Abstract
Background
Pancreatic solid pseudopapillary neoplasms (SPN) are generally indolent; however, some patients present with “malignant” SPN. An orthogonal analysis of multiple datasets was performed to investigate the utility of complete surgical resection (CSR) for malignant SPN.
Methods
A systematic review was performed for cases of malignant SPN, defined as T4, N1, and/or M1. Malignant SPN was analyzed within the National Cancer Database (NCDB) and compared with T1-3N0M0 SPN. Predictors of malignant SPN were assessed, and treatments were analyzed by using survival analysis.
Results
The systematic review yielded 164 cases of malignant SPN. Of 31 children, only one died due to malignant SPN. Among adults, CSR was associated with improved disease-specific survival (DSS) (P = 0.0002). Chemotherapy did not improve malignant SPN DSS, whether resected (P = 0.8485) or not (P = 0.2219). Of 692 adults with SPN within the NCDB, 93 (13.4%) had malignant SPN. Pancreatic head location (odds ratio [OR] 2.174; 95% confidence interval [CI] 1.136–4.166; P = 0.0186) and tumor size (OR 1.154; 95% CI 1.079–1.235; P < 0.0001) associated with the malignant phenotype. Malignant SPN predicted decreased overall survival (OS) compared with T1-3N0M0 disease (P < 0.0001). Resected malignant SPN demonstrated improved OS (P < 0.0001), including resected stage IV malignant SPN (P = 0.0003). Chemotherapy did not improve OS for malignant SPN, whether resected (P = 0.8633) or not (P = 0.5734). Within a multivariable model, resection was associated with decreased hazard of death (hazard ratio 0.090; 95% CI 0.030–0.261; P < 0.0001).
Conclusions
Approximately 13% of patients with SPN present with a malignant phenotype. Pediatric cases may be less aggressive. Resection may improve survival for malignant SPN, which does not appear chemosensitive.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Solid pseudopapillary neoplasm of the pancreas (SPN) comprises less than 2% of all pancreatic tumors.1 SPN demonstrates a tenfold higher incidence in females and represents the most common pancreatic tumor in childhood.2,3,4 First reported in 1959, SPN was designated a low-grade pancreatic malignancy by the World Health Organization in 1996.5, 6 SPN is associated with a favorable prognosis, and organ-preserving surgical resection can provide excellent recurrence-free survival.1, 7
Some SPN demonstrate a more aggressive phenotype with extra-pancreatic extension, invasion of adjacent organs, vascular encasement, lymph node metastases, distant metastatic disease, disease relapse, and/or disease-specific mortality.8,9,10 These cases are sometimes referred to as “malignant” SPN. Predictors of the malignant SPN phenotype, and its impact on disease-specific survival (DSS) are not well-defined.8, 11,12,13 Some data have suggested that malignant SPN in children follows a fairly indolent course, even with distant metastatic disease.3, 4, 8 No consensus guidelines regarding the treatment of malignant SPN currently exist. Data supporting complete surgical resection (CSR) of metastatic disease and the utility of adjuvant therapies in patients with distant metastases remain anecdotal.14, 15 In these contexts, an orthogonal approach to data analysis can incorporate multiple comparative analyses of independent data sources to add validity to the results of each individual analysis.16, 17 This methodology increases the reliability of the results of each analysis and is seen as a means of “cross checking” the results of one analysis against another independent analysis within the same scientific experiment.16, 17
The current study comprises an orthogonal analysis of multiple datasets to further characterize the natural history and optimal treatment of malignant SPN.16 The first goal of this study was to perform a systematic review and pooled data analysis of all reported cases of malignant SPN in children and adults. These data were used to compare the disease-specific survival (DSS) of pediatric and adult patients and to assess the impact of CSR on disease-specific survival (DSS) for patients with malignant SPN. The second goal of this study was to identify cases of malignant SPN among all cases of SPN within the National Cancer Database (NCDB). These data were used to identify predictors of the malignant SPN phenotype and further validate the utility of surgical resection in the setting of metastatic disease. The third goal was to use each dataset to evaluate the utility of adjuvant treatments for malignant SPN, including the use of systemic chemotherapy and non-surgical liver-directed therapies for unresected liver metastases.
Methods
Institutional Review Board Approval and Prospective Registration
The University of Tennessee Health Science Center Institutional Review Board (IRB) determined this study to be Not Human Subjects Research (NHSR) status (IRB number: 22-08891-NHSR). This study was prospectively registered through the International Prospective Register of Systematic Reviews (PROSPERO ID: CRD42022349312).
Systematic Review of Reported Malignant SPN Cases—Eligibility Criteria
Reported cases were defined as having “malignant SPN” if they had T4 tumors according to the American Joint Committee on Cancer (AJCC) 8th edition staging system, AND/OR if they had lymph node metastases (N1), AND/OR if they had distant metastatic disease (M1). Unresected cases reported in the literature determined to be T4 were clinically staged or noted to be T4 based on the intraoperative findings. Resected tumors were pathologically staged. All cases meeting these staging criteria were included for analysis. Cases were excluded from pooled analysis if the patients had T1-3N0M0 disease (not the malignant SPN phenotype), if there were no treatment data (manuscripts purely focused on histopathology), or if relevant patient data were not available in the English language.
Systematic Review of Reported Malignant SPN Cases—Information Sources
PubMed, MEDLINE, EMBASE, the Cochrane database, and SCOPUS were systematically reviewed for all reported cases of malignant SPN. The international prospective register of systematic reviews (PROSPERO) was analyzed for reviews of similar scope. All publication dates from 1959 onward were included in the search, with the final query performed on July 22, 2022.
Systematic Review of Reported Malignant SPN Cases—Search Strategy
The text words “solid pseudopapillary neoplasm,” “solid pseudopapillary tumor,” and “pancreas,” and the medical subjects headings (MeSH) terms “Pancreas” and “Neoplasm” were used alone and in combination with the text “Metastatic Disease,” “Metastasis,” and the MeSH term “Metastasis” using the Boolean logic term “OR.” The search was augmented by using the Boolean logic term “AND” to add the terms text words “Metastasis,” “Liver Metastasis,” “Lymph Node Metastasis,” and “Distant Metastasis.” The “case reports” and “review” filter options were toggled to refine the search further. A thorough review of all citations and abstracts identified was performed, and the search was expanded via the “related articles” function. The bibliographies of all retrieved papers were screened for additional eligible literature. The prospectively registered search strategy document can be found on PROSPERO for a complete list of search terms used in this analysis (https://www.crd.york.ac.uk/PROSPEROFILES/349312_STRATEGY_20220726.pdf).
Systematic Review of Reported Malignant SPN Cases—Selection Process
Selected studies underwent detailed review to determine if they met inclusion criteria. The predetermined protocol for disagreements regarding inclusion of a study consisted of resolution by consensus or by the decision of a third reviewer.
Systematic Review of Reported Malignant SPN Cases—Data Collection Process
After the selection process, data were abstracted regarding the primary data items of interest in each of the included studies (achievement of CSR, DSS in months). Study characteristics were abstracted into the standardized data collection spreadsheet (first author, year of publication, location of study institution, journal of publication). Important patient, tumor, and treatment data also were abstracted, including patient age, patient biological sex, presence of locally invasive disease, presence of nodal metastases, presence of distant metastatic disease, timing of metastatic disease, location of metastatic disease, receipt of systemic therapy, and receipt of nonsurgical liver-directed therapy.
Systematic Review of Reported Malignant SPN Cases of Data Items
Reported cases were defined as having “malignant SPN” if they had T4 tumors according to the American Joint Committee on Cancer (AJCC) 8th edition staging system (invading adjacent celiac axis or superior mesenteric artery), AND/OR demonstrated invasion of adjacent organs (stomach, duodenum, colon, porta hepatis), AND/OR had nodal metastases (N1), AND/OR if they had distant metastatic disease (M1). CSR designation was applied to a reported case of malignant SPN when the included operative description recorded resection of all reported disease for that patient. Patients who underwent resection of their primary tumors, but not metastatic disease, were not denoted “CSR.” Patients were denoted “pediatric patient” status if under the age of 18 years.
Primary data items of interest included the following:
-
Complete surgical resection (CSR)
-
Disease-specific survival in months
Secondary data items of interest included the following:
-
Patient data
-
Patient age
-
Patient biological sex
-
-
Disease data
-
Presence of extra-pancreatic tumor extension into adjacent vascular structures and/or adjacent organs (T4 disease)
-
Presence of lymph node metastases (N1 disease)
-
Presence of distant metastatic disease (M1 disease)
-
Synchronous vs. metachronous metastatic disease
-
Location of metastatic disease (liver, peritoneum, lung, other)
-
-
Treatment data
-
Extent of pancreatectomy (local excision/enucleation, distal pancreatectomy, pancreatoduodenectomy, total pancreatectomy, multivisceral resection)
-
Extent of hepatectomy (nonanatomic wedge resection, segmentectomy, sectionectomy, hemihepatectomy, trisectionectomy, total hepatectomy with transplantation), if applicable
-
Receipt of systemic chemotherapy
-
Receipt of nonsurgical liver-directed therapy (transcatheter arterial chemoembolization, bland transarterial embolization, radiofrequency ablation, hepatic artery infusion)
-
Systematic Review of Reported Malignant SPN Cases—Study Risk of Bias Assessment
This analysis intrinsically contained a high risk of both selection and reporting bias given the nonstandardized nature of case reports and case series. The Joanna Briggs Institute critical appraisal checklist for case reports was used as a reference to assess the quality of included cases.18
National Cancer Database—Data Source and Patient Selection
The NCDB is estimated to include most cancer cases in the United States and functions as a joint endeavor of the American College of Surgeons Commission on Cancer and the American Cancer Society. Cases within the NCDB are classified using the International Classification of Disease for Oncology (ICD-O-3) histology codes. Cases were included for analysis from the 2004-2017 Pancreas dataset if they had ICD-O-3 codes corresponding to “Solid Pseudopapillary Neoplasm of the Pancreas” (ICD-O-3 8452). Patients with all other histology codes were excluded from this analysis, as were patients with incomplete staging data. Cases of SPN in the NCDB were defined as having “malignant SPN” if they had T4 tumors, OR if they had lymph node metastases (N1), OR if they had distant metastatic disease (M1).
Statistical Analysis
All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC) and GraphPad Prism Version 9.4.0 (GraphPad Software, LLC., San Diego, CA). Data from the systematic review were analyzed independently from those abstracted from the NCDB. Patient characteristics, tumor characteristics, treatment data, and outcomes data were tabulated with descriptive statistics. Data from the systematic review were analyzed as disease-specific survival (DSS), while data from the NCDB were analyzed as overall survival (OS), as data regarding disease relapse and cause of death are not provided within the NCDB. Variables associated with increased hazard of death were analyzed with univariable and multivariable Cox proportional hazards models. Patients with data missing for variables incorporated in the multivariable model were excluded from multivariable analysis. Survival curves were generated by using the Kaplan-Meier method, stratified by relevant variables, and compared by using log-rank tests. The incidence of malignant SPN was analyzed over time in both datasets by using one-way ANOVA with testing for linear trend. All hypothesis testing was two-sided. P values < 0.05 were considered statistically significant for all analyses.
Results
Systematic Review of Reported Cases of Malignant SPN—Study Selection
Complete details regarding the results of the study selection process are depicted in Fig. 1A. A total of 665 records were initially identified in our systematic review. Of these, 428 were found to be off-topic or duplicate publications. A total of 237 studies were reviewed in more detail. Of these, 97 studies were excluded as they did not meet criteria for malignant SPN status, whereas 46 did not have patient data available in the English language. All 94 reports sought for retrieval were successfully retrieved via institutional access or institutional interlibrary loan and document delivery systems. Ninety-four publications were included for analysis, comprising 164 total cases of malignant SPN.1, 9, 10, 19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109 Details regarding all included studies can be found in Supplemental Table S1.
Case selection flow diagram from A the systematic review of reported cases and B the National Cancer Database. Adapted from Page et al.120 mSPN malignant SPN
Systematic Review of Reported Malignant SPN Cases—Patient Characteristics, Tumor Characteristics, and Treatment Data
A total of 164 reported cases of malignant SPN from Austria, Canada, China, Croatia, France, Germany, Hong Kong, India, Italy, Japan, Korea, Pakistan, Poland, Portugal, Puerto Rico, Singapore, South Africa, Spain, Sri Lanka, Switzerland, Turkey, the United Kingdom, and the United States of America were included for analysis (Table 1). Patients with malignant SPN were a median age of 39.0 years (interquartile range [IQR] 20.0–50.0), with 31 patients younger than age 18 years captured in the review. There were 142 female patients with malignant SPN (86.6%). Sixty-eight patients had locally invasive disease, consisting of T4 tumors with invasion into adjacent vascular structures or organs (41.5%), and 144 patients had metastatic disease (87.8%). Of these 144 patients, 79 had metastases at diagnosis (56.9%), whereas 62 were noted to have metastases at time of disease relapse (43.1%). The most common sites of metastases were the liver (n = 123), peritoneum (n = 34), and lymph nodes (n = 19). CSR was reported in 92 patients (56.1%). Thirty-one patients received systemic therapies (18.9%), and 37 patients underwent nonsurgical liver directed therapies (22.6%). A detailed treatment analysis flow diagram can be found in Supplemental Fig. S1. Reported cases of malignant SPN in the surgical literature were not found to be significantly increasing over time within the publication period of 1980–2022 (P = 0.4158).
Systematic Review of Reported Malignant SPN Cases—Disease-Specific Survival Analysis
One-year, 5-year, and 10-year DSS for the entire cohort were 94.3% (95% CI 88.9–97.1%), 81.2% (95% CI 71.9–87.7%), and 71.0% (95% CI 57.5–80.9%), respectively (Fig. 2A). Adult patients had a significantly decreased 10-year DSS of 62.6% (95% CI 44.8–76.1%) compared with children, who had a 96.4% (95% CI 77.2–99.5%) 10-year DSS (log-rank P = 0.0248) (Fig. 2B). One pediatric death attributable to malignant SPN was captured within the current study’s systematic review.44 Among 99 adult patients with malignant SPN and complete survival data, CSR was associated with a significant improvement in DSS (log-rank P = 0.0002; Fig. 2D). Receipt of systemic therapy was not associated with improved DSS for adults who underwent incomplete resection (log-rank P = 0.2219; Fig. 2E) or CSR (log-rank P = 0.8485; Fig. 2E). Subgroup analysis of adult patients with unresected liver metastases revealed that nonsurgical liver-directed therapies were not associated with a significant difference in DSS (log-rank P = 0.3507; Fig. 2F). The impact of CSR, systemic therapies, and liver-directed therapies were not evaluated for pediatric patients given the low event rate of patient mortality.
Disease-specific survival of A all patients in the cohort stratified by B pediatric patient status. DSS of adult patients stratified by C receipt of complete surgical resection, D receipt of systemic therapy in the absence of complete surgical resection, E receipt of systemic after complete surgical resection, and F receipt of non-surgical liver-directed therapies in the setting of unresected liver metastases. mSPN malignant SPN
National Cancer Database—Patient Characteristics, Tumor Characteristics, and Treatment Data
Complete details regarding the results of the NCDB case selection process are depicted in Fig. 1B. Among 692 cases of SPN included from the NCDB for analysis, 93 patients had a malignant phenotype, consisting of T4 disease, N1 disease, and/or M1 disease (13.4%; Table 2). All other patients (599/692) had T1-3N0M0 disease and were determined to not possess the malignant SPN phenotype. Patients with malignant SPN were older (44 vs. 35 years, P < 0.0001) and more often male (28.0% vs. 13.0%, P = 0.0005). Fewer patients with malignant SPN had private insurance (49.5% vs. 62.6%, P = 0.0028). Patients with malignant SPN had a larger median tumor size (8.0 cm vs. 4.5 cm, P < 0.0001), less often presented with tumors in the body or tail of the pancreas (37.6% vs. 58.9%, P < 0.0001), and less often underwent distal pancreatectomy for their primary tumors (22.6% vs. 50.6%, P < 0.0001). Among resected patients, those with malignant SPN had more lymph nodes examined (11.0 vs. 8.0, P = 0.0028) and more often received systemic chemotherapy (29.0% vs. 3.0%, P < 0.0001). Postoperative length of stay was longer in the malignant SPN group (7.0 vs. 6.0 days, P = 0.0340). Within a multiple logistic regression model accounting for age, sex, insurance status, tumor location, and tumor size, only tumor location in the pancreatic head (odds ratio (OR) 2.174; 95% CI 1.136-4.166, P = 0.0186) and increasing tumor size (OR 1.154 per cm; 95% CI 1.079-1.235; P < 0.0001) were significantly associated with increased risk of a malignant phenotype for patients with SPN (Table 3). A complete treatment analysis flow diagram for the OS analyses of the NCDB cohort can be found in Supplemental Fig. S2. Test for linear trend revealed that the incidence of the malignant SPN phenotype was found to be significantly increasing over time within the NCDB (P = 0.0027).
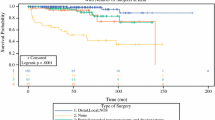
National Cancer Database—Overall Survival Analysis
One-year, 5-year, and 10-year OS for the entire cohort were 96.4% (95% CI 94.5–97.7%), 91.4% (95% CI 88.3–93.8%), and 85.5% (95% CI 80.7–89.2%; Fig. 3A). Patients with malignant SPN had significantly decreased OS compared with patients with T1-3N0M0 disease (log-rank P < 0.0001; Fig. 3B). One-year, 5-year, and 10-year OS for patients with malignant SPN versus T1-3N0M0 disease were 77.2% (95% CI 66.3–85.0%), 64.6% (95% CI 52.3–74.6%), and 50.8% (95% CI 35.7–64.0%) versus 99.6% (95% CI 98.0–99.8%), 96.2% (95% CI 93.2–97.8%), and 92.2% (95% CI 87.7–95.1%), respectively. For patients with malignant SPN, resection was associated with significantly improved OS (log-rank P < 0.0001; Fig. 3C). Subgroup analysis of patients with stage IV disease, defined as distant metastatic disease, revealed that resection was associated with significantly improved OS (log-rank P = 0.0001; Fig. 3D). Among patients with malignant SPN, receipt of systemic chemotherapy was not associated with improved OS whether they did (log-rank P = 0.8633; Fig. 3E) or did not undergo resection (log-rank P = 0.5734; Fig. 3F).
Overall survival of A all patients in the cohort stratified by B presence of malignant phenotype, C receipt of resection in the setting of malignant phenotype, D receipt of resection in the setting of distant metastatic disease, E receipt of systemic chemotherapy after resection of malignant SPN, and F receipt of systemic chemotherapy for unresected malignant SPN. mSPN malignant SPN
Within a multivariable Cox proportional hazards regression model adjusting for age, sex, comorbid disease, tumor location within the pancreas, tumor size, and tumor resection, the malignant SPN phenotype was associated with significantly increased hazard of death (HR 3.768; 95% CI 1.524–9.001; P = 0.0031; Table 4). Disease resection was associated with significantly decreased hazard of death within the same model (HR 0.087; 95% CI 0.032–0.233; P < 0.0001).
Discussion
Given its rarity, predictors of the malignant SPN phenotype and treatment outcomes for these patients are difficult to study. Utilizing orthogonal data analysis, the current study provides evidence supporting resection for malignant SPN and limited efficacy of adjunct nonsurgical therapies for these patients. However, there are several points of consideration when translating these data to clinical practice.
Children with Malignant SPN Demonstrated Superior Disease-Specific Survival Compared with Adults
In the pediatric population, only one disease-specific death was reported.44 The likelihood of publication bias in this finding is high and mandates external validation.110 Lee et al. analyzed 62 consecutive pediatric and adult patients with SPN at a single center.8 Children and adults demonstrated similar rates of malignant features, and there were no tumor-related deaths in their series. Hwang et al. demonstrated 95% disease-free survival and 100% DSS for 45 children with resected SPN, including nine malignant SPN, two of which had distant metastatic disease.111 Among 228 pancreatic malignancies in children and young adults analyzed within the Surveillance, Epidemiology, and End Results database by Brecht et al., eight patients with “malignant” SPN were identified.112 The 5-year OS for this cohort was 88%, but cause of death was not available for analysis.112 Collectively, results of these studies as well as those of the current analysis suggest an indolent behavior of malignant SPN in children. The impact of CSR on DSS for children could not be directly analyzed in this study given that only one child died of disease; however, given the unpredictable natural history of malignant SPN, its relative insensitivity to conventional chemotherapy, and the likelihood of surgeons underreporting individual children who died of their disease, consideration should be given to CSR in children when able to be performed without significant morbidity.
Surgical Resection Improved Survival for Adults with Malignant SPN
Within the current pooled analysis of reported cases, adult patients with malignant SPN who had CSR demonstrated significantly improved DSS. Within the NCDB, patients with malignant SPN, including the subgroup of patients with stage IV disease, had improved OS when they underwent resection. Few data are published comparing resection to observation for malignant SPN, but these data echo previous reports of excellent long term survival for patients with malignant phenotypes who undergo resection.7, 8, 12 Notably absent from the current analysis are selection criteria for resection of malignant SPN, which could not be reliably defined. As with other rare cancers, the decision to aggressively resect malignant SPN should be made within the context of a goal-oriented treatment plan that incorporates multidisciplinary expertise and a realistic assessment of surgical candidacy.
Larger Tumor Size and Pancreatic Head Tumor Location Associated with the Malignant SPN Phenotype
Increasing tumor size was found to be independently associated with the malignant SPN phenotype. This is concordant with previously published observations.12, 111, 113,114,115 However, that tumor location in the pancreatic head is associated with malignant SPN has not been previously reported. Hwang et al. reported similar rates of pancreatic head tumors in children with “benign” SPN and malignant SPN.111 Lee et al. similarly reported no difference in tumor location between “benign” SPN and malignant SPN.8 The clinical significance of this finding is unclear, as pancreatic head tumor location was not associated with differences in OS after adjusting for patient age, tumor size, malignant phenotype, and resection within the current analysis of the NCDB. More sophisticated radiographic observations have been reported to predict malignant SPN, such as focal capsular discontinuity, although these data are not concordant and warrant further study.111, 116
Adjuvant Therapies were not Associated with Improved Survival for Patients with Malignant SPN
There are no standardized chemotherapy, radiotherapy, or liver ablation regimens for unresected malignant SPN.117 Within this orthogonal analysis, the use of systemic chemotherapy failed to demonstrate a survival benefit for patients with malignant SPN, regardless of whether CSR was achieved. Within the pooled analysis, the use of nonsurgical, liver-directed therapies was not associated with a significant difference in DSS. While there are reports of long-term survival among individual patients with unresectable malignant SPN receiving chemotherapy, the inherently slow progression of these tumors makes it hard to appreciate the influence of systemic treatment.117, 118
Limitations
This study has several limitations that warrant mention. First, the selection criteria for resection of malignant SPN remain undefined and cannot be determined with the current data, introducing an inherent selection bias. The systematic review portion of this analysis is prone to publication bias and limited by its retrospective nature and the nonstandardized reporting of individual cases. Another limitation of the systematic review is the high likelihood that individual cases of malignant SPN within large series of nonmalignant SPN were not captured, as the prespecified search protocol emphasized search terms, such as “malignant” and “metastatic.” Within the NCDB, the incidence of malignant SPN was noted to be increasing over time. Whether this is due to increased recognition of extrapancreatic disease or a true increase in the malignant phenotype cannot be determined within the current study, although age-adjusted incidence rates of numerous rare cancers are increasing over time, making this finding plausible.119 However, as treatments evolve over time, caution must be used when externally applying conclusions from observational analyses with a lengthy study period. Also, information regarding the type or number of cycles of chemotherapy is not captured in the NCDB, and there is no data regarding extent of metastasectomy, disease relapse, or cause of death. Finally, although the NCDB captures the majority of cancer cases in the United States, some cases of SPN may not be captured within either dataset, which limits the extrapolation of the epidemiologic portions of these analyses to the population level.
Conclusions
Malignant SPN is an uncommon clinical phenotype of a rare pancreatic tumor. The current analysis supports resection of all disease when feasible. Notable findings are that children appear have a more indolent disease course than adults; larger tumors and those located within the pancreatic head have a higher association with malignant SPN; and the use of adjuvant chemotherapy, radiotherapy, and liver-directed therapies were not associated with improved survival. Given the rarity of malignant SPN, prospective, randomized trials are not feasible. Future studies should include multicentered experiences with standardized data collection and detailed histopathological data.
Data availability
Data from this analysis were presented at the Society of Surgical Oncology International Congress on Surgical Cancer Care 2023.
References
Martin RC, Klimstra DS, Brennan MF, et al. Solid-pseudopapillary tumor of the pancreas: A surgical enigma? Ann Surg Oncol. 2002;9(1):35–40.
Papavramidis T, Papavramidis S. Solid pseudopapillary tumors of the pancreas: review of 718 patients reported in English literature. J Am Coll Surg. 2005;200(6):965–72.
Picado O, Ferrantella A, Zabalo C, et al. Treatment patterns and outcomes for pancreatic tumors in children: an analysis of the National Cancer Database. Pediatr Surg Int. 2020;36(3):357–63.
Vasudevan SA, Ha TN, Zhu H, et al. Pancreaticoduodenectomy for the treatment of pancreatic neoplasms in children: A Pediatric Surgical Oncology Research Collaborative study. Pediatr Blood Cancer. 2020;67(9):e28425.
Frantz VK. Tumors of the pancreas. Armed Forces Institute of Pathology; 1959.
Klöppel G, Solcia E, Longnecker DS, et al. Histological typing of tumours of the exocrine pancreas / G. Klöppel ... [et al.] in collaboration with pathologists in 7 countries, 2nd edn. Berlin: Springer-Verlag; 1996.
Reddy S, Cameron JL, Scudiere J, et al. Surgical management of solid-pseudopapillary neoplasms of the pancreas (Franz or Hamoudi tumors): A large single-institutional series. J Am Coll Surg. 2009;208(5):950–7 (discussion 957-9).
Lee SE, Jang JY, Hwang DW, et al. Clinical features and outcome of solid pseudopapillary neoplasm: differences between adults and children. Arch Surg. 2008;143(12):1218–21.
Hanada K, Kurihara K, Itoi T, et al. Clinical and pathological features of solid pseudopapillary neoplasms of the pancreas: a nationwide multicenter study in Japan. Pancreas. 2018;47(8):1019–26.
Tanoue K, Mataki Y, Kurahara H, et al. Multidisciplinary treatment of advanced or recurrent solid pseudopapillary neoplasm of the pancreas: Three case reports. Surg Case Rep. 2022;8(1):7.
Raman SP, Kawamoto S, Law JK, et al. Institutional experience with solid pseudopapillary neoplasms: focus on computed tomography, magnetic resonance imaging, conventional ultrasound, endoscopic ultrasound, and predictors of aggressive histology. J Comput Assist Tomogr. 2013;37(5):824–33.
Estrella JS, Li L, Rashid A, et al. Solid pseudopapillary neoplasm of the pancreas: clinicopathologic and survival analyses of 64 cases from a single institution. Am J Surg Pathol. 2014;38(2):147–57.
Kim CW, Han DJ, Kim J, et al. Solid pseudopapillary tumor of the pancreas: can malignancy be predicted? Surgery. 2011;149(5):625–34.
Romics L Jr, Oláh A, Belágyi T, et al. Solid pseudopapillary neoplasm of the pancreas–proposed algorithms for diagnosis and surgical treatment. Langenbecks Arch Surg. 2010;395(6):747–55.
Maffuz A, Bustamante Fde T, Silva JA, et al. Preoperative gemcitabine for unresectable, solid pseudopapillary tumour of the pancreas. Lancet Oncol. 2005;6(3):185–6.
Allen M. The SAGE Encyclopedia of Communication Research Methods. Thousand Oaks, California: SAGE Publications, Inc; 2017.
Zhou Y, Zhou B, Pache L, et al. Metascape provides a biologist-oriented resource for the analysis of systems-level datasets. Nat Commun. 2019;10(1):1523.
JBI. JBI Critical Appraisal Checklist for Case Reports: JBI2022.
Corrente RF. Cystadenocarcinoma of the pancreas. Am J Surg. 1980;139(2):265–7.
Dales RL, Garcia JC, Davies RS. Papillary-cystic carcinoma of the pancreas. J Surg Oncol. 1983;22(2):115–7.
Sanfey H, Mendelsohn G, Cameron JL. Solid and papillary neoplasm of the pancreas. A potentially curable surgical lesion. Ann Surg. 1983;197(3):272–5.
Morrison DM, Jewell LD, McCaughey WT, et al. Papillary cystic tumor of the pancreas. Arch Pathol Lab Med. 1984;108(9):723–7.
Fried P, Cooper J, Balthazar E, et al. A role for radiotherapy in the treatment of solid and papillary neoplasms of the pancreas. Cancer. 1985;56(12):2783–5.
Warren RB. Papillary cystic tumor of the pancreas. Arch Pathol Lab Med. 1985;109(8):706–7.
Kaufman SL, Reddick RL, Stiegel M, et al. Papillary cystic neoplasm of the pancreas: a curable pancreatic tumor. World J Surg. 1986;10(5):851–9.
Rustin RB, Broughan TA, Hermann RE, et al. Papillary cystic epithelial neoplasms of the pancreas: A clinical study of four cases. Arch Surg. 1986;121(9):1073–6.
Lieber MR, Lack EE, Roberts JR Jr, et al. Solid and papillary epithelial neoplasm of the pancreas. An ultrastructural and immunocytochemical study of six cases. Am J Surg Pathol. 1987;11(2):85–93.
Stachura J, Popiela T, Pietroń M, et al. Cytology of solid and papillary epithelial neoplasms of the pancreas: a case report. Diagn Cytopathol. 1988;4(4):339–41.
Todani T, Shimada K, Watanabe Y, et al. Frantz’s tumor: A papillary and cystic tumor of the pancreas in girls. J Pediatric Surg. 1988;23(2):116–21.
Heitz PU, Stolte M, Kloeppel G. Large pancreatic tumor in a young woman. Ultrastruct Pathol. 1989;13(5–6):589–92.
Hernandez-Maldonado JJ, Rodriguez-Bigas MA, Gonzalez de Pesante A, et al. Papillary cystic neoplasm of the pancreas. A report of a case presenting with carcinomatosis. Am Surg. 1989;55(9):552-9.
Yamaguchi K, Miyagahara T, Tsuneyoshi M, et al. Papillary cystic tumor of the pancreas: an immunohistochemical and ultrastructural study of 14 patients. Jpn J Clin Oncol. 1989;19(2):102–11.
Cappellari JO, Geisinger KR, Albertson DA, et al. Malignant papillary cystic tumor of the pancreas. Cancer. 1990;66(1):193–8.
Matsunou H, Konishi F, Yamamichi N, et al. Solid, infiltrating variety of papillary cystic neoplasm of the pancreas. Cancer. 1990;65(12):2747–57.
Zinner MJ, Shurbaji MS, Cameron JL. Solid and papillary epithelial neoplasms of the pancreas. Surgery. 1990;108(3):475–80.
Sclafani LM, Reuter VE, Coit DG, et al. The malignant nature of papillary and cystic neoplasm of the pancreas. Cancer. 1991;68(1):153–8.
Stömmer P, Kraus J, Stolte M, et al. Solid and cystic pancreatic tumors. Clinical, histochemical, and electron microscopic features in ten cases. Cancer. 1991;67(6):1635-41.
Tsunoda T, Eto T, Tsurifune T, et al. Solid and cystic tumor of the pancreas in an adult male. Acta Pathol Jpn. 1991;41(10):763–70.
Jaksic T, Yaman M, Thorner P, et al. A 20-year review of pediatric pancreatic tumors. J Pediatric Surg. 1992;27(10):1315–7.
Kingsnorth AN, Galloway SW, Lewis-Jones H, et al. Papillary cystic neoplasm of the pancreas: presentation and natural history in two cases. Gut. 1992;33(3):421–3.
Nishihara K, Nagoshi M, Tsuneyoshi M, et al. Papillary cystic tumors of the pancreas. Assessment of their malignant potential. Cancer. 1993;71(1):82–92.
González-Cámpora R, Rios Martin JJ, Villar Rodriguez JL, et al. Papillary cystic neoplasm of the pancreas with liver metastasis coexisting with thyroid papillary carcinoma. Arch Pathol Lab Med. 1995;119(3):268–73.
Mao C, Guvendi M, Domenico DR, et al. Papillary cystic and solid tumors of the pancreas: a pancreatic embryonic tumor? Studies of three cases and cumulative review of the world’s literature. Surgery. 1995;118(5):821–8.
Ky A, Shilyansky J, Gerstle J, et al. Experience with papillary and solid epithelial neoplasms of the pancreas in children. J Pediatric Surg. 1998;33(1):42–4.
Panieri E, Krige JE, Bornman PC, et al. Operative management of papillary cystic neoplasms of the pancreas. J Am Coll Surg. 1998;186(3):319–24.
Shimizu M, Matsumoto T, Hirokawa M, et al. Solid-pseudopapillary carcinoma of the pancreas. Pathol Int. 1999;49(3):231–4.
Saiura A, Umekita N, Matsui Y, et al. Successful surgical resection of solid cystic tumor of the pancreas with multiple liver metastases and a tumor thrombus in the portal vein. Hepatogastroenterology. 2000;47(33):887–9.
Müller-Höcker J, Zietz CH, Sendelhofert A. Deregulated expression of cell cycle-associated proteins in solid pseudopapillary tumor of the pancreas. Mod Pathol. 2001;14(2):47–53.
Rebhandl W, Felberbauer FX, Puig S, et al. Solid-pseudopapillary tumor of the pancreas (Frantz tumor) in children: report of four cases and review of the literature. J Surg Oncol. 2001;76(4):289–96.
Lee YR, Kim Y, Koh BH, et al. Solid and papillary epithelial neoplasm of the pancreas with peritoneal metastasis and its recurrence: a case report. Abdom Imaging. 2003;28(1):96–8.
Podevin J, Triau S, Mirallié E, et al. Solid-pseudopapillary tumor of the pancreas: a clinical study of five cases, and review of the literature. Ann Chir. 2003;128(8):543–8.
Usatoff V, Wittkop B, Devalia K, et al. Solid papillary-cystic carcinoma of the pancreas with portal vein tumour thrombus. ANZ J Surg. 2004;74(4):291–3.
Ahmad Z, Yaqoob N, Muzaffar S, et al. Solid and cystic epithelial neoplasm of pancreas with metastasis: report of a highly unusual case. J Pak Med Assoc. 2005;55(1):37–9.
Alexandrescu DT, O’Boyle K, Feliz A, et al. Metastatic solid-pseudopapillary tumour of the pancreas: clinico-biological correlates and management. Clin Oncol (R Coll Radiol). 2005;17(5):358–63.
Chen X, Zhou GW, Zhou HJ, et al. Diagnosis and treatment of solid-pseudopapillary tumors of the pancreas. Hepatobiliary Pancreat Dis Int. 2005;4(3):456–9.
Hassan I, Celik I, Nies C, et al. Successful treatment of solid-pseudopapillary tumor of the pancreas with multiple liver metastases. Pancreatology. 2005;5(2–3):289–94.
Huang HL, Shih SC, Chang WH, et al. Solid-pseudopapillary tumor of the pancreas: clinical experience and literature review. World J Gastroenterol. 2005;11(9):1403–9.
Sun CD, Lee WJ, Choi JS, et al. Solid-pseudopapillary tumours of the pancreas: 14 years experience. ANZ J Surg. 2005;75(8):684–9.
Takahashi Y, Fukusato T, Aita K, et al. Solid pseudopapillary tumor of the pancreas with metastases to the lung and liver. Pathol Int. 2005;55(12):792–6.
Tang LH, Aydin H, Brennan MF, et al. Clinically aggressive solid pseudopapillary tumors of the pancreas: a report of two cases with components of undifferentiated carcinoma and a comparative clinicopathologic analysis of 34 conventional cases. Am J Surg Pathol. 2005;29(4):512–9.
Adamthwaite JA, Verbeke CS, Stringer MD, et al. Solid pseudopapillary tumour of the pancreas: Diverse presentation, outcome and histology. JOP. 2006;7(6):635–42.
Arias de la Vega F, Gómez Dorronsoro ML, Jiménez FJ. Subcutaneous metastasis as the first manifestation of a solid-pseudopapillary tumor of the pancreas. Clin Transl Oncol. 2006;8(2):136-8.
Cao D, Antonescu C, Wong G, et al. Positive immunohistochemical staining of KIT in solid-pseudopapillary neoplasms of the pancreas is not associated with KIT/PDGFRA mutations. Mod Pathol. 2006;19(9):1157–63.
Frago R, Fabregat J, Jorba R, et al. Solid pseudopapillary tumors of the pancreas: diagnosis and curative treatment. Rev Esp Enferm Dig. 2006;98(11):809–16.
Gedaly R, Toledano A, Millan G, et al. Treatment of liver metastases from a solid pseudopapillary tumor of the pancreas. J Hepatobiliary Pancreat Surg. 2006;13(6):587–90.
Hao CY, Lu AP, Xing BC, et al. Solid pseudopapillary tumor of the pancreas: report of 8 cases in a single institution and review of the Chinese literature. Pancreatology. 2006;6(4):291–6.
Kang CM, Kim KS, Choi JS, et al. Solid pseudopapillary tumor of the pancreas suggesting malignant potential. Pancreas. 2006;32(3):276–80.
Okino HH, Kitaura Y, Onitsuka K, et al. An operative case of metastatic solid-pseudopapillary tumor in the liver after curative resection. Japanese J Gastroenterol Surg. 2006;39(3):340–6.
Tipton SG, Smyrk TC, Sarr MG, et al. Malignant potential of solid pseudopapillary neoplasm of the pancreas. Br J Surg. 2006;93(6):733–7.
Zauls JA, Dragun AE, Sharma AK. Intensity-modulated radiation therapy for unresectable solid pseudopapillary tumor of the pancreas. Am J Clin Oncol. 2006;29(6):639–40.
Goh BK, Tan YM, Cheow PC, et al. Solid pseudopapillary neoplasms of the pancreas: An updated experience. J Surg Oncol. 2007;95(8):640–4.
Hah JO, Park WK, Lee NH, et al. Preoperative chemotherapy and intraoperative radiofrequency ablation for unresectable solid pseudopapillary tumor of the pancreas. J Pediatr Hematol Oncol. 2007;29(12):851–3.
Nagri S, Abdu A, Anand S, et al. Liver metastasis four years after Whipple’s resection for solid-pseudopapillary tumor of the pancreas. JOP. 2007;8(2):223–7.
Sumida W, Kaneko K, Tainaka T, et al. Liver transplantation for multiple liver metastases from solid pseudopapillary tumor of the pancreas. J Pediatric Surg. 2007;42(12):e27-31.
Kocman B, Jadrijević S, Skopljanac A, et al. Living donor liver transplantation for unresectable liver metastases from solid pseudo-papillary tumor of the pancreas: a case report. Transplant Proc. 2008;40(10):3787–90.
Shaikh S, Arya S, Ramadwar M, et al. Three cases of unusual solid pseudopapillary tumors. Can radiology and histology aid decision-making? JOP. 2008;9(2):150-9.
Sperti C, Berselli M, Pasquali C, et al. Aggressive behaviour of solid-pseudopapillary tumor of the pancreas in adults: a case report and review of the literature. World J Gastroenterol. 2008;14(6):960–5.
Li WH, Chan C, Cheung MT. A young woman with metastatic solid pseudopapillary tumour of the pancreas. ANZ J Surg. 2009;79(10):750–1.
Dovigo AG, Díaz MB, Gütierrez MG, et al. Liver transplantation as treatment in a massive metastasis from Gruber-Frantz pancreatic tumor: A case report. Transplant Proc. 2011;43(6):2272–3.
Gomez P, Yorke R, Ayala AG, et al. Solid-pseudopapillary neoplasm of pancreas with long delayed liver metastasis. Ann Diagn Pathol. 2012;16(5):380–4.
Honore C, Goere D, Dartigues P, et al. Peritoneal carcinomatosis from solid pseudopapillary neoplasm (Frantz’s tumour) of the pancreas treated with HIPEC. Anticancer Res. 2012;32(3):1069–73.
Ji S, Xu J, Zhang B, et al. Management of a malignant case of solid pseudopapillary tumor of pancreas: a case report and literature review. Pancreas. 2012;41(8):1336–40.
Krug S, Bartsch DK, Schober M, et al. Successful selective internal radiotherapy (SIRT) in a patient with a malignant solid pseudopapillary pancreatic neoplasm (SPN). Pancreatology. 2012;12(5):423–7.
Li JX, Wu H, Huang JW, et al. Synchronous intraoperative radiofrequency ablation for multiple liver metastasis and resection of giant solid pseudopapillary tumors of the pancreas. Chin Med J (Engl). 2012;125(9):1661–3.
Tajima Y, Kohara N, Maeda J, et al. Peritoneal and nodal recurrence 7 years after the excision of a ruptured solid pseudopapillary neoplasm of the pancreas: report of a case. Surg Today. 2012;42(8):776–80.
Yoon HJ, Lim JH. Solid pseudopapillary tumor of the pancreas with hepatic metastasis: spontaneous regression over 10-year follow-up period. Korean J Radiol. 2012;13(5):648–51.
Dixon M, Cannon J, Kagedan D, et al. Management of metastatic solid pseudopapillary cancer of the pancreas: a case report. World J Oncol. 2013;4(4–5):201–4.
Łągiewska B, Pacholczyk M, Lisik W, et al. Liver transplantation for nonresectable metastatic solid pseudopapillary pancreatic cancer. Ann Transplant. 2013;18:651–3.
Morikawa T, Onogawa T, Maeda S, et al. Solid pseudopapillary neoplasms of the pancreas: an 18-year experience at a single Japanese Institution. Surg Today. 2013;43(1):26–32.
Yagcı A, Yakan S, Coskun A, et al. Diagnosis and treatment of solid pseudopapillary tumor of the pancreas: experience of one single institution from Turkey. World J Surg Oncol. 2013;11:308.
Hosokawa I, Shimizu H, Ohtsuka M, et al. Preoperative diagnosis and surgical management for solid pseudopapillary neoplasm of the pancreas. J Hepato-biliary-Pancreatic Sci. 2014;21(8):573–8.
Prasad TV, Madhusudhan KS, Srivastava DN, et al. Transarterial chemoembolization for liver metastases from solid pseudopapillary epithelial neoplasm of pancreas: a case report. World J Radiol. 2015;7(3):61–5.
Violari EG, Brody LA, Covey AM, et al. Successful control of liver metastases from pancreatic solid-pseudopapillary neoplasm (SPN) using hepatic arterial embolization. Cardiovasc Intervent Radiol. 2015;38(2):479–83.
Choi HW, Park HJ, Hong SA, et al. Radiologic findings in extrapancreatic solid pseudopapillary tumor with aggressive behavior: a case report. J Korean Med Sci. 2017;32(12):2079–84.
Escobar MA, Jr., McClellan JM, Thomas W. Solid pseudopapillary tumour (Frantz's tumour) of the pancreas in childhood: successful management of late liver metastases with sunitinib and chemoembolisation. BMJ Case Reports. 2017.
Lee HS, Kim HK, Shin BK, et al. A rare case of recurrent metastatic solid pseudopapillary neoplasm of the pancreas. J Pathol Transl Med. 2017;51(1):87–91.
Yang F, Jin C, Fu D. Evolution of liver metastasis from solid pseudopapillary tumor of the pancreas. Surgery. 2017;161(6):1739–40.
Neill KG, Saller J, Al Diffalha S, et al. EGFR L861Q Mutation in a Metastatic Solid-pseudopapillary Neoplasm of the Pancreas. Cancer Genom Proteomics. 2018;15(3):201–5.
Prakash PS, Chan DYS, Madhavan K. The stomach: a rare site for metastatic solid pseudopapillary neoplasm of the pancreas. J Gastrointest Surg. 2018;22(4):759–60.
Wójciak M, Gozdowska J, Pacholczyk M, et al. Liver transplantation for a metastatic pancreatic solid-pseudopapillary tumor (Frantz Tumor): a case report. Ann Transplant. 2018;23:520–3.
Song TL, Chen H, Wang FR, et al. Combined treatment for solid pseudopapillary tumor of the pancreas with liver metastasis. Hepatobiliary Pancreat Dis Int. 2019;18(5):495–7.
Dyas AR, Johnson DT, Rubin E, et al. Yttrium-90 selective internal radiotherapy as bridge to curative hepatectomy for recurrent malignant solid pseudopapillary neoplasm of pancreas: case report and review of literature. J Surg Case Rep. 2020;2020(9):rjaa325.
Santos D, Calhau A, Bacelar F, et al. Solid pseudopapillary neoplasm of pancreas with distant metastasis during pregnancy: A diagnostic and treatment challenge. BMJ Case Rep. 2020;13(12).
Takaichi S, Iwagami Y, Kobayashi S, et al. Minimally invasive approach for pancreatic solid pseudopapillary neoplasm and initially undiagnosed slowly progressing liver tumor: a case report. Pancreas. 2020;49(8):e70–2.
Tomioka K, Ohike N, Aoki T, et al. Solid pseudopapillary neoplasm of the pancreas with high-grade malignant transformation involving p16-RB pathway alterations. Case Rep Surg. 2020;2020:5980382.
Ichimura K, Uesaka T, Kikuchi H, et al. Repeated resection for recurrent metastatic solid pseudopapillary neoplasm of the pancreas. Am J Case Rep. 2021;22:e934798.
Wang X, Zhu D, Bao W, et al. Case report: Targeted therapy for metastatic solid pseudopapillary neoplasm of the pancreas with CTNNB1 and PTEN mutations. Front Oncol. 2021;11:729151.
Park S, Park MG, Roh YH, et al. Solid pseudopapillary neoplasm of the pancreas with lymph node metastasis in a young male patient. Korean J Gastroenterol. 2022;79(2):77–82.
Ranaweera K, Nandasena M, de Silva U, et al. Solid pseudopapillary neoplasm of the pancreas with multiple liver metastases successfully managed with staged resection. SAGE Open Med Case Rep. 2022;10:2050313x221101995.
Nissen T, Wynn R. The clinical case report: a review of its merits and limitations. BMC Res Notes. 2014;7:264.
Hwang J, Kim DY, Kim SC, et al. Solid-pseudopapillary neoplasm of the pancreas in children: can we predict malignancy? J Pediatric Surg. 2014;49(12):1730–3.
Brecht IB, Schneider DT, Klöppel G, et al. Malignant pancreatic tumors in children and young adults: evaluation of 228 patients identified through the Surveillance, Epidemiology, and End Result (SEER) database. Klin Padiatr. 2011;223(6):341–5.
Kim MJ, Choi DW, Choi SH, et al. Surgical treatment of solid pseudopapillary neoplasms of the pancreas and risk factors for malignancy. Br J Surg. 2014;101(10):1266–71.
Butte JM, Brennan MF, Gönen M, et al. Solid pseudopapillary tumors of the pancreas. Clinical features, surgical outcomes, and long-term survival in 45 consecutive patients from a single center. J Gastrointest Surg. 2011;15(2):350-7.
You L, Yang F, Fu DL. Prediction of malignancy and adverse outcome of solid pseudopapillary tumor of the pancreas. World J Gastrointest Oncol. 2018;10(7):184–93.
Yin Q, Wang M, Wang C, et al. Differentiation between benign and malignant solid pseudopapillary tumor of the pancreas by MDCT. Eur J Radiol. 2012;81(11):3010–8.
Soloni P, Cecchetto G, Dall'igna P, et al. Management of unresectable solid papillary cystic tumor of the pancreas. A case report and literature review. J Pediatr Surg. 2010;45(5):e1-6.
Yalçın B, Yağcı-Küpeli B, Ekinci S, et al. Solid pseudopapillary neoplasm of the pancreas in children: Hacettepe experience. ANZ J Surg. 2019;89(6):E236–40.
Botta L, Gatta G, Trama A, et al. Incidence and survival of rare cancers in the US and Europe. Cancer Med. 2020;9(15):5632–42.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Clin Res ed). 2021;372:n71.
Acknowledgment
The National Cancer Database (NCDB) is a joint project of the Commission on Cancer (CoC) of the American College of Surgeons and the American Cancer Society. The CoC's NCDB and the hospitals participating in the CoC’s NCDB are the source of the de-identified data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Author information
Authors and Affiliations
Contributions
The authors included each contributed substantially to this research as per the guidelines of the International Committee of Medical Journal Editors (ICMJE).
Corresponding author
Ethics declarations
Disclosures
The authors declare no financial disclosures or conflicts of interest related to the research described in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10434_2023_14343_MOESM2_ESM.tiff
Supplemental Fig. S1 Treatment analysis flow diagram for 164 reported cases of malignant solid pseudopapillary neoplasm of the pancreas. mSPN malignant SPN (TIFF 11531 KB)
10434_2023_14343_MOESM3_ESM.tiff
Supplemental Fig. S2 Treatment analysis follow diagram for 692 cases of solid pseudopapillary neoplasm of the pancreas in the National Cancer Database. mSPN malignant SPN (TIFF 11531 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fleming, A.M., Hendrick, L.E., Yakoub, D. et al. Malignant Solid Pseudopapillary Neoplasm of the Pancreas: An Orthogonal Analysis. Ann Surg Oncol 31, 475–487 (2024). https://doi.org/10.1245/s10434-023-14343-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-14343-0