Abstract
Introduction
Despite the increasing widespread adoption and experience in minimally invasive liver resections (MILR), open conversion occurs not uncommonly even with minor resections and as been reported to be associated with inferior outcomes. We aimed to identify risk factors for and outcomes of open conversion in patients undergoing minor hepatectomies. We also studied the impact of approach (laparoscopic or robotic) on outcomes.
Methods
This is a post-hoc analysis of 20,019 patients who underwent RLR and LLR across 50 international centers between 2004–2020. Risk factors for and perioperative outcomes of open conversion were analysed. Multivariate and propensity score-matched analysis were performed to control for confounding factors.
Results
Finally, 10,541 patients undergoing either laparoscopic (LLR; 89.1%) or robotic (RLR; 10.9%) minor liver resections (wedge resections, segmentectomies) were included. Multivariate analysis identified LLR, earlier period of MILR, malignant pathology, cirrhosis, portal hypertension, previous abdominal surgery, larger tumor size, and posterosuperior location as significant independent predictors of open conversion. The most common reason for conversion was technical issues (44.7%), followed by bleeding (27.2%), and oncological reasons (22.3%). After propensity score matching (PSM) of baseline characteristics, patients requiring open conversion had poorer outcomes compared with successful MILR cases as evidenced by longer operative times, more blood loss, higher requirement for perioperative transfusion, longer duration of hospitalization and higher morbidity, reoperation, and 90-day mortality rates.
Conclusions
Multiple risk factors were associated with conversion of MILR even for minor hepatectomies, and open conversion was associated with significantly poorer perioperative outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Minimally invasive liver resection (MILR) has been an exciting new endeavour that is now an essential part of a hepatobiliary surgeon’s armamentarium. Commonly reported benefits of the minimally invasive approach include reduced blood loss, fewer complications, and shorter hospital stays.1,2 With the advent of surgical technology, refinement of patient selection, accumulation of surgical expertise, and development of anaesthetic protocols and experience, there are numerous robust studies in the current literature supporting improved perioperative outcomes with MILR compared with open liver resection (OLR).3,4,5,6,7,8 In addition, the 2014 Morioka consensus has proposed that MILR should be deemed the standard of care for minor liver resections.9 Subsequently, the Southampton Consensus Guidelines has reported that when performed by expert surgeons, MILR offers significant advantages in terms of reduced risk of post-operative ascites and liver decompensation in patients with cirrhosis.10 Small parenchymal volumes, straight and superficial transection lines, anteromedial location of tumors, and predictable vascular anatomy are just some of the anatomical and technical characteristics that make minor liver resections ideal procedures for MILR.11,12 Today, MILR for minor liver resections is generally accepted to be the “gold standard” of treatment for benign and malignant hepatic tumors at specialized hepatobiliary centers.9,13,14,15
In recent years, there has been an interest and trend toward increasing utilization of the robotic platform for MILR. Its implementation in liver surgery is encouraged by the purported advantages provided by the robotic platform, including a magnified, stable, and three-dimensional (3D) view of the operative field, increased degrees of freedom, and tremor filtration—all of which work synergistically to allow finer and more precise movements during dissection and suturing.16 The robotic platform additionally allows for convenient proctoring with dual consoles.17 These technical advantages contribute to a plethora of existing reports that suggest a shorter learning curve and improved perioperative outcomes with robotic liver resection (RLR).13,18,19,20,21,22 There has, however, been a woeful lack of high-quality evidence comparing the rates of and reasons for conversion between RLR and laparoscopic liver resection (LLR) and a subsequent comparison between outcomes of converted RLR and LLR cases.
Our study was designed to identify risk factors and assess outcomes after open conversion during MILR for minor hepatectomies. Additionally, we investigated whether outcomes of these converted cases differed significantly according to the reasons for conversion and the surgical approach (RLR vs. LLR). Unlike previous studies, we have used propensity-score matching (PSM) to reduce confounding baseline clinicopathological factors between successful MILR and converted cases, to ascertain factors independently predictive of conversion, and perioperative outcomes after conversion.
Methods
This was a retrospective review of 20,019 patients who underwent RLR and LLR across 50 international centers between 2004–2020. The study was approved by the institution review board of the coordinating center (Singapore General Hospital), which waived the need for patient consent. All other institutions obtained their respective approvals according to the local institution review board requirements. Anonymized data were collected in individual centers. This was collated and analyzed at Singapore General Hospital. This study was designed and the results were reported according to the Strengthening the Reporting of Observational Studies in Epidemiology statement.23
Only patients who underwent pure RLR or LLR were included. Laparoscopic-assisted (hybrid) and hand-assisted laparoscopic resections were excluded. After exclusion of patients who underwent technical major hepatectomies (MH; right anterior and right posterior sectionectomies), conventional MH, and left lateral sectionectomies (LLS), there were 12,222 patients. Patients who underwent multiple minor liver resections also were excluded. Finally, 10,541 cases met the study inclusion criteria; 1,148 (10.9%) patients underwent RLR, and 9,392 (89.1%) patients underwent LLR.
Definitions
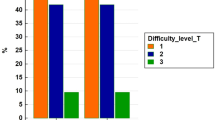
Liver resections were defined according to the 2000 Brisbane classification.24 Our study population consisted of patients undergoing wedge resections, segmentectomies, and bisegmentectomies. Of note, LLS and technical MH (right anterior and posterior sectionectomies) were excluded from our study in recognition of their complexity (wide surface area of parenchymal transection, posteriorly oriented transection plane) and as supported by multiple MILR difficulty scores.8,25,26,27,28 Difficult posterosuperior locations included tumors within segments I, VII, VIII, and IVa, whereas anterolateral segments included tumors in segments II, III, IVb, and VI. Difficulty of MILR was graded according to the IWATE score.26 Diameter of the largest lesion was used in the cases of multiple tumors. Reasons for open conversion were classified into bleeding-related, oncological reasons, and technical issues, such as dense adhesions, unable to localize tumor, slow progress, or injury to adjacent structures.
Our study period was divided into two equal intervals: 2004–2012; 2013–2020. This was included in the analyses of factors associated with open conversion (taking into account the learning curve and early adopter effect). Perioperative and postoperative outcomes were recorded for up to 30 days or during the same hospitalization. Postoperative morbidity was classified according to the Clavien-Dindo classification.29 Mortality was recorded up to 90 postoperative days.
Statistical Analyses
We used PSM to estimate the effect of open conversion on the surgical outcomes of patients who underwent minor liver resection. For propensity-score matching, the propensity score is estimated with logistic regression. The factors used in calculating the propensity score are the baseline variables stated in Table 1. Patients with open conversion are matched 1:1 by using nearest neighbor matching without replacement or discard, utilizing logit link, to patients without open conversion. To improve matching, a small caliper of 0.2 is used. During matching, any patient with missing data in any of the variables used for matching will be discarded. The same methodology is reapplied to propensity-score matching for open conversion due to bleeding versus nonbleeding reasons, and open conversion in RLR versus LLR approaches.
For unpaired comparisons of frequencies categorical variables, chi-squared is used. For the unpaired comparisons of median values and interquartile ranges, Mann-Whitney U test is used. For paired sample tests, McNemar's test is used for categorical variables and Wilcoxon signed-rank test is used for continuous variables not normally distributed.
Multivariate analysis of statistically significant variables is done via a generalized linear model. Odds ratio (OR) is expressed as odds of the first row to undergo open conversion compared with odds of the second row to undergo open conversion. Software used is RStudio version 1.4.1717, R version 4.1.0.
Results
A total of 20,019 patients underwent pure RLR and LLR, of which 10,541 cases met the final inclusion criteria. Of these patients, 1,148 (10.9%) underwent RLR, whereas 9,293 (89.1%) underwent LLR. The conversion rate was 2.4% (n = 27) and 5.4% (n = 510) for RLR and LLR respectively. Of total patients, 3,317 (31.5%) were cirrhotics with 957 (9.1%) suffering from concomitant portal hypertension. Of our study population, 6,894 (65.4%) underwent wedge resection, whereas the rest received anatomical hepatectomies. Of hepatectomies, 2,427 (23.0%) were of IWATE high/expert difficulty level. The overall conversion rate was 5.1% (n = 537) in the study population.
Risk Factors for Conversion to Open Surgery in Entire Population
Univariate and multivariate analysis of risk factors for open conversion are presented in Table 1. On multivariate analysis, LLR (OR 0.40; 95% confidence interval [CI] 0.27–0.59; p < 0.001), earlier period of MILR (OR 1.67; 95% CI 1.33–2.08; p < 0.001), malignant pathology (OR 1.40; 95% CI 1.05–1.89; p = 0.027), cirrhosis (OR 1.29; 95% CI 1.03-1.60; p = 0.028), portal hypertension (OR 1.51; 95% CI 1.12–2.02; p = 0.007), previous abdominal surgery (OR 1.36; 95% CI 1.13–1.64; p = 0.001), larger tumor size (OR 1.01; 95% CI 1.01–1.02; p < 0.001), and posterosuperior tumor location (OR 1.29; 95% CI 1.06–1.58; p = 0.012) were significant independent predictors of open conversion.
Outcomes of Successful MILR Versus Open Conversion: Entire Cohort
A comparison of the perioperative outcomes between patients undergoing successful MILR and those requiring open conversion is shown in Table 1. In the unmatched entire cohort, open conversion was associated with longer operative time (240.0 vs. 180.0; p < 0.001), higher blood loss (300.0 vs. 100.0; p < 0.001), greater need for intraoperative blood transfusions (20.7% vs. 4.9%; p < 0.001), longer duration of postoperative hospital stay (7.0 vs. 5.0; p < 0.001), higher postoperative all-morbidity (31.8% vs. 15.2%; p < 0.001), and major-morbidity (9.9% vs. 4.3%; p < 0.001), higher reoperation rates (2.8% vs. 1.0%; p < 0.001), and higher 30-day (0.9% vs. 0.1%; p < 0.001) and 90-day (1.3% vs. 0.3%; p < 0.001) mortality rates.
Outcomes of Successful MILR Versus Open Conversion: Matched Cohorts
After 1:1 PSM, two cohorts of 523 patients were analyzed. After matching, there were no remnant baseline clinopathological differences between patients undergoing successful MILR and open conversion except for portal hypertension (group undergoing successful MILR had significantly more patients with portal hypertension; p = 0.008). This comparison is demonstrated in Table 2.
In the analysis of perioperative outcomes in matched populations, patients undergoing successful MILR were associated with shorter median operative times (195.5 vs. 240.0; p < 0.001), less blood loss (152.0 vs. 300.0; p < 0.001), decreased need for blood transfusion (6.1% vs. 20.9%; p < 0.001), shorter duration of postoperative hospital stay (5.0 vs. 7.0; p < 0.001), lower postoperative all-morbidity (15.5% vs. 31.4%; p < 0.001) and major-morbidity (4.2% vs. 9.8%; p < 0.001), lower reoperation rates (0.4% vs. 2.9%; p = 0.003), and lower 90-day mortality rates (0.0% vs. 1.3%; p = 0.023).
Comparison of Outcomes of Conversions According to Reason or Conversion (Bleeding vs. Other Causes)
Reasons for open conversion in our study cohort are listed in Table 3. Technical issues were the most common reason for open conversion (44.7%), with uncontrolled bleeding being the second-most common reason (27.2%). Technical issues faced most commonly included adhesions, limited exposure, injury to surrounding structures, and failure of progression.
After 1:1 PSM, there were no significant baseline clinopathological differences between patients who underwent open conversion for uncontrolled bleeding versus other causes (Table 4). A comparison of outcomes demonstrated that patients who required open conversion because of uncontrolled bleeding had longer operative times (250.0 vs. 230.0; p = 0.047). Not unexpectedly, this group suffered from greater blood loss and a higher rate of intraoperative blood transfusions. However, there were no significant differences in terms of duration of postoperative hospitalization duration, morbidity, mortality, readmission, and reoperation rates.
Outcomes of Conversions According to MILR Approach (RLR vs. LLR)
Conversions occurred in 27 (2.4%) and 510 (5.4%) patients undergoing RLR and LLR respectively. After 1:1 PSM, it was found that patients who underwent open conversion with RLR were still more likely to possess multifocal disease than their counterparts undergoing open conversion during LLR (p < 0.001) (Table 5). There were no other significant baseline clinicopathological differences between patients who underwent open conversion as part of RLR or LLR. Our study reports no significant differences in perioperative outcomes of open conversion between the RLR and LLR group in terms of operative time, blood loss, hospitalization duration, morbidity, mortality, reoperation, and readmission.
Discussion
This study was designed to identify risk factors associated with open conversion of minor liver resections and to assess perioperative outcomes in patients who underwent open conversion. A substantial number of patients analyzed underwent RLR (n = 1,148), permitting analysis on the differences between RLR and LLR approaches with regards to rates of and outcomes after open conversion. We reported an overall conversion rate of 5.1%, a result largely comparable and reflective of the current literature available.1,2,30,31 The leading cause of open conversion in our study was technical difficulties, unlike previous studies that reported bleeding as the most common cause.30,31,32,33 With wedge resections and segmentectomies forming our study population, smaller parenchymal transection planes and decreased need for dissection and control of major Glissonian pedicles and hepatic veins makes uncontrolled hemorrhage a relatively lesser concern. Conversely, the posterosuperior and non-anatomical planes of transection commonly encountered in patients of our study population make for unergonomic and technically more demanding retraction and dissection, even compared with comparatively more “major resections,” such as left hepatectomies or LLS. In addition, this result could be explained by our study lacking a subgroup analysis under the “technical difficulties” category, a factor commonly subdivided in other studies into inability to identify the tumor, adhesions, difficulties with exposure, injury to surrounding structures or failure of progression.30,31,32,33
Remaining less common reasons for open conversion included anesthetic and oncological concerns. Given the prevalence of MILR for minor hepatectomies today, this study serves as an important guide for risk stratification and identification of patients at high risk for open conversion and offers an insight into the perioperative outcomes of these patients who undergo unexpected conversion. Importantly, this study is the first major study to make use of PSM to reduce confounding baseline clinicopathological biases when comparing outcomes of open conversion between different groups of patients (successful MILR vs. open conversion, conversion due to bleeding vs. other causes, RLR vs. LLR patients undergoing conversion).
Our study identified several factors independently associated with open conversion during MILR for minor hepatectomy. Cirrhosis and portal hypertension are factors commonly reported to be associated with increased technical difficulty of MILR.33,34,35,36,37 This is largely attributed to its association with coagulopathy, stiff parenchyma, distorted biliovascular anatomy, and difficult intraoperative localization of tumor margins (especially for deeply located lesions and lesions in postero-superior segments). Unsurprisingly, larger tumors also were strongly associated with higher rates of open conversion, likely because of technical difficulties in mobilization, extensive adhesions to surrounding structures, anatomical distortion, development of dense collaterals, and oncological concerns with obtaining clear margins.33,38,39,40 The association of MILR involving tumors in difficult posterosuperior locations and open conversion was not unexpected, given the recognition of this technically challenging approach amongst the majority of difficulty scores in today’s literature.25,26,27,28 Furthermore, with a large proportion of patients in our study undergoing nonanatomical wedge resections, tumor location proved to be a specifically important consideration given the need for optimal exposure and access to these posterosuperior locations (as opposed to patients undergoing anatomical hepatectomies where parenchymal transection lines may not require a similarly optimal exposure of the actual tumor location). An earlier period of MILR was expectedly associated with higher rates of open conversion, representing the early-adopter phenomenon and reflecting the learning curve that is associated with MILR.13 RLR was significantly associated with fewer open conversions compared with LLR, which may be attributed to the advantages of the robotic platform. However, these findings could possibly be attributed to better patient selection, increased surgeon experience in MILR, and a reluctance for a surgeon to convert to open surgery. Unsurprisingly, malignant pathology and previous abdominal surgery were found to be significant predictors of open conversion, largely attributable to technical difficulties with adhesions, exposure, mobilization, and obtaining surgical margins.
Our study confirms multiple, previous reports of poorer outcomes in patients undergoing MILR with open conversion.30,31,32,33,34,35,36,37,41,42 This association with poorer outcomes were, however, confounded by the significant association of patients undergoing open conversion with poorer baseline physiology and more unfavorable clinicopathological characteristics. As demonstrated in Table 1, patients undergoing open conversion were significantly associated with an earlier period of resection, higher rates of cirrhosis, previous abdominal surgery, higher ASA score, portal hypertension, multifocal disease, and a larger tumor size. In addition, open conversion amounts to a negation of all purported benefits of the minimally invasive approach. In an attempt to determine whether open conversion in itself was a significant risk factor for poorer perioperative outcomes, PSM matching was used to control for baseline clinicopathological differences. Results in Table 2 suggest that a failed MILR is in itself a strong contributory factor to poorer perioperative outcomes (longer operative time, more blood loss, and need for intraoperative transfusion, longer duration of hospital stay, lower postoperative morbidity, mortality, and reoperation rates). This is supported by multiple previous studies and highlights the importance of MIS surgeons selecting cases concordant with their level of expertise and experience, even in the context of MILR for minor hepatectomies being considered the standard of care in many tertiary institutions today.31,32,33
Additional analysis was performed on the outcomes of converted MILRs based on the reason for conversion (bleeding vs. nonbleeding causes). With no significant differences in baseline characteristics after PSM, our study demonstrated that apart from a longer operative time and expectedly greater blood loss, there were no other significant differences in perioperative outcomes based on the reason for conversion (duration of hospitalization, morbidity, mortality, readmission, and reoperation). This is contrary to previous reports, suggesting poorer outcomes (higher morbidity and mortality rates) associated with open conversion due to uncontrolled bleeding compared with other causes.30,31,33,41,42 In addition, the majority of current studies report uncontrolled bleeding as the most common reason for open conversion in contrast to technical difficulties in ours.30,31,32,33,34,41,42 One likely explanation for this is the inclusion of patients undergoing MH and LLS in almost all of these studies.33,42 The association of these procedures with larger parenchymal transection surfaces and the need for dissection, control, and ligation of major vascular and Glissonian structures makes uncontrolled bleeding a common concern in these operations. In contrast, wedge resections and segmentectomies have a smaller cut surface area and less commonly require the extent of dissection and hemostasis associated with major hepatic vasculature. Moreover, the majority of these studies report the extent of resection as a factor significantly predictive of open conversion in itself.30,33,41 This highlights the unique prevalence of technical challenges (adhesions, exposure, proximity, and injury to surrounding structures) in minor MILR compared with the primary concern of hemorrhage control in major hepatectomies, a phenomenon specifically exemplified in “minor hepatectomies” of a higher difficulty level with posterosuperiorly located parenchymal transection planes that makes exposure and dissection extremely unergonomic.
Our study reports a 60% risk reduction (OR 0.403) in conversion to open surgery with assistance from the robotic platform. The conversion rate for pure LLR (5.4%) was more than two times as high than when the robotic platform was used (2.4%). Furthermore, these results remained significant after multivariate analysis, indicating that utilization of the robotic platform is an independently significant predictor of successful MILR. Important comparisons can be made to two previous studies comparing the outcomes of LLR and RLR. Wang et al. reported on equivalent outcomes between LLR and RLR in a cohort of 2,445 patients undergoing MILR for LLS.42 In contrast, Montalti et al. reported significantly lower conversion rates with the RLR platform in a study that included 3,880 patients undergoing exclusively MH.33 With its relatively short and anterior parenchymal transection line, LLS has been widely regarded as the optimal procedure for MIS hepatobiliary surgeons mounting the learning curve.8,9,10,11,12 It has been postulated in previous studies that the benefits of a robotic platform are fully realized only in technically more demanding technical and conventional MH.23,33,42,43,44,45 Our study included patients undergoing MILR for wedge resections and segmentectomies and found a significantly lower conversion rate with the RLR platform as well. Of note, our study included 34.3% (n = 3,618) of patients with posterosuperior tumors, and 23.0% (n = 2,427) of patients who underwent IWATE high/expert difficulty resections. In line with abovementioned observations of the unique technical difficulties associated with wedge resections and segmentectomies in unfavourable locations, our study shows that the benefits of the robotic platform extends to patients undergoing minor hepatectomies as well. RLR provides a stable magnified view of the operative field, with articulating instruments providing much-required flexibility and maneuverability in unergonomic dissection planes. Furthermore, the fourth robotic arm provides stable organ retraction when dealing with larger tumors or a heavy right hepatic lobe.33
We performed comparisons in Table 5 between perioperative outcomes of converted patients after initial attempts at LLR versus RLR. No significant differences were found in terms of blood loss, operative time, morbidity, mortality, and reoperation rates. It has been a common fear amongst robotic surgeons that emergency conversion during robotic surgery represents a more challenging and time-consuming exercise, contributing to detrimental perioperative and postoperative outcomes. The main concern revolves around an inability to achieve swift and complete control of the operative field due to the time required for robot undocking. Of course, reluctance to convert once the robotic platform has been chosen because of higher costs considerations is a factor that cannot be denied.46 With wedge resections and segmentectomies, conversions to open largely arose from technical difficulties and nonprogression as opposed to uncontrolled bleeding. Conceivably, the additional minutes required for robot undocking and open conversion did not have significant impact on perioperative outcomes. The reduced rates of conversion and similar outcomes even when conversion is required suggests that RLR might be an ideal platform for difficult minor hepatectomies.
This study has important clinical implications, because it will serve as an important guide for surgeons embarking and performing MILR to enable better selection of patients for the minimally invasive approach. This will hopefully reduce the rate of unplanned open conversion, which we have demonstrated to be associated with worst outcomes. Although cost-analysis was not performed in this study, it is likely that an unplanned open conversion also would result in a significant cost increase as demonstrated with other laparoscopic procedures.47
Our study was associated with several limitations. The lack of a control group of patients undergoing planned open hepatectomy precludes a definitive comparison to clarify whether open conversion in itself is responsible for poorer perioperative outcomes. The retrospective nature of our study carries with selection biases, whereas PSM was only able to control for known confounders. While we were able to control for the early adopter effect (stratification according to time period), it was not possible to take into account individual surgeon experience and interinstitutional differences in expertise and infrastructure. Being an international study, there exists a degree of heterogeneity between selection criteria (for MILR), surgeon experience, anesthetic expertise, and postoperative protocols. Nevertheless, this heterogeneity contributes to the generalizability of our findings as well. Another potential confounder arises from the fact that the robotic platform is commonly utilized only by more experienced MILR surgeons with extensive exposure to LLR already.48,49 Lastly, inherent information biases associated with retrospective studies also could result in inaccuracies, such as the reason for open conversion.
Conclusions
Our study highlights the factors associated with open conversion in minor hepatectomies (wedge resections and segmentectomies). Patients undergoing open conversion had poorer outcomes compared with those undergoing successful MILR. There was no difference between perioperative outcomes when patients were analyzed according to the cause for open conversion (bleeding vs. nonbleeding). The robotic platform was shown to be a significant predictor for lower conversion rates, while demonstrating comparable perioperative outcomes even after open conversion. Larger randomized studies will have to be undertaken to confirm our results.
References
Fretland AA, Dagenborg VJ, Bjornelv GMW, et al. Laparoscopic versus open resection for colorectal liver metastases: the OSLO-COMET randomized controlled trial. Ann Surg. 2018;267(2):199–207.
Ciria, R., Cherqui, D. & Geller, D. A., et al. Comparative short-term benefits of laparoscopic liver resection: 9000 cases and climbing. Ann. Surg. 263(4), 761–77 (2016).
Vigano L, Tayar C, Laurent A, Cherqui D. Laparoscopic liver resection: a systematic review. J Hepatobiliary Pancreat Surg. 2009;16(4):410–21.
Simillis C, Constantinides VA, Tekkis PP, Darzi A, Lovegrove R, Jiao L, et al. Laparoscopic versus open hepatic resections for benign and malignant neoplasms–a meta-analysis. Surgery. 2007;141(2):203–11.
Nguyen KT, Marsh JW, Tsung A, Steel JJ, Gamblin TC, Geller DA. Comparative benefits of laparoscopic vs open hepatic resection: a critical appraisal. Arch Surg. 2011;146(3):348–56.
Lesurtel M, Cherqui D, Laurent A, Tayar C, Fagniez PL. Laparoscopic versus open left lateral hepatic lobectomy: a case-control study. J Am Coll Surg. 2003;196(2):236–42.
Buell JF, Thomas MT, Rudich S, Marvin M, Nagubandi R, Ravindra KV, et al. Experience with more than 500 minimally invasive hepatic procedures. Ann Surg. 2008;248(3):475–86.
Wakabayashi G. What has changed after the Morioka consensus conference 2014 on laparoscopic liver resection? Hepatobiliary Surg Nutr. 2016;5(4):281–9.
Wakabayashi G, Cherqui D, Geller DA, Buell JF, Kaneko H, Han HS, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg. 2015;261(4):619–29.
Hilal MA, Aldrighetti L, Dagher I, Edwin B, Troisi RI, Alikhanov R, Aroori S, Belli G, Besselink M, Briceno J, Gayet B. The Southampton consensus guidelines for laparoscopic liver surgery: from indication to implementation. Ann Surg. 2018;268(1):11–8.
Rao A, Rao G, Ahmed I. Laparoscopic left lateral liver resection should be a standard operation. Surg Endosc. 2011;25(5):1603–10.
Macacari RL, Coelho FF, Bernardo WM, Kruger JAP, Jeismann VB, Fonseca GM, et al. Laparoscopic vs. open left lateral sectionectomy: An update meta-analysis of randomized and non-randomized controlled trials. Int J Surg. 2019;61:1–10.
Chua D, Syn N, Koh YX, et al. Learning curves in minimally invasive hepatectomy: systematic review and meta-regression analysis. Br J Surg. 2021;108(4):351–8.
Kawaguchi Y, Hasegawa K, Wakabayashi G, Cherqui D, Geller DA, Buell JF, et al. Survey results on daily practice in open and laparoscopic liver resections from 27 centers participating in the second International Consensus Conference. J Hepatobiliary Pancreat Sci. 2016;23(5):283–8.
Dokmak S, Raut V, Aussilhou B, Fteriche FS, Farges O, Sauvanet A, et al. Laparoscopic left lateral resection is the gold standard for benign liver lesions: a case-control study. HPB (Oxford). 2014;16(2):183–7.
Goh BK, Teo RY. Current status of laparoscopic and robotic pancreatic surgery and its adoption in Singapore. Ann Acad Med Singap. 2020;49(6):377–83.
Troisi RI, Pegoraro F, Giglio MC, et al. Robotic approach to the liver: Open surgery in a closed abdomen or laparoscopic surgery with technical constraints? Surg Oncol. 2020;33:239–48.
Chen PD, Wu CY, Hu RH, et al. Robotic major hepatectomy: Is there a learning curve? Surgery. 2017;161(3):642–9.
Nomi T, Fuks D, Kawaguchi Y, et al. Learning curve for laparoscopic major hepatectomy. Br J Surg. 2015;102(7):796–804.
Kadam P, Sutcliffe RP, Scatton O, et al. An international multicenter propensity-score matched and coarsened-exact matched analysis comparing robotic versus laparoscopic partial liver resections of the anterolateral segments. J Hepatobiliary Pancreat Sci. 2022.
Ciria R, Berardi G, Alconchel F, et al. The impact of robotics in liver surgery: A worldwide systematic review and short-term outcomes meta-analysis on 2,728 cases. J Hepatobiliary Pancreat Sci. 2022;29(2):181–97.
Chiow AK, Fuks D, Choi GH, Syn N, Sucandy I, Marino MV, Prieto M, Chong CC, Lee JH, Efanov M, Kingham TP. International multicentre propensity score-matched analysis comparing robotic versus laparoscopic right posterior sectionectomy. Br J Surg. 2021;108(12):1513–20.
von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9.
Strasberg SM. Nomenclature of hepatic anatomy and resections: a review of the Brisbane 2000 system. J Hepatobiliary Pancreat Surg. 2005;12(5):351–5.
Hasegawa Y, Wakabayashi G, Nitta H, et al. A novel model for prediction of pure laparoscopic liver resection surgical difficulty. Surg Endosc. 2017;31(12):5356–63.
Kawaguchi Y, Fuks D, Kokudo N, et al. Difficulty of laparoscopic liver resection: proposal for a new classification. Ann Surg. 2018;267(1):13–7.
Halls MC, Berardi G, Cipriani F, et al. Development and validation of a difficulty score to predict intraoperative complications during laparoscopic liver resection. Br J Surg. 2018;105(9):1182–91.
Ban D, Tanabe M, Ito H, et al. A novel difficulty scoring system for laparoscopic liver resection. J Hepatobiliary Pancreat Sci. 2014;21(10):745–53.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Halls MC, Cipriani F, Berardi G, et al. Conversion for unfavorable intraoperative events results in significantly worse outcomes during laparoscopic liver resection: Lessons learned from a multicenter review of 2861 cases. Ann Surg. 2018;268(6):1051–7.
Goh BK, Chan CY, Wong JS, et al. Factors associated with and outcomes of open conversion after laparoscopic minor hepatectomy: initial experience at a single institution. Surg Endosc. 2015;29(9):2636–42.
Abu Hilal M, Underwood T, Taylor MG, et al. Bleeding and hemostasis in laparoscopic liver surgery. Surg Endosc. 2010;24(3):572–7.
Montalti R, Giglio MC, Wu AG, Cipriani F, D’Silva M, Suhool A, Nghia PP, Kato Y, Lim C, Herman P, Coelho FF. Risk factors and outcomes of open conversion during minimally invasive major hepatectomies: an international multicenter study on 3880 procedures comparing the laparoscopic and robotic approaches. Ann Surg Oncol. 2023. https://doi.org/10.1245/s10434-023-13525-0.
Ban D, Kudo A, Ito H, et al. The difficulty of laparoscopic liver resection. Updates Surg. 2015;67(2):123–8.
Kabir T, Tan ZZ, Syn NL, et al. Laparoscopic versus open resection of hepatocellular carcinoma in patients with cirrhosis: meta-analysis. Br J Surg. 2021;109(1):21–9.
Troisi RI, Berardi G, Morise Z, et al. Laparoscopic and open liver resection for hepatocellular carcinoma with Child-Pugh B cirrhosis: multicentre propensity score-matched study. Br J Surg. 2021;108(2):196–204.
Goh BKP, Syn N, Lee SY, et al. Impact of liver cirrhosis on the difficulty of minimally invasive liver resections: a 1:1 coarsened exact-matched controlled study. Surg Endosc. 2021;35(9):5231–8.
Levi Sandri GB, Spoletini G, Vennarecci G, et al. Laparoscopic liver resection for large HCC: short- and long-term outcomes in relation to tumor size. Surg Endosc. 2018;32(12):4772–9.
Cheung TT, Wang X, Efanov M, et al. Minimally invasive liver resection for huge (≥10 cm) tumors: an international multicenter matched cohort study with regression discontinuity analyses. Hepatobiliary Surg Nutr. 2021;10(5):587–97.
Kabir T, Syn N, Koh YX, et al. Impact of tumor size on the difficulty of minimally invasive liver resection. Eur J Surg Oncol. 2022;48(1):169–76.
Troisi RI, Montalti R, Van Limmen JG, et al. Risk factors and management of conversions to an open approach in laparoscopic liver resection: analysis of 265 consecutive cases. HPB (Oxford). 2014;16(1):75–82.
Wang HP, Yong CC, Wu AGR, et al. Factors associated with and impact of open conversion on the outcomes of minimally invasive left lateral sectionectomies: an international multicenter study. Surgery. 2022;172(2):617–24.
Tsung A, Geller DA, Sukato DC, et al. Robotic versus laparoscopic hepatectomy: a matched comparison. Ann Surg. 2014;259(3):549–55.
Chong CCN, Lok HT, Fung AKY, et al. Robotic versus laparoscopic hepatectomy: application of the difficulty scoring system. Surg Endosc. 2020;34(5):2000–6.
D’Silva M, Han HS, Liu R, et al. Limited liver resections in the posterosuperior segments: international multicetnre propensity score-matched and coarsened exact-matched analysis comparing the laparoscopic and robotic approaches. Br J Surg. 2022;109(11):1140–9.
Costi R, Scatton O, Haddad L, et al. Lessons learned from the first 100 laparoscopic liver resections: not delaying conversion may allow reduced blood loss and operative time. J Laparoendosc Adv Surg Tech A. 2012;22(5):425–31.
Shah AA, Bhatti U, Petrosyan M, et al. The heavy price of conversion from laparoscopic to open procedures for emergent cholecystectomies. Am J Surg. 2019;217:732–8.
Chong CC, Fuks D, Lee KF, et al. Propensity score-matched analysis comparing robotic and laparoscopic right and extended right hepatectomy. JAMA Surg. 2022;157(5):436–44.
Yang HY, Choi GH, Chin KM, et al. Robotic and laparoscopic right anterior sectionectomy and central hepatectomy: multicentre propensity score-matched analysis. Br J Surg. 2022;109(4):311–4.
Acknowledgment
Mikel Gastaca (Hepatobiliary Surgery and Liver Transplantation Unit, Biocruces Bizkaia Health Research Institute, Cruces University Hospital, University of the Basque Country, Bilbao, Spain). Juul Meurs (Department of Digestive and Hepatobiliary/Pancreatic Surgery, Groeninge Hospital, Kortrijk, Belgium). Celine De Meyere (Department of Digestive and Hepatobiliary/Pancreatic Surgery, Groeninge Hospital, Kortrijk, Belgium). Eric C. H. Lai (Department of Surgery, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China). Felix Krenzien (Department of Surgery, Campus Charité Mitte and Campus Virchow-Klinikum, Charité-Universitätsmedizin, Corporate Member of Freie Universität Berlin, and Berlin Institute of Health, Berlin, Germany). Kit-Fai Lee (Department of Surgery, Prince of Wales Hospital, The Chinese University of Hong Kong, New Territories, Hong Kong SAR, China). Pavel Tarakanov (Department of Hepato-Pancreato-Biliary Surgery, Moscow Clinical Scientific Center, Moscow, Russia). Ruslan Alikhanov (Department of Hepato-Pancreato-Biliary Surgery, Moscow Clinical Scientific Center, Moscow, Russia). Nita Thiruchelvam (Hepatopancreatobiliary Unit, Department of Surgery, Changi General Hospital, Singapore). Jae Young Jang (Department of General Surgery, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea). Kevin P. Labadie (Department of Surgery, University of Washington Medical Center. Seattle, USA). Masayuki Kojima (Department of Surgery, Fujita Health University School of Medicine, Aichi, Japan). Asmund Avdem Fretland (Interventional Centre and Department of HPB Surgery, Oslo University Hospital, Oslo, Norway). Jacob Ghotbi (Interventional Centre and Department of HPB Surgery, Oslo University Hospital, Oslo, Norway). Jaime Arthur Pirola Kruger (Liver Surgery Unit, Department of Gastroenterology, University of Sao Paulo School of Medicine, Sao Paulo, Brazil). Victor Lopez-Lopez (Department of General, Visceral and Transplantation Surgery, Clinic and University Hospital Virgen de la Arrixaca, IMIB-ARRIXACA, El Palmar, Murcia, Spain). Paolo Magistri (HPB Surgery and Liver Transplant Unit, University of Modena and Reggio Emilia, Modena, Italy). Giammauro Berardi (Division of General Surgery and Liver Transplantation, San Camillo Forlanini Hospital, Rome, Italy). Marco Colasanti (Division of General Surgery and Liver Transplantation, San Camillo Forlanini Hospital, Rome, Italy). Margarida Casellas I Robert (Hepatobiliary and Pancreatic Surgery Unit, Department of Surgery, Dr. Josep Trueta Hospital, IdIBGi, Girona, Spain). Edoardo Poletto (General and Hepatobiliary Surgery, Department of Surgery, Dentistry, Gynecology and Pediatrics University of Verona, GB Rossi Hospital, Verona, Italy). Federica Cipriani (Hepatobiliary Surgery Division, IRCCS San Raffaele Hospital, Milan, Italy). Mizelle D’Silva (Department of Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seoul, Korea). Roberto Montalti (Department of Public Health, Division of HPB, Minimally Invasive and Robotic Surgery, Federico II University Hospital Naples, Naples, Italy). Hao-Ping Wang (Department of Surgery, Chang Gung Memorial Hospital, Kaohsiung). Shian Yu (Department of Hepatobiliary Surgery, Affiliated Jinhua Hospital, Zhejiang University School of Medicine, Jinhua, China). Zewei Chen (Department of Hepatobiliary Surgery, Affiliated Jinhua Hospital, Zhejiang University School of Medicine, Jinhua, China). Simone Vani (Hepatobiliary Surgery Unit, Fondazione Policlinico Universitario A. Gemelli, IRCCS, Catholic University of the Sacred Heart, Rome, Italy). Francesco Ardito (Hepatobiliary Surgery Unit, Fondazione Policlinico Universitario A. Gemelli, IRCCS, Catholic University of the Sacred Heart, Rome, Italy). Ugo Giustizieri (HPB Surgery, Hepatology and Liver Transplantation, Fondazione IRCCS Istituto Nazionale Tumori di Milano, Milan, Italy). Davide Citterio (HPB Surgery, Hepatology and Liver Transplantation, Fondazione IRCCS Istituto Nazionale Tumori di Milano, Milan, Italy). Federico Mocchegiani (HPB Surgery and Transplantation Unit, United Hospital of Ancona, Department of Experimental and Clinical Medicine Polytechnic University of Marche). Fabio Forchino (Department of General and Oncological Surgery. Mauriziano Hospital, Turin, Italy). Epameinondas Dogeas (Department of Surgery, Division of Hepatobiliary and Pancreatic Surgery, University of Pittsburgh Medical Center, Pittsburgh, PA, USA). Tiing Foong Siow (Division of General Surgery, Far Eastern Memorial Hospital, New Taipei City, Taiwan).
Funding
Dr. T. P. Kingham was partially supported by the US National Cancer Institute MSKCC Core Grant number P30 CA008747 for this study. Dr. M. Yin was partially funded by the Research Project of Zhejiang Provincial Public Welfare Fund project in the Field of Social development (LGF20H160028).
Author information
Authors and Affiliations
Consortia
Contributions
Dr. Goh BK has received travel grants, honorarium and research grants from Johnson and Johnson, Olympus, and Intuitive Surgery. Dr. Marino MV is a consultant for CAVA robotics LLC. Dr Pratschke J reports a research grant from Intuitive Surgical Deutschland GmbH and personal fees or nonfinancial support from Johnson & Johnson, Medtronic, AFS Medical, Astellas, CHG Meridian, Chiesi, Falk Foundation, La Fource Group, Merck, Neovii, NOGGO, pharma-consult Peterson, and Promedicis. Dr Schmelzle M reports personal fees or other support outside of the submitted work from Merck, Bayer, ERBE, Amgen, Johnson & Johnson, Takeda, Olympus, Medtronic, Intuitive. Dr Rotellar F reports speaker fees and support outside the submitted work from Integra, Medtronic, Olympus, Corza, Sirtex, and Johnson & Johnson. Dr Troisi R reports speaker fees and support outside the submitted work from Integra, Stryker, Medtronic, Medistim, MSD. Dr. López-Ben S reports Grants from Johnson & Johnson, Baxter, and Abex.
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Saleh, M., Pascual, F., Ghallab, M. et al. Factors Associated with and Impact of Open Conversion in Laparoscopic and Robotic Minor Liver Resections: An International Multicenter Study of 10,541 Patients. Ann Surg Oncol 31, 5615–5630 (2024). https://doi.org/10.1245/s10434-024-15498-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-024-15498-0