Abstract
Background
The risks of intensive blood glucose lowering may outweigh the benefits in vulnerable older people.
Objectives
Our primary aim was to determine whether age, frailty, or dementia predict discharge treatment types for patients with type 2 diabetes (T2D) and related complications. Secondly, we aimed to determine the association between prior hypoglycemia and discharge treatment types.
Design, Setting and Participants
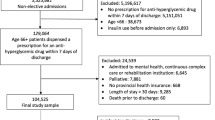
We conducted a cohort study involving 3,067 patients aged 65–99 years with T2D and related complications, discharged from Melbourne’s Eastern Health Hospital Network between 2012 and 2016.
Measurements
Multinomial logistic regression was used to estimate odds ratios (ORs) with 95% confidence intervals (CI) for the association between age, frailty, dementia and hypoglycemia, and being prescribed insulin-only, non-insulin glucose-lowering drugs (GLDs) or combined insulin and non-insulin GLDs compared to no GLD. International Classification of Diseases-10 codes were used to identify dementia status and prior hypoglycemia; frailty was quantified using the Hospital Frailty Risk Score.
Results
Insulin-only, non-insulin GLDs, combined insulin and non-insulin GLDs, and no GLDs were prescribed to 19%, 39%, 20%, and 23% of patients, respectively. Patients >80 years were less likely than patients aged 65–80 to be prescribed any of the GLD therapies, (eg. non-insulin GLDs [OR 0.67; 95%CI 0.55–0.82]), compared to no GLD. Similarly, high vs. low frailty scores were associated with not being prescribed any of the three GLD therapies, (eg. non-insulin GLDs [OR 0.63; 95%CI 0.45–0.87]). However, dementia was not associated with discharge prescribing of GLD therapies. Patients with a hypoglycemia-related admission were more likely than those not hospitalized with hypoglycemia to receive insulin-only (OR 4.28; 95%CI 2.89–6.31).
Conclusions
Clinicians consider age and frailty when tailoring diabetes treatment regimens for patients discharged from hospital with T2D and related complications. There is scope to optimize prescribing for patients with dementia and for those admitted with hypoglycemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The benefits of intensive glycemic control for preventing microvascular outcomes in middle and older age people with Type 2 diabetes (T2D) have been demonstrated in the ACCORD, ADVANCE, and VADT trials (1–3). However, intensive treatment is associated with an increased risk of hypoglycemia and does not improve survival or the incidence of macrovascular outcomes in people with limited life expectancies (1–3). The risks of intensive treatment may outweigh the benefits in frail older people (4). The guidelines of the American Diabetes Association (ADA) recommend less stringent glycemic targets of <8% and <8.5% (64 mmol/mol and 69 mmol/mol) for older individuals with complex and very complex health status (5). Similarly, Australian guidelines advise less intensive and individualized treatment for these patient groups (6). Nevertheless, UK data suggest that those who are frail and have dementia are treated with similar glucose-lowering drugs (GLDs) and with the aim to achieve similar glycemic targets as robust older people without dementia (7).
Frailty is an important complication of diabetes (8, 9), and is characterized by vulnerability to stressors and a reduced ability to maintain homeostasis (10). Frailty increases the risk of adverse drug events, including falls, disability and death (11). There are reciprocal relationships between hypoglycemia, dementia, and frailty (12). There have been calls for frailty status to guide treatment selection (13), with frail people with diabetes at 71% higher adjusted risk of all-cause hospitalization and twice the risk of mortality than non-frail people (14). Furthermore, older people with diabetes who develop dementia have three times the risk of hypoglycemia compared to those who do not develop dementia (15). The ACCORD-MIND study reported that cognitive decline over 20 months was associated with a higher risk of hypoglycemia regardless of treatment intensity (15).
Hospitalization represents an opportunity for clinicians to adjust T2D treatment regimens, although it is unclear to what extent hospital clinicians consider age, frailty and dementia in prescribing decisions. There is also a paucity of information about GLDs prescribed for older people who are frail and/or live with dementia, who may have different goals of care and treatment benefits and risks (5, 6). The primary aim of this study was to determine whether age, frailty, or dementia predict discharge treatment types for patients with T2D and related complications. Our secondary aim was to determine the association between prior hypoglycemia and discharge treatment types.
Methods
Data source, study design, and study population
The study was conducted at Eastern Health, a large metropolitan public hospital network in Melbourne, with three acute and four subacute hospitals (1,423 beds) (16). Eastern Health services a catchment area of 750,000 people and recorded 1,175,249 patient episodes between July 2015 and June 2016 (16). Eastern Health implemented an Electronic Medical Record (EMR) with electronic prescribing (e-prescribing) in 2011 (17). EMR discharge prescriptions record all medications intended for use by a patient after being discharged from the hospital (17). Demographic information and discharge diagnoses were extracted by the health service’s Decision Support Unit, which relies upon the standard practice of Clinical Coders within the Health information Unit (17). Diagnoses were recorded using International Classification of Diseases-10 (ICD-10) codes with up to 40 diagnoses per patient. Discharge medications were identified from the EMR using Anatomical Therapeutic Chemical (ATC) classification codes (18).
We conducted a cohort study of 3,067 adults aged between 65 and 99 years with T2D who were discharged from one of the Eastern Health hospital locations in Melbourne, Australia, between 2012 and 2016 with a principal diagnosis of T2D with a diabetes related complication.
Measures and definitions
Our study population included all patients with a principal diagnosis of T2D, identified using ICD-10 code E11, and an ICD-10 code (E11-E14) for a diabetes-related complication recorded at hospital discharge (index hospitalization) (18). Medications for T2D were broadly classified as insulins (ATC code A10A) or non-insulin GLDs (A10B). ATC codes used to identify GLDs classes are provided in Appendix A. A modified version of the Diabetes Complications Severity Index (DCSI) [19], which converts ICD-10 codes into a 13-level metric to quantify effects of diabetes on seven body systems, was used as an indicator of T2D severity. Although this version of the DCSI does not require laboratory data, validation studies have shown that its capacity to predict diabetes severity is comparable to other versions which do (19, 20). The DCSI is also likely to be indicative of diabetes duration as it has been shown that for every additional year of diabetes duration in people over 60 years, the adjusted odds of microvascular disease increases by 6% (p<0.001) (21).
We utilized a validated Hospital Frailty Risk Score, which categorizes people into three frailty categories based on the sum of weighted scores identified from International Classification of Diseases (ICD-10) codes (22). Gilbert et. al (2018) derived this score using 109 ICD-10 codes at least twice as prevalent in frail versus non-frail patients weighted according to how strongly they predict frailty (22). Codes used to derive the Hospital Frailty Risk Score (HFRS) reflect conditions linked to frailty (for example, volume depletion, cognitive impairment, and falls) or conditions overrepresented in frail populations such as lung disease, heart conditions and elective cataracts. Cut-point scores of <5, 5–15, and >15, as published by Gilbert et. al. indicated low, moderate, and high degrees of frailty, respectively. ICD-10 codes used to identify dementia and hypoglycemia are given in Appendix B.
Statistical analysis
Baseline characteristics were presented as means with standard deviations (SDs), medians with interquartile ranges (IQRs) or as frequencies and percentages. Predictors of treatment initiation were estimated using multinomial logistic regression. Variables were included in the final model if the unadjusted p-value associated with the odds ratio (OR) was <0.25. We included age (65-80 and >80), frailty (low, moderate or high) and dementia in our regression model and estimated adjusted odds ratios (ORs) with 95% confidence intervals (CI), adjusted for sex, index year, DCSI score, congestive cardiac failure (CCF), myocardial infarction (MI), renal disease, transient ischemic attack (TIA) or stroke, and hypoglycemia, (ICD-10 codes for comorbidities given in Appendix B). Variance Inflation Factors (VIF) with a cut-off of 2 were used to assess collinearity between the variables in the model. Statistical differences were evaluated using Pearson’s chisquared test and ANOVA for categorical and continuous variables, respectively. We excluded the Charlson Comorbidity Index (CCI) from our adjusted model because it was collinear with several comorbidities in our model, though it is included in Table 1 for completeness. Comorbidities and concomitant medications were not included in the same model because concomitant medications were conceptualized as intermediate variables in the causal pathway between the comorbidity and the diabetes treatment regimen.
All analyses were conducted using the statistical software package SAS version 9.4 (SAS Institute Inc., Cary, NC, USA). This study was approved by the Eastern Health and Monash University Human Research Ethics Committees (study number LR41/2017).
Results
Cohort Characteristics
Of the 3,067 people hospitalized with T2D, 19% were prescribed insulin-only, 39% non-insulin GLDs, 20% insulin and non-insulin combinations and 23% no GLDs (Table 1). Slightly less than half of the cohort were female (48%), and the mean age of the cohort was 78.6 years (SD 7.8). Patients not prescribed GLDs were older (81.0, SD 8.1) than those prescribed non-insulin GLDs (78.3, SD 7.7), insulin only (78.2, SD 7.3), or combination therapy (76.5, SD 7.3). Based on ICD-10 codes, 9% of the cohort had a dementia diagnosis, and 11% had been hospitalized with hypoglycemia.
Frailty scores were non-normally distributed, therefore medians and interquartile ranges (IQR) were reported. The median frailty score for the study population was 5.8 (IQR 2.5–10.2), with median frailty scores being higher amongst those who were not prescribed GLDs (6.9, IQR 3.0–11.5) and lower amongst those prescribed combinations (5.3, IQR 2.3–9.3), (Table 1). The Pearson correlation coefficient between age and frailty scores was 0.23 (p<0.0001).
Figure 1a) shows that 69.7% of patients prescribed insulin-only therapy had a DCSI score >1, p<0.0001. Figure 1b) indicates that 21.6% and 16.0% of the insulin-only and combination therapy groups had a documented prior hypoglycemia during their index hospitalization. In contrast, 5.7% and 6.7% of individuals receiving no GLD and noninsulin hypoglycemic agents had a documented episode of hypoglycemia, p<0.0001. Patients in the combination group were least likely (9.5%), to have a HFRS >15, p<0.0001 and to have dementia (4.3%), p=0.0002, (Figure 1c). Those with HFRS >15 were most likely (12.5%) to have had an episode of hypoglycemia, but this was not significantly higher than the other groups, p=0.16 (Figure 1d).
Predictors of Prescribed Anti-Hyperglycemic Therapy
People aged >80 versus those aged 65–80 were less likely to be prescribed insulin only (OR 0.54 95%CI 0.42–0.69), non-insulin GLDs only (OR 0.67 95%CI 0.55–0.82) or combinations of the two (OR 0.37 95%CI 0.29–0.47), compared to no GLDs (Table 2, Figure 2a). People with high frailty scores, compared to low scores, were less likely to be prescribed insulin only (OR 0.62 95%CI 0.42–0.91), non-insulin GLDs (OR 0.63 95%CI 0.45–0.87), or combinations of the two (OR 0.65 95%CI 0.43–0.96), compared to no GLDs (Table 2, Figure 2b).
People with dementia were less likely to be prescribed non-insulin GLDs (OR 0.73 95%CI 0.53–1.01) or insulin and non-insulin GLD combinations (OR 0.72 95%CI 0.47–1.10) compared to no GLDs, although these results were non-statistically significant (Table 2). People hospitalized with hypoglycemia, were more likely to receive insulin only (OR 4.28 95%CI 2.89–6.31) or combinations of insulin and non-insulin GLDs, (OR 3.15 95%CI 2.11–4.69), compared to no GLDs.
Types of T2D Therapy Prescribed
The most commonly prescribed insulin types within the group receiving insulin-only therapy were mixed (64.7%), fast-acting (30.0%) and long-acting (29.8%), with most individuals being prescribed either 1 (71.6%) or 2 (28.1%) different insulin products (Appendix C). Within the group receiving combination therapy, mixed (51.4%), long-acting (41.4%), and fast-acting (17.1%) insulins were most likely to be prescribed. All individuals in this group were prescribed either one (83.5%) or two (16.5%) types of insulin.
People in the non-insulin GLD group were most likely to be prescribed either metformin (69.9%) or a sulfonylurea (57.8%), with the majority being issued with either 1 (59.6%) or 2 (34.3%) non-insulin GLDs (Appendix C). Metformin (74.0%) and sulfonylureas (47.1%) were also the most commonly prescribed non-insulin GLDs in the combination group, and people in this group were most likely to receive either 1 (69.7%) or 2 (28.6%) non-insulin GLDs.
Discussion
This was the first study to investigate how age, frailty, and dementia predict hospital discharge prescribing for people with T2D. Older age and frailty predicted less intense treatment of T2D, people 80 and older were 63% less likely than those aged between 65–80 years to receive combinations of insulin and non-insulin GLDs, compared to no GLDs. Moreover, frail people were 35% less likely than robust people to be discharged on a combination of insulin and non-insulin GLDs versus no GLDs.
Our findings suggest clinicians consider age and frailty by tailoring diabetes treatment regimens. This is encouraging because frail older individuals are more vulnerable to adverse events, such as hypoglycemia and mortality (23). In addition, weight loss and sarcopenia associated with frailty (12) may be exacerbated by changes in the natural history of T2D, which shifts from a progressive to a regressive course in individuals who are frail (24). Older age is a well-known risk factor for hypoglycemia, and our findings demonstrate adherence to national and international prescribing guidelines, which advise that individuals with shorter life expectancy derive limited benefits from stringent glycemic targets (5, 6). Older people with T2D are also less likely to recognize early signs of hypoglycemia due to reduced awareness of hypoglycemic symptoms and slower reaction times than younger counterparts (25). Severe hypoglycemia can cause sudden cardiovascular death, and episodes of mild hypoglycemia can cause falls, fractures, cognitive impairment, seizures, coma, cardiovascular events, and arrhythmias (23). National estimates in the US indicate that insulin users >80 years are hospitalized for hypoglycemia or insulin-related errors at five times the rate of insulin users aged 45–64 years (26). Reasons postulated for this increase include reduced food intake and administration of the wrong insulin product (26).
People with dementia tended to be less likely to be discharged on insulin and non-insulin GLD combinations compared to no GLDs. Although not statistically significant, this result suggests possible increasing awareness of the need to align treatment with goals of care (27). It may also reflect prescribers’ awareness that individuals with dementia have a reduced capacity to manage complex regimens, particularly those involving insulin, due to difficulties in remembering dosage directions, to take doses on time or to take with food. Insulin and oral hypoglycemic agents such as sulfonylureas are considered high-risk medications and are associated with preventable hospitalizations, including among residents of nursing homes and long-term care facilities.
People hospitalized with hypoglycemia were over three times as likely to be prescribed insulin and non-insulin GLD combinations and over four times as likely to be prescribed insulin only compared to no GLDs. While we were not able to assess the clinical appropriateness of T2D regimens for individual patients, this suggests a possible opportunity for treatment de-intensification in ‘at risk’ population groups. It is also possible that there is scope for regimen simplification, as 28.5% of individuals prescribed insulin only and 16.5% prescribed combination treatment used at least two insulin products. It has been shown that simplification of multiple insulin regimens to basal insulin glargine only, reduced duration of hypoglycemia by 65% after eight months (28).
Strengths and limitations
Our study analyzed five years of discharge prescribing data from a large public hospital network in Melbourne. To our knowledge, this is the first study to investigate the impact of age, frailty, and dementia status as predictors of T2D discharge treatment intensity. One limitation of this study is that the Hospital Frailty Risk Score was validated for individuals >75 years, whereas we included individuals >65 years. The Hospital Frailty Risk Score was calculated using ICD-10 codes including dementia and, therefore, it is possible that there was overlap between dementia and frailty. Prescribing patterns may have evolved since 2016, particularly with the introduction of sodium-glucose cotransporter-2 inhibitors (SGLT-2Is). We considered age, dementia, and frailty status as categorical rather than continuous variables. However, age, frailty and dementia severity are continuous and there is no evidence for specific cut-points to define prescribing appropriateness in relation to these parameters. Lack of data on diabetes duration is a limitation. However, we presented the diabetes treatment according to less and more severe diabetes complications, which are related to diabetes duration (21). We did not have data on pre-admission treatment. However, we have presented the proportion of patients with documented prior hypoglycemia in each of the treatment groups. We hypothesized that prior hypoglycemia would prompt clinicians to modify treatment. Analyzing discharge prescribing is consistent with the treatment decision design in which cohorts are anchored at the point when treatment decisions are made (29). This is because medication regimens are typically evaluated during a hospital episode (29). Additionally, given that the sample comprised Australians who had been hospitalized, the results are not necessarily generalizable to all older patients with T2D across all clinical settings. We were not able to analyze data on HbA1C levels and ethnicity. Finally, a common limitation with the use of prescribing data, is that we do not know whether prescribed medications are actually taken by patients as directed.
Conclusion
Frail older people hospitalized with T2D and diabetes-related complications are less likely to be prescribed insulin-only GLDs, non-insulin GLDs or a combination of both, compared to no GLDs. Increasing age is also associated with receiving less intensive GLD regimens. Conversely, people hospitalized with hypoglycemia are considerably more likely to be discharged with a medication regimen which includes insulin. Clinicians appear to consider age and frailty when prescribing for people with T2D, but there is further opportunity for treatment de-intensification in ‘at risk’ groups.
References
The Action to Control Cardiovascular Risk in Diabetes Study Group, Effects of Intensive Glucose Lowering in Type 2 Diabetes. The New England Journal of Medicine, 2008. 358(24): p. 2545–2559.
Heller, S.R., A Summary of the ADVANCE Trial. Diabetes Care, 2009. 32(supplement 2): p. S357.
Duckworth, W., et al., Glucose Control and Vascular Complications in Veterans with Type 2 Diabetes. New England Journal of Medicine, 2009. 360(2): p. 129–139.
Abdelhafiz, A.H. and Sinclair, A.J., Deintensification of Hypoglycaemic Medications-use of a Systematic Review Approach to Highlight Safety Concerns in Older People with Type 2 Diabetes. Journal of Diabetes Complications, 2018. 32(4): p. 444–450.
American Diabetes Association, Older Adults: Standards of Medical Care in Diabetes—2018. Diabetes Care, 2018. 41(Supplement 1): p. S119.
RACGP. General Practice Management of Type 2 Diabetes 2016–2018. 2016.
Hambling, C.E., et al., Older People with Type 2 Diabetes, Including those with Chronic Kidney Disease or Dementia, are Commonly Overtreated with Sulfonylurea or Insulin Therapies. Diabetic Medicine, 2017. 34(9): p. 1219–1227.
Strain, W.D., et al., Type 2 Diabetes Mellitus in Older People: A Brief Statement of Key Principles of Modern Day Management Including the Assessment of Frailty. A National Collaborative Stakeholder Initiative. Diabetic Medicine, 2018. 35(7): p. 838–845.
Maddaloni, E., L. D’Onofrio, and P. Pozzilli, Frailty and Geography: Should These Two Factors Be Added to the ABCDE Contemporary Guide to Diabetes Therapy? Diabetes/Metabolism Research and Reviews, 2016. 32(2): p. 169–175.
Sinclair, A.J., Dunning, T., and Rodriguez-Mañas, L., Diabetes in Older People: New Insights and Remaining Challenges. The Lancet Diabetes & Endocrinology, 2015. 3(4): p. 275–285.
Liau, S.J., et al., Medication Management in Frail Older People: Consensus Principles for Clinical Practice, Research, and Education. Journal of the American Medical Directors Association, 2020. 22(1): p43–49.
Abdelhafiz, A.H., McNicholas, E., and Sinclair, A.J., Hypoglycemia, Frailty and Dementia in Older People with Diabetes: Reciprocal Relations and Clinical Implications. Journal of Diabetes Complications, 2016. 30(8): p. 1548–1554.
Orlandini, L. and Cesari, M., Should We Care More About Frailty When We Treat Diabetes? The Journal of Frailty & Aging, 2020. 9(2): p. 66–67.
Ferri-Guerra, J., et al., The Association of Frailty with Hospitalizations and Mortality among Community Dwelling Older Adults with Diabetes. The Journal of Frailty & Aging, 2020. 9(2): p. 94–100.
Punthakee, Z., et al., Poor Cognitive Function and Risk of Severe Hypoglycemia in Type 2 Diabetes. Diabetes Care, 2012. 35(4): p. 787.
Fanning, L., et al., Validity of Electronic Hospital Discharge Prescription Records as a Source of Medication Data for Pharmacoepidemiological Research. Therapeutic Advances in Drug Safety, 2018. 9(8): p. 425–438.
Fanning, L., et al., The Representativeness of Direct Oral Anticoagulant Clinical Trials to Hospitalized Patients with Atrial Fibrillation. European Journal of Clinical Pharmacology, 2017. 73(11):1427–1436.
Dugan, J. and Shubrook, J., International Classification of Diseases, 10th Revision, Coding for Diabetes. Clinical Diabetes. 2017. 35(4): p. 232–238.
Chang, H.-Y., et al., Validating the adapted Diabetes Complications Severity Index in claims data. The American Journal of Managed Care, 2012. 18(11): p. 721–726.
Glasheen, W.P., Renda, A., and Y. Dong, Diabetes Complications Severity Index (DCSI)-Update and ICD-10 translation. Journal of Diabetes Complications, 2017. 31(6): p. 1007–1013.
Nanayakkara, N., et al., Age, Age at Diagnosis and Diabetes Duration are all Associated with Vascular Complications in Type 2 Diabetes. Journal of Diabetes and its Complications, 2018. 32(3): p. 279–290.22.
Gilbert, T., et al., Development and Validation of a Hospital Frailty Risk Score Focusing on Older People in Acute Care Settngs using Electronic Hospital Records: an Observational Study. The Lancet, 2018. 391(10132): p. 1775–1782.
Sinclair, A.J., et al., Evaluating Glucose-Lowering Treatment in Older People with Diabetes: Lessons from the IMPERIUM Trial. Diabetes, Obesity & Metabolism, 2020.24.
Abdelhafiz, A.H., Koay, L., and Sinclair, A.J. The Effect of Frailty should be Considered in the Management Plan of Older People with Type 2 diabetes. Future Science OA, 2016. 2(1): p. FSO102–FSO102.25.
McCall, A.L., Insulin Therapy and Hypoglycemia. Endocrinology and Metabolism Clinics of North America, 2012. 41(1): p. 57–87.
Geller, A.I., et al., National Estimates of Insulin-Related Hypoglycemia and Errors Leading to Emergency Department Visits and Hospitalizations. JAMA Internal Medicine, 2014. 174(5): p. 678–86.
Reeve, E., J.S. Bell, and Hilmer, S.N., Barriers to Optimising Prescribing and Deprescribing in Older Adults with Dementia: A Narrative Review. Current Clinical Pharmacology, 2015. 10(3): p. 168–177.
Munshi, M.N., et al., Simplification of Insulin Regimen in Older Adults and Risk of Hypoglycemia. JAMA Internal Medicine, 2016. 176(7): p. 1023–1025.
Brookhart, M.A., Counterpoint: The Treatment Decision Design. American Journal of Epidemiology, 2015. 182(10): p. 840–845.
Acknowledgements
S.W. is supported through an Australian Government Research Training Program Scholarship. J.S.B. is supported by a NHMRC Boosting Dementia Research Leadership Fellowship [grant number #1140298].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest: J.S.B. has received grant income paid to his employer from NHMRC, Australian Government Department of Health, Victorian Government Department of Health and Human Services, Dementia Australia Research Foundation, Yulgilbar Foundation, GSK Independent Medical Education and several aged care provider organizations. M.C reports personal fees from Nestlé, outside the submitted work. J.I. reports grants from AstraZeneca, Amgen, Dementia Australia Research Foundation, National Health and Medical Research Council, and National Breast Cancer Foundation, outside the submitted work. S.W., D.J.M., L.F., and C.K. have no competing interests to declare.
Ethical standards: This study was approved by the Eastern Health and Monash University Human Research Ethics Committees (study number LR41/2017).
Supplemental Material
Rights and permissions
About this article
Cite this article
Wood, S.J., Bell, J.S., Magliano, D.J. et al. Impact of Age, Frailty, and Dementia on Prescribing for Type 2 Diabetes at Hospital Discharge 2012–2016. J Frailty Aging 10, 343–349 (2021). https://doi.org/10.14283/jfa.2021.6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.14283/jfa.2021.6