Abstract
Microneedles are microscale needle-shaped devices that have attracted attention from the biomedical engineering community for transdermal drug delivery, sensing, and vaccine delivery. These devices do not inflict significant discomfort during skin penetration. Microneedles have recently been used to detect physiologically relevant molecules in interstitial fluid for health monitoring. In this review, technical challenges associated with microneedle processing are considered. The mechanical requirements associated with microneedle penetration of the skin are described. The use of polymers, bioceramics, and natural materials in microneedle fabrication is described. Recent uses of microneedles in biosensing, drug delivery, and vaccine delivery are described.
Graphical abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The skin is the largest organ of the body, which protects the body from harmful external materials and microorganisms; in addition, it prevents water evaporation.[1] Efforts at transdermal drug delivery are described in ancient Babylonian and Egyptian history.[2] The use of ointments and salves can be considered an early form of drug delivery. In the 1940s and 1950s, nitroglycerin ointment was used to treat Raynaud’s disease and angina pectoris.[3] The transderm-Scop patch, which administered the anticholinergic agent scopolamine for preventing nausea and vomiting, was approved by the US Food & Drug Administration in 1979.[4,5,6,7] Patches for some small lipophilic drugs such as nitroglycerine, nicotine, and fentanyl were subsequently developed.[8]
Oral delivery is a common route for delivering drugs; however, oral delivery is not suitable for some drugs due to poor absorption in the gastrointestinal tract or high rates of first-pass metabolism.[9] The conventional syringe-based injection is associated with pain and injury at the injection site; in addition, specialized training is required for the appropriate use of a syringe.[10] Microneedles are an alternative approach for drug delivery[11]; these devices penetrate the outermost layer of the epidermis, the stratum corneum layer, which acts as an obstacle to the transdermal delivery of non-lipophilic drugs.[12,13] Other methods for transdermal drug delivery have also been demonstrated, including thermal ablation, ultrasound-facilitated delivery, iontophoresis, and the use of chemical enhancers. There are several benefits of microneedles over other techniques for transdermal drug delivery.[14,15] Furthermore, microneedles with have been integrated with various sensor platforms to fabricate wearable biosensors.[16] These devices can be used to detect biomarkers, including glucose, lactate, ions, cytokines, proteins, and immunoglobulins.[17,18] For example, microneedle-incorporated wearable patches may be used to detect transdermal pH levels in interstitial fluid (ISF). These wearable biosensors allow for the long-term assessment of biomarker levels.[19,20]
In this review paper, we consider recent studies involving novel materials that are used for microneedle fabrication. The use of microneedles for sensor, drug delivery, and vaccine delivery applications is also considered. For example, devices containing microneedles and biosensors may be used to detect glucose and other biochemicals in a continuous manner.[21]
The stratum corneum is the outermost skin layer; it exhibits a thickness of 10–15 µm[22] and serves as a barrier to the transepidermal delivery of many types of drugs. Microneedles can be painless if they do not interact with the unmyelinated nerve endings that detect pain or the mechanoreceptors that detect pressure, which are located in a lower layer of the skin known as the dermis (the thickness of the dermis varies based on the body location).[23,24]
Materials commonly used to make microneedles
Non-biodegradable (e.g., polystyrene (PS) and poly(methylmethacrylate) (PMMA)) and biodegradable polymers (e.g., poly lactic acid (PLA) and polylactic-co-glycolic acid (PGLA)) are the two major types of materials that are used for fabricating microneedle arrays.[25] Chitosan[26] and silk[27] are some of the natural polymers that are used to prepare microneedle arrays.[28] Polyvinyl alcohol (PVA), poly (methyl vinyl ether-co-maleic acid) (PMVE/MA), polystyrene-block-poly (acrylic acid) (PS-b-PAA), and hyaluronic acid (HA) acrylate are hydrogel-forming polymers that are used to prepare microneedles.[29] Crosslinking polymers such as ethylene glycol dimethacrylate and poly(2-hydroxyethyl methacrylate) (PHEMA) are photoactive hydrogel-forming polymers[30] that are used to prepare microneedle arrays.[31] Microneedles must possess sufficient mechanical properties to pierce the topmost layers of skin; in addition, they need to be biocompatible with cells in the epidermis and underlying dermis. Both biodegradable and non-biodegradable materials are used for microneedle fabrication. The following sections will consider the use of polymers, bioceramics, natural materials, and metals for microneedle fabrication.
Polymers
A variety of synthetic polymers have been used for microneedle fabrication. For example, Pere et al. coated insulin and carriers (e.g., trehalose, mannitol, and xylitol) using an inkjet printer on microneedles made from a biocompatible Class I resin called Dental SG. They fabricated microneedles in two shapes, conical and pyramidal; the release time for both microneedle types was below 30 min.[32] Another study used fused deposition modeling (FDM) to prepare microneedles out of polylactic acid; a post-fabrication etching protocol was used to obtain tip sizes as small as 1 μm. A drug was subsequently coated on the microneedles. Drug diffusion using the microneedles was demonstrated in porcine skin.[33] Poly lactic acid (PLA), carboxymethyl cellulose (CMC), and polylactic-co-glycolic acid (PGLA) microneedles were fabricated using a molding process; the microneedle tips were then dip-coated in bleomycin.[34] The hydrophobic PLA surface was converted into a hydrophilic surface by ozone treatment. 80% of the coated drug was released in skin within 15 min. A study that involved piercing the microneedle in porcine skin showed that the microneedle possessed sufficient skin penetration properties for transdermal use.[34] Pamornpathomkul et al. described the use of a microneedle made of the commercial biodegradable polymer Gantrez® S-97 to deliver acyclovir. The acyclovir Gantrez® microneedle was dissolved in porcine skin in two hours. Acyclovir-loaded microneedle arrays showed better topical delivery than a commercial cream formulation in terms of delivering the drug to the basal epidermis. In vivo studies showed that the drug-loaded microneedles delivered acyclovir successfully to the skin, and a very low concentration of the drug was detected in the blood.[35] In another study, a patient-controlled drug delivery system for analgesia was developed, which contained a photo-triggered microneedle. Near-infrared (NIR) light stimulation was used for enabling on-demand delivery of pain medication to the skin. Polymeric microneedles were fabricated using the combination of NIR absorbers, analgesics, and poly(L-lactide-co-D,L-lactide). The NIR absorbers[36] absorb the light energy in order to increase the phase transition by NIR light irradiation; drug release is induced by this process. The lidocaine was absorbed into the blood circulation in ten minutes, enabling rapid onset of pain relief. Figure 1 shows the schematic of the microneedle used in this study, which contains a polycaprolactone (PCL) microneedle.[37] Table I shows different polymers, drugs, and microneedle shapes that were evaluated as well as the relevant results from recent studies. This table shows that most microneedles have a range between 450 μm and 1.2 mm. The lower limit of microneedle height is determined by two considerations: (a) skin penetration is less uniform at lower microneedle heights due to individual-to-individual variations in skin thickness and roughness, and (b) microneedle application protocols are a more dominant consideration in determining microneedle penetration depth at lower microneedle heights. The upper limit of microneedle height is determined by the presence of nerve endings that detect pressure and pain, which are located in the upper (papillary) layer of the dermis.
Schematic of PCL–PLA microneedle patch fabrication process. Republished with permission of the Royal Society of Chemistry from Ref. 37; the permission was conveyed through the Copyright Clearance Center.
Bioceramics
Microneedles have many benefits for transdermal drug delivery; however, many polymers have poor mechanical properties that make them unsuitable for some skin penetration applications.[34,35] The controlled porosity of certain types of ceramics makes them a strong candidate for use in microneedle applications.[38,39] Cai et al. presented a self-setting bioceramic for use in microneedle fabrication. They developed CaS-based and CaP-based ceramic microneedle arrays; monocalcium phosphate monohydrate, beta-tricalcium phosphate, calcium sulfate alpha hemihydrates, and citric acid were used to synthesize self-setting ceramics. They adjusted the drug release properties by modifying the needle dimensions and porosity. The results of this study showed that the drug release rate was dependent on the bulk surface area, porosity, and resorption rate of the ceramic needles. The capability of sustained release from porous ceramic microparticles is related to the surface pore size distribution as well as the electrostatic interactions between both the interior and exterior microparticle surface and the drug.[40] Another study used a self-swelling flexible substrate and bioceramic microneedles to optimize the drug release profile. The microneedles on the flexible substrate were released into the skin faster than those on the rigid substrate. Figure 2 shows drug release from BCMN-G450, BCMN-G600, SCMN-450, and SCMN-600 microneedle devices; the BCMN-G450 and BCMN-G600 bioceramic[41] microneedles on the swellable substrate exhibited needle lengths of 450 µm and 600 µm, respectively. The result showed that the model drug, clonidine hydrochloride, was released faster from microneedles with a flexible and self-swelling substrate than from microneedles with a rigid substrate.[42] Vallhov et al. covered patches with biodegradable ceramic (calcium sulfate) to deliver ovalbumin (OVA) into the epidermis. Two different lengths (300 and 600 µm) were fabricated; the penetration ability of the devices was evaluated. The taller microneedle with an average pore size of 12 ± 1 µm was shown to be more efficient in delivering OVA. 90% of the loaded OVA was released in one hour from microneedles with a height of 600 µm. This study demonstrated the use of ceramic microneedles for the penetration of human ex vivo skin. Sharper needles, which were prepared by increasing the aspect ratio, were more successful in penetrating human stratum corneum.[43] Alumina (Al2O3) is one of the frequently used ceramics for making microneedle arrays; the covalent bonding between the Al and O atoms provides the material with unusual chemical stability.[44] The devices also show good mechanical strength under compression but can fail by brittle fracture under tensile stress. Another material for making microneedles is silica glass,[45] which can be fabricated into devices with different geometric shapes.
Drug release from bioceramic microneedles with a flexible and swellable substrate with 450 µm and 600 µm needle length. SCMN microneedle arrays with a rigid substrate. Reprinted from Ref. 42, Copyright 2015, with permission of Elsevier.
Natural materials
Natural polymers are a suitable candidate for biocompatible microneedle fabrication due to their relatively low cost and compatibility with straightforward processing procedures. These materials need to exhibit suitable biocompatibility and appropriate mechanical properties for skin penetration. Several natural polymers have been utilized in recent years to manufacture microneedles.[46] The popular natural polymers for microneedles fabrication are CMC (a soluble polysaccharide),[47] silk fibroin (a protein in silk that is usually produced by various insects),[20] fish scale (a material extracted from the scales of tilapia and other types of fish),[48] alginate (a salt of alginic acid),[49] and chitosan (a derivative of glucose).[26] Hwa fabricated polysaccharide-based microneedle arrays.[50] Dextrin, CMC, amylopectin (AMP), and trehalose (TRE) were used for micromolding; CMC is a derivative of cellulose, dextrin is a water-soluble carbohydrate that is produced by the hydrolysis of starch, AMP is a water-soluble polysaccharide, and TRE is a natural disaccharide by two glucose units. Aluminum was used to create the mold that was used for micromolding of the microneedles.[50] Another study confirmed that CMC and TRE possess no cytotoxicity.[51] Several efforts have been made to evaluate microneedles made of silk fibroin.[46,52] Silk fibroin microneedles containing influenza, Clostridium difficile, and Shigella vaccines were shown to successfully vaccinate mice.[53] Another study demonstrated the use of silk fibroin microneedles to deliver insulin. Insulin was dissolved in Tris–HCl buffer solution (pH 7); different mass ratios of insulin and fibroin were prepared using a lithography approach. Insulin stability in the microneedles, dissolution performance, swelling performance, in vitro release of insulin, pharmacodynamics delivery of insulin, and pharmacokinetics of insulin delivery were demonstrated.[54] Recently, Bletilla striata polysaccharide (BSP)-based dissolving microneedles were prepared for use in transdermal drug delivery.[55] BSP is a natural glucomannan material made from the Chinese ground orchid that shows very good moldability. Other natural materials have been considered for use in microneedles, including chitosan, maltose, alginates,[56] hyaluronic acid,[57] and zein.[58]
Metals
Microneedles have been made from several types of metals via laser cutting, micromolding, and micromachining methods.[59] Laser cutting and electrodeposition are typical techniques for producing metallic microneedles. Hot embossing of 316 stainless steel microneedle arrays followed by sintering at 1100°C and successive electropolishing has been described.[60] One issue that limits the use of hollow metal microneedles is clogging of the microneedle core during skin entry; moreover, the walls of hollow microneedles must resist fracture during the skin penetration process.[61] Permeable Ti microneedles have been produced by casting-based methods in a polydimethylsiloxane (PDMS) mold, followed by drying and sintering steps. The Ti microneedles showed appropriate strength; however, a limitation of these devices is their high manufacturing cost.[59]
Applications of microneedles
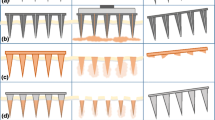
One of the applications of microneedles technology involves the use of microneedles for drug delivery in place of a conventional injection. A number of studies have been conducted on vaccine delivery with microneedles. Another application involves the detection of biomolecules in skin interstitial fluid using microneedles, with most of the attention being focused on glucose sensing. Microneedles can be used in different ways. One approach involves the use of a solid microneedle for creating transient micropores in the skin, followed by the use of a conventional transdermal patch. Another approach involves the use of a solid microneedle containing a drug such that the microneedle will be removed after the drug is dissolved. Another approach involves the use of a biocompatible polymer microneedle that dissolves and releases a drug over time after insertion into the skin. Another approach involves the application of a hollow microneedle to the skin, which delivers a fluid containing the drug. Another approach for delivering drugs involves applying hydrogel-forming polymeric microneedles to the skin, which form conduits between the skin and the drug reservoirs that are connected with the microneedles.[29]
Microneedles biosensors
Microneedles may be used to detect physiologically related analytes under the skin surface. One advantage of microneedle sensors is that they can be used to monitor chemical and physical processes under the skin surface in a continuous manner. For example, microneedles can be incorporated with thermal flow sensors to measure low speed liquid flow.[62] In addition, chemical sensors for ascorbic acid, lactate, hydrogen peroxide, and glucose have been incorporated with microneedles in previous studies.[63,64,65] Several recent studies have focused on the simultaneous detection of multiple analytes using a single microneedle device. For example, pH, lactate, and glucose were detected using an array of acrylate-based polymer microneedles that contained electrochemical sensors within their bores. The device was able to detect pH, lactate, and glucose in complex solutions.[66]
Several methodologies are used to monitor blood alcohol levels. Urine testing, blood testing, saliva testing, breath testing, and sweat testing are commonly used. Although blood testing is accurate, the administration of blood tests can be painful. A microneedle-based biosensor was proposed by Mohan et al. to assess alcohol levels in a continuous manner. Ag and Pt wires were incorporated within the hollow microneedles; the platinum wire was modified using o-phenylene diamine, alcohol oxidase, a chitosan layer, and a Nafion layer.
This structure was used to continuously monitor alcohol in an artificial interstitial fluid.[67] In another recent study, titanium alloy microneedles were coated with nitrogen-incorporated ultra-nanocrystalline diamond (N-UNCD) thin films.[68] In vitro detection of dopamine and uric acid was demonstrated using linear scanning voltammetry [Fig. 3(a), (b)][69]. Figure 3(c), (d) shows linear sweep voltammograms on N-UNCD electrodes in a 1 × PBS (pH 7.4) solution that contains uric acid concentration over the range of 1 to 200 µm, and a dopamine concentration over the range of 0 to 30 μm versus an Ag/AgCl reference and a Pt wire counter electrode, respectively. Song et al. presented a novel approach to detect vascular endothelial growth factor (VEGF) in the blood for potential use in cancer diagnosis. These sensors were incorporated with a peptide aptamer-based microneedle for the electrochemical detection of VEGF. The biosensor was able to detect VEGF over the range from 0.1 to 1000 pM.[70] Ciui et al. created microneedle biosensors for the rapid detection of melanoma; the microneedle device was used for the detection of melanoma biomarker tyrosinase in porcine skin and a tyrosinase-containing agarose phantom gel.[71] Another study described the electrochemical monitoring of levodopa for the management of Parkinson's disease. A new dual-mode sensing approach, which involved independent enzymatic-amperometric and nonenzymatic voltammetric detection methods, provided built-in redundancy for the levodopa measurements; the sensor demonstrated high selectivity, high sensitivity, and stability when tested in artificial interstitial fluid.[21] Senel et al. made gold microneedle sensors by casting conductive gold ink; the microneedles were modified with an epoxy- and ferrocene-functional polymeric mediator; urease was covalently immobilized on the surface of the sensor. The sensor was tested with a skin mimic and artificial interstitial fluid. The sensor was used to detect urea over a 50–2500 µm range; a 2.8 µm limit of detection was demonstrated using this approach.[72]
SEM images of uncoated titanium alloy microneedle arrays of (a) N-UNCD-coated microneedle array and (b) single N-UNCD-coated microneedle. Linear sweep voltammograms on N-UNCD electrodes in a 1 × PBS (pH 7.4) solution that contains (c) uric acid concentration in the range of 1 to 200 µM and (d) dopamine concentration ranging from 0 to 30 μM versus Ag/AgCl reference and Pt wire counter electrode. Reprinted from Ref. 69, Copyright 2015, with permission of Elsevier.
Another study demonstrated the use of microneedles containing nanoparticulate palladium powder and either a polycarbonate binder or a polystyrene binder for transdermal sensing.[73] Samavat et. al. detected glucose using microneedles that were created using three different methods, including spray deposition of materials in subsequent layers (SL), conventional drop-cast of tetrathiafulvalene and glucose oxidase compounds in the subsequent layer, and spray mixing of the compounds as one uniform layer (SM). A uniform sensing layer of mixed aerosol particles of tetrathiafulvalene and glucose oxidase was produced by the SM technique. Glucose sensors made using this approach can be mass produced at low cost.[74]
Thermocurable materials were used to fabricate a wireless glucose sensor containing microneedles. Microneedles made from gold provided an interface with electrical conductivity and biocompatibility. Nafion™ membrane was used to prevent detachment of the enzyme layer. Terthiophene carboxylic acid was employed for stable immobilization of FAD-glucose oxidase onto the electrode surface. The glucose concentration was measured wirelessly by a transmitter that was attached to a sensing module. The sensing module included an analog-to-digital converter, miniaturized potentiostat, Bluetooth, near-field communication, and flexible lithium-ion polymer battery. Finally, this device was assessed by performing glucose level measurements in finger prick blood samples. The sensor showed an excellent linear glucose concentration response.[75] Dardano et al. synthesized microneedle arrays from polyethylene glycol, diacrylate hydrogel, an enzyme (glucose oxidase), as well as a redox mediator (vinylferrocene). The microneedle array was used as a working electrode. The redox reaction with glucose created a charge transfer that was enhanced by the redox mediator, which resulted in a current proportional to the glucose concentration.[76] Lee et al. described the incorporation of graphene within a microneedle biosensor. Graphene is a versatile material in microelectronics because of its carrier mobility, flexibility, conductivity, and optical transparency; however, the low electrochemical density of bare graphene limits its biosensing ability. The incorporation of gold mesh with graphene provided better electrochemical activity than bare graphene. The device included sensors for humidity, temperature, glucose, and pH as well as a polymeric microneedle for drug delivery. The fabricated patch was thermally actuated to deliver metformin and was able to reduce the blood glucose level in diabetic mice.[77] Hegarty et al. prepared carbon-loaded polystyrene microneedle patches for transdermal sensing. Figure 4 shows the basic composition of the measurement system. Carbon-loaded polystyrene was the main component of the working and reference electrodes; the polymer was used to facilitate skin penetration. Tomato skin was used to examine the electroanalytical performance of the carbon-loaded microneedles.[78]
Configuration of the proposed carbon-loaded polystyrene microneedle sensing array. Reprinted from Ref. 78, Copyright 2019, with permission of Elsevier.
Valadeiro et al. demonstrated a microneedle device in which the probes were able to record electric and magnetic fields simultaneously with micrometer spatial resolution. The microneedles were integrated with magnetoresistive sensing elements and a thin film electrode. The fabricated probe was inserted into a mouse hippocampus brain slice for the magnetic recordings.[79] The pH is precisely controlled by the kidney, lung, and buffer systems; small changes in the pH levels may affect many organs. Mani et al. proposed a novel technique for determining real-time pH.[80] A study by Sulaiman et al. identified nucleic acid biomarkers in liquid biopsies that are used for early cancer diagnosis. Microneedles coated with an alginate-peptide nucleic acid hybrid were used for the sequence-specific sampling and monitoring of nucleic acid biomarkers in interstitial fluid. Figure 5 shows the microneedle sampling and detection mechanism.[81]
(a) Mean fluorescence microscopy data, (b) microneedle patch ability to discriminate between a complementary and a noncomplementary DNA target, (c) mechanisms for sensing, (d) significant difference in fluorescence between microneedle sampling DNA-210 and control group, and (e) PNA:DNA duplex into solution plot. Reprinted with permission from Ref. 81, Copyright 2019, American Chemical Society.
One recent study proposed a novel approach for tracking antimicrobial concentrations in real time to allow for individualized drug dosing. The electrode surface of the microneedle biosensors was coated with a layer of iridium oxide that detected changes in pH. The fabricated biosensor was stable for up to two weeks at a temperature of − 20ºC. β-lactam concentrations were measured in vivo using this approach. Figure 6 shows the pH responses for pure iridium oxide and both iridium oxide and β-lactamase hydrogel layers.[82] In another study, microneedle biosensors were proposed for detecting organophosphate (OPs) chemical agents. An organophosphorus hydrolase (OPH) was reported in this study that detected OP compounds under the skin. The OPH microneedle sensor was validated using skin samples collected from mice that were exposed to various levels of OP methyl paraoxon (MPOx). Microneedle arrays containing CP transducers coated with OPH-Nafion ™ reagents were used to electrochemically monitor the nerve agents. Figure 7 contains a schematic, which shows the approach for electrochemical detection of OP nerve agents with the OPH microneedle sensor containing carbon and Ag/AgCl components.[83]
pH responses of MNs coated with iridium oxide only (purple) and both iridium oxide and β-lactamase hydrogel layers (blue). Reprinted with permission from Ref. 82, Copyright 2019, American Chemical Society.
Schematic of the electrochemical detection of OP nerve agents by OPH microneedle sensor. Republished with permission of the Royal Society of Chemistry from Ref. 83, permission conveyed through Copyright Clearance Center.
Microneedle-based wearable sensors
Microneedle sensors include wearable miniaturized devices containing microneedles and sensors. Tehrani et al. described the fabrication of a portable and wireless microneedle-based wearable device for real-time monitoring, specifically for the simultaneous detection of glucose, lactate, and alcohol level in human participants while conducting daily activities.[84] This fully integrated device was connected to mobile software, which may be able to overcome challenges associated with cross-talk-free detection and analysis. The device was composed of disposable and recyclable components, which enabled the fabrication of a low-cost wearable biosensor. Bollella et al. developed a painless microneedle-based wearable biosensor for real-time probing of lactate levels in ISF.[85] The gold-plated microneedle was surface functionalized with multiwalled carbon nanotubes (MWCNTs) by electrodeposition and modified with a redox couple, methylene blue (MB). Figure 8 shows the microneedle structures metallized with gold (for use as working electrodes) and metallized with silver. The Au-MWCNTs/polyMB microneedle array platform was later modified with a lactate recognition enzyme, lactate oxidase. The device may be used for the detection of lactate in vitro as well as in realistic samples (human serum) for potential sport medicine and clinical care applications.[85] In another study, Gao et al. fabricated a mechanically flexible and portable wearable multiplexed sensor for monitoring sweat metabolites (e.g., glucose and lactate), electrolytes (e.g., potassium and sodium), and surface temperatures.[86] The device was integrated with electronic components for rapid signal transduction, amplification, and processing.
Polycarbonate structure of four 4 × 4 microneedle arrays metallized with gold and silver. Reprinted from Ref. 85, distributed under the terms of the Creative Commons CC BY license.
Microneedles for drug delivery
Drugs can be loaded in polymeric microneedles; drug delivery can be accomplished by the dissolution of the polymer in the interstitial fluid that is located in the skin. Drugs can also be coated on non-biocompatible microneedles; the microneedles penetrate the skin barrier and enable the delivery of the drug to deeper layers of the skin and eventually to the systemic circulation. In recent years, the delivery of anticancer drugs has become increasingly important. For example, an alternative approach to the surgical treatment of cancer involves intratumoral delivery of anticancer drugs. Ma et al. used PLGA that encapsulated with doxorubicin (DOX)[87] in order to deliver anticancer drugs; a near-infrared (NIR)-light-activated microneedle was developed to repeatedly release encapsulated drugs. The tip of the microneedles is fabricated from plasmonic lanthanum hexaboride nanoparticles (LaB6), PCL, and the anticancer drug doxorubicin (DOX). The supporting array patch was made from PVA and PVP. The LaB6 nanomaterials[88,89] were used to absorb NIR irradiation and served as an alternative plasmonic material for cancer cell thermal ablation. Furthermore, it was encapsulated in microneedles to prevent rapid clearance from the tumor, thus minimizing the need for repeated dosing. The laser energy was converted to heat by LaB6; the microneedles were released when 50°C was reached. Upon insertion into the interstitial fluid of the skin, the supporting array was released, and the tip component containing the drug was left at the target tissue for localized cancer therapy.[90] The same approach was used in another study for delivering doxorubicin hydrochloride in rat skin. In this technique, the laser was used to heat the polymer chain in order to release the drug.[91]
Another study described a NIR-responsive polymer hollow mesoporous SiO2 microneedle that was loaded with metformin and coated with polydopamine/lauric acid. Using a diffusion-based approach, an antidiabetic drug was loaded into hollow mesoporous SiO2 nanoparticles (HMSNs). A photothermal conversion agent (PDA) and phase change material, lauric acid, were incorporated in a subsequent step. The microneedle package was encapsulated with a biocompatible polymer, PVP. After insertion into the skin, the effect of NIR light on the PDA will melt the lauric acid, releasing the encapsulated metformin. After insertion of fabricated microneedles in diabetic rats, the bioavailability of 95.8 ± 2.7% was achieved. One advantage associated with the use of the NIR-responsive polymer is that the drug release can be adjusted by changing the time and power density.[92] Another study considered the use of microneedles for the treatment of melanoma. Microneedles were fabricated using hyaluronic acid combined with pH-sensitive dextran nanoparticles (NPs), which were encapsulated with glucose oxide and PD1. Blood glucose is converted to gluconic acid by glucose oxide; this acidic environment increases the self-dissociation of NPs and facilitates PD1 release.[93] Kearney et al. delivered donepezil hydrochloride through hydrogel-forming microneedles. They inserted hydrogel-forming microneedles into the skin; the drug loaded in the reservoir moved through the microneedles into the skin. Figure 9 shows the hydrogel-forming technique for microneedle fabrication. The microneedles, which exhibited a conical shape and a height of 600 µm, were made from PMVE/MAH and PMVE/MA. A in vitro study demonstrated the delivery of 854.71 µg ± 122.71 µg donepezil hydrochloride in neonatal porcine skin.[94]
Hydrogel-forming microneedles in combination with drug-loaded reservoir. Reprinted from Ref. 94, Copyright 2015, with permission of Elsevier.
Microneedles for vaccine delivery
The accessibility of the dermal route and the presence of dermal immune cells (e.g., Langerhans cells) make the skin an ideal route for vaccine delivery. Microneedles are able to deliver vaccines to the dermis, which can enhance the efficacy of immunization.[95] Almost all of the fabrication techniques for microneedle manufacturing are based on micromolding. One consideration is that heat can be disruptive to vaccines or protein-based drugs. The high melting temperature (160°C) of molten galactose during the microneedle fabrication has been associated with significant changes to 5-aminolevulinic acid and bovine serum albumin (BSA).[96] A subsequent study examined the effect of thermal exposure (135°C) on BSA in melted PLGA; little difference was noted in the α-helix/β-sheet of heated BSA compared with that of intact BSA.[97]
The microneedle release time is dependent on the type of polymer and can be prolonged or shortened based on the application. For example, a recent study evaluated the performance of carboxymethylcellulose (CMC) and hyaluronan (HN) microneedles. Both polymeric microneedles were dissolved completely in rat skin after 5 min of insertion. Compared to conventional injections, both microneedles were associated with increased antigen-specific IgG levels; both microneedles were used to deliver antigens to resected human dermal tissue. Finally, no significant skin irritation was seen after microneedle insertion into human skin.[98] The delivery of vaccines is limited by poor immunogenicity and low transfection efficiency. The delivery of vaccines to antigen-presenting cells and the subsequent stimulation of CD4 + and CD8 + T cell immunity are not efficient for current DNA vaccines. Several studies have attempted to enhance the immunogenicity of DNA vaccines. An array of microneedles coated with polyelectrolyte multilayers and reversible pH-responsive copolymer and heparin was developed for the rapid delivery of polyplex-based DNA vaccines. A pH-responsive copolymer that contains oligo(sulfamethazine)-b-poly(ethylene glycol)-b-poly(amino urethane) (OSM-b-PEG-b-PAEU) was used as a triggering layer in the polyelectrolyte multilayer. The electrostatic repulsion between heparin and OSM-b-PEG-b-PAEU released the DNA vaccine.[99] Another study developed a smart DNA vaccine delivery system containing nanoengineered DNA vaccines, ultra-pH-responsive OSM-(PEG-PAEU), and an immunostimulatory adjuvant poly(I:C).[100] Another recent study described a double-decker microneedle that is suitable for use with various vaccine antigens. Two types of microneedle patches were made, which were made of polyglycolic acid and Nylon-6. Both microneedles could deliver antigens into the dermal tissue; antigen-specific IgG levels increased after using microneedles in comparison with conventional injection. PGA microneedles were noted to be better than Nylon microneedles for puncturing human skin.[101] Silk fibroin protein was used to produce microneedles for the delivery of Clostridium difficile, influenza, and Shigella vaccine. Fibroin protein from the silkworm Bombyx mori has suitable properties for use in microneedle manufacturing such as appropriate mechanical strength in dry form, biocompatibility, and the ability to stabilize biomacromolecules.[53] The other study used corn protein, zein, for microneedle fabrication. Micromolding was used for the microneedle fabrication process; the delivery of an antigen, ovalbumin, was confirmed via confocal microscopy and histological evaluation. Both OVA-coated microneedles and OVA intradermal injection showed significantly greater antibody production than the control group.[102]
Conclusions
Microneedle technology has evolved since it was introduced in 1976.[103,104,105] Microneedles have been constructed using a variety of materials, including biocompatible polymers and silicon. Both natural polymers and synthetic polymers have been considered for use in microneedles. In addition to the delivery of drugs and vaccines, the use of microneedles for transdermal sensing has been demonstrated. The major materials challenge related to microneedle technology involves creating microneedles with sufficient mechanical strength to pierce the skin without fracture. Moreover, the costs associated with large-scale microneedle fabrication must be reduced (e.g., through the elimination of steps that involve human labor) before microneedle technology can be successfully translated to commercial-scale manufacturing and large-scale clinical use.
References
J.S. Kochhar, W.J. Soon, J. Choi, S. Zou, L. Kang, Effect of microneedle geometry and supporting substrate on microneedle array penetration into skin. J. Pharm. Sci. 102(11), 4100–4108 (2013)
J. J. Escobar-Chávez, Current technologies to increase the transdermal delivery of drugs, (Bentham Science Publishers, 2010)
F. Home, Orange book: approved drug products with therapeutic equivalence evaluations (US Food & Drug Administration, Silver Spring, 2013)
M. Ochoa, C. Mousoulis, B. Ziaie, Polymeric microdevices for transdermal and subcutaneous drug delivery. Adv. Drug Deliv. Rev. 64(14), 1603–1616 (2012)
D.V. McAllister, M.G. Allen, M.R. Prausnitz, Microfabricated microneedles for gene and drug delivery. Annu. Rev. Biomed. Eng. 2(1), 289–313 (2000)
B.H. Kim, Y.H. Seo, Transdermal drug delivery devices based on microneedles: a review. J. Mucopolysaccharidosis Rare Dis. 1(1), 5–14 (2015)
J. M. Roe, R. A. Webster, and A. Ganesan, Synthesis of Cyclic Enamides via Ring-Closing Olefin Metathesis
B. Berner, V.A. John, Pharmacokinetic characterisation of transdermal delivery systems. Clin. Pharmacokinet. 26(2), 121–134 (1994)
B.A. Jana, A.D. Wadhwani, Microneedle–future prospect for efficient drug delivery in diabetes management. Indian J. Pharmacol. 51(1), 4 (2019)
V.K. Rai, N. Mishra, A.K. Agrawal, S. Jain, N.P. Yadav, Novel drug delivery system: an immense hope for diabetics. Drug Delivery 23(7), 2371–2390 (2016)
S. Shukla, R.H. Huston, B.D. Cox, A.R. Satoskar, R.J. Narayan, Transdermal delivery via medical device technologies. Expert Opin. Drug Deliv. 19(11), 1505–1519 (2022)
R.D. Boehm, P. Jaipan, S.A. Skoog, S. Stafslien, L. VanderWal, R.J. Narayan, Inkjet deposition of itraconazole onto poly (glycolic acid) microneedle arrays. Biointerphases 11(1), 011008 (2016)
P. Miller, M. Moorman, R. Manginell, C. Ashlee, I. Brener, D. Wheeler, R. Narayan, R. Polsky, Towards an integrated microneedle total analysis chip for protein detection. Electroanalysis 28(6), 1305–1310 (2016)
P.C. Pandey, S. Shukla, S.A. Skoog, R.D. Boehm, R.J. Narayan, Current advancements in transdermal biosensing and targeted drug delivery. Sensors 19(5), 1028 (2019)
M.R. Prausnitz, R. Langer, Transdermal drug delivery. Nat. Biotechnol. 26(11), 1261–1268 (2008)
H. Teymourian, F. Tehrani, K. Mahato, J. Wang, Lab under the skin: microneedle based wearable devices. Adv. Healthcare Mater. 10(17), 2002255 (2021)
M. Dervisevic, E. Dervisevic, L. Esser, C.D. Easton, V.J. Cadarso, N.H. Voelcker, Wearable microneedle array-based sensor for transdermal monitoring of pH levels in interstitial fluid. Biosens. Bioelectron. 222, 114955 (2023)
S. Shukla, P. Joshi, P. Riley, R.J. Narayan, Square wave voltammetric approach to leptin immunosensing and optimization of driving parameters with chemometrics. Biosens. Bioelectron. 216, 114592 (2022)
Z. Xie, X. Zhang, G. Chen, J. Che, D. Zhang, Wearable microneedle-integrated sensors for household health monitoring. Eng. Regen. 3(4), 420–426 (2022)
Y. Abe, R. Takizawa, N. Kimura, H. Konno, S. Yoshida, M. Nishizawa, Porous microneedle-based wearable device for monitoring of trans epidermal potential. Biomed. Eng. Adv. 1, 10004 (2021)
K.Y. Goud, C. Moonla, R.K. Mishra, C. Yu, R. Narayan, I. Litvan, J. Wang, Wearable electrochemical microneedle sensor for continuous monitoring of levodopa: toward Parkinson management. ACS Sensors 4(8), 2196–2204 (2019)
S. Henry, D.V. McAllister, M.G. Allen, M.R. Prausnitz, Microfabricated microneedles: a novel approach to transdermal drug delivery. J. Pharm. Sci. 87(8), 922–925 (1998)
M. Schmelz, R. Schmid, H.O. Handwerker, H.E. Torebjörk, Encoding of burning pain from capsaicin-treated human skin in two categories of unmyelinated nerve fibres. Brain 123(3), 560–571 (2000)
F. Salburgo, S. Garcia, A. Lagier, D. Estève, J.-P. Lavieille, M. Montava, Histological identification of nasopharyngeal mechanoreceptors. Eur. Arch. Otorhinolaryngol. 273(12), 4127–4133 (2016)
K.J. Lee, M.J. Goudie, P. Tebon, W. Sun, Z. Luo, J. Lee, S. Zhang, K. Fetah, H.J. Kim, Y. Xue, M.A. Darabi, S. Ahadian, E. Sarikhani, W.H. Ryu, Z. Gu, P.S. Weiss, M.R. Dokmeci, N. Ashammakhi, S. Khademhosseini, Non-transdermal microneedles for advanced drug delivery. Adv. Drug Deliv. Rev. 165, 41–59 (2020)
M.C. Chen, M.H. Ling, K.Y. Lai, E. Pramudityo, Chitosan microneedle patches for sustained transdermal delivery of macromolecules. Biomacromol 13(12), 4022–4031 (2012)
T. Dyakonov, C.H. Yang, D. Bush, S. Gosangari, S. Majuru, A. Fatmi, Design and characterization of a silk-fibroin-based drug delivery platform using naproxen as a model drug. J. Drug Deliv. (2012). https://doi.org/10.1155/2012/490514
P.R. Yadav, M.N. Munni, L. Campbell, G. Mostofa, L. Dobson, M. Shittu, S.K. Pattanayek, M.J. Uddin, D.B. Das, Translation of polymeric microneedles for treatment of human diseases: recent trends, progress, and challenges. Pharmaceutics 13(8), 1132 (2021)
R.F. Donnelly, T.R. Singh, M.J. Garland, K. Migalska, R. Majithiya, C.M. McCrudden, P.L. Kole, T.M. Mahmood, H.O. McCarthy, A.D. Woolfson, Hydrogel-forming microneedle arrays for enhanced transdermal drug delivery. Adv. Funct. Mater. 22(23), 4879–4890 (2012)
P. Joshi, P.R. Riley, W. Denning, S. Shukla, N. Khosla, J. Narayan, R. Narayan, Laser-patterned carbon coatings on flexible and optically transparent plastic substrates for advanced biomedical sensing and implant applications. J. Mater. Chem. C 10(8), 2965–2975 (2022)
A. Rajput, M. Kulkarni, P. Deshmukh, P. Pingale, A. Garkal, S. Gandhi, S. Butani, A key role by polymers in microneedle technology: a new era. Drug Dev. Ind. Pharm. (2022). https://doi.org/10.1080/03639045.2022.2058531
C.P.P. Pere, S.N. Economidou, G. Lall, C. Ziraud, J.S. Boateng, B.D. Alexander, D.A. Lamprou, D. Douroumis, 3D printed microneedles for insulin skin delivery. Int. J. Pharm. 544(2), 425–432 (2018)
M.A. Luzuriaga, D.R. Berry, J.C. Reagan, R.A. Smaldone, J.J. Gassensmith, Biodegradable 3D printed polymer microneedles for transdermal drug delivery. Lab Chip 18(8), 1223–1230 (2018)
H.S. Lee, H.R. Ryu, J.Y. Roh, J.H. Park, Bleomycin-coated microneedles for treatment of warts. Pharm. Res. 34(1), 101–112 (2017)
B. Pamornpathomkul, T. Ngawhirunpat, I.A. Tekko, L. Vora, H.O. McCarthy, R.F. Donnelly, Dissolving polymeric microneedle arrays for enhanced site-specific acyclovir delivery. Eur. J. Pharm. Sci. 121, 200–209 (2018)
S. Shukla, P.C. Pandey, R.J. Narayan, Tunable quantum photoinitiators for radical photopolymerization. Polymers 13(16), 2694 (2021)
M.C. Chen, H.A. Chan, M.H. Ling, L.C. Su, Implantable polymeric microneedles with phototriggerable properties as a patient-controlled transdermal analgesia system. J. Mater. Chem. B 5(3), 496–503 (2017)
T.M. Tuan-Mahmood, M.T.C. McCrudden, B.M. Torrisi, E. McAlister, M.J. Garland, T.R.R. Singh, R.F. Donnelly, Microneedles for intradermal and transdermal drug delivery. Eur. J. Pharm. Sci. 50(5), 623–637 (2013)
B. Cai, W. Xia, S. Bredenberg, H. Engqvist, Self-setting bioceramic microscopic protrusions for transdermal drug delivery. J. Materi. Chem. B 2(36), 5992–5998 (2014)
R. Byrne, P. Deasy, Use of commercial porous ceramic particles for sustained drug delivery. Int. J. Pharm. 246(1–2), 61–73 (2002)
P.C. Pandey, M.D. Mitra, S. Shukla, R.J. Narayan, Organotrialkoxysilane-functionalized noble metal monometallic, bimetallic, and trimetallic nanoparticle mediated non-enzymatic sensing of glucose by resonance rayleigh scattering. Biosensors 11(4), 122 (2021)
B. Cai, W. Xia, S. Bredenberg, H. Li, H. Engqvist, Bioceramic microneedles with flexible and self-swelling substrate. Eur. J. Pharm. Biopharm. 94, 404–410 (2015)
H. Vallhov, W. Xia, H. Engqvist, A. Scheynius, Bioceramic microneedle arrays are able to deliver OVA to dendritic cells in human skin. J. Mater. Chem. B 6(42), 6808–6816 (2018)
K. Ita, Ceramic microneedles and hollow microneedles for transdermal drug delivery: two decades of research. J. Drug Deliv. Sci. Technol. 44, 314–322 (2018)
R. Jamaledin, C. Di Natale, V. Onesto, Z.B. Taraghdari, E.N. Zare, P. Makvandi, R. Vecchione, P.A. Netti, Progress in microneedle-mediated protein delivery. J. Clin. Med. 9(2), 542 (2020)
O. Olatunji, Natural polymers: industry techniques and applications (Springer, Cham, 2015)
Y.H. Park, S.K. Ha, I. Choi, K.S. Kim, J. Park, N. Choi, B. Kim, J.H. Sung, Fabrication of degradable carboxymethyl cellulose (CMC) microneedle with laser writing and replica molding process for enhancement of transdermal drug delivery. Biotechnol. Bioprocess Eng. 21(1), 110–118 (2016)
P. Medhi, O. Olatunji, A. Nayak, C.T. Uppuluri, R.T. Olsson, B.N. Nalluri, D.B. Das, Lidocaine-loaded fish scale-nanocellulose biopolymer composite microneedles. AAPS PharmSciTech 18(5), 1488–1494 (2017)
W. Yu, G. Jiang, Y. Zhang, D. Liu, B. Xu, J. Zhou, Polymer microneedles fabricated from alginate and hyaluronate for transdermal delivery of insulin. Mater. Sci. Eng., C 80, 187–196 (2017)
K.Y. Hwa, V.H.S. Chang, Y.Y. Cheng, Y.D. Wang, P.S. Jan, B. Subramani, M.J. Wu, B.K. Wang, Analyzing polymeric matrix for fabrication of a biodegradable microneedle array to enhance transdermal delivery. Biomed. Microdevice 19(4), 1–13 (2017)
E.P. Yalcintas, D.S. Ackerman, E. Korkmaz, C.A. Telmer, J.W. Jarvik, P.G. Campbell, M.P. Bruchez, O.B. Ozdoganlar, Analysis of in vitro cytotoxicity of carbohydrate-based materials used for dissolvable microneedle arrays. Pharm. Res. 37(3), 1–18 (2020)
X. You, J.H. Chang, B.-K. Ju, J.J. Pak, Rapidly dissolving fibroin microneedles for transdermal drug delivery. Mater. Sci. Eng. C 31(8), 1632–1636 (2011)
J.A. Stinson, W.K. Raja, S. Lee, H.B. Kim, I. Diwan, S. Tutunjian, B. Panilaitis, F.G. Omenetto, S. Tzipori, D.L. Kaplan, Silk fibroin microneedles for transdermal vaccine delivery. ACS Biomater. Sci. Eng. 3(3), 360–369 (2017)
M. Zhu, Y. Liu, F. Jiang, J. Cao, S.C. Kundu, S. Lu, Combined silk fibroin microneedles for insulin delivery. ACS Biomater. Sci. Eng. 6(6), 3422–3429 (2020)
L. Hu, Z. Liao, Q. Hu, K.G. Maffucci, Y. Qu, Novel Bletilla striata polysaccharide microneedles: fabrication, characterization, and in vitro transcutaneous drug delivery. Int. J. Biol. Macromol. 117, 928–936 (2018)
Y. Zhang, G. Jiang, W. Yu, D. Liu, B. Xu, Microneedles fabricated from alginate and maltose for transdermal delivery of insulin on diabetic rats. Mater. Sci. Eng. C 85, 18–26 (2018)
S. Liu, M.N. Jin, Y.S. Quan, F. Kamiyama, H. Katsumi, T. Sakane, A. Yamamoto, The development and characteristics of novel microneedle arrays fabricated from hyaluronic acid, and their application in the transdermal delivery of insulin. J. Control. Release 161(3), 933–941 (2012)
S. Bhatnagar, P. Kumari, S.P. Pattarabhiran, V.V.K. Venuganti, Zein microneedles for localized delivery of chemotherapeutic agents to treat breast cancer: drug loading, release behavior, and skin permeation studies. AAPS PharmSciTech 19(4), 1818–1826 (2018)
E.M. Cahill, S. Keaveney, V. Stuettgen, P. Eberts, P. Ramos-Luna, N. Zhang, M. Dangol, E.D. O’Cearbhaill, Metallic microneedles with interconnected porosity: a scalable platform for biosensing and drug delivery. Acta Biomater. 80, 401–411 (2018)
S. Dharadhar, A. Majumdar, S. Dhoble, V. Patravale, Microneedles for transdermal drug delivery: a systematic review. Drug Dev. Ind. Pharm. 45(2), 188–201 (2019)
Z. Hu, C.S. Meduri, R.S. Ingrole, H.S. Gill, G. Kumar, Solid and hollow metallic glass microneedles for transdermal drug-delivery. Appl. Phys. Lett. 116(20), 203703 (2020)
H. Lee, S. Baek, E. Jeon, and J. Lee, Microneedle thermal flow sensor, in 2016 IEEE SENSORS, (2016), pp. 1–3: IEEE
P.R. Miller, S.D. Gittard, T.L. Edwards, D.M. Lopez, X. Xiao, D.R. Wheeler, N.A. Monteiro-Riviere, S.M. Brozik, R. Polsky, R.J. Narayan, Integrated carbon fiber electrodes within hollow polymer microneedles for transdermal electrochemical sensing. Biomicrofluidics 5(1), 013415 (2011)
J.R. Windmiller, N. Zhou, M.C. Chuang, G. Valdés-Ramírez, P. Santhosh, P.R. Miller, R. Narayan, J. Wang, Microneedle array-based carbon paste amperometric sensors and biosensors. Analyst 136(9), 1846–1851 (2011)
J.R. Windmiller, G. Valdés-Ramírez, N. Zhou, M. Zhou, P.R. Miller, C. Jin, S.M. Brozik, R. Polsky, E. Katz, R. Narayan, J. Wang, Bicomponent microneedle array biosensor for minimally-invasive glutamate monitoring. Electroanalysis 23(10), 2302–2309 (2011)
P.R. Miller, S.A. Skoog, T.L. Edwards, D.M. Lopez, D.R. Wheeler, D.C. Arango, X. Xiao, S.M. Brozik, J. Wang, R. Polsky, R.J. Narayan, Multiplexed microneedle-based biosensor array for characterization of metabolic acidosis. Talanta 88, 739–742 (2012)
A.V. Mohan, J.R. Windmiller, R.K. Mishra, J. Wang, Continuous minimally-invasive alcohol monitoring using microneedle sensor arrays. Biosens. Bioelectron. 91, 574–579 (2017)
P.C. Pandey, S. Shukla, G. Pandey, R.J. Narayan, Nanostructured diamond for biomedical applications. Nanotechnology 32, 132001 (2021)
S.A. Skoog, P.R. Miller, R.D. Boehm, A.V. Sumant, R. Polsky, R.J. Narayan, Nitrogen-incorporated ultrananocrystalline diamond microneedle arrays for electrochemical biosensing. Diam. Relat. Mater. 54, 39–46 (2015)
S. Song, J. Na, M. Jang, H. Lee, H.S. Lee, Y.B. Lim, H. Choi, Y. Chae, A CMOS VEGF sensor for cancer diagnosis using a peptide aptamer-based functionalized microneedle. IEEE Trans. Biomed. Circuits Syst. 13(6), 1288–1299 (2019)
B. Ciui, A. Martin, R.K. Mishra, B. Brunetti, T. Nakagawa, T.J. Dawkins, M. Lyu, C. Cristea, R. Sandulescu, J. Wang, Wearable wireless tyrosinase bandage and microneedle sensors: toward melanoma screening. Adv. Healthcare Mater. 7(7), 1701264 (2018)
M. Senel, M. Dervisevic, N.H. Voelcker, Gold microneedles fabricated by casting of gold ink used for urea sensing. Mater. Lett. 243, 50–53 (2019)
A. McConville, J. Davis, Transdermal microneedle sensor arrays based on palladium: polymer composites. Electrochem. Commun. 72, 162–165 (2016)
S. Samavat, J. Lloyd, L. O’Dea, W. Zhang, E. Preedy, S. Luzio, K.S. Teng, Uniform sensing layer of immiscible enzyme-mediator compounds developed via a spray aerosol mixing technique towards low cost minimally invasive microneedle continuous glucose monitoring devices. Biosens. Bioelectron. 118, 224–230 (2018)
K.B. Kim, W.C. Lee, C.H. Cho, D.S. Park, S.J. Cho, Y.B. Shim, Continuous glucose monitoring using a microneedle array sensor coupled with a wireless signal transmitter. Sens. Actuators B Chem. 281, 14–21 (2019)
P. Dardano, A. Caliò, V. Di Palma, M. F. Bevilacqua, A. Di Matteo, and L. De Stefano, Glucose sensing electrode system based on polymeric microneedles, in 2016 IEEE Sensors Applications Symposium (SAS), (2016), pp. 1–5: IEEE
H. Lee, T.K. Choi, Y.B. Lee, H.R. Cho, R. Ghaffari, L. Wang, H.J. Choi, T.D. Chung, N. Lu, T. Hyeon, S.H. Choi, D.H. Kim, A graphene-based electrochemical device with thermoresponsive microneedles for diabetes monitoring and therapy. Nat. Nanotechnol. 11(6), 566–572 (2016)
C. Hegarty, A. McConville, R.J. McGlynn, D. Mariotti, J. Davis, Design of composite microneedle sensor systems for the measurement of transdermal pH. Mater. Chem. Phys. 227, 340–346 (2019)
J. Valadeiro, M. Silva, S. Cardoso, M. Martins, J. Gaspar, P. P. Freitas, A. M. Sebastião, Microneedles with integrated magnetoresistive sensors: a precision tool in biomedical instrumentation, in 2017 IEEE Sensors Applications Symposium (SAS), (2017), pp. 1–6: IEEE
G.K. Mani, K. Miyakoda, A. Saito, Y. Yasoda, K. Kajiwara, M. Kimura, K. Tsuchiya, Microneedle pH sensor: direct, label-free, real-time detection of cerebrospinal fluid and bladder pH. ACS Appl. Mater. Interfaces 9(26), 21651–21659 (2017)
D. Al Sulaiman, J.Y. Chang, N.R. Bennett, H. Topouzi, C.A. Higgins, D.J. Irvine, S. Ladame, Hydrogel-coated microneedle arrays for minimally invasive sampling and sensing of specific circulating nucleic acids from skin interstitial fluid. ACS Nano 13, 9620–9628 (2019)
S.A.N. Gowers, D.M.E. Freeman, T.M. Rawson, M.L. Rogers, R.C. Wilson, A.H. Holmes, A.E. Cass, D. O’Hare, Development of a minimally invasive microneedle-based sensor for continuous monitoring of β-lactam antibiotic concentrations in vivo. ACS Sensors 4(4), 1072–1080 (2019)
R.K. Mishra, A.V. Mohan, F. Soto, R. Chrostowski, J. Wang, A microneedle biosensor for minimally-invasive transdermal detection of nerve agents. Analyst 142(6), 918–924 (2017)
F. Tehrani, H. Teymourian, B. Wuerstle, J. Kavner, R. Patel, A. Furmidge, R. Aghavali, H. Hosseini-Toudeshki, C. Brown, F. Zhang, K. Mahato, An integrated wearable microneedle array for the continuous monitoring of multiple biomarkers in interstitial fluid. Nature Biomedical Engineering 6, 1–11 (2022)
P. Bollella, S. Sharma, A.E.G. Cass, R. Antiochia, Microneedle-based biosensor for minimally-invasive lactate detection. Biosens. Bioelectron. 123, 152–159 (2019)
W. Gao, S. Emaminejad, H.Y.Y. Nyein, S. Challa, K. Chen, A. Peck, H.M. Fahad, H. Ota, H. Shiraki, D. Kiriya, D.H. Lien, Fully integrated wearable sensor arrays for multiplexed in situ perspiration analysis. Nature 529, 509–514 (2016)
Y. Ma, S.E. Boese, Z. Luo, N. Nitin, H.S. Gill, Drug coated microneedles for minimally-invasive treatment of oral carcinomas: development and in vitro evaluation. Biomed. Microdevice 17(2), 1–14 (2015)
P.C. Pandey, S. Shukla, Solvent dependent fabrication of bifunctional nanoparticles and nanostructured thin films by self assembly of organosilanes. J. Sol-Gel. Sci. Technol. 86, 650–663 (2018)
P.C. Pandey, M.D. Mitra, S. Shukla, R.J. Narayan, Organotrialkoxysilane-functionalized mesoporous Pd–Ni nanocatalyst for selective hydrazine decomposition and sensing. MRS Commun. 11, 78–85 (2021)
M.C. Chen, Z.W. Lin, M.H. Ling, Near-infrared light-activatable microneedle system for treating superficial tumors by combination of chemotherapy and photothermal therapy. ACS Nano 10(1), 93–101 (2016)
M.C. Chen, M.H. Ling, K.W. Wang, Z.W. Lin, B.H. Lai, D.H. Chen, Near-infrared light-responsive composite microneedles for on-demand transdermal drug delivery. Biomacromol 16(5), 1598–1607 (2015)
Y. Zhang, G. Jiang, W. Hong, M. Gao, B. Xu, J. Zhu, Gao Song, and Tianqi Liu, “Polymeric microneedles integrated with metformin-loaded and PDA/LA-coated hollow mesoporous SiO2 for NIR-triggered transdermal delivery on diabetic rats,.” ACS Appl. Bio Mater. 1(6), 1906–1917 (2018)
C. Wang, Y. Ye, G.M. Hochu, H. Sadeghifar, Z. Gu, Enhanced cancer immunotherapy by microneedle patch-assisted delivery of anti-PD1 antibody. Nano Lett. 16(4), 2334–2340 (2016)
M.-C. Kearney, E. Caffarel-Salvador, S.J. Fallows, H.O. McCarthy, R.F. Donnelly, Microneedle-mediated delivery of donepezil: potential for improved treatment options in Alzheimer’s disease. Eur. J. Pharm. Biopharm. 103, 43–50 (2016)
M. Leone, J. Mönkäre, J.A. Bouwstra, G. Kersten, Dissolving microneedle patches for dermal vaccination. Pharm. Res. 34(11), 2223–2240 (2017)
Y. Ye, J. Yu, D. Wen, A.R. Kahkoska, Z. Gu, Polymeric microneedles for transdermal protein delivery. Adv. Drug Deliv. Rev. 127, 106–118 (2018)
J.H. Park, M.G. Allen, M.R. Prausnitz, Polymer microneedles for controlled-release drug delivery. Pharm. Res. 23(5), 1008–1019 (2006)
A. Ono, S. Ito, S. Sakagami, H. Asada, M. Saito, Y.S. Quan, F. Kamiyama, S. Hirobe, N. Okada, Development of novel faster-dissolving microneedle patches for transcutaneous vaccine delivery. Pharmaceutics 9(3), 27 (2017)
H.T.T. Duong, N.W. Kim, T. Thambi, V.H.G. Phan, M.S. Lee, Y. Yin, J.H. Jeong, D.S. Lee, Microneedle arrays coated with charge reversal pH-sensitive copolymers improve antigen presenting cells-homing DNA vaccine delivery and immune responses. J. Control. Release 269, 225–234 (2018)
S. Sharma, Z. Huang, M. Rogers, M. Boutelle, A.E. Cass, Evaluation of a minimally invasive glucose biosensor for continuous tissue monitoring. Anal. Bioanal. Chem. 408(29), 8427–8435 (2016)
A.A. Ono, H. Azukizawa, S. Ito, Y. Nakamura, H. Asada, Y.S. Quan, F. Kamiyama, I. Katayama, S. Hirobe, N. Okada, Development of novel double-decker microneedle patches for transcutaneous vaccine delivery. Int. J. Pharm. 532(1), 374–383 (2017)
S. Bhatnagar, S.R. Chawla, O.P. Kulkarni, V.V.K. Venuganti, Zein microneedles for transcutaneous vaccine delivery: fabrication, characterization, and in vivo evaluation using ovalbumin as the model antigen. ACS Omega 2(4), 1321–1332 (2017)
S. Machekposhti, M. Soltani, P. Najafizadeh, S. Ebrahimi, P. Chen, Biocompatible polymer microneedle for topical/dermal delivery of tranexamic acid. J. Control. Release 261, 87–92 (2017)
Y. Lu, S.N. Mantha, D.C. Crowder, S. Chinchilla, K.N. Shah, Y.H. Yun, R.B. Wicker, J.W. Choi, Microstereolithography and characterization of poly (propylene fumarate)-based drug-loaded microneedle arrays. Biofabrication 7(4), 045001 (2015)
M.C. Chen, M.H. Ling, S.J. Kusuma, Poly-γ-glutamic acid microneedles with a supporting structure design as a potential tool for transdermal delivery of insulin. Acta Biomater. 24, 106–116 (2015)
A.R. Hutton, H.L. Quinn, P.J. McCague, C. Jarrahian, A. Rein-Weston, P.S. Coffey, E. Gerth-Guyette, D. Zehrung, E. Larrañeta, R.F. Donnelly, Transdermal delivery of vitamin K using dissolving microneedles for the prevention of vitamin K deficiency bleeding. Int. J. Pharm. 541, 56–63 (2018)
Funding
The NCSU authors were supported by National Science Foundation Awards 1762202 and 2029974.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Azizi Machekposhti, S., Khanna, S., Shukla, S. et al. Microneedle fabrication methods and applications. MRS Communications 13, 212–224 (2023). https://doi.org/10.1557/s43579-023-00355-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1557/s43579-023-00355-0