind to the Cox-sackievirus and adenovirus receptor of the target cells to initiate the infection. [39,44] Internalization occurs via receptor-mediated endocytosis followed by release from the endosome.[45] Once inside the cytoplasm, the viral capsid undergoes disassembly as it migrates to the nuclear pore. Nuclear entry of the viral DNA is completed upon capsid dissociation, leading to an active transcription and replication within the nucleus episomally.
In principle, recombinant adenoviral vectors are prepared from two components: a viral DNA vector and a packaging cell line. The first generation of adenoviral DNA vector is a plasmid DNA that contains a portion of the viral genome with E1 and E3 regions deleted and the desired gene sequence cloned into the space of the deletion in the genome. The adenoviral vector is produced using either in vitro homologous recombination or ligation. Both the adenoviral vector and the plasmid carrying the necessary viral genes are co-transfected into the packaging cell line. These DNA species are then left to undergo homologous recombination within the cells resulting in vector production. The 293 cells that constitutively express the E1 gene are utilized for viral vector production as a packaging cell. Generally, approximately 1013–1014 viral particles can be produced by fifty 150 mm cell culture plates (about a billion 293 cells).[46]
Although adenoviral vectors are of human origin, numerous other animals have been used to demonstrate efficient gene transfer, including mice, rats, pigs, rabbits and nonhuman primates. Many types of cells can be transduced depending on the route of administration. Direct injection into the peritoneum, kidney, pancreas, cerebral spinal fluid, skeletal muscle, brain, cardiac muscle, coronary artery and many other tissues, results in transgene expression. However, intravenous injection into rodents results primarily in transgene expression in the liver and spleen. Typically, transgene expression that results from the first generation of adenoviral vectors is transient regardless of the route of administration and the type of cells. [47] Expression usually peaks in 1–7 days and declines rapidly to an undetectable level by 2–4 weeks. Both cellular and humoral immune response against viral proteins is observed and is believed to be responsible for the short duration of transgene expression.[48,49]
Viral DNA included in the vectors is believed to be responsible for transient gene expression. Methods have been examined to eliminate all adenoviral genes and the helper-dependent or ‘gutless’ adenoviral vectors have been developed that carry no viral sequences except for 100 bp of ITR, which is required for replication, and the cis-acting packaging signal. Those removed viral proteins are supplied from the replication incompetent (helper) viruses, in trans, in helper cell lines, such as HEK293 cells.[50,51] Through such an improvement, helper-dependent adenoviral vectors have a large cloning capacity up to 37 kb and have an improved safety profile, which results in sustained transgene expression in vivo. The persistent gene expression has been shown in mice and baboons for more than 1 year with little decline.[52,53] It is clear from these studies that the toxicology of the helper-dependent adenoviral vectors is significantly less than that of the first generation of adenoviral vectors. While the gutless vectors exhibit much improved properties for gene delivery, the remaining challenge for further development of gutless vectors is to improve vector production and the immunogenicity intrinsic to viral proteins.
Adenoviral vectors have been extensively studied for cancer gene therapy. Recently, efforts have been made in the development of oncolytic adenoviral vectors that are capable of replicating in tumour cells. Replication of adenoviral vectors in cancer cells amplifies the initial viral inoculum, resulting in the destruction of the infected tumour cells. H101 (Shanghai Sunway Biotech, Shanghai, China), the E1b55K-deleted oncolytic adenoviruses, have been approved as a drug in China for the treatment of cancer.[54] A response rate of 79% (41/52) in patients injected with H101 while maintaining chemotherapy has been reported in a phase III trial.[54] In the US, there are several clinical trials involving oncolytic adenovirus such as ONYX-015 (Onyx Pharmaceuticals, Emeryville, CA, USA).[55]
2.2.2 Adeno-Associated Viral Vectors
Adeno-associated virus (AAV) vectors are derived from a nonpathogenic parvovirus, a satellite virus of human adenovirus and the herpes simplex virus (HSV).[56,57] There are 12 human serotypes and more than 100 serotypes of AAVs from nonhuman primates identified with different targeting capacities.[58] Among these serotypes, the AAV serotype 2 (AAV2) was the first clone identified and used to deliver transgene.[59] The small icosahedra virion is approximately 18–26nm in diameter and contains a single strand DNA of 4–5 kb. The virion contains either the sense or antisense strand of the DNA and appears to have no strand preference. There are two genes in viral genome DNA, rep and cap, which encode seven major transcription units, Rep40, Rep52, Rep68, Rep78, VP1, VP2 and VP3, respectively. The viral genome has a palindromic sequence at each end, referred to as the ITR. These ITRs are important in the site-specific integration of AAV DNA into a specific site in chromosome 19,[60] although AAV exist primarily in episomal form. The ability of the wild-type AAV to selectively integrate into chromosome 19 made it an attractive candidate as a vector for the treatment of genetic diseases. Rep proteins are required for replication and packaging, and VP proteins are structural proteins forming viral capsid. The viral particle enters the cell through receptor-mediated endocytosis followed by migration and release of its genome into the nucleus. It is worth noting that each serotype of AAV has its unique approach for infecting the host cells. Single-stranded DNA is converted to double-stranded vector genome from which the transgene is expressed.
Construction of AAV vectors consists of the recombinant AAV vector plasmid DNA replacing the viral rep and cap genes with transgene sequences, and a non-rescueable AAV helper plasmid that encodes for the AAV capsid proteins. The AAV vector is produced by a plasmid-based system analogous to retroviral plasmid vectors but, in this case, the gene of interest is bracketed by ITRs. Also required is either a wild-type adenovirus or an HSV, and a cell line for viral propagation.[59,61] Unlike the vector systems described in this section, the cell line does not need to contain any portion of the AAV genome since all required genomic elements are provided by the two plasmids. Cells are first infected with the wild-type adenovirus or HSV, and then both recombinant AAV vector plasmid DNA and the helper plasmid are co-transfected into the cells. The cells produce mature recombinant AAV vectors as well as wild-type adenovirus or HSV. The wild-type adenovirus or HSV is removed by either density gradient centrifugation or heat inactivation. Further improvement to reduce the risk of production of a wild-type virus was made by establishing the helper virus-free method. In this system, the transfection of mini-adenovirus helper plasmid together with vector and packaging plasmid into the adenovirusE1 -expressing HEK293 cells is achieved using a standard procedure of transfection. [62,63]
The target-organ preference depends on the infectivity of wild serotype to those organs. AAV1, 2 and 5, preferentially transduce into neuronal and muscular cells and AAV8 prefer hepatocytes.[58] As AAV vectors do not contain the rep gene, the majority of the AAV genome stays in episomal form in the host cell nucleus. The toxicity of AAV vectors is much lower than other viral vectors.
Phase I studies were performed using AAV2 vectors for gene therapy of haemophilia B, initially through intramuscular injection and later by intraportal injection to target liver cells. [64,65] Factor IX protein was detected in two cases and sustained for 4–9 weeks. [66] The transient gene expression is likely caused by the activation of the memory CD8+ T cells against the AAV capsid protein, rather than Factor IX protein.[66] Additional efforts are needed to reduce the immune response and extend its packaging capacity of the AAV imposed by the small size of the AAV genome (4681 nt), and inefficient delivery of genes that are larger than its genome.
2.2.3 Herpes Simplex Viral Vectors
HSV is a human neurotropic virus with an overall diameter of 180–200 nm. Its genome is a double-stranded DNA molecule of about 150 kb in length, encoding over 80 proteins.[67] The virus itself is transmitted by direct contact and replicates in the skin or mucosal membranes before infecting cells of the CNS.[67] It exhibits both lytic and latent activity. The lytic cycle results in viral replication and cell death. The latent infection allows for the virus to be maintained in the host for an extended period of time. The virus enters cells by fusion triggered by binding of viral glycoprotein gB and gD to the heparin sulfate moiety of the cell surface protein.[68] DNA enters the cell and circularizes.
A similar strategy to that of producing adenoviral vectors has been used to generate HSV vectors.[68] A few of the immediate early protein genes were removed to generate viral vectors unable to replicate except in a complementing cell line. Because of its large genome size, the recombinant HSV vectors should be capable of containing an inserted gene up to 30 kb.[67,69] Since HSV is a neurotropic virus, many studies have shown persistent gene expression in neuronal cells, and clinical trials for gene therapy of brain tumours have been performed using HSV vectors.[70,71] Recent studies revealed that the HSV vector-mediated gene transfer resulted in blockade pain transmission or reversal of the chronic pain state in vivo.[72,73]
2.3 Other Types of Viral Vectors
In addition to the more commonly used viral vectors described in the previous sections, many other viruses have been considered as a potential carrier for gene delivery. While most of them have not been used in clinical studies, there is an abundance of developmental and preclinical data demonstrating the various merits of these systems. Several members of the alphavirus genus, including the Semliki Forest virus, Sindbis virus and Venezuelan equine encephalitis, have been developed into gene delivery vectors. While their use has not been widespread, and problems related to virus-induced toxicity have been seen, their prominent neurotropism has made them attractive for use in gene delivery to cells in the CNS. In addition, efforts to blend properties of different viral vectors to obtain new and more desirable vectors are seen.[3] One active area is the combination of AAV and adenoviruses. A double-stranded AAV genome inserted into an adenoviral capsid to produce a combination of AAV and adenoviral ITR, has been shown to transduce and integrate in cells.[74] A different approach involves the placement of an AAV vector into gutless adenoviruses and engineering the vector to transiently express Rep protein in an attempt to get site-specific integration and to avoid insertional mutagenesis.[75] Other hybrid viral vectors include HSV/AAV and HSV/Epstein-Barr virus.[76] Interestingly, several groups have attempted to coat the viral vectors with polymers or lipids.[77] The primary objective of the coating is to hide the virus from the host immune system upon in vivo administration, which in turn prevents degradation and increases vector circulation time and, subsequently, tissue transduction. Another function of viral encapsulation is to retarget viral vectors by ablating its native tropism and then re-targeting the virus by conjugating targeting ligands directly to the polymers.
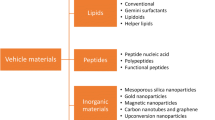
3. Nonviral Vector-Based Gene Delivery
Another strategy for gene delivery is based on the use of natural or synthetic compounds (also called nonviral vectors) in which complexes of DNA, proteins, polymers or lipids are formed in particles capable of efficiently transferring genes into cells. Delivery of genetic material using nonviral vectors preceded the development of viral-based vectors. The nonviral approach for gene delivery can be traced back to the work of Avery, MacLeod and McCarthy who showed a change of cellular phenotype following exogenous DNA exposure.[78] The first nonviral technique to gain wide acceptance was calcium phosphate-mediated transfection.[79] This system has undergone little change since being developed in the early 1970s. Since then, the nonviral vectors earned their candidacy for gene therapy and various clinical trials are ongoing.[80,81] The major characteristics of the nonviral approach for gene delivery are summarized in table II.
3.1 Liposome-Based Nonviral Vectors
The most effective nonviral vectors developed so far are made of liposomes. Liposomes were first described in 1965 as a model of cellular membrane,[82] and were quickly applied to the delivery of substances to cells. They are microscopic particles consisting of one or more concentric lipid bilayers enclosing an aqueous compartment and are formed spontaneously when a film of lipids is hydrated in an aqueous solution. Many different types of liposomes have been developed in the past and liposomes composed of cationic lipids are found to be most active in gene delivery.[83] These lipids are made of mono- or multicationic head groups and a hydrophobic anchor (alphatic chains or cholesterol moiety) bridged together by a linker.[84] Depending on the chemical structure and the conditions for liposome preparation, these cationic lipids can be used to make cationic liposomes with or without additional lipids (helper lipids). A variety of positively charged lipid formulations are now commercially available and many others are under development (for reviews see Liu et al.[85] and Montier et al.[86] ).
Cationic liposomes and DNA interact spontaneously to form complexes (lipoplexes) with 100% DNA loading efficiency. In other words, all of the DNA molecules are complexed with the liposomes, provided enough cationic liposomes are available. It is believed that the negative charges of the DNA interact with the positively charged groups of the liposomes. The lipid to DNA ratio, and overall lipid concentrations used in forming these complexes, are extremely important for efficient gene delivery and vary with applications.[87]
Liposomes offer several advantages in delivering genes to cells as follows: (i) being synthetic, they are relatively cheap to make and do not cause disease; (ii) they offer a degree of protection to the DNA from nuclease-mediated degradation; (iii) they can carry large pieces of DNA, potentially as large as a chromosome; and (iv) can be targeted to specific cells or tissues. In addition, liposomes overcome problems inherent with viral vectors with regard to immunogenicity and replication-competent virus contamination. The ability to synthesize a wide variety of lipids has resulted in a highly adaptable and flexible system capable of gene delivery both in vitro and in vivo. As liposome technology is further developed, it should be possible to produce reagents with improved in vivo gene delivery into specific tissues. Successful delivery of DNA and RNA to a variety of cell types has been reported, including tumour, airway epithelial cells, endothelial cells, hepatocytes, muscle cells and others by intratissue or intravenous injection into animals.[88–90]
Various liposome-based vectors have been utilized in a number of clinical trials for cancer treatment. For example, Stopeck et al.[91,92] reported the results of phase I and II clinical trials assessing the safety and efficacy of Allovectin-7® (Vical, San Diego, CA, USA), a plasmid DNA carrying HLAB7 and β2 microglobulin genes complexed with DMRIE/DOPE liposomes. Currently, this immunotherapeutic is in phase III development for patients with stage III or IV melanoma. The remaining challenge for liposome-based gene delivery is to enhance their in vivo delivery efficiency.
3.2 Polymer-Based Nonviral Vectors
Cationic polymers constitute another category of nonviral vectors that have been used for gene delivery. A significant number of polymers, such as polyethylenimine,[93–95] polyamidoamine,[96–98] polyallylamine,[99] chitosan,[100] dendrimers,[101] cationic proteins[102] and peptides,[103] have been studied for in vivo and in vitro gene delivery. These cationic polymers condense DNA into small particles and prevent DNA from degradation. The cellular uptake is via receptor-mediated endocytosis. Similar to cationic lipids, polymers are also easy to make and flexible for additionalmodifications. Combining ‘stealth’ properties of polyethylene glycol for prolonged half-life in blood with cationic polymer for DNA condensation has resulted in a very attractive property of DNA/polymer complexes (polyplexes) for gene delivery to tumours.[104] In fact, polyplexes are being investigated in phase I and phase II clinical trials for the treatment of cystic fibrosis and ocular degenerative diseases.[105]
Hybrids of lipids with polymers have been explored to improve gene delivery.[106] In this system, DNA is pre-condensed with either poly-L-lysine,[107] protamine,[108] histone or several synthetic polypeptides,[109] followed by lipid wrapping using either cationic liposomes, anionic liposomes or amphiphilic polymers.[110] Additional efforts are needed to prove that the lipid/polymer hybrid system is superior to that of lipoplexes or polyplexes for in vivo gene delivery.[111]
4. Gene Delivery Using Physical Approaches
Gene delivery using physical principles, commonly called physical methods, has attracted increasing attention in recent years. It usually employs a physical force to overcome the membrane barrier of the cells and facilitates intracellular gene transfer. An obvious advantage of physical methods is the simplicity. A fragment of DNA or plasmid containing transgene, and the regulatory elements for its expression, is directly delivered into cells without involving any substances that could be cytotoxic or immunogenic as commonly seen in viral or nonviral vectors.
4.1 Gene Delivery by Needle Injection
The simplest physical method for gene delivery is by direct injection of DNA through a needle-carrying syringe into tissue. Following the initial report of successful gene transfer to muscle cells in mice by Wolff et al.,[112] tissues that exhibit transgene expression following a plasmid DNA injection have been expanded to skin,[113] cardiac muscle,[114] liver[115] and solid tumour.[116] The major application of this gene delivery method is DNA vaccination.[117] The shortfall of this procedure is low gene delivery efficiency, and the transfected cells are limited to the needle track. Some efforts have been made to achieve a higher level of transgene expression by optimizing plasmid construct.[118]
4.2 Ballistic DNA Injection
This method of gene delivery is also known as particle bombardment, microprojectile gene transfer or gene gun, and was first developed for gene transfer into plants in 1987. [119] Since its initial introduction, it has been modified to transfer genes into mammalian cells both in vitro and in vivo.[120] The principle of this method is to propel DNA-coated gold particles against cells and force intracellular DNA transfer. The accelerating force for DNA-containing particles can be a high-voltage electronic discharge, spark discharge or helium pressure discharge. Ballistic DNA injection has been successfully used to transfer genes into a wide variety of cell lines. In vivo applications have predominantly focused on the liver, skin, muscle or other organs that can be surgically exposed.[121] Ballistic DNA injection also offers the capacity to deliver precise DNA dosages. Unfortunately, genes delivered by this method are expressed transiently, and there is considerable cell damage occurring at the centre of the discharge site. The gun-based gene delivery method is more appropriate for gene delivery to skin for vaccination[122–125] and immune therapy[126] because of the shallow penetration of DNA. This method has been utilized in vaccination against the influenza virus[127] and in gene therapy for treatment of ovarian cancer.[128]
4.3 Electroporation
Electroporation was first utilized for gene transfer to mammalian cells by Neumann et al.[129] Gene delivery is achieved by generating pores on a cell membrane through electric pulses. Electroporation works best on cells that are suspended in solution, but also works on cells in solid tissue where electrodes can be applied.[130] Gene delivery efficiency is determined by the pulse intensity, duration and frequency.[131] In vivo electroporation creates transient permeability of the cell membrane and induces a low level of inflammation at the injection site, facilitating DNA uptake by parenchyma cells and antigen-presenting cells.[132] Thus, this method has been clinically tested for DNA-based vaccination and for cancer treatment.[132–135] Currently, clinical trials are ongoing in the treatment of melanoma, prostate cancer, papilloma virus infection, hepatitis C virus infection and HIV infection.[135] The limitation of the current procedure is that the number of cells transfected is relatively small and that surgery is required to reach internal organs.
4.4 Sonoporation
The sonoporation gene delivery technique was developed in the 1990s.[136–138] It utilizes ultrasound to temporarily permeabilize the cell membrane to allow cellular uptake of DNA. Unlike other nonviral methods, sonoporation combines gene delivery with the possibility of restricting the effect to the area where ultrasound is applied. Gene delivery efficiency appears to be controlled by pulse intensity, frequency and duration.[139] Sonoporation-mediated gene delivery has been demonstrated in the cornea,[140] brain,[141] CNS,[142–144] bone,[145] peritoneal cavity,[146] kidney,[147] pancreas,[148] liver,[149,150] embryonic tissue,[151] dental pulp,[152] muscle[153,154] and heart.[155,156] More recent studies in mouse liver showed that inclusion of gasfilled microbubbles enhanced gene delivery efficiency.[149,150] Similar results were also obtained in tumour,[157–159] vascular tissue[160] and skeletal muscles.[161] Compared with other nonviral approaches, sonoporation-mediated gene delivery remains in its infancy. Additional efforts are needed to improve its efficiency, especially for in vivo applications.
4.5 Laser-Assisted Method (Photoporation)
The photoporation method, first reported by Zeira et al.,[162] employs a single laser pulse as the physical force to generate transient pores on a cell membrane to allow DNA to enter. Gene delivery efficiency appears to be controlled by the size of the focal point and pulse frequency of the laser. The level of transgene expression reported was similar to that of electroporation. In recent years, several advances have been made to improve gene delivery efficiency, one of which involved the use of carbon black nanoparticles to generate photoacoustic force upon laser stimulation.[163] More study is needed before this highly sophisticated procedure becomes a practical technique for gene delivery, not only in vitro but also in vivo.
4.6 Magnetofection
Magnetofection utilizes a magnetic field to promote transfection. Magnetofection employs magnetic nanoparticles made of iron oxide and coated with cationic lipids or polymers to complex with DNA through electrostatic interaction. The magnetic particles are then concentrated on the target cells by the influence of an external magnetic field. Similar to the mechanism of nonviral vector-based gene delivery, the cellular uptake of DNA is accomplished by endocytosis and pinocytosis.[164] It is postulated that DNA are released into the cytoplasm depending on the composition of the magnetic nanoparticles.[165] Magnetofection has been successfully applied to a wide range of primary cells and cells that are hard to transfect using other nonviral methods.[166] Recent work using a local injection of the nanoparticles into the gastrointestinal track and the ear vasculature[167] imply that this well accepted method for in vitro gene delivery may be applicable to in vivo gene delivery.
4.7 Hydrodynamic Gene Delivery (Hydroporation)
The hydrodynamic gene delivery method was reported by Liu et al.[168] and Zhang et al.[169] in 1999 and, since then, it has become one of the most commonly used methods for gene delivery to hepatocytes in rodents. Intrahepatic gene delivery is achieved by a rapid injection of a large volume of DNA solution via the tail vein in rodents that results in a transient enlargement of fenestrae, generation of a transient membrane defect on the plasma membrane and gene transfer into hepatocytes.[170] In mice, the optimal condition for gene delivery includes an injection volume equal to 8–10% of bodyweight, an injection time of 5–7 seconds and <20 μg of plasmid DNA per mouse.[168] Because of its simplicity, high efficiency and reproducibility, hydrodynamic gene delivery has been utilized for the delivery of DNA, small interfering RNA, proteins, small compounds and even viral vectors.[171–179] This technique has been widely used for gene therapy studies, gene knockdown, functional analysis of genetic elements and for establishing a disease model in animals.[171,176,180]
In an attempt to apply this simple procedure of gene delivery to the clinic, efforts have been made to reduce the total injection volume. Eastman et al.[181] demonstrated in rabbits that a volume of 15mL/kg can be safely injected into an isolated rabbit liver. Similar studies have been reported by several groups using pigs as an animal model.[172,182–184] A computer-controlled injection device has been developed for hydrodynamic gene delivery in large animals.[185] Using this system, Suda and colleagues[185] have reported safe and efficient gene delivery in pig liver, kidney and muscle. By combining the computer-controlled injection device with the imageguided catheterization technique, Kamimura et al.[186] has demonstrated lobe-specific gene delivery to the liver of pigs. Kamimura et al.[187] also assessed the effectiveness of the procedure in gene delivery to skeletal muscle in pigs. Comprehensive assessment of tissue damage has been conducted for hydrodynamic gene delivery to liver and muscles in small and large animals and the results showed no major tissue damage [186,187] The image-guided, lobe-specific hydrodynamic procedure has great potential to become the method of choice for human gene therapy without using viral or nonviral vectors.
5. Conclusions and Future Perspectives
The three gene delivery systems described in this review are not inclusive, but represent those commonly used in preclinical and clinical research or at an advanced stage of development. Considering the clinical trials conducted so far, 67% employed viral vectors and approximately 24% were performed using nonviral methods. [188] Although the methods summarized in this review have made and will continue to make important contributions in research and gene therapy, a number of different viral and nonviral vectors, some of which have yet to be fully exploited or even discovered, are likely to complement the current armamentarium. Practically, no single gene delivery method is likely to be optimal for all gene delivery needs. For a specific application, however, a ‘perfect’ method could be developed for gene delivery through noninvasive delivery routes, capable of targeting to the desired cells with high delivery efficiency and the appropriate amount of gene product for a desirable period of time.
Significant progress has been made in each of the three gene delivery systems. However, the success of gene therapy still needs a significant effort made to develop a safe and effective method applicable to human gene therapy. While viral vectors are highly effective and have been used in a few clinical trials, the intrinsic property of viral genome and proteins in stimulating carcinogenesis and an immune response remains the largest hurdle.[189,190] The key to this problem may lie in the effort to find a mechanism capable of integrating transgenes into a selected site in a chromosome and, thus, avoiding the need for repeated administration and insertion mutagenesis. For nonviral vector-based gene delivery, a variety of natural and synthetic compounds has been used in gene delivery studies, but their effectiveness in gene delivery remains orders of magnitude lower than that of viral vectors. As a result, current nonviral vectors are generally considered unacceptable for clinical use. Nevertheless, studies designed to identify factors critical for successful gene delivery in vitro and in vivo have provided important information to guide the future design of nonviral vectors. The concept of tailor-made gene carriers for gene delivery to specific types of cells may hold the key for future success. Gene delivery using a physical approach is relatively new, but has demonstrated its potential to transfer DNA into cells directly. The techniques described in this review have both positive and negative features, and it is unlikely that a single approach will be ideal for all applications. With the involvement of new technology and computer systems, and improved understanding of biological systems, solving technical problems of current physical methods is highly feasible. It is highly likely that the future of gene delivery for gene therapy lies in the hands of those who are able to integrate the principles of cell biology, engineering and computer sciences.
References
Blaese RM, Culver KW, Miller AD, et al. T lymphocyte-directed gene therapy for ADA-SCID: initial trial results after 4 years. Science 1995; 270: 475–80
Thomas CE, Ehrhardt A, Kay MA. Progress and problems with the use of viral vectors for gene therapy. Nat Rev Genet 2003; 4: 346–58
Kay MA, Glorioso JC, Naldini L. Viral vectors for gene therapy: the art of turning infectious agents into vehicles of therapeutics. Nat Med 2001; 7: 33–40
Barquinero J, Eixarch H, Perez-Melgosa M. Retroviral vectors: new applications for an old tool. Gene Ther 2004; 11 (Suppl. 1): S3–9
Daniel R, Smith JA. Integration site selection by retroviral vectors: molecular mechanism and clinical consequences. Hum Gene Ther 2008; 19: 557–68
St George JA. Gene therapy progress and prospects: adenoviral vectors. Gene Ther 2003; 10: 1135–41
Hacein-Bey-Abina S, Le Deist F, Carlier F, et al. Sustained correction of X-linked severe combined immunodeficiency by ex vivo gene therapy. N Engl J Med 2002; 346: 1185–93
Aiuti A, Cattaneo F, Galimberti S, et al. Gene therapy for immunodeficiency due to adenosine deaminase deficiency. N Engl J Med 2009; 360: 447–58
Hacein-Bey-Abina S, Hauer J, Lim A, et al. Efficacy of gene therapy for Xlinked severe combined immunodeficiency. N Engl J Med 2010; 363: 355–64
Danos O, Mulligan RC. Safe and efficient generation of recombinant retroviruses with amphotropic and ecotropic host ranges. Proc Natl Acad Sci U S A 1988; 85: 6460–4
Sinn PL, Sauter SL, McCray PBJ. Gene therapy progress and prospects: development of improved lentiviral and retroviral vectors — design, biosafety, and production. Gene Ther 2005; 12: 1089–98
Pear WS, Nolan GP, Scott ML, et al. Production of high-titer helper-free retroviruses by transient transfection. Proc Natl Acad Sci U S A 1993; 90: 8392–6
Roe T, Reynolds TC, Yu G, et al. Integration of murine leukemia virus DNA depends on mitosis. EMBO J 1993; 12: 2099–108
Fischer A, Hacein-Bey-Abina S, Cavazzana-Calvo M. 20 years of gene therapy for SCID. Nat Immunol 2010; 11: 457–60
Hacein-Bey-Abina S, Von Kalle C, Schmidt M, et al. LMO2-associated clonal T cell proliferation in two patients after gene therapy for SCID-X1. Science 2003; 302: 415–9
Howe SJ, Mansour MR, Schwarzwaelder K, et al. Insertional mutagenesis combined with acquired somatic mutations causes leukemogenesis following gene therapy of SCID-X1 patients. J Clin Invest 2008; 118: 3143–50
Lombardo A, Genovese P, Beausejour CM, et al. Gene editing in human stem cells using zinc finger nucleases and integrase-defective lentiviral vector delivery. Nat Biotechnol 2007; 25: 1298–306
Frankel AD, Young JA. HIV-1: fifteen proteins and an RNA. Annu Rev Biochem 1998; 67: 1–25
Lewis PF, Emerman M. Passage through mitosis is required for oncoretroviruses but not for the human immunodeficiency virus. J Virol 1994; 68: 510–6
Naldini L, Blomer U, Gallay P, et al. In vivo gene delivery and stable transduction of nondividing cells by a lentiviral vector. Science 1996; 272: 263–7
Vigna E, Naldini L. Lentiviral vectors: excellent tools for experimental gene transfer and promising candidates for gene therapy. J Gene Med 2000; 2: 308–16
Maátrai J, Chuah MK, Vanden Driessche T. Recent advances in lentiviral vector development and applications. Mol Ther 2010; 18: 477–90
Xu K, Ma H, McCown TJ, et al. Generation of a stable cell line producing high-titer self-inactivating lentiviral vectors. Mol Ther 2001; 3: 97–104
Thomas S, Stauss HJ, Morris EC. Molecular immunology lessons from therapeutic T-cell receptor gene transfer. Immunology 2010; 129: 170–7
Qasim W, Mackey T, Sinclair J, et al. Lentiviral vectors for T-cell suicide gene therapy: preservation of T-cell effector function after cytokine-mediated transduction. Mol Ther 2007; 15: 355–60
Cavalieri S, Cazzaniga S, Geuna M, et al. Human T lymphocytes transduced by lentiviral vectors in the absence of TCR activation maintain an intact immune competence. Blood 2003; 102: 497–505
Frecha C, Levy C, Cosset FL, et al. Advances in the field of lentivector-based transduction of T and B lymphocytes for gene therapy. Mol Ther 2010; 18: 1748–57
Kaiser J. Gene therapy: beta-thalassemia treatment succeeds, with a caveat. Science 2009; 326: 1468–9
Cartier N, Hacein-Bey-Abina S, Bartholomae CC, et al. Hematopoietic stem cell gene therapy with a lentiviral vector in X-linked adrenoleukodystrophy. Science 2009; 326: 818–23
Mergia A, Heinkelein M. Foamy virus vectors. Curr Top Microbiol Immunol 2003; 277: 131–59
Trobridge G, Josephson N, Vassilopoulos G, et al. Improved foamy virus vectors with minimal viral sequences. Mol Ther 2002; 6: 321–8
Erlwein O, McClure MO. Progress and prospects: foamy virus vectors enter a new age. Gene Ther 2010; 17: 1423–9
Trobridge GD. Foamy virus vectors for gene transfer. Expert Opin Biol Ther 2009; 9: 1427–36
Bauer Jr TR, Allen JM, Hai M, et al. Successful treatment of canine leukocyte adhesion deficiency by foamy virus vectors. Nat Med 2008; 14: 93–7
Si Y, Pulliam AC, Linka Y, et al. Overnight transduction with foamyviral vectors restores the long-term repopulating activity of Fancc-/- stem cells. Blood 2008; 112: 4458–65
Rowe WP, Huebner RJ, Gilmore LK, et al. Isolation of a cytopathogenic agent from human adenoids undergoing spontaneous degeneration in tissue culture. Proc Soc Exp Biol Med 1953; 84: 570–3
Graham FL, Smiley J, Russell WC, et al. Characteristics of a human cell line transformed by DNA from human adenovirus type 5. J Gen Virol 1977; 36: 59–74
Arnberg N. Adenovirus receptors: implications for tropism, treatment and targeting. Rev Med Virol 2009; 19: 165–78
Sharma A, Li X, Bangari DS, et al. Adenovirus receptors and their implications in gene delivery. Virus Res 2009; 143: 184–94
Flint J, Shenk T. Viral transactivating proteins. Ann Rev Genet 1997; 31: 177–212
Danthinne X, Imperiale MJ. Production of first generation adenovirus vectors: a review. Gene Ther 2000; 7: 1707–14
Nevins JR. Mechanism of activation of early viral transcription by the adenovirus E1A gene product. Cell 1981; 26: 213–20
Bett AJ, Haddara W, Prevec L, et al. An efficient and flexible system for construction of adenovirus vectors with insertions or deletions in early regions 1 and 3. Proc Natl Acad Sci U S A 1994; 91: 8802–6
Bergelson JM, Cunningham JA, Droguett G, et al. Isolation of a common receptor for Coxsackie B viruses and adenoviruses 2 and 5. Science 1997; 275: 1320–3
Leopold PL, Kreitzer G, Miyazawa N, et al. Dynein- and microtubulemediated translocation of adenovirus serotype 5 occurs after endosomal lysis. Hum Gene Ther 2000; 11: 151–65
He TC, Zhou S, da Costa LT, et al. A simplified system for generating recombinant adenoviruses. Proc Natl Acad Sci U S A 1998; 95: 2509–14
Spergel JM, Chen Kiang S. Interleukin 6 enhances a cellular activity that functionally substitutes for E1A protein in transactivation. Proc Natl Acad Sci U S A 1991; 88: 6472–6
Yang Y, Nunes FA, Berencsi K, et al. Cellular immunity to viral antigens limits E1-deleted adenoviruses for gene therapy. Proc Natl Acad Sci U S A 1994; 91: 4407–11
Liu Q, Muruve DA. Molecular basis of the inflammatory response to adenovirus vectors. Gene Ther 2003; 10: 935–40
Kochanek S, Schiedner G, Volpers C. High-capacity ‘gutless’ adenoviral vectors. Curr Opin Mol Ther 2001; 3: 454–63
Palmer DJ, Ng P. Helper-dependent adenoviral vectors for gene therapy. Hum Gene Ther 2005; 16: 1–16
Kim IH, Jozkowicz A, Piedra PA, et al. Lifetime correction of genetic deficiency in mice with a single injection of helper-dependent adenoviral vector. Proc Natl Acad Sci U S A 2001; 98: 13282–7
Brunetti Pierri N, Palmer DJ, Beaudet AL, et al. Acute toxicity after high-dose systemic injection of helper-dependent adenoviral vectors into nonhuman primates. Hum Gene Ther 2004; 15: 35–46
Yu W, Fang H. Clinical trials with oncolytic adenovirus in China. Curr Cancer Drug Targets 2007; 7: 141–8
Nemunaitis J, Khuri F, Ganly I, et al. Phase II trial of intratumoral administration of ONYX-015, a replication-selective adenovirus, in patients with refractory head and neck cancer. J Clin Oncol 2001; 19: 289–98
Atchison RW, Casto BC, Hammon WM. Adenovirus-associated defective virus particles. Science 1965; 149: 754–6
Hoggan MD, Blacklow NR, Rowe WP. Studies of small DNA viruses found in various adenovirus preparations: physical, biological, and immunological characteristics. Proc Natl Acad Sci U S A 1966; 55: 1467–74
Daya S, Berns KI. Gene therapy using adeno-associated virus vectors. Clin Microbiol Rev 2008; 21: 583–93
Hermonat PL, Muzyczka N. Use of adeno-associated virus as a mammalian DNA cloning vector: transduction of neomycin resistance into mammalian tissue culture cells. Proc Natl Acad Sci U S A 1984; 81: 6466–70
Smith RH. Adeno-associated virus integration: virus versus vector. Gene Ther 2008; 15: 817–22
Samulski RJ, Chang LS, Shenk T. Helper-free stocks of recombinant adenoassociated viruses: normal integration does not require viral gene expression. J Virol 1989; 63: 3822–8
Grimm D, Kern A, Rittner K, et al. Novel tools for production and purification of recombinant adenoassociated virus vectors. Hum Gene Ther 1998; 9: 2745–60
Xiao X, Li J, Samulski RJ. Production of high-titer recombinant adenoassociated virus vectors in the absence of helper adenovirus. J Virol 1998; 72: 2224–32
Kay MA, Manno CS, Ragni MV, et al. Evidence for gene transfer and expression of factor IX in haemophilia B patients treated with an AAV vector. Nat Genet 2000; 24: 257–61
Manno CS, Chew AJ, Hutchison S, et al. AAV-mediated factor IX gene transfer to skeletal muscle in patients with severe hemophilia B. Blood 2003; 101: 2963–72
Manno CS, Pierce GF, Arruda VR, et al. Successful transduction of liver in hemophilia by AAV-Factor IX and limitations imposed by the host immune response. Nat Med 2006; 12: 342–7
Epstein AL. Progress and prospects: biological properties and technological advances of herpes simplex virus type 1-based amplicon vectors. Gene Ther 2009; 16: 709–15
Manservigi R, Argnani R, Marconi P. HSV recombinant vectors for gene therapy. Open Virol J 2010; 4: 123–56
Burton EA, Bai Q, Goins WF, et al. Replication-defective genomic herpes simplex vectors: design and production. Curr Opin Biotechnol 2002; 13: 424–8
Friedman GK, Pressey JG, Reddy AT, et al. Herpes simplex virus oncolytic therapy for pediatric malignancies. Mol Ther 2009; 17: 1125–35
Shah AC, Benos D, Gillespie GY, et al. Oncolytic viruses: clinical applications as vectors for the treatment of malignant gliomas. J Neurooncol 2003; 65: 203–26
Glorioso JC, Fink DJ. Herpes vector-mediated gene transfer in the treatment of chronic pain. Mol Ther 2009; 17: 13–8
Goss JR, Gold MS, Glorioso JC. HSV vector-mediated modification of primary nociceptor afferents: an approach to inhibit chronic pain. Gene Ther 2009; 16: 493–501
Lieber A, Steinwaerder DS, Carlson CA, et al. Integrating adenovirus-adenoassociated virus hybrid vectors devoid of all viral genes. J Virol 1999; 73: 9314–24
Recchia A, Parks RJ, Lamartina S, et al. Site-specific integration mediated by a hybrid adenovirus/adeno-associated virus vector. Proc Natl Acad Sci U S A 1999; 96: 2615–20
Oehmig A, Fraefel C, Breakefield XO, et al. Herpes simplex virus type 1 amplicons and their hybrid virus partners, EBV, AAV, and retrovirus. Curr Gene Ther 2004; 4: 385–408
Fisher KD, Stallwood Y, Green NK, et al. Polymer-coated adenovirus permits efficient retargeting and evades neutralising antibodies. Gene Ther 2001; 8: 341–8
Avery OT, MacLeod CM, McCarty M. Studies on the chemical nature of the substance inducing transformation of pneumococcal types: inductions of transformation by a deoxyribonucleic acid fraction isolated from pneumococcus type III. J Exp Med 1979; 149: 297–326
Graham FL, van der Eb AJ. Transformation of rat cells by DNA of human adenovirus 5. Virology 1973; 54: 536–9
Pathak A, Patnaik S, Gupta Kailash C. Recent trends in non-viral vectormediated gene delivery. Biotechnol J 2009; 4: 1559–72 81._Mintzer MA, Simanek EE. Nonviral vectors for gene delivery. Chem Rev 2009; 109: 259–302 82._Bangham AD, Standish MM, Watkins JC. Diffusion of univalent ions across the lamellae of swollen phospholipids. J Mol Biol 1965; 13: 238–52
Mintzer MA, Simanek EE. Nonviral vectors for gene delivery. Chem Rev 2009; 109: 259–302
Bangham AD, Standish MM, Watkins JC. Diffusion of univalent ions across the lamellae of swollen phospholipids. J Mol Biol 1965; 13: 238–52
Felgner PL, Gadek TR, Holm M, et al. Lipofection: a highly efficient, lipidmediated DNA-transfection procedure. Proc Natl Acad Sci U S A 1987; 84: 7413–7
Simoes S, Filipe A, Faneca H, et al. Cationic liposomes for gene delivery. Expert Opin Drug Deliv 2005; 2: 237–54
Liu D, Ren T, Gao X. Cationic transfection lipids. Curr Med Chem 2003; 10: 1307–15
Montier T, Benvegnu T, Jaffres PA, et al. Progress in cationic lipid-mediated gene transfection: a series of bio-inspired lipids as an example. Curr Gene Ther 2008; 8: 296–312
Zhou X, Huang L. DNA transfection mediated by cationic liposomes containing lipopolylysine: characterization and mechanism of action. Biochim Biophys Acta 1994; 1189: 195–203
Xu L, Huang CC, Huang W, et al. Systemic tumor-targeted gene delivery by anti-transferrin receptor scFv-immunoliposomes. Mol Cancer Ther 2002; 1: 337–46
Pardridge WM. Re-engineering biopharmaceuticals for delivery to brain with molecular Trojan horses. Bioconjug Chem 2008; 19: 1327–38
Durcan N, Murphy C, Cryan SA. Inhalable siRNA: potential as a therapeutic agent in the lungs. Mol Pharm 2008; 5: 559–66
Stopeck AT, Hersh EM, Akporiaye ET, et al. Phase I study of direct gene transfer of an allogeneic histocompatibility antigen, HLA-B7, in patients with metastatic melanoma. J Clin Oncol 1997; 15: 341–9
Stopeck AT, Jones A, Hersh EM, et al. Phase II study of direct intralesional gene transfer of allovectin-7, an HLA-B7/beta2-microglobulin DNAliposome complex, in patients with metastatic melanoma. Clin Cancer Res 2001; 7: 2285–91
Boussif O, Lezoualc’h F, Zanta MA, et al. A versatile vector for gene and oligonucleotide transfer into cells in culture and in vivo: polyethylenimine. Proc Natl Acad Sci U S A 1995; 92: 7297–301
Goula D, Remy JS, Erbacher P, et al. Size, diffusibility and transfection performance of linear PEI/DNA complexes in the mouse central nervous system. Gene Ther 1998; 5: 712–7
Chemin I, Moradpour D, Wieland S, et al. Liver-directed gene transfer: a linear polyethlenimine derivative mediates highly efficient DNA delivery to primary hepatocytes in vitro and in vivo. J Viral Hepat 1998; 5: 369–75
Haensler J, Szoka FC J. Polyamidoamine cascade polymers mediate efficient transfection of cells in culture. Bioconjug Chem 1993; 4: 372–9
Tang MX, Redemann CT, Szoka FC J. In vitro gene delivery by degraded polyamidoamine dendrimers. Bioconjug Chem 1996; 7: 703–14
Rudolph C, Lausier J, Naundorf S, et al. In vivo gene delivery to the lung using polyethylenimine and fractured polyamidoamine dendrimers. J Gene Med 2000; 2: 269–78
Nimesh S, Kumar R, Chandra R. Novel polyallylamine-dextran sulfate-DNA nanoplexes: highly efficient non-viral vector for gene delivery. Int J Pharm 2006; 320: 143–9
Erbacher P, Zou S, Bettinger T, et al. Chitosan-based vector/DNA complexes for gene delivery: biophysical characteristics and transfection ability. Pharm Res 1998; 15: 1332–9
Schatzlein AG, Zinselmeyer BH, Elouzi A, et al. Preferential liver gene expression with polypropylenimine dendrimers. J Control Release 2005; 101: 247–58
Balicki D, Beutler E. Histone H2A significantly enhances in vitro DNA transfection. Mol Med 1997; 3: 782–7
Balicki D, Putnam CD, Scaria PV, et al. Structure and function correlation in histoneH2A peptide-mediated gene transfer. Proc Natl Acad Sci U S A 2002; 99: 7467–71
Sweeney P, Karashima T, Ishikura H, et al. Efficient therapeutic gene delivery after systemic administration of a novel polyethylenimine/DNA vector in an orthotopic bladder cancer model. Cancer Res 2003; 63: 4017–20
Konstan MW, Davis PB, Wagener JS, et al. Compacted DNA nanoparticles administered to the nasal mucosa of cystic fibrosis subjects are safe and demonstrate partial to complete cystic fibrosis transmembrane regulator reconstitution. Hum Gene Ther 2004; 15: 1255–69
Avrameas A, Ternynck T, Nato F, et al. Polyreactive anti-DNA monoclonal antibodies and a derived peptide as vectors for the intracytoplasmic and intranuclear translocation of macromolecules. Proc Natl Acad Sci U S A 1998; 95: 5601–6
Lee RJ, Huang L. Folate-targeted, anionic liposome-entrapped polylysinecondensedDNAfor tumor cell-specific gene transfer. J Biol Chem 1996; 271: 8481–7
Sorgi FL, Bhattacharya S, Huang L. Protamine sulfate enhances lipidmediated gene transfer. Gene Ther 1997; 4: 961–8
Lee LK, Williams CL, Devore D, et al. Poly(propylacrylic acid) enhances cationic lipid-mediated delivery of antisense oligonucleotides. Biomacromolecules 2006; 7: 1502–8
Murphy EA, Waring AJ, Haynes SM, et al. Compaction of DNA in an anionic micelle environment followed by assembly into phosphatidylcholine liposomes. Nucleic Acids Res 2000; 28: 2986–92
Li S, Huang L. In vivo gene transfer via intravenous administration of cationic lipid-protamine-DNA (LPD) complexes. Gene Ther 1997; 4: 891–900
Wolff JA, Malone RW, Williams P, et al. Direct gene transfer into mouse muscle in vivo. Science 1990; 247: 1465–8
Choate KA, Khavari PA. Direct cutaneous gene delivery in a human genetic skin disease. Hum Gene Ther 1997; 8: 1659–65
Park SW, Gwon HC, Jeong JO, et al. Intracardiac echocardiographic guidance and monitoring during percutaneous endomyocardial gene injection in porcine heart. Hum Gene Ther 2001; 12: 893–903
Hickman MA, Malone RW, Lehmann-Bruinsma K, et al. Gene expression following direct injection of DNA into liver. Hum Gene Ther 1994; 5: 1477–83
Habib NA, Ding SF, el-Masry R, et al. Preliminary report: the short-term effects of direct p53 DNA injection in primary hepatocellular carcinomas. Cancer Detect Prev 1996; 20: 103–7
Prausnitz MR, Mikszta JA, Cormier M, et al. Microneedle-based vaccines. Curr Top Microbiol Immunol 2009; 333: 369–93
Hartikka J, Sawdey M, Cornefert Jensen F, et al. An improved plasmid DNA expression vector for direct injection into skeletal muscle. Hum Gene Ther 1996; 7: 1205–17
Klein RM, Wolf ED, Wu R, et al. High-velocity microprojectiles for delivering nucleic acids into living cells: 1987. Biotechnology 1992; 24: 384–6
O’Brien J, Lummis SC. An improved method of preparing microcarriers for biolistic transfection. Brain Res Brain Res Protoc 2002; 10: 12–5
Yang NS, Burkholder J, Roberts B, et al. In vivo and in vitro gene transfer to mammalian somatic cells by particle bombardment. Proc Natl Acad Sci U S A 1990; 87: 9568–72
Wang S, Joshi S, Lu S. Delivery of DNA to skin by particle bombardment. Methods Mol Biol 2004; 245: 185–96
Kim D, Hoory T, Monie A, et al. Enhancement of DNA vaccine potency through coadministration of CIITA DNA with DNA vaccines via gene gun. J Immunol 2008; 180: 7019–27
Roberts LK, Barr LJ, Fuller DH, et al. Clinical safety and efficacy of a powdered hepatitis B nucleic acid vaccine delivered to the epidermis by a commercial prototype device. Vaccine 2005; 23: 4867–78
Drape RJ, Macklin MD, Barr LJ, et al. Epidermal DNA vaccine for influenza is immunogenic in humans. Vaccine 2006; 24: 4475–81
Cassaday RD, Sondel PM, King DM, et al. A phase I study of immunization using particle-mediated epidermal delivery of genes for gp100 and GM-CSF into uninvolved skin of melanoma patients. Clin Cancer Res 2007; 13: 540–9
Yager EJ, Dean HJ, Fuller DH. Prospects for developing an effective particlemediated DNA vaccine against influenza. Expert Rev Vaccines 2009; 8: 1205–20
Kaur T, Slavcev RA, Wettig SD. Addressing the challenge: current and future directions in ovarian cancer therapy. Curr Gene Ther 2009; 9: 434–58
Neumann E, Schaefer-Ridder M, Wang Y, et al. Gene transfer into mouse lyoma cells by electroporation in high electric fields. EMBO J 1982; 1: 841–5
Favard C, Dean DS, RolsM-P. Electrotransfer as a nonviral method of gene delivery. Curr Gene Ther 2007; 7: 67–77
Heller LC, Ugen K, Heller R. Electroporation for targeted gene transfer. Expert Opin Drug Deliv 2005; 2: 255–68
van Drunen Littel-van den Hurk S, Hannaman D. Electroporation for DNA immunization: clinical application. Expert Rev Vaccines 2010; 9: 503–17
Wells DJ. Gene therapy progress and prospects: electroporation and other physical methods. Gene Ther 2004; 11: 1363–9
Heller R, Jaroszeski MJ, Glass LF, et al. Phase I/II trial for the treatment of cutaneous and subcutaneous tumors using electrochemotherapy. Cancer 1996; 77: 964–71
Bodles-Brakhop AM, Heller R, Draghia-Akli R. Electroporation for the delivery of DNA-based vaccines and immunotherapeutics: current clinical developments. Mol Ther 2009; 17: 585–92
Kim HJ, Greenleaf JF, Kinnick RR, et al. Ultrasound-mediated transfection of mammalian cells. Hum Gene Ther 1996; 7: 1339–46
Tata DB, Dunn F, Tindall DJ. Selective clinical ultrasound signals mediate differential gene transfer and expression in two human prostate cancer cell lines: LnCap and PC-3. Biochem Biophys Res Commun 1997; 234: 64–7
Bao S, Thrall BD, Gies RA, et al. In vivo transfection of melanoma cells by lithotripter shock waves. Cancer Res 1998; 58: 219–21
Huber PE, Jenne J, Debus J, et al. Acomparison of shockwave and sinusoidalfocused ultrasound-induced localized transfection of HeLa cells. Ultrasound Med Biol 1999; 25: 1451–7
Sonoda S, Tachibana K, Uchino E, et al. Gene transfer to corneal epithelium and keratocytes mediated by ultrasound with microbubbles. Invest Ophthalmol Vis Sci 2006; 47: 558–64
Hynynen K, McDannold N, Martin H, et al. The threshold for brain damage in rabbits induced by bursts of ultrasound in the presence of an ultrasound contrast agent (Optison). Ultrasound Med Biol 2003; 29: 473–81
Manome Y, Nakayama N, Nakayama K, et al. Insonation facilitates plasmid DNA transfection into the central nervous system and microbubbles enhance the effect. Ultrasound Med Biol 2005; 31: 693–702
Shimamura M, Sato N, Taniyama Y, et al. Development of efficient plasmid DNA transfer into adult rat central nervous system using microbubbleenhanced ultrasound. Gene Ther 2004; 11: 1532–9
Shimamura M, Sato N, Taniyama Y, et al. Gene transfer into adult rat spinal cord using naked plasmid DNA and ultrasound microbubbles. J Gene Med 2005; 7: 1468–74
Sheyn D, Kimelman-Bleich N, Pelled G, et al. Ultrasound-based nonviral gene delivery induces bone formation in vivo. Gene Ther 2007; 15: 257–66
Guo H, Leung JCK, Chan LYY, et al. Ultrasound-contrast agent mediated naked gene delivery in the peritoneal cavity of adult rat. Gene Ther 2007; 14: 1712–20
Hou C-C, Wang W, Huang XR, et al. Ultrasound-microbubble-mediated gene transfer of inducible Smad7 blocks transforming growth factor-beta signaling and fibrosis in rat remnant kidney. Am J Pathol 2005; 166: 761–71
Chen S, Ding J-H, Bekeredjian R, et al. Efficient gene delivery to pancreatic islets with ultrasonic microbubble destruction technology. Proc Natl Acad Sci U S A 2006; 103: 8469–74
Shen ZP, Brayman AA, Chen L, et al. Ultrasound with microbubbles enhances gene expression of plasmid DNA in the liver via intraportal delivery. Gene Ther 2008; 15: 1147–55
Miao CH, Brayman AA, Loeb KR, et al. Ultrasound enhances gene delivery of human factor IX plasmid. Hum Gene Ther 2005; 16: 893–905
Ohta S, Suzuki K, Tachibana K, et al. Microbubble-enhanced sonoporation: efficient gene transduction technique for chick embryos. Genesis 2003; 37: 91–101
Nakashima M, Tachibana K, Iohara K, et al. Induction of reparative dentin formation by ultrasound-mediated gene delivery of growth/differentiation factor 11. Hum Gene Ther 2003; 14: 591–7
Taniyama Y, Tachibana K, Hiraoka K, et al. Development of safe and efficient novel nonviral gene transfer using ultrasound: enhancement of transfection efficiency of naked plasmidDNAin skeletal muscle. Gene Ther 2002; 9: 372–80
Lu QL, Liang H-D, Partridge T, et al. Microbubble ultrasound improves the efficiency of gene transduction in skeletal muscle in vivo with reduced tissue damage. Gene Ther 2003; 10: 396–405
Bekeredjian R, Chen S, Frenkel PA, et al. Ultrasound-targeted microbubble destruction can repeatedly direct highly specific plasmid expression to the heart. Circulation 2003; 108: 1022–6
Bekeredjian R, Grayburn PA, Shohet RV. Use of ultrasound contrast agents for gene or drug delivery in cardiovascular medicine. J Am Coll Cardiol 2005; 45: 329–35
Suzuki R, Takizawa T, Negishi Y, et al. Tumor specific ultrasound enhanced gene transfer in vivo with novel liposomal bubbles. J Control Release 2008; 125: 137–44
Hayashi S, Mizuno M, Yoshida J, et al. Effect of sonoporation on cationic liposome-mediated IFNbeta gene therapy for metastatic hepatic tumors of murine colon cancer. Cancer Gene Ther 2009; 16: 638–43
Suzuki R, Namai E, Oda Y, et al. Cancer gene therapy by IL-12 gene delivery using liposomal bubbles and tumoral ultrasound exposure. J Control Release 2010; 142: 245–50
Barreiro O, Aguilar Rio J, Tejera E, et al. Specific targeting of human inflamed endothelium and in situ vascular tissue transfection by the use of ultrasound contrast agents. JACC Cardiovasc Imaging 2009; 2: 997–1005
Kodama T, Aoi A, Watanabe Y, et al. Evaluation of transfection efficiency in skeletal muscle using nano/microbubbles and ultrasound. Ultrasound Med Biol 2010; 36: 1196–205
Zeira E, Manevitch A, Khatchatouriants A, et al. Femtosecond infrared laseran efficient and safe in vivo gene delivery system for prolonged expression. Mol Ther 2003; 8: 342–50
Chakravarty P, Qian W, El-Sayed MA, et al. Delivery of molecules into cells using carbon nanoparticles activated by femtosecond laser pulses. Nat Nanotechnol 2010; 5: 607–11
Plank C, Anton M, Rudolph C, et al. Enhancing and targeting nucleic acid delivery by magnetic force. Expert Opin Biol Ther 2003; 3: 745–58
Dobson J. Gene therapy progress and prospects:magnetic nanoparticle-based gene delivery. Gene Ther 2006; 13: 283–7
Mykhaylyk O, Antequera YS, Vlaskou D, et al. Generation of magnetic nonviral gene transfer agents and magnetofection in vitro. Nat Protoc 2007; 2: 2391–411
Scherer F, Anton M, Schillinger U, et al. Magnetofection: enhancing and targeting gene delivery by magnetic force in vitro and in vivo. Gene Ther 2002; 9: 102–9
Liu F, Song Y, Liu D. Hydrodynamics-based transfection in animals by systemic administration of plasmid DNA. Gene Ther 1999; 6: 1258–66
Zhang G, Budker V, Wolff JA. High levels of foreign gene expression in hepatocytes after tail vein injections of naked plasmid DNA. Hum Gene Ther 1999; 10: 1735–7
Zhang G, Gao X, Song YK, et al. Hydroporation as the mechanism of hydrodynamic delivery. Gene Ther 2004; 11: 675–82
Suda T, Liu D. Hydrodynamic gene delivery: its principles and applications. Mol Ther 2007; 15: 2063–9
Brunetti-Pierri N, Stapleton GE, Palmer DJ, et al. Pseudo-hydrodynamic delivery of helper-dependent adenoviral vectors into non-human primates for liver-directed gene therapy. Mol Ther 2007; 15: 732–40
Brunetti-Pierri N, Palmer DJ, Mane V, et al. Increased hepatic transduction with reduced systemic dissemination and proinflammatory cytokines following hydrodynamic injection of helper-dependent adenoviral vectors. Mol Ther 2005; 12: 99–106
Condiotti R, Curran MA, Nolan GP, et al. Prolonged liver-specific transgene expression by a non-primate lentiviral vector. Biochem Biophys Res Commun 2004; 320: 998–1006
Arad U, Zeira E, El-Latif MA, et al. Liver-targeted gene therapy by SV40- based vectors using the hydrodynamic injection method. Hum Gene Ther 2005; 16: 361–71
Herweijer H, Wolff JA. Gene therapy progress and prospects: hydrodynamic gene delivery. Gene Ther 2007; 14: 99–107
Qiao C, Li J, Zheng H, et al. Hydrodynamic limb vein injection of adenoassociated virus serotype 8 vector carrying caninemyostatin propeptide gene into normal dogs enhances muscle growth. Hum Gene Ther 2009; 20: 1–10
Chen L, Zhu F, Li J, et al. The enhancing effects of the light chain on heavy chain secretion in split delivery of factor VIII gene. Mol Ther 2007; 15: 1856–62
Doenecke A, Kromer A, Scherer MN, et al. AAV plasmid DNA simplifies liver-directed in vivo gene therapy: comparison of expression levels after plasmid DNA-, adeno-associated virus- and adenovirus-mediated liver transfection. J Gene Med 2010; 12: 810–7
Suda T, Kamimura K, Kubota T, et al. Progress toward liver-based gene therapy. Hepatol Res 2009; 39: 325–40
Eastman SJ, Baskin KM, Hodges BL, et al. Development of catheter-based procedures for transducing the isolated rabbit liver with plasmid DNA. Hum Gene Ther 2002; 13: 2065–77
Yoshino H, Hashizume K, Kobayashi E. Naked plasmidDNA transfer to the porcine liver using rapid injection with large volume. Gene Ther 2006; 13: 1696–702
Alino SF, Herrero MJ, Noguera I, et al. Pig liver gene therapy by noninvasive interventionist catheterism. Gene Ther 2007; 14: 334–43
Fabre JW, Grehan A, Whitehorne M, et al. Hydrodynamic gene delivery to the pig liver via an isolated segment of the inferior vena cava. Gene Ther 2008; 15: 452–62
Suda T, Suda K, Liu D. Computer-assisted hydrodynamic gene delivery. Mol Ther 2008; 16: 1098–104
Kamimura K, Suda T, Xu W, et al. Image-guided, lobe-specific hydrodynamic gene delivery to swine liver. Mol Ther 2009; 17: 491–9
Kamimura K, Guisheng Z, Liu D. Image-guided, intravascular hydrodynamic gene delivery to skeletal muscle in pigs. Mol Ther 2010; 18: 93–100
The Journal of Gene Medicine. Gene therapy clinical trials worldwide [online]. Available from URL: http://www.wiley.com/legacy/wileychi/genmed/clinical/ [Accessed 2011 Aug 2]
Marshall E. Gene therapy death prompts review of adenovirus vector. Science 1999; 286: 2244–5
Check E. Second cancer case halts gene-therapy trials. Nature 2003; 421: 305
Acknowledgements
The research in the authors’ laboratory has been supported in part by grant support from the National Institutes of Health (EB002946, EB007357 and HL075542) to D. Liu, and from the Japanese Society for the Promotion of Sciences (22890064 and 23790595) and the Tsukada Grant for the Niigata University Medical Research to K. Kamimura. The authors would like to thank Professor Balwant N. Dixit for the critical reading and English editing. The authors have no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kamimura, K., Suda, T., Zhang, G. et al. Advances in Gene Delivery Systems. Pharm Med 25, 293–306 (2011). https://doi.org/10.1007/BF03256872
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03256872