Abstract
Objectives
This study investigated associations between three types of child maltreatment (exposure to intimate partner violence, sexual, and physical abuse) and multimorbidity (chronic physical conditions, pain conditions, and mental disorders) in adults.
Methods
Multinomial logistic regression was used to analyze weighted data from the 2012 Canadian Community Health Survey (CCHS - MH 2012), a representative population sample (N = 23,846) of respondents ages 18+.
Results
All three subtypes of child maltreatment independently predicted increased odds of experiencing multimorbidity as an adult, while adjusting for covariates (adjusted odds ratios ranged from 1.34 (95% CI = 1.00, 1.80) to 4.87 (95% CI = 2.75, 8.63)). A dose-response relationship between the number of child maltreatment subtypes and risk for multimorbidity was also observed (adjusted odds ratios ranged from 1.38 (95% CI = 1.11, 1.73) to 10.96 (95% CI = 6.12, 19.64)).
Conclusion
The current results highlight the importance of considering a range of childhood adversities and suggest that public health approaches that aim to decrease the prevalence and severity of child maltreatment have the potential to ameliorate adult multimorbidities. Future research is encouraged to investigate these issues using longitudinal population-level data.
Résumé
Objectifs
Examiner les associations entre trois types de maltraitance des enfants (exposition à la violence envers la ou le partenaire intime, violence sexuelle et violence physique) et la multimorbidité (douleurs, troubles mentaux et troubles physiques chroniques) à l’âge adulte.
Méthode
Nous avons employé la régression logistique multinomiale pour analyser les données pondérées de l’Enquête sur la santé dans les collectivités canadiennes de 2012 (ESCC - Santé mentale 2012), une population-échantillon représentative (N = 23 846) de répondants de 18 ans et plus.
Résultats
Les trois sous-types de maltraitance des enfants ont prédit indépendamment des probabilités accrues de multimorbidité à l’âge adulte en tenant compte des covariables (les rapports de cotes ajustés allaient de 1,34 [IC de 95% = 1,00, 1,80] à 4,87 [IC de 95% = 2,75, 8,63]). Une relation dose-réponse a aussi été observée entre le nombre de sous-types de maltraitance des enfants et le risque de multimorbidité (les rapports de cotes ajustés allaient de 1,38 [IC de 95% = 1,11, 1,73] à 10,96 [IC de 95% = 6,12, 19,64]).
Conclusion
Ces résultats font ressortir l’importance de tenir compte d’une gamme d’épreuves pouvant être vécues par les enfants et indiquent que des démarches de santé publique qui visent à réduire la prévalence et la gravité de la maltraitance des enfants pourraient améliorer la multimorbidité chez les adultes. Nous encourageons l’étude de ces questions à l’aide de données populationnelles longitudinales.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The World Health Organization recognizes multimorbidity as one of the major medical challenges of the twenty-first century (World Health Organization 2008). Multimorbidity is defined as the co-occurrence of two or more chronic health conditions within the same patient (Richardson et al. 2014). Understanding the epidemiology of multimorbidity is important, as two or more co-occurring chronic conditions affect clinical diagnosis, treatment strategy, and quality of life (Richardson et al. 2014). There is significant overlap between physical conditions and mental disorders, with North American prevalence estimates for the co-occurrence of chronic physical conditions and mental disorders ranging from 3% to 17% (Schmitz et al. 2007; Egede 2007). Multimorbidity, particularly in the context of co-occurring physical and mental health problems, can confer significant impairment, as their co-occurrence leads to increased healthcare resource utilization, greater functional disability, and poorer prognosis (Richardson et al. 2014; Egede 2007). Investigating multiple chronic conditions can be difficult when attempting to identify general disease clusters, as these tend to evade diagnostic categorization within traditional “somatic” and “mental health” domains; multimorbidity often violates this dichotomy (Tomasdottir et al. 2014; Tomasdottir et al. 2015). Furthermore, despite shared risk factors, mental disorders and physical conditions continue to be conceptualized and investigated separately (Richardson et al. 2014). This is problematic, as assessment and treatment of individual conditions continue to dominate healthcare delivery, thereby creating medical “silo” thinking (Tomasdottir et al. 2014, Tomasdottir et al. 2015).
Recognized risk factors for multimorbidity include health-harming behaviours (e.g., smoking, substance abuse, inactivity), socioeconomic deprivation, and older age (i.e., 65+ years) (Bellis et al. 2014; Ording and Henrik Toft Sørensen 2013). In addition, childhood maltreatment, which includes exposure to various forms of abuse and neglect, has been identified as a key risk indicator for adult morbidity and mortality disparities (Bellis et al. 2014; Brown et al. 2009). Childhood history of abuse increases the likelihood of engaging in health-harming behaviours (Bellis et al. 2014; Anda et al. 2006) and increases risk for both chronic physical conditions (Afifi et al. 2016; Springer et al. 2007) and mental disorders (Springer et al. 2007). Previous work has shown that childhood adversity not only is associated with increased risk of multimorbidity (Bellis et al. 2014; Gonzalez et al. 2012), but may also display a dose-response relationship, such that there is a rise in prevalence of both individual conditions as well as multimorbid diseases with increasing levels of childhood adversity (Tomasdottir et al. 2015). However, relatively few studies have examined associations between child maltreatment and adult multimorbidity using nationally representative data across the lifespan (Bellis et al. 2014). To the best of our knowledge, no prior work has delineated between subtypes of maltreatment, with the inclusion of childhood exposure to intimate partner violence as a distinct category, in their examination of childhood experiences and adult multimorbidity.
To address these gaps, this study examines associations between multiple subtypes of child maltreatment, with the novel inclusion of childhood exposure to intimate partner violence, and adult multimorbidity using data from the 2012 Canadian Community Health Survey - Mental Health (CCHS - MH 2012), a representative population sample. Previous investigations utilizing an earlier version and concurrent version of this dataset have shown that experiences of child maltreatment are associated with increased risk for heart disease (Fuller-Thomson et al. 2010), chronic physical conditions (i.e., diabetes, respiratory disease, etc.) (Afifi et al. 2016), and mental health disorders (i.e., depression, bipolar disorder, etc.) (Afifi et al. 2014). In line with recent recommendations to measure multimorbidity across a range of health domains (Richardson et al. 2014; Barnett et al. 2012), the current project adopts a comprehensive approach. We separate chronic medical conditions into three broad categories for analyses: mental disorders (e.g., depression, anxiety disorders), pain conditions (e.g., arthritis, back problems, migraines), and other physical conditions (e.g., cardiovascular disease, diabetes, respiratory disease). These distinctions were made as the prevalence of certain health conditions is expected to vary based on age of the sample, and prior research has shown that pain conditions are more strongly associated with mental disorders like depression and anxiety (Scott et al. 2007). The main objective of the current study was to examine the impact of multiple forms of maltreatment on multimorbidity across a range of health domains in a Canadian national sample. Additional analyses explore the influence of covariates such as age, sex, health-harming behaviours, and sociodemographic variables on these relationships. This study is an important extension, as retrospective examination of childhood experiences on adult health outcomes can provide a rapid and informative approach to identify the impact of child maltreatment on public health and healthcare systems.
Methods
Sample
Data come from the 2012 Canadian Community Health Survey - Mental Health (CCHS - MH 2012), in which a multi-stage stratified cluster sampling design was employed to obtain a representative sample of respondents aged 15+ from the 10 Canadian provinces (Statistics Canada 2013). Respondents completed the survey on a voluntary basis. The national household rate (79.8%) and individual-level response rate (68.9%) yielded a sample of 25,113 individuals. The sampling frame excluded people living on reserves and other Indigenous communities, full-time members of the Canadian Forces, and institutionalized populations (altogether < 3% of the Canadian population). Due to the sensitive nature of child maltreatment questions, they were administered only to respondents aged 18+ (N = 23,846).
Measures
Child maltreatment
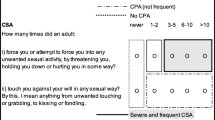
Respondents were asked about maltreatment experiences prior to the age of 16 that occurred at school, in their neighbourhood, or in the family. Respondents were assessed for childhood exposure to physical abuse and intimate partner violence using items from the Childhood Experiences of Violence Questionnaire (CEVQ) (Walsh et al. 2008), and exposure to sexual abuse using items based on a previous survey administered by Statistics Canada (Statistics Canada 2013). Responses were dichotomized for each maltreatment subtype (present/absent) following guidelines from the CEVQ (Walsh et al. 2008) and using approaches similar to prior CCHS - MH 2012 analyses (Afifi et al. 2014, 2016). Childhood sexual abuse was classified as present if a respondent indicated experiencing one of the following criteria by an adult on at least one occasion: (1) being forced, or any attempt of being forced, into unwanted sexual activity by threat, physical restraint, or harm; or (2) any unwanted sexual touching against their will. Childhood physical abuse was classified as present if a respondent indicated experiencing at least one of the following criteria by an adult: (1) being slapped on the face or head, spanked, or hit with something hard on three or more occasions; (2) being pushed, grabbed, shoved, or having something thrown at them on three or more occasions; or (3) being kicked, bit, punched, choked, burned, or physically attacked on at least one occasion. Childhood exposure to intimate partner violence was classified as present if a respondent indicated seeing or hearing parents, step-parents, or any guardian hitting each other or another adult in the home on three or more occasions.
Chronic physical and pain conditions
Respondents were assessed for 12 different chronic conditions through a group of questions pertaining to long-term health. Respondents were classified as having a chronic condition if they indicated they were diagnosed by a health professional with a chronic condition that had lasted (or was expected to last) at least 6 months. These individual chronic conditions were separated into two broad categories for analysis: physical conditions (i.e., asthma, arthritis, high blood pressure, diabetes, epilepsy, heart disease, cancer, stroke, bowel disease, chronic fatigue syndrome) and pain conditions (i.e., back pain, migraine headaches).
Mental disorders
Respondents were assessed for diagnoses of Axis I disorders using the World Mental Health version of the Composite International Diagnostic Interview (WMH-CIDI) of the World Health Organization (WHO) (Statistics Canada 2013) and based on criteria of the 4th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) (American Psychological Association 2000). Specific mental disorders assessed included major depressive episode, bipolar (I and II) disorder, generalized anxiety disorder, alcohol abuse/dependence, cannabis abuse/dependence, and other drug abuse/dependence. Respondents were classified as having a mental disorder if they met criteria for any 1 or more of these disorders within the last 12 months.
Derived variable: multimorbid condition clusters
There were eight derived clusters: (i) no conditions (reference group), (ii) mental disorder only, (iii) chronic pain condition only, (iv) chronic physical condition only, (v) chronic mental health and pain condition, (vi) chronic mental health and physical condition, (vii) chronic pain and physical condition, and (viii) all three types of conditions.
Sociodemographic covariates and risk factors
Relevant sociodemographic characteristics (i.e., sex, age, country of birth, visible minority status, education, income level, and marital status) and other risk factors (i.e., smoking status, body mass index) for the development of chronic diseases were evaluated.
Data analysis
Using STATA 14, multinomial logistic regressions examined relationships between child maltreatment and multimorbidity, while adjusting for covariates (adjusted odds ratios (AOR)). All analyses completed compared respondents reporting exposure to maltreatment to those who did not report such experiences. Regressions were run based on dichotomized variables for the subtypes of child maltreatment, as well as a model exploring the dose-response relationship between the number of child maltreatment types and multimorbidity. Weights created by Statistics Canada were used in the analysis to adjust for non-response and maintain representativeness with the Canadian population.
Missing data
Data were missing from approximately 3% of the sample. Data were determined to be missing at random and multiple imputations in STATA 14 were used to impute missing values. The Multiple Imputation by Chained Equations command was utilized to impute 10 separate datasets which were then used in regression models to produce estimated values.
Results
Maltreatment and multimorbidity prevalence
Data on the prevalence of child maltreatment in Canada by subtype and sociodemographic variables from the CCHS - MH 2012 (N = 23,846) have been previously published. The prevalence of any childhood maltreatment was 32.1% (n = 7700), with childhood physical abuse being the most common (26.1%, n = 6070), followed by childhood sexual abuse (10.1%, n = 2760), and then by childhood exposure to intimate partner violence (7.9%, n = 1900) (Afifi et al. 2014). Females were more likely than males to have experienced child sexual abuse (14.4% vs. 5.8%, p < 0.05) and been exposed to intimate partner violence (8.9% vs. 6.9%, p < 0.05), and males were more likely than females to have experienced child physical abuse (31.0% vs. 21.3%, p < 0.05) and any child abuse (34.0% vs. 30.3%, p < 0.05) (Afifi et al. 2014).
Based on the data analyzed in the current study, in terms of overall health, nearly half of the sample (41.9%, n = 10,207; reference group) reported no conditions. With respect to the derived condition clusters, 4.0% (n = 903) reported a mental disorder, 8.4% (n = 1920) reported a pain condition, 26.7% (n = 6097) reported a physical condition, 1.4% (n = 327) reported a multimorbid mental disorder and pain condition, 2.0% (n = 459) reported a multimorbid mental disorder and physical condition, 13.1% (n = 3031) reported a multimorbid pain and physical condition, and 2.5% (n = 583) reported all three types of multimorbid conditions. There was variation in reports of overall health based on respondents’ exposure to child maltreatment, and prevalence estimates of the derived condition clusters in regard to history of child maltreatment outcomes are delineated in Table 1. Post hoc models examined whether associations between the subtypes of child maltreatment and adult multimorbidity were moderated by sex or age. No significant interactions were found (not shown).
Childhood exposure to physical abuse and multimorbidity
All effects reported herein are adjusted for covariates (e.g., age, sex, and sociodemographic variables). Compared to respondents not reporting exposure to CPA, exposure to CPA was significantly associated with increased odds of all the derived condition clusters, with the exception of physical conditions (Table 2). Among respondents reporting CPA, the likelihood of developing mental disorders as a singular morbidity or a multimorbid condition with another chronic condition was two to three times higher (AORs from 2.40 to 3.78). Respondents reporting CPA also had odds three times higher of developing multimorbidity of all three types of conditions (AOR = 3.57, 95% CI = 2.75, 4.64). The effects of risk factors and sociodemographic characteristics on multimorbidity were similar across models (Tables 2, 3, 4, and 5).
Childhood exposure to sexual abuse and multimorbidity
Compared to respondents not reporting to CSA, exposure to CSA was significantly associated with increased onset of all the derived condition clusters, except for physical conditions (Table 3). Respondents reporting CSA had a higher risk of developing mental disorders, either as a single morbidity or multimorbid with other chronic conditions (AORs from 2.08 to 4.87). Furthermore, respondents reporting CSA were over four times more likely to develop multimorbid mental health and pain conditions (AOR = 4.87, 95% CI = 2.75, 8.63) and multimorbidity of all three types of conditions (AOR = 4.18, 95% CI = 3.06, 5.70).
Childhood exposure to intimate partner violence and multimorbidity
Similar to the other maltreatment subtypes, exposure CEIPV, compared to respondents not reporting CEIPV, was significantly associated with onset of the same six derived condition clusters (Table 4). Respondents reporting CEIPV had a two times greater risk of developing multiple chronic conditions, such as multimorbid mental health and pain/physical conditions (AORs from 2.03 to 2.37). Additionally, respondents reporting CEIPV were three times more likely to develop multimorbidity of all three types of conditions (AOR = 3.70, 95% CI = 2.67, 5.12).
Number of maltreatment subtypes and multimorbidity
There was a general trend of increasing number of child maltreatment subtypes experienced corresponding with greater odds of all the derived condition clusters, with the exception of physical conditions, thus indicating a dose-response relation (Table 5). For exposure to one subtype of maltreatment, AORs across multimorbid condition clusters ranged from 1.44 to 4.06, for exposure to two subtypes, AORs ranged from 2.41 to 6.66, and for exposure to all three subtypes, AORs ranged from 3.38 to 10.96. Thus, respondents exposed to all three subtypes of maltreatment were approximately 3–11 times more likely to experience various multimorbid conditions than respondents not exposed to child maltreatment.
Discussion
Compared to respondents without childhood maltreatment experiences, exposure to each maltreatment subtype was significantly associated with increased odds for mental disorders, chronic pain conditions, multimorbid mental health and pain/physical conditions, multimorbid pain and physical conditions, and all three types of conditions. These results are consistent with prior evidence linking history of child maltreatment with increased risk for chronic conditions (Afifi et al. 2016; Springer et al. 2007), mental disorders (Springer et al. 2007), and multimorbidity (Bellis et al. 2014; Gonzalez et al. 2012). To our knowledge, this is the first study to examine childhood exposure to intimate partner violence in addition to other forms of child maltreatment in regard to risk for adult multimorbidity. Although this subtype assessed childhood accounts of witnessing intimate partner violence, there were the same patterns of results for this subtype as for the other experiences of child abuse. This study delineated chronic conditions into physical health and pain disorders to provide evidence that these clusters are differentially associated with childhood maltreatment; such that significant associations arose for the subtypes and number of subtypes of maltreatment in terms of risk for pain conditions, but not in terms of risk for physical conditions. The development of chronic diseases involves a complex interplay between genetic factors, early life events, and chronological aging (Belsky et al. 2017), and not enough is currently known about how child maltreatment experiences may differentially incur risk for different chronic conditions. Future research is needed to investigate possible factors (e.g., pain sensitivity) (Fillingim and Edwards 2018) that may influence the relationships between childhood experiences and adult risk for chronic pain versus physical conditions. Furthermore, our finding that across maltreatment types, the greatest odds for multimorbidity were primarily between mental disorders and another chronic pain and/or physical condition, complements and extends prior international research showing that mental disorders are more prevalent in the general population with increasing numbers of chronic illnesses (Barnett et al. 2012; Moussavi et al. 2007).
Furthermore, our findings support the previously reported dose-response relationship between childhood trauma and disease prevalence, such that increasing levels of childhood adversity are associated with a rise in singular and multimorbid disease prevalence (Tomasdottir et al. 2015). In the current sample, when exposure to increasing number of maltreatment subtypes was taken into consideration, there was a dose-response relation observed for mental health conditions, multimorbid chronic physical/pain and mental health conditions, multimorbid chronic physical and pain conditions, and multimorbidity of all three types of conditions. In accordance with previous studies examining the dose-response association between disease prevalence and increasing childhood difficulties, steeper slopes were observed for multimorbid mental health problems and chronic physical/pain conditions (Tomasdottir et al. 2015; Gonzalez et al. 2012). With the novel finding in our study, the slope was steepest for multimorbidity of all three types of conditions. Beyond this, our study provides additional evidence that patterns of morbidity transcend the traditional “somatic’ and “mental health” domains, thus illustrating a fundamental conflict in the current biomedical definitions of risk, disease, and recovery (Tomasdottir et al. 2014, 2015). These are important findings, as they suggest that public health approaches targeting child maltreatment and integrated, patient-centered medical systems may allow for the potential reduction of illness and premature death (Tomasdottir et al. 2014; Bousquet et al. 2011).
The concepts of allostatic overload and biological aging may explain the links between chronic stress during childhood and disease development in adulthood (Tomasdottir et al. 2015; Belsky et al. 2015). Allostasis refers to an organism’s physiological ability to maintain internal homeostasis in conditions of stress, and thus allostatic overload occurs when this restorative capacity is overtaxed and this results in increased risk for disease (Tomasdottir et al. 2014, 2015). Therefore, there may be a distinguishable trajectory from childhood maltreatment to health problems in adulthood. Increasing evidence supports an association between childhood adversity and allostatic overload, suggesting that it serves as a general mechanism through which childhood trauma becomes biologically embedded (Tomasdottir et al. 2015; Shonkoff et al. 2012). Research has proposed several specific biological mediators through which childhood maltreatment can lead to higher rates of morbidity and mortality in adulthood (Shonkoff et al. 2012). Studies investigating how early adversity can incur risk for poor adult health have shown that survivors of child maltreatment can present with neuroendocrine stress response desensitization, epigenetic modifications, elevated levels of inflammatory cytokines, and altered pain sensitivity (Fillingim and Edwards 2018; Shonkoff et al. 2012). All of these perturbations illustrate how childhood maltreatment can become biologically embodied, and alterations in these systems are linked to increased disease prevalence (Tomasdottir et al. 2015; Shonkoff et al. 2012). Furthermore, there is substantial heterogeneity in human aging, as adults of the same chronological age can vary in their pace of “biological” aging as determined by rates of deterioration across multiple organ systems (Belsky et al. 2015). The “healthspan” includes the years of life lived free of disease and disability (Burch et al. 2014), and a recent cohort study from New Zealand has shown that accumulation of more personal history risk factors (e.g., lower childhood social class, more adverse childhood experiences) predicts faster paces of biological aging (Belsky et al. 2017). These findings suggest that anti-aging and geroprotective therapies may help to mitigate the adult health consequences of childhood maltreatment.
Limitations
Certain limitations should be considered when interpreting this study’s results. All data come from self-report measures, instead of substantiated court or clinic cases of child maltreatment or medical chart review of chronic health conditions and mental disorders. While prior research on the validity of adult retrospective reports of child maltreatment indicate that recall bias is minimal and false positives are rare (Hardt and Rutter 2004), only a limited range of subtypes were assessed, with lack of data on exposure to child neglect being a notable limitation. Although previous research has described the complexity and heterogeneity of maltreatment experiences (Bellis et al. 2014; Afifi et al. 2016), this study is limited by lack of information collected pertaining to the timing, duration, and perpetrator of maltreatment experiences. Due to the nature of survey data collected and previously established definitions of child maltreatment in regard to the 2012 CCHS - MH (Afifi et al. 2014), additional analyses regarding frequency or co-occurrence of child maltreatment subtypes were not possible, and future research using population-based datasets is encouraged to examine the impact of these factors on adult health outcomes. Also, no information was collected regarding the age of onset of chronic conditions. Due to the cross-sectional nature of the data, no conclusions can be made regarding causation. Furthermore, given the link between childhood adversity and premature mortality (Brown et al. 2009), use of a cross-sectional design also limits possible inferences regarding the long-term health outcomes of child maltreatment. Longitudinal data could help inform the underlying mechanisms in associations between child maltreatment and multimorbidities.
Conclusion
To our knowledge, this is the first study to assess multiple maltreatment subtypes and a comprehensive range of multimorbid conditions using nationally representative data. These findings highlight the importance of considering the range of adversities to which individuals have been exposed in childhood. This may have implications for healthcare providers in determining risk for chronic conditions and multimorbidities among their patients. Although strategies for reducing chronic conditions at the population level have typically focused on health promotion approaches to reduce smoking, substance abuse, and obesity, perhaps there needs to be a greater emphasis on preventing child maltreatment as a key strategy in chronic disease prevention and in particular, adult multimorbidities. It is essential that longitudinal population-level data include comprehensive measures of health as well as adversity, to address this important issue.
References
Afifi, T. O., MacMillan, H. L., Boyle, M., Taillieu, T., Cheung, K., & Sareen, J. (2014). Child abuse and mental disorders in Canada. Canadian Medical Association Journal, (9), E324–E332. https://doi.org/10.1503/cmaj.131792.
Afifi, T. O., MacMillan, H., Boyle, M. H., Cheung, K., Taillieu, T., Turner, S., & Sareen, J. (2016). Child abuse and physical health in Canada. Statistics Canada. Health Reports, 27(3), 10–18.
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders, 4th edn. Text Revision. Washington, DC: American Psychiatric Association.
Anda, R. F., Felitti, V. J., Bremner, J. D., et al. (2006). The enduring effects of abuse and related adverse experiences in childhood. European Archives of Psychiatry and Clinical Neuroscience, 256(3), 174–186. https://doi.org/10.1007/s00406-005-0624-4.
Barnett, K., Mercer, S. W., Norbury, M., Watt, G., Wyke, S., & Guthrie, B. (2012). Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet, 380(9836), 37–43. https://doi.org/10.1016/S0140-6736(12)60240-2.
Bellis, M. A., Lowey, H., Leckenby, N., Hughes, K., & Harrison, D. (2014). Adverse childhood experiences: retrospective study to determine their impact on adult health behaviours and health outcomes in a UK population. Journal of Public Health (Bangkok), 36(1), 81–91. https://doi.org/10.1093/pubmed/fdt038.
Belsky, D. W., Caspi, A., Houts, R., et al. (2015). Quantification of biological aging in young adults. Proceedings of the National Academy of Sciences of the United States of America, 112(30), E4104–E4110. https://doi.org/10.1073/pnas.1506264112.
Belsky, D. W., Caspi, A., Cohen, H. J., et al. (2017). Impact of early personal-history characteristics on the pace of aging: implications for clinical trials of therapies to slow aging and extend healthspan. Aging Cell, 16(4), 644–651. https://doi.org/10.1111/acel.12591.
Bousquet, J., Anto, J. M., Sterk, P. J., et al. (2011). Systems medicine and integrated care to combat chronic noncommunicable diseases. Genome Medicine, 3(7), 43. https://doi.org/10.1186/gm259.
Brown, D. W., Anda, R. F., Tiemeier, H., et al. (2009). Adverse childhood experiences and the risk of premature mortality. American Journal of Preventive Medicine, 37(5), 389–396. https://doi.org/10.1016/j.amepre.2009.06.021.
Burch, J. B., Augustine, A. D., Frieden, L. A., et al. (2014). Advances in geroscience: impact on healthspan and chronic disease. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 69(Suppl 1), S1–S3. https://doi.org/10.1093/gerona/glu041.
Canadian Community Health Survey: Mental Health and Well- Being Derived Variable (DV) Specifications. (2013). Statistics Canada, Ottawa.
Egede, L. E. (2007). Major depression in individuals with chronic medical disorders: prevalence, correlates and association with health resource utilization, lost productivity and functional disability. General Hospital Psychiatry, 29(5), 409–416. https://doi.org/10.1016/j.genhosppsych.2007.06.002.
Fillingim, R. B., & Edwards, R. R. (2018). Is self-reported childhood abuse history associated with pain perception among healthy young women and men? The Clinical Journal of Pain, 21(5), 387–397. http://www.ncbi.nlm.nih.gov/pubmed/16093744. Accessed February 2.
Fuller-Thomson, E., Brennenstuhl, S., & Frank, J. (2010). The association between childhood physical abuse and heart disease in adulthood: findings from a representative community sample. Child Abuse & Neglect, 34(9), 689–698. https://doi.org/10.1016/J.CHIABU.2010.02.005.
Gonzalez, A., Boyle, M. H., Kyu, H. H., Georgiades, K., Duncan, L., & MacMillan, H. L. (2012). Childhood and family influences on depression, chronic physical conditions, and their comorbidity: findings from the Ontario Child Health Study. Journal of Psychiatric Research, 46(11), 1475–1482. https://doi.org/10.1016/j.jpsychires.2012.08.004.
Hardt, J., & Rutter, M. (2004). Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. Journal of Child Psychology and Psychiatry, 45(2), 260–273. https://doi.org/10.1111/j.1469-7610.2004.00218.x.
Moussavi, S., Chatterji, S., Verdes, E., Tandon, A., Patel, V., & Ustun, B. (2007). Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet, 370(9590), 851–858. https://doi.org/10.1016/S0140-6736(07)61415-9.
Ording, A., & Henrik Toft Sørensen, H. (2013). Concepts of comorbidities, multiple morbidities, complications, and their clinical epidemiologic analogs. Journal of Clinical Epidemiology, 5, 199. https://doi.org/10.2147/CLEP.S45305.
Richardson, W. S., Doster, L. M., Sibbald, B., et al. (2014). Comorbidity and multimorbidity need to be placed in the context of a framework of risk, responsiveness, and vulnerability. Journal of Clinical Epidemiology, 67(3), 244–246. https://doi.org/10.1016/j.jclinepi.2013.10.020.
Schmitz, N., Wang, J., Malla, A., & Lesage, A. (2007). Joint effect of depression and chronic conditions on disability: results from a population-based study. Psychosomatic Medicine, 69(4), 332–338. https://doi.org/10.1097/PSY.0b013e31804259e0.
Scott, K. M., Bruffaerts, R., Tsang, A., et al. (2007). Depression–anxiety relationships with chronic physical conditions: results from the World Mental Health surveys. Journal of Affective Disorders, 103(1–3), 113–120. https://doi.org/10.1016/j.jad.2007.01.015.
Shonkoff, J. P., Garner, A. S., Committee on Psychosocial Aspects of Child and Family Health BS, et al. (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics, 129(1), e232–e246. https://doi.org/10.1542/peds.2011-2663.
Springer, K. W., Sheridan, J., Kuo, D., & Carnes, M. (2007). Long-term physical and mental health consequences of childhood physical abuse: results from a large population-based sample of men and women. Child Abuse & Neglect, 31(5), 517–530. https://doi.org/10.1016/j.chiabu.2007.01.003.
Statistics Canada. (2013). Canadian Community Health Survey (CCHS)- mental health user guide. Ottawa: Statistics Canada.
Tomasdottir, M. O., Getz, L., Sigurdsson, J. A., et al. (2014). Co-and multi-morbidity patterns in an unselected Norwegian population: cross-sectional analysis based on the HUNT Study and theoretical reflections concerning basic medical models. European Journal of Person Centered Healthcare - Eur J Pers Cent Healthc, 2(3), 335–345.
Tomasdottir, M. O., Sigurdsson, J. A., Petursson, H., et al. (2015). Self reported childhood difficulties, adult multimorbidity and allostatic load. A cross-sectional analysis of the Norwegian HUNT Study. Gao C-Q, ed. PLoS One, 10(6), e0130591. https://doi.org/10.1371/journal.pone.0130591.
Walsh, C. A., MacMillan, H. L., Trocmé, N., Jamieson, E., & Boyle, M. H. (2008). Measurement of victimization in adolescence: development and validation of the Childhood Experiences of Violence Questionnaire. Child Abuse & Neglect, 32(11), 1037–1057. https://doi.org/10.1016/j.chiabu.2008.05.003.
World Health Organization. (2008). The world health report 2008: primary health care—now more than ever. New York: World Health Organization http://www.who.int/whr/2008/en/. Accessed February 21, 2017.
Acknowledgements
Statistics Canada collected and provided the data for academic purposes, but the analyses are the sole responsibility of the authors. The opinions expressed do not represent the views of Statistics Canada.
Funding
M. Ferro currently holds the Canada Research Chair in Youth Mental Health. H.L. MacMillan is supported by the Chedoke Health Chair in Child Psychiatry. A. Gonzalez is supported by a Canadian Institutes of Health Research New Investigator Award.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
England-Mason, G., Casey, R., Ferro, M. et al. Child maltreatment and adult multimorbidity: results from the Canadian Community Health Survey. Can J Public Health 109, 561–572 (2018). https://doi.org/10.17269/s41997-018-0069-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.17269/s41997-018-0069-y