Abstract
Background
The advantages of the robotic approach in minimally invasive liver surgery (MILS) are still debated. This study compares the short-term outcomes between laparoscopic (LLR) and robotic (RLR) liver resections in propensity score matched cohorts.
Methods
Data regarding minimally invasive liver resections in two liver surgery units were retrospectively reviewed. A propensity score matched analysis (1:1 ratio) identified two groups of patients with similar characteristics. Intra- and post-operative outcomes were then compared. The difficulty of MILS was based on the IWATE criteria.
Results
Two hundred sixty-nine patients underwent MILS between January 2014 and December 2021 (LLR = 192; RLR = 77). Propensity score matching identified 148 cases (LLR = 74; RLR = 74) consisting of compensated cirrhotic patients (100%) underwent non-anatomic resection of IWATE 1–2 class (90.5%) for a solitary tumor < 5 cm in diameter (93.2%). In such patients, RLRs had shorter operative time (227 vs. 250 min, p = 0.002), shorter Pringle’s cumulative time (12 vs. 28 min, p < 0.0001), and less blood loss (137 vs. 209 cc, p = 0.006) vs. LLRs. Conversion rate was nihil (both groups). In RLRs compared to LLRs, R0 rate (93 vs. 96%, p > 0.71) and major morbidity (4.1 vs. 5.4%, p > 0.999) were similar, without post-operative mortality. Hospital stay was shorter in the robotic group (6.2 vs. 6.6, p = 0.0001).
Conclusion
This study supports the non-inferiority of RLR over LLR. In compensated cirrhotic patients underwent resection of low-to-intermediate difficulty for a solitary nodule < 5 cm, RLR was faster, with less blood loss despite the shorter hilar clamping, and required shorter hospitalization compared to LLR.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Minimally invasive surgery (MILS) is spreading among liver surgeons. The advantages of MILS over the classic open approach (open liver resection, OLR) have been showed for both short- and long-term outcomes for healthy livers and in the setting of chronic liver disease [1, 2]. Moreover, MILS seems to provide similar oncologic results to OLR for hepatocellular carcinoma (HCC) and colorectal liver metastases (CRLM) [3,4,5,6].
MILS can be performed with two approaches: laparoscopic liver resection (LLR) and the more recently refined robotic-assisted liver resection (RLR). The latter has been introduced in 2003 by Giulianotti et al. [7]. There are theoretical advantages of RLR over LLR, such as an easier access to posterior–superior liver segments (once considered “non-laparoscopic” segments) [8]. The robotic instruments provide a vast range of motion thanks to the augmented dexterity of the robotic wrist, allowing a better exposure of narrow cavities, easier dissection, easier vascular and biliary reconstruction, better control of unexpected bleeding, and optimal camera stability [2, 9]. A shorter learning curve has also been suggested for RLR in comparison to LLR [10,11,12]. However, it must be noted that in most of surgical realities robotic liver surgery programs are developed once a solid experience in laparoscopic liver surgery is achieved, while only few centers reported the introduction of the two MILS techniques at the same time [13,14,15]. In a technical perspective, laparoscopic liver surgery disposes of a specific hepatic parenchymal dissection (CUSA) which is not currently available for the robotic platform; though, surgeons recur to the classic “clamp-crush” technique with the robotic instruments or to a hybrid technique using the laparoscopic CUSA handled by a second surgeon at the table (the so-called “RoboLap” approach) [16,17,18,19].
In recent years, awareness emerged on the fact that the difficulty of MILS does not rely merely on the number, size of the tumor, or volume of the resected liver, but it may be rather the resultant of several factors. Accordingly, difficulty score systems have been originally developed to optimize the selection of candidates for laparoscopic hepatectomy [20,21,22]. These criteria have been subsequently validated in the setting of RLR, providing a reliable tool to select patients for MILS irrespective of the technique (either LLR or RLR) and to compare the results of RLRs and LLRs [23,24,25,26].
In summary, despite more than 15 years of co-existence, the superiority of one MILS technique over the other has not been confirmed [2, 27,28,29].
With this study we compare the short-term results of RLRs and LLRs stratified according to the IWATE criteria. For the purpose of the study, we hypothesized the non-inferiority of the robotic approach over the well-settled laparoscopy for liver resections.
Methods
Study design and setting
This is a retrospective analysis of patients who underwent minimally invasive liver resections (either robotic or laparoscopic) at two referral centers: the Hepatobiliary surgery and Liver transplant Unit at the University of Pisa Medical School Hospital in Italy (robotic and laparoscopic procedures) where the MILS program was developed alongside the activity of liver transplantation (LT) and the Hepatobiliary surgery Unit at the Regional Hospital of Lugano, Switzerland (laparoscopic procedures). The study period ranged from January 2014 to 31st December 2021. Patients were followed up for at least 90 days after surgery. This study was conducted in compliance with the STROBE guidelines for reporting observational studies [30].
Participants
All MILS patients and relative procedures were extracted from each institute’s prospectively maintained database and were reviewed. We focused on population features, tumors, details of the surgical procedures, and surgery-related outcomes.
One of the centers (Pisa) provide high-volume liver transplant activity alongside liver resections, within a region (Tuscany, Italy) where the overall donor rate reach up to 49 per million of population (www.trapianti.salute.gov.it). In this center HCC represents roughly 40% of the indications to liver transplant. The allocation of patients to resection or transplantation was initially based on the BCLC criteria and then the indications to liver transplant progressively expanded following the Extended Toronto criteria and a treatment hierarchy policy [31,32,33,34]. Practically, MILS was considered first in the case of a single HCC with favorable location (i.e., subcapsular) in the setting of compensated cirrhosis (i.e., Child A) with or without signs of portal hypertension, especially when contraindications to liver transplant exist (i.e., age > 70 years old, general comorbidities, refusal of the patient to undergo liver transplant). MILS could be eventually followed by salvage transplantation in case of liver-limited recurrence or liver function decompensation in selected cases as described elsewhere [15]. Liver transplant was the first option considered in case of single-nodule patients with advanced cirrhosis or with 2 or more HCC nodules. However, in the presence of the abovementioned contraindications, resection may be offered to those patients.
Inclusion criteria
Elective minimally invasive liver resections (either robotic or laparoscopic) for malignant or benign indications based on intention-to-treat principle in adult patients (> 18 years). Cirrhotic patients were considered for MILS at both institutions in case of well-compensated cirrhosis (Child–Pugh score A or B).
Exclusion criteria
Hand-assisted procedures, cyst’s fenestration, and non-elective surgery.
Patients were divided in two groups according to the minimally invasive technique used to perform the resection: robotic liver resection (RLR) or laparoscopic liver resection (LLR). All resections were stratified as per level of difficulty according to the IWATE criteria [22]. In case of patients with multiple liver resections, the resection with the highest score was considered to calculate the difficulty index. Type of resections were defined according to the updated Brisbane nomenclature [35]. Posterior–superior segments of the liver were defined as Segment 4a, 7, 1, and 8. Parenchymal sparing surgery (PSS) was adopted whenever oncologically and technically feasible.
Surgery details
Laparoscopic approach
Patients were placed in dorsal decubitus with French position (open legs) or left partial decubitus according to the location of the tumor to be resected (i.e., left partial decubitus for resection involving the posterior–superior liver segments). The surgeon operated standing between the legs in most of the cases or standing at the right of the patient (i.e., resection involving the posterior–superior liver segments) with the assistant on the left and/or the right side of the patient. Four to five operative ports were placed along a J-shaped line that could be used in case of conversion to open surgery. Parenchymal transection was performed by laparoscopic CUSA in both the institutions. Pringle maneuver was used according to surgeon’s preference.
Robotic approach
The robotic procedures were performed using the Da Vinci Si® for few cases at the beginning of the experience and then with Da Vinci Xi® robotic platform (Intuitive). In case of resections involving the antero-lateral liver segments, the patient was placed in supine position. A total of 4 or 5 ports were used: three-to-four 8-mm ports for the robotic instruments (monopolar scissors, bipolar forceps, or Maryland® bipolar forceps, prograsp, robotic vessel sealer) and the camera in a transversal linear fashion and one 11-mm assistance port in umbilical (resections in segments 2 and 3) or left para-umbilical position (resections in segment 4). In case of resections in the posterior–superior segments or in the right hemi-liver, we used three-to-four 8-mm ports for robotic instruments and camera in a right subcostal linear approach, with one 11-mm assistance port along the right pararectal line (resections in segments 6 and 7) or in umbilical position (resections in segments 5 and 8). Parenchymal transection was performed by the clamp-crush technique; laparoscopic assistance with CUSA was not used in robotic procedures. Pringle maneuver was applied according to surgeon’s preference.
For both LLR and RLR, intra-operative ultrasound (IO-US) was routinely performed to assess the anatomy of the liver, the relation within tumors and intra-hepatic vessels or biliary structures, and to confirm resectability.
All the procedures were performed by senior hepatobiliary surgeons who were in their learning curve for MILS during the study period (both the institutions). As previously published, in the center of Pisa robotic and laparoscopic liver surgery programs were introduced simultaneously [15]. Indication to surgery was validated case by case by weekly multidisciplinary team discussion and according to current guidelines.
Variables and outcomes
The endpoint of the study was the non-inferiority of RLR over LLR. The outcomes of interest were operative time, adoption and duration of Pringle’s maneuver, conversion to open surgery, intraoperative blood loss, 90-day overall and major post-operative morbidity (complications), and 90-day mortality rates. Complications were graded according to Clavien–Dindo classification of surgical complications; major complications included grade IIIA or higher complications [36]. Bile leak was categorized according the International study group for liver surgery (ISGLS) definition [37].
Statistical analysis
According to their level of measurement and distribution, continuous variables were expressed as means and standard deviations (SD) or medians and ranges, while categorical variables were described as frequencies. Data were compared with the t test for continuous values with normal distribution, the Mann–Whitney U test or Kruskal–Wallis test for continuous values without normal distribution, and the Pearson’s χ2 or Fisher’s exact tests for categorical values. The level of significance was set at 5%. A 1:1 propensity score matching (PSM) analysis was performed to reduce the risk of selection bias. We included in the PSM the following 4 variables: underlying cirrhosis (yes or no), previous abdominal surgery (yes or no), size of the largest lesion (≥ 5 cm), and technical difficulty according to the IWATE score (1 = low; 2 = intermediate; 3 = advanced; 4 = expert). All analyses were conducted with MedCalc® Statistical Software version 22.002 (MedCalc Software Ltd, Ostend, Belgium; https://www.medcalc.org; 2023).
Results
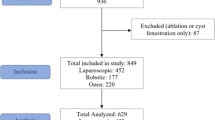
A total of 269 patients underwent MILS in the two institutions between January 2014 and October 2021 (LLR = 192; RLR = 77).
Before PSM analysis
Descriptive data
At baseline before the PSM analysis, LLR and RLR population were similar in terms of age (both mean age of 66, p = 0.74), male sex (63.6 vs. 57.3%, p = 0.63), mean BMI (26.0 vs. 25.0 kg/m2, p = 0.05), and previous abdominal and liver surgery rate (respectively, 59.0 vs. 53.0%, p = 0.66 and 8.6 vs. 10.4%, p = 0.72). Chronic liver disease was significantly more frequent in RLR cohort (100 vs. 61.5%, p < 0.01). In LLR group, there was a higher number of nodules per patient of 312/192 (1.6) vs. 87/77 (1.1) in RLR (p = 0.007) without differences in median size (24.0 vs. 25.0 mm, p = 0.30). Tumor location did not differ between the two groups except for segment 8 which was more frequently involved in RLR than in LLR group (25.3 vs. 13.1%, p = 0.02) and segment 1 which tended to be more frequently involved in RLR (2.3 vs. 0.3%, p = 0.06).
Procedures consisted in wedge or non-anatomic resections (61.5 vs. 84.4%, p = 0.12), followed by segmentectomies (16.7 vs. 7.8%, p = 0.10), bi-segmentectomies (13.5 vs. 5.2%, p = 0.074), and major hepatectomies (8.3 vs. 0%), respectively, in LLR vs. RLR group. Pringle maneuver was used more often during laparoscopic vs. robotic procedures (60.0 vs. 21.0%, p = 0.0003) but the median duration of hilar clamping was similar (40.0 vs. 45.0 min, p = 0.60 for LLR and RLR, respectively). Of note, the laparoscopic group consisted in more difficult resections (mean IWATE score of 4.9 vs. 4.3; p = 0.047 in LLRs vs. RLRs, respectively), with 10% of expert level resections which instead were absent in the robotic group.
Outcomes
Operative time was longer in LLRs vs. RLRs (median of 270 vs. 210 min, p = 0.0001), but conversion rate was not significantly different (14.0 vs. 9.1, p = 0.32) as well as intraoperative transfusion rate (2.1 vs. 2.6%, p = 0.80), intraoperative estimated blood loss (median of 100 ml in each group, p = 0.13), and length of hospital stay (median of 6 days in each group, p = 0.16). 90-day morbidity and major morbidity rate also did not differ significantly in both groups (21.0 vs. 18.0%, p = 0.70 and 6.2 vs. 3.9%, p = 0.50, respectively). 90-day mortality was nihil in the entire series. R0 rate was 94.0 vs. 92% (p = 0.92) in LLRs vs. RLR.
Indications to surgery and the subsequent final pathology were also slightly different in the two groups: the robotic group consisted mainly of patients with HCC (88%) with underlying cirrhosis; while in the laparoscopic cohort the indications were more evenly distributed, with the most frequent being HCC (46%), followed by CRLM (22.4%), other liver metastases (14%), benign tumors (10%), and intra-hepatic cholangiocarcinoma (iCCA) (5.7%). Baseline characteristics of the unmatched populations, procedures, and outcomes before the PSM are reported in Table 1. Intra- and post-operative results of MILS stratified by the technique used and by level of difficulty (IWATE criteria) are provided in Supplementary Material, Table S1. The final pathology after MILS in the unmatched population is reported in Supplementary Material, Table S2.
After PSM analysis
Descriptive data
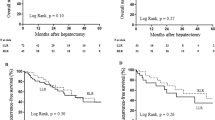
After a 1:1 PSM a total of 148 cases were included in the analysis (LLR = 74; RLR = 74). The two cohorts of patients were well balanced in terms of baseline characteristics. The propensity score analysis identified two subgroups represented by well-compensated cirrhotic patients (100%) who underwent non-anatomic liver resection (laparoscopic or robotic) of IWATE 1–2 class (90.5%) and 3–4 (9.5%) mostly for a solitary nodule of < 5 cm diameter (93.2%). Final pathology revealed HCC in 85.1 vs. 70.3% of RLRs and LLRs. The distribution of the procedures according to the difficulty score after the PSM is reported in Fig. 1. The balanced characteristics of LLR and RLR cohorts before and after PSM are displayed in Table 2. The final pathology and the liver status of laparoscopic and robotic resections after the PSM are summarized in Supplementary material Table S3.
Outcomes
After the PSM analysis, the robotic group had significantly shorter operative time [227 (78) vs. 250 (104) min, p = 0.002], shorter Pringle’s cumulative time [12 (23) vs. 28 (27) min, p ≤ 0.0001], and less blood loss [137 (71) vs. 209 (179) cc, p = 0.006] vs. the laparoscopic group. The R0 resection rate [69 (93%) vs. 71 (96%), p > 0.71] was similar in RLRs vs. LLRs, and the conversion rate was nihil in both groups. Regarding post-operative outcomes, the robotic group had similar post-operative major morbidity [3 (4.1) vs. 4 (5.4), p > 0.999], as well as incidence of bile leak [0 (0) vs. 4 (5.4%), p > 0.11] (all grade A according to ISGLS definition). Post-operative mortality was nihil in both groups. Patients who underwent robotic hepatectomy had shorter length of hospital stay compared to laparoscopy [6.2 (2.5) vs. 6.6 (3.2), p = 0.0001]. Table 3 summarizes the intra- and post-operative outcomes of RLRs and LLRs after the PSM.
Discussion
The superiority of one MILS technique (laparoscopic and robotic) over the other is debated. The laparoscopic approach has spread in the last 30 years and is now largely adopted by liver surgeons; while the more recently introduced robotic assistance for liver resections is still in a developing phase, with more and more centers at the early stages of their robotic activity. We conducted this study to add further insights in the advantages and drawbacks of the two techniques. The short-term results of 269 consecutive MILS cases (of which approximately 30% RLRs), performed according to the principles of PSS from two referral centers for liver surgery, were analyzed.
In the unmatched analysis, we found similar outcomes of both approaches (blood loss, overall and major morbidity, hospital stay) at the expense of longer operative time with a tendency to more conversions to open surgery in LLR group.
The two populations were slightly different for the presence of chronic liver disease, number of nodules, and histology: the robotic group consisted mostly of single HCC in cirrhotic patients, while CRLMs and multiple nodules on non-cirrhotic livers were more frequent in the laparoscopic group. Technical difficulty of MILS measured according to the IWATE criteria was also different in the two groups (mean IWATE score of 4.9 vs. 4.3, p = 0.047 in LLRs vs. RLRs). Because of such differences we decided to conduct a PSM analysis. In the post-matching analysis, we identified two groups represented by well-compensated cirrhotic patients (100%) who underwent non-anatomic resection (laparoscopic or robotic) of low-to-intermediate difficulty, mostly for a solitary HCC of < 5 cm. Despite the absence of a specific robotic instrument to perform the parenchymal dissection, we found shorter operative time with less blood loss and shorter duration of the Pringle maneuver in the robotic group compared to laparoscopy. Hospital stay was also in favor of robotics. These findings suggest an easier parenchymal dissection with the robotic approach along the nonlinear planes of non-anatomic resections, further supporting the facilitating role of robotics over laparoscopy in liver resections [14, 38].
For parenchymal transection, our preference for the clamp-crush technique was to use bipolar forceps (i.e., Maryland®, Intuitive) and monopolar curved scissor. Our experience is still quite limited, but we hypothesized a more precise dissection with these instruments (i.e., compared to the harmonic scalpel) when dealing with stiff livers like in the setting of cirrhosis. However, we do not have any data to compare the impact of different instruments on operative time and other outcomes.
The use of CUSA in a hybrid fashion for RLR is used from around 25% of robotic liver surgeons according to a recent survey [39]. However, while the technical benefit of CUSA in RLRs remains debated, it surely requires a second surgeon with experience in MILS at the operating table, leaving to the robotic surgeon/instruments a “secondary” role of exposure/mobilization/hemostasis. For such reasons, we did not use the laparoscopic CUSA for robotic resections.
In the preliminary study about the implementation of MILS in the center from Pisa, we found shorter operative time in favor of laparoscopic resections [15]. The former study included a smaller population of patients operated during the learning curve, and the use of the Da Vinci Si® robotic platform at the beginning of the program could have impacted the duration of surgery (time-consuming docking). Moreover, we did not use any propensity score strategy to mitigate selection bias nor any stratification of liver resections as per difficulty score. We believe that these elements could explain the different results of the current analysis especially concerning the operative time.
Several papers attempted a comparison between the two MILS approaches in the last 10 years [2, 13, 15, 26, 40,41,42,43].
A recent multicenter study by Cipriani et al. compared pure LLRs to RLRs stratified according to three available difficulty scores for MILS. The study found lower conversion rates to open surgery, reduced blood loss, and intra-operative transfusions for high-complexity robotic procedures compared to laparoscopic resections. Conversely, the advantages of robotic assistance progressively decreased for minor complexity procedures. The authors concluded that robotics did not add a clinical benefit for MILS of low-to-intermediate difficulty [26]. A recent meta-analysis by Ciria et al. grouped the whole body of robotic hepatectomies reported in the literature up to November 2019 (more than 2700 operations); slightly reduced morbidity and hospital stay were noted in favor of robotics, in spite of a shorter operative time and less blood losses for laparoscopic hepatectomies (overall and minor resections). Only in case of major resections the robotic approach was faster than laparoscopy [2]. In line with the abovementioned studies, the recent multicenter trial from Chong et al. adopted a PSM strategy to compare high-difficulty resections (robotic vs. laparoscopic right and right-extended hepatectomy). The authors found lower conversion rate and shorter hospital stay with the robotic approach (supporting the facilitating role of robotics in very complex procedures), but no differences in blood loos and Pringle adoption [44]. This study differed from our one not only in the complexity of the procedures but also in the design (multicenter, larger size, mixed East–West) and in the population included (roughly half of HCCs and less than 30% of cirrhotic patients after the PSM). We believe that these differences prevent a real comparison between the two studies and may explain the different results (i.e., conversions, Pringle adoption, and blood loos).
Our study adds further evidence to the topic and mitigates the conclusions of previous studies, suggesting an advantage of robotics even for anatomically and technically minor hepatectomies (operative time, bleeding, hospital stay).
This study has some limitations. First, this is a retrospective study of a small sample size including neither high difficulty RLRs (IWATE class 4) nor major robotic hepatectomies. However, complex minimally invasive resections may be those for which robotics could provide the highest benefit [25, 26]. Similarly, our series did not include any vascular or biliary reconstruction in either of the two cohorts, thus making impossible to comment on the superiority of one technique in the reconstructive phases of liver surgery. Second, a selection bias cannot be completely excluded even after proper PSM: data were collected from two expert centers in hepatobiliary surgery in which the selection of patients to MILS may reflect different protocols, clinical practice, and phases of the learning curve. One of the centers provides liver transplantation activity with high availability of liver donors (University of Pisa); this indeed could have had an impact in the decision-making process to allocate patients to resection or transplantation. In the case of cirrhotic patients with HCC inside Milan criteria, who represent the majority in the population examined, single-nodule patients were referred to MILS whether patients with two or three HCCs were generally listed for upfront liver transplant if indicated [31]. Finally, the robotic approach has been classically questioned about its cost-effectiveness compared to laparoscopic liver surgery with the recent literature showing discordant data [2, 14, 45]. We did not perform any cost analysis due to existing differences in calculating interventions costs between Italy and Switzerland and the absence of RLRs in the Swiss center.
The availability of the robotic platform is another important aspect to consider which is often underestimated. While laparoscopy is basically available on demand, the robotic platform is usually shared with other surgical specialties and access can be limited. Moreover, a specific training is necessary not only for the surgeon but also for the other members of the operating room team. These could be sources of selection bias as well as factors slowing the progression of robotic resections toward more difficult cases and should be considered in future prospective studies.
In conclusion, this study supports the non-inferiority of RLR over LLR performed in centers with extensive liver surgery practice. Moreover, in compensated cirrhotic patients who underwent low-to-intermediate resections of single HCC of < 5 cm in diameter, RLR was associated with shorter duration of surgery, less blood loss, and shorter hospitalization after the PSM. Further studies with prospective design are needed to compare robotics to laparoscopy in the setting of high difficulty liver resections (IWATE class 3–4).
References
Gavriilidis P, Roberts KJ, Aldrighetti L, Sutcliffe RP (2020) A comparison between robotic, laparoscopic and open hepatectomy: a systematic review and network meta-analysis. Eur J Surg Oncol 46(7):1214–1224
Ciria R, Berardi G, Alconchel F, Briceño J, Choi GH, Wu Y et al (2022) The impact of robotics in liver surgery: a worldwide systematic review and short-term outcomes meta-analysis on 2,728 cases. J Hepatobiliary Pancreat Sci 29(2):181–197
Takahara T, Wakabayashi G, Beppu T, Aihara A, Hasegawa K, Gotohda N et al (2015) Long-term and perioperative outcomes of laparoscopic versus open liver resection for hepatocellular carcinoma with propensity score matching: a multi-institutional Japanese study. J Hepatobiliary Pancreat Sci 22(10):721–727
Beppu T, Wakabayashi G, Hasegawa K, Gotohda N, Mizuguchi T, Takahashi Y et al (2015) Long-term and perioperative outcomes of laparoscopic versus open liver resection for colorectal liver metastases with propensity score matching: a multi-institutional Japanese study. J Hepatobiliary Pancreat Sci 22(10):711–720
Khan S, Beard RE, Kingham PT, Fong Y, Boerner T, Martinie JB et al (2018) Long-term oncologic outcomes following robotic liver resections for primary hepatobiliary malignancies: a multicenter study. Ann Surg Oncol 25(9):2652–2660
Aghayan DL, Kazaryan AM, Dagenborg VJ, Røsok BI, Fagerland MW, Waaler Bjørnelv GM et al (2021) Long-term oncologic outcomes after laparoscopic versus open resection for colorectal liver metastases: a randomized trial. Ann Intern Med 174(2):175–182
Giulianotti PC (2003) Robotics in general surgery: personal experience in a large community hospital. Arch Surg 138(7):777
Buell JF, Cherqui D, Geller DA, O’Rourke N, Iannitti D, Dagher I et al (2009) The international position on laparoscopic liver surgery: the Louisville statement, 2008. Ann Surg 250(3):825–830
Cillo U, D’Amico FE, Furlanetto A, Perin L, Gringeri E (2021) Robotic hepatectomy and biliary reconstruction for perihilar cholangiocarcinoma: a pioneer western case series. Updates Surg 73(3):999–1006
Efanov M, Alikhanov R, Tsvirkun V, Kazakov I, Melekhina O, Kim P et al (2017) Comparative analysis of learning curve in complex robot-assisted and laparoscopic liver resection. HPB 19(9):818–824
Magistri P, Guerrini GP, Ballarin R, Assirati G, Tarantino G, Di Benedetto F (2019) Improving outcomes defending patient safety: the learning journey in robotic liver resections. Biomed Res Int 2019:1–8
Zhu P, Liao W, Ding ZY, Chen L, Zhang WG, Zhang BX et al (2019) Learning curve in robot-assisted laparoscopic liver resection. J Gastrointest Surg 23(9):1778–1787
Lorenz E, Arend J, Franz M, Rahimli M, Perrakis A, Negrini V et al (2021) Robotic and laparoscopic liver resection—comparative experiences at a high-volume German academic center. Langenbecks Arch Surg 406(3):753–761
D’Hondt M, Devooght A, Willems E, Wicherts D, De Meyere C, Parmentier I et al (2022) Transition from laparoscopic to robotic liver surgery: clinical outcomes, learning curve effect, and cost-effectiveness. J Robot Surg. https://doi.org/10.1007/s11701-022-01405-w
Balzano E, Bernardi L, Tincani G, Ghinolfi D, Melandro F, Bronzoni J et al (2021) Implementing a robotic liver resection program does not always require prior laparoscopic experience. Surg Endosc. https://doi.org/10.1007/s00464-021-08645-1
Abu Hilal M, Aldrighetti L, Dagher I, Edwin B, Troisi RI, Alikhanov R et al (2018) The Southampton consensus guidelines for laparoscopic liver surgery: from indication to implementation. Ann Surg 268(1):11–18
Liu R, Wakabayashi G, Kim HJ, Choi GH, Yiengpruksawan A, Fong Y et al (2019) International consensus statement on robotic hepatectomy surgery in 2018. World J Gastroenterol 25(12):1432–1444
Aldrighetti L, Catena M, Ratti F (2022) Maximizing performance in complex minimally invasive surgery of the liver: the RoboLap approach. J Gastrointest Surg. https://doi.org/10.1007/s11605-022-05340-x
Camerlo A, Magallon C, Vanbrugghe C, Chiche L, Gaudon C, Rinaldi Y et al (2021) Robotic hepatic parenchymal transection: a two-surgeon technique using ultrasonic dissection and irrigated bipolar coagulation. J Robot Surg 15(4):539–546
Ban D, Tanabe M, Ito H, Otsuka Y, Nitta H, Abe Y et al (2014) A novel difficulty scoring system for laparoscopic liver resection. J Hepatobiliary Pancreat Sci 21(10):745–753
Kawaguchi Y, Fuks D, Kokudo N, Gayet B (2018) Difficulty of laparoscopic liver resection: proposal for a new classification. Ann Surg 267(1):13–17
Wakabayashi G (2016) What has changed after the Morioka consensus conference 2014 on laparoscopic liver resection? Hepatobiliary Surg Nutr 5(4):281–289
Labadie KP, Droullard DJ, Lois AW, Daniel SK, McNevin KE, Gonzalez JV et al (2021) IWATE criteria are associated with perioperative outcomes in robotic hepatectomy: a retrospective review of 225 resections. Surg Endosc. https://doi.org/10.1007/s00464-021-08345-w
Chong CCN, Lok HT, Fung AKY, Fong AKW, Cheung YS, Wong J et al (2020) Robotic versus laparoscopic hepatectomy: application of the difficulty scoring system. Surg Endosc 34(5):2000–2006
Luberice K, Sucandy I, Modasi A, Castro M, Krill E, Ross S et al (2021) Applying IWATE criteria to robotic hepatectomy: is there a “robotic effect”? HPB 23(6):899–906
Cipriani F, Fiorentini G, Magistri P, Fontani A, Menonna F, Annecchiarico M et al (2022) Pure laparoscopic versus robotic liver resections: multicentric propensity score-based analysis with stratification according to difficulty scores. J Hepatobiliary Pancreat Sci 29(10):1108–1123
Coletta D, Levi Sandri GB, Giuliani G, Guerra F (2021) Robot-assisted versus conventional laparoscopic major hepatectomies: systematic review with meta-analysis. Int J Med Robot 17(3):e2218. https://doi.org/10.1002/rcs.2218
Guan R, Chen Y, Yang K, Ma D, Gong X, Shen B et al (2019) Clinical efficacy of robot-assisted versus laparoscopic liver resection: a meta analysis. Asian J Surg 42(1):19–31
Hu Y, Guo K, Xu J, Xia T, Wang T, Liu N et al (2021) Robotic versus laparoscopic hepatectomy for malignancy: a systematic review and meta-analysis. Asian J Surg 44(4):615–628
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP (2014) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg 12(12):1495–1499
Reig M, Forner A, Rimola J, Ferrer-Fàbrega J, Burrel M, Garcia-Criado Á et al (2022) BCLC strategy for prognosis prediction and treatment recommendation: the 2022 update. J Hepatol 76(3):681–693
Sapisochin G, Goldaracena N, Laurence JM, Dib M, Barbas A, Ghanekar A et al (2016) The extended Toronto criteria for liver transplantation in patients with hepatocellular carcinoma: a prospective validation study. Hepatology 64(6):2077–2088
Vitale A, Trevisani F, Farinati F, Cillo U (2020) Treatment of hepatocellular carcinoma in the precision medicine era: from treatment stage migration to therapeutic hierarchy. Hepatology 72(6):2206–2218
Vitale A, Cabibbo G, Iavarone M, Viganò L, Pinato DJ, Ponziani FR et al (2023) Personalised management of patients with hepatocellular carcinoma: a multiparametric therapeutic hierarchy concept. Lancet Oncol 24(7):e312–e322
Wakabayashi G, Cherqui D, Geller DA, Abu Hilal M, Berardi G, Ciria R et al (2022) The Tokyo 2020 terminology of liver anatomy and resections: updates of the Brisbane 2000 system. J Hepatobiliary Pancreat 29(1):6–15
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L et al (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery 149(5):680–688
Winckelmans T, Wicherts DA, Parmentier I, De Meyere C, Verslype C, D’Hondt M (2023) Robotic versus laparoscopic hepatectomy: a single surgeon experience of 629 consecutive minimally invasive liver resections. World J Surg. https://doi.org/10.1007/s00268-023-07060-y
Zwart MJW, Görgec B, Arabiyat A, Nota CLM, van der Poel MJ, Fichtinger RS et al (2022) Pan-European survey on the implementation of robotic and laparoscopic minimally invasive liver surgery. HPB 24(3):322–331
Zhu P, Liao W, Zhang WG, Chen L, Shu C, Zhang ZW et al (2022) A prospective study using propensity score matching to compare long-term survival outcomes after robotic-assisted, laparoscopic or open liver resection for patients with BCLC stage 0-A hepatocellular carcinoma. Ann Surg. https://doi.org/10.1097/SLA.0000000000005380
Han DH, Choi SH, Park EJ, Kang DR, Choi GH, Choi JS (2016) Surgical outcomes after laparoscopic or robotic liver resection in hepatocellular carcinoma: a propensity-score matched analysis with conventional open liver resection: minimally invasive liver resection for hepatocellular carcinoma. Int J Med Robot Comput Assist Surg 12(4):735–742
Duong LM, Cai H, Shrubsole MJ, Bailey CE, Idrees K, Shu X (2022) Outcomes of robotic-assisted liver surgery versus laparoscopic liver surgery for treatment of stage I hepatocellular carcinoma. Cancer 128(4):762–769
Lim C, Salloum C, Tudisco A, Ricci C, Osseis M, Napoli N et al (2019) Short- and long-term outcomes after robotic and laparoscopic liver resection for malignancies: a propensity score-matched study. World J Surg 43(6):1594–1603
Chong CC, Fuks D, Lee KF, Zhao JJ, Choi GH, Sucandy I et al (2022) Propensity score-matched analysis comparing robotic and laparoscopic right and extended right hepatectomy. JAMA Surg 157(5):436
Miller HP, Hakim A, Kellish A, Wozniak M, Gaughan J, Sensenig R et al (2022) Cost-benefit analysis of robotic vs. laparoscopic hepatectomy: a propensity-matched retrospective cohort study of American College of Surgeons National Surgical Quality Improvement Program database. Am Surgeon 88(12):2886–2892
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Emanuele Balzano, Lorenzo Bernardi, Raffaello Roesel, Filippo Vagelli, Davide Ghinolfi, Giovanni Tincani, Gabriele Catalano, Fabio Melandro, Sotirios-Georgios Popeskou, Dimitri Christoforidis, Pietro Majno-Hurst, Paolo De Simone, and Alessandra Cristaudi have no conflicts of interest or financial ties to disclose.
Ethical approval
This study was approved by the local ethics committee of both the institutions participating in the study.
Informed consent
Patients provided informed consent to participate to the study at first referral at Pisa University Hospital as per institutional policy. Patients in Regional Hospital of Lugano were informed of the ongoing study and received a non-objection letter from the institution.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Balzano, E., Bernardi, L., Roesel, R. et al. Robotic versus laparoscopic liver resections: propensity-matched comparison of two-center experience. Surg Endosc 37, 8123–8132 (2023). https://doi.org/10.1007/s00464-023-10358-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10358-6