Abstract
Background
Solid pseudopapillary neoplasms (SPN) are rare tumors of the pancreas, typically affecting young women. Resection is the mainstay of treatment but is associated with significant morbidity and potential mortality. We explore the idea that small, localized SPN could be safely observed.
Methods
This retrospective review of the Pancreas National Cancer Database from 2004 to 2018 identified SPN via histology code 8452.
Results
A total of 994 SPNs were identified. Mean age was 36.8 ± 0.5 years, 84.9% (n = 844) were female, and most had a Charlson–Deyo Comorbidity Coefficient (CDCC) of 0–1 (96.6%, n = 960). Patients were most often staged clinically as cT2 (69.5%, n = 457) followed by cT3 (17.6%, n = 116), cT1 (11.2%, n = 74), and cT4 (1.7%, n = 11). Clinical lymph node and distant metastasis rates were 3.0 and 4.0%, respectively. Surgical resection was performed in 96.6% of patients (n = 960), most commonly partial pancreatectomy (44.3%) followed by pancreatoduodenectomy (31.3%) and total pancreatectomy (8.1%). In patients clinically staged as node (N0) and distant metastasis (M0) negative, occult pathologic lymph node involvement was found in 0% (n = 28) of patients with stage cT1 and 0.5% (n = 185) of patients with cT2 disease. The risk of occult nodal metastasis significantly increased to 8.9% (n = 61) for patients with cT3 disease. The risk further increased to 50% (n = 2) in patients with cT4 disease.
Conclusions
Herein, the specificity of excluding nodal involvement clinically is 99.5% in tumors ≤ 4 cm and 100% in tumors ≤ 2 cm. Therefore, there may be a role for close observation in patients with cT1N0 lesions to mitigate morbidity from major pancreatic resection.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Solid pseudopapillary neoplasm (SPN) is a rare pancreatic tumor defined by the World Health Organization as an epithelial low-grade malignant neoplasm with a gross pseudopapillary appearance and a cystic microscopic appearance.1,2 Young women are predominantly affected and often diagnosed in the second and third decades of life.3,4 Lesions can occur throughout the pancreas, but most commonly arise in the tail or body of the pancreas (61%), followed by the head of the pancreas (34%).1,2 Symptoms can vary on the basis of location of the tumor and include abdominal pain, nausea, vomiting, weight loss, and obstructive jaundice.5 Increasingly, asymptomatic SPNs are identified incidentally (up to 38% of SPN diagnoses) in patients who undergo imaging for an unrelated reason.6
Currently there are no defined stage-specific guidelines or recommendations in the existing literature as to direct management of SPN.7 Due to the rarity of SPN, all studies are retrospective and are mostly limited to case reviews or small single-institution studies with less than 50 patients.4,8,9,10,11 Most research congregates all T stages of SPN together, with special dispensation given only for those with nodal or distant metastasis. Complete resection is the generally accepted treatment with surgical approach dependent on the location of the tumor. Overall 5-year survival is excellent and has been quoted as high as 95%. However, there is the potential for significant morbidity and mortality following pancreatic resection, and in some cases the risks of surgery may outweigh the risks of a small SPN.1 Given the indolent nature of SPN, this study set out to evaluate the reliability of clinical staging to determine if there was a subset of patients with small, localized SPN who could be considered for observation as an alternative to surgical resection.
Patients and methods
Data Source
This study was a retrospective review from 2004 to 2018 of the National Cancer Database (NCDB), a clinical oncology database sponsored by the American College of Surgeons and the American Cancer Society. These self-reported and unverified data represent more than 1500 Commission on Cancer (CoC)-accredited institutions, and as such, the NCDB is not responsible for the validity of the data provided or the conclusions drawn.
Study Population
All patients within the pancreas NCDB with ICD-0-3 code 8452, delineating solid pseudopapillary carcinoma, were selected. Only patients with invasive disease (T1 and higher) were analyzed. NCDB uses the 7th edition of the American Joint Committee on Cancer (AJCC) Cancer Staging Manual for clinical and pathologic staging. T stage is defined as follows: T1: 0–2 cm, T2: 2–4 cm, T3: > 4 cm, and T4: tumor extends past the pancreas. N1 is defined as any nodal involvement and M1 denotes distant metastasis. Clinical staging is denoted as cTxNxMx and pathologic staging denoted as pTxNxMx. For analysis of strictly clinical or pathologic staging, only patients with full staging profiles were selected. Similarly, for survival analysis, only those with complete clinical staging profiles were selected.
Study Variables
Demographic data collected included age, sex, race, and Charlson–Deyo Comorbidity Coefficient (CDCC). Patients were grouped by race into four groups: white, Black, Asian, or other. Treatment with chemotherapy or surgery, as well as type of surgical procedure, was collected. Surgical procedure was defined as the most invasive procedure performed during the patient’s treatment course. These included site-specific codes for localized pancreatic resection (25), partial pancreatectomy (30, i.e., distal/central pancreatectomy), pancreatectomy with associated duodenectomy with or without partial gastrectomy (35, 36, 37), and total pancreatectomy with or without gastrectomy/duodenectomy (40, 60).
Statistical Analysis
Statistical analysis was performed SPSS 21.0 (IBM Corp, Armonk, NY) and graphs were created using SPSS and Prism 7 (GraphPad Software, La Jolla, CA). Binary outcomes compared between two groups were assessed via chi-squared with Bonferroni post hoc analysis, whereas continuous variables were compared for significance with analysis of variance (ANOVA) analysis of the means. Continuous variables are reported as mean (± standard deviation). Overall survival was analyzed via Cox regression. Significance was set at p ≤ 0.05.
Results
SPN is a Rare Tumor
A total of 994 patients were identified as having been diagnosed with SPN between 2004 and 2018 (Fig. 1, left axis). The number of SPNs recorded in the NCDB increased from 19 patients in 2004 to 144 patients in 2018, a greater than sevenfold increase. The NCDB also grew during this time, and the proportion of SPN within the NCDB grew from 0.1 to 0.4%, a fourfold increase (Fig. 1, right axis). AJCC cT1 and cT2 stage tumors make up a majority of these cases (82.8%), a composition that has been maintained over the identified study period.
Total SPN Demographics, Treatment, and Staging
All 994 patients were included in this analysis (Table 1). Patients had a mean age of 36.8 ± 0.5 years, with a pediatric (≤ 18 years old) population of 11.7% (n = 116). Patients were predominantly female (84.9%, n = 844). Most patients were white (67.5%, n = 663) or Black (23.2%, n = 228) and had a CDCC of 0–1 (96.6%, n = 960). Of the total cohort, 91.6% (n = 911) patients underwent surgical resection of their tumors. A total of 3.4% (n = 34) of the population received chemotherapy in conjunction with surgery, and 1.4% (n = 24) were treated with chemotherapy alone. The majority of patients were staged clinically as cT2 (n = 457), with predominantly cN0 (98%, n = 448) and cM0 (98.2%, n = 449) disease. Compared with patients with cT2 disease, patients with cT3 disease (n = 116) had a significantly higher rate of N1 (6.9% vs. 2.0%, p = 0.005) and M1 (9.5% vs. 1.8%, p < 0.001) disease. Patients with cT1 disease (n = 74) had no nodal disease (100%, n = 74). One patient was clinically noted to have distant metastasis (1.4%), which was later confirmed on pathologic assessment as pT1N0M1 disease. Patients with cT4 disease (n = 11) had high rates of N1 (27.3%, n = 3) and M1 (54.5%, n = 6) disease.
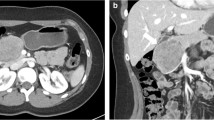
Occult Lymph Node/Metastatic Spread Is Rare in Patients with cT 1 /cT 2 Disease
Preoperative clinical staging was compared with postoperative pathologic staging in patients who were clinically node negative and distant metastasis negative to evaluate the likelihood of occult disease. To adequately assess the accuracy of clinical staging, only patients with full clinical and pathologic assessment were included in this analysis (Table 2, n = 276). For patients staged as cT1N0M0, pathological staging demonstrated upstaging to pT2 or pT3 disease in 28.6% (n = 8) of patients, while no patients were found to have nodal or metastatic disease. Patients with cT2N0M0 disease were upstaged to pT3 and pT4 disease in 19.5% of patients (n = 36), and 1.6% were downstaged to pT1 disease (n = 3). Only one patient with cT2 disease was discovered to have occult nodal disease (0.5%, n = 184), and none of these patients had occult metastatic disease (0.0%, n = 185). Seven patients with cT3 disease were downstaged to pT2 (11.5%) and one patient (1.6%) was upstaged to pT4. Interestingly, the likelihood of discordant nodal staging significantly increased to 8.9% (n = 5) in cT3 compared with cT1 (0%, n = 0) and cT2 (0.5%, n = 1, p < 0.001), though no metastatic disease was identified in these patients. Therefore, the specificity of predicting nodal involvement was 0% for cT1, 0.5% for cT2, 8.9% for cT3, and 50% for cT4.
Perioperative Outcomes
The previous population of patients with cTxN0M0 disease was subsequently analyzed as to their operative interventions. Most patients underwent major resections in the form of distal/central pancreatectomy (Table 3, 47.5%), followed by pancreatoduodenectomy (41.0%), total pancreatectomy ± gastrectomy/duodenectomy (5.8%), or other (5.8%). Post-surgical outcomes for stages cT1, cT2, and cT3 were similar, with no significant differences in length of stay (range 7.39–7.97 days), 30-day readmission rates (range 6.7–10.7%), and 30- and 90-day mortality (0.0–5.6%). Overall perioperative mortality was low for these patients, however, the cT3 cohort did report one postoperative death within 90 days (5.6%) after extended pancreatectomy.
Stage-Specific Survival
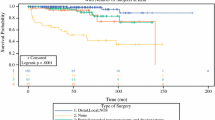
Cox regression analysis in patients with a full clinical staging profile, controlling for age and CDCC, was conducted after stratifying by AJCC clinical T stage in patients who are clinically node and metastasis negative (n = 621, Fig. 2a). Overall survival for cT1, cT2, and cT3 was similar with excellent long-term survival. The 5- and 10-year survival was 100% for cT1, 97.5% for cT2, and 94.4% for cT3. A marked drop in survival to 50% (for 5- and 10-year survival) was seen in patients with cT4 disease. There was a significant difference when compared with cT2 disease as there was sufficient power to establish significance (HR 14.80, 95% CI 1.29–170.07, p = 0.03).
a Cox regression analysis controlling for age and Charlson–Deyo Comorbidity Coefficient stratifying by AJCC clinical T stage in patients who are clinically node negative, metastasis negative, b survival in all patients stratified by clinical nodal status age, CDCC, and AJCC clinical T stage, c survival in all patients stratified by clinical metastasis controlling for age, CDCC, and AJCC clinical T stage
After controlling for age, CDCC, and AJCC clinical T stage in all patients with full clinical profiles (n = 662), median OS was significantly worse in patients with node positive disease compared with those without nodal disease (HR 3.60, CI 1.66–7.82, p = 0.001, Fig. 2b). Similarly, patients with metastatic disease had significantly worse median OS compared with those without distant metastatic disease (HR 10.49, CI 5.38–20.44, p = 0.001, Fig. 2c).
Discussion
The current literature on SPN lacks granularity regarding stage-specific outcomes and treatment strategies. This study aimed to approach long-term outcomes of SPN as one would in the outpatient setting, with clinical staging as a potential decision point.
SPN remains a rare diagnosis, making up approximately 0.9–3% of exocrine pancreatic tumors.12,13 This study showed a fourfold increase in the proportion of SPNs within the NCDB for pancreatic cancer over the study period, and a sevenfold increase in total diagnoses. Most likely, this increase in detection in the NCDB is due to the improvement and increased utilization of advanced imaging and the subsequent increasing identification of incidental pancreatic masses.14,15 One review demonstrated that SPN accounted for 3–15% of all solid pancreatic incidentalomas.15 As the detection of incidental pancreas tumors increases due to improved imaging modalities, it stands to reason that these tumors will be detected at smaller sizes in otherwise asymptomatic patients. Law et al. showed that there has been a decrease in the size of SPN (9.8–8.1 cm) when comparing those identified before 2000 to those found between 2000 and 2012.6 Our study shows that a majority (83%) are cT1–2, and most do not have nodal involvement or distant metastasis. Earlier detection of SPN necessitates adjustment of our approach to treatment.
It is well established that the rates of nodal and distant metastasis are low in all comers with SPN, approximately 0.5–2.0 and 1.8–7.7%, respectively.6,16,17 This is confirmed in this study, with overall lymph node and distant metastasis rates on pathologic assessment of 3.5 and 4.4%, respectively. Interestingly, there were 16 patients found to have metastatic disease without lymph node involvement. Patients with large tumors or clinical lymph node involvement require pancreatectomy to prevent local complications and metastatic spread. Those with extensive distant metastasis are unlikely to benefit from surgical resection, but there may be a role for resection in patients with limited oligometastatic disease. Most patients have localized disease without radiographic evidence of lymph node involvement or distant metastasis (cT1–3N0M0). This study confirms that occult lymph node involvement on pathologic assessment is exceedingly rare in small tumors, 0% for cT1 and 0.5% for cT2 tumors. Importantly, this risk increases to 8.9% in cT3 lesions. However, given the lack of stage-specific treatment guidelines, surgeons typically treat a 5 mm localized tumor in the same manner as a bulky T3 lesion with clinical lymph node involvement.
Irrespective of stage, early surgical resection is the mainstay of treatment for SPN. There is even evidence supporting prolonged survival with resection in metastatic disease.12,18 For body/tail lesions, a distal pancreatectomy is performed, with or without splenic preservation (47.5% of study population).4,16 For pancreatic head lesions, a much more complex procedure is warranted, as evidenced by the 41% of patients who underwent pancreatoduodenectomy in this study. Our study shows favorable outcomes regardless of T stage, as these patients are typically young and otherwise healthy. However, that does not mean that these invasive procedures are without risk. Though mortality has improved over the years (2–4%), morbidity remains high for the Whipple procedure (38–51%).19,20,21 Bearing in mind that these may be incidental, localized, sub-centimeter pancreatic masses, it calls to question the intense nature of the treatment. For instance, although there was only one perioperative mortality in this study (0.4%), it was a 22-year-old woman with no comorbidities, a devastating outcome for such a young patient. One institution performed local disease resection (even in the pancreatic head) for 62 patients and reported no local recurrence or distant metastasis over a median follow-up period of 46 months, suggesting extensive oncologic resection may not be required for SPN.22
Immediate postoperative complications and mortality rates are likely not comparable to general Whipple morbidity and mortality in this highly selected group of young patients, however, even in cases without complication, it requires subjecting young adults to life-altering operations and the subsequent long-term complications. These include bowel obstruction, nutritional deficiency, hernia, and undesired cosmetic outcomes. Perhaps most importantly, new onset diabetes mellitus (DM) is a potential consequence of pancreatic resection, and with rates estimated between 9 and 31% for pancreatectomy depending on extent of resection and patient risk factors, the potential morbidity of subjecting an individual to DM for the majority of their adult life is significant.23,24
There is increased interest in observing small lesions within the pancreas, including pancreatic neuroendocrine tumor (pNET) and intraductal papillary mucinous neoplasm (IPMN). SPN is less common than IPMN and pNET, and as such, there has been less opportunity to consider a nonoperative approach. Furthermore, these tumors have traditionally been diagnosed in the setting of symptoms related to large tumors, but as smaller SPNs are increasingly diagnosed incidentally, the management approach needs to evolve. Previously, all patients with pNET qualified for resection. Now, data show that a subset of these tumors, < 1–2 cm in size, can be safely observed with short interval follow-up during which any disease progression triggers an intervention.25,26,27 The malignant potential of NET can be as high as 50%, whereas that of SPN is approximately 10–15%.22,28 There have even been isolated case reports of spontaneous regression and resolution of SPN without treatment.29,30,31 We have established in this study that the specificity of predicting nodal involvement clinically is 99.5% in tumors ≤ 4 cm (T1/2) and 100% in tumors ≤ 2 cm (T1). We suggest that there could be a role for short-interval observation in small, localized SPN without nodal involvement (T1, ≤ 2 cm).
We propose that all patients with symptomatic SPN, high-risk pathologic features, or SPN > 2 cm undergo surgical resection, as is current standard practice. For a small localized cN0M0 SPN < 2 cm, we suggest that it is reasonable to consider observation after an informed discussion with the patient about the risk/benefits of both observation and the potential morbidity of resection. Each patient will have a different perspective regarding the risks/benefits of surgery versus observation, and a careful, nuanced, and personalized decision will need to be made in conjunction with their surgeon on the basis of patient age, comorbidities, location of the SPN, and personal preferences. As the data regarding growth kinetics of SPN is not yet sufficient to base formal long-term recommendations, we propose an initial period of surveillance of 3–6 months with high quality computed tomography (CT)/MRI, with the opportunity to further space to 6–12 months on the basis of the specific growth pattern and patient risk factors for resection, in keeping with surveillance recommendations for small, asymptomatic IPMN32,33 and pNET.34,35 Though we acknowledge these are distinct disease processes, they are the most similar to small, asymptomatic SPN at this time. A multi-institutional disease-specific registry would allow for future SPN-specific, evidence-based recommendations.
As is evident in this paper, this population of patients is relatively young, and as such, long-term surveillance may continue for decades. One major downside of long-term surveillance is the increased anxiety associated with a perceived delay in therapy, and this needs to be addressed with the patient from the beginning. Further analysis of the healthcare costs incurred with both approaches is also required, though this should not dictate care by itself. Given the serious nature of pancreatic surgery and the complications listed above, patients should be counseled on the risks/benefits of observation versus surgery and share in the decision making.
Limitations
There are several limitations in this study, including missing data and lack of granularity of the available data with the NCDB. Firstly, the NCDB does not capture all incidence throughout the USA as it reports only Commission on Cancer (CoC) institutions, which only represent approximately 70% of all cancer diagnoses and allows for bias in the types of institutions participating in this registry. Most significantly for this study, complete clinical and pathologic staging was absent for a significant proportion of the 911 patients that underwent resection, leaving 276 patients who were node negative and metastasis negative for analysis. Additionally, modality of clinical staging is not listed and can vary on the basis of institution and resources; though most clinical staging is obtained from endoscopic ultrasound (EUS), CT scans, or MRI, each of these carry its own sensitivity and specificity for all aspects of TNM stage. Further, as almost all patients underwent surgery, there is no control group for which to compare overall survival in a balanced way. Similarly, though almost all patients underwent resection, the true accuracy of clinical staging cannot be known as long as some patients do not have pathologic confirmation. Therefore, one cannot draw conclusions so much as make observations. The next step should be a multicenter, small-cohort observational study with serial imaging to evaluate the growth of small, localized SPN to gain prospective data regarding this disease.
Conclusions
This study is one of the largest retrospective reviews of SPNs and may be able to provide new data that can help to direct treatment and counsel patients. These data show that low grade SPN has low propensity for aggressive disease and may be acceptable for surveillance in select patients. Further prospective studies are needed to categorize the growth and malignant transformation potential of SPN.
References
Torres OJM, Rezende MB, Waechter FL, et al. Pancreatoduodenectomy for solid pseudopapillary tumor of the pancreas: a multi-institution study. Arq Bras Cir Dig. 2019;32(2):e1442.
Hamilton S, Aaltonen L, World Health Organization classificaiton of tumors. Pathology and genetics of tumours of the digestive system. USA: IARC Press; 2000.
Vollmer CM Jr, Dixon E, Grant DR. Management of a solid pseudopapillary tumor of the pancreas with liver metastases. HPB. 2003;5(4):264–7.
Yagci A, Yakan S, Coskun A, et al. Diagnosis and treatment of solid pseudopapillary tumor of the pancreas: experience of one single institution from Turkey. World J Surg Oncol. 2013;11:308.
Lanke G, Ali FS, Lee JH. Clinical update on the management of pseudopapillary tumor of pancreas. World J Gastrointest Endosc. 2018;10(9):145–55.
Law JK, Ahmed A, Singh VK, et al. A systematic review of solid-pseudopapillary neoplasms: are these rare lesions? Pancreas. 2014;43(3):331–7.
Romics L Jr, Olah A, Belagyi T, Hajdu N, Gyurus P, Ruszinko V. Solid pseudopapillary neoplasm of the pancreas–proposed algorithms for diagnosis and surgical treatment. Langenbecks Arch Surg. 2010;395(6):747–55.
Shuja A, Alkimawi KA. Solid pseudopapillary tumor: a rare neoplasm of the pancreas. Gastroenterol Rep. 2014;2(2):145–9.
Abudalou M, Vega EA, Dhingra R, et al. Solid pseudopapillary neoplasm-diagnostic approach and post-surgical follow up: three case reports and review of literature. World J Clin Cases. 2021;9(7):1682–95.
Jena SS, Ray S, Das SAP, Mehta NN, Yadav A, Nundy S. Rare Pseudopapillary neoplasm of the pancreas: a 10-year experience. Surg Res Pract. 2021;2021:7377991.
Lubezky N, Papoulas M, Lessing Y, et al. Solid pseudopapillary neoplasm of the pancreas: management and long-term outcome. Eur J Surg Oncol. 2017;43(6):1056–60.
Martin RC, Klimstra DS, Brennan MF, Conlon KC. Solid-pseudopapillary tumor of the pancreas: a surgical enigma? Ann Surg Oncol. 2002;9(1):35–40.
Sharma I, Cho WC, Thaker S, et al. Solid pseudopapillary neoplasm of the pancreas. J Pediatr Surg Case Rep. 2018;37:63–9.
Stensbol AB, Krogh J, Holmager P, et al. Incidence, Clinical presentation and trends in indication for diagnostic work-up of small intestinal and pancreatic neuroendocrine tumors. Diagnostics. 2021;11(11):2030.
Santo E, Bar-Yishay I. Pancreatic solid incidentalomas. Endosc Ultrasound. 2017;6(Suppl 3):S99–103.
Yu PF, Hu ZH, Wang XB, et al. Solid pseudopapillary tumor of the pancreas: a review of 553 cases in Chinese literature. World J Gastroenterol. 2010;16(10):1209–14.
De Robertis R, Marchegiani G, Catania M, et al. Solid pseudopapillary neoplasms of the pancreas: clinicopathologic and radiologic features according to size. AJR Am J Roentgenol. 2019;213(5):1073–80.
Albuquerque GPX, Ramos A, Anaissi AKM, et al. Hepatic metastasis in Frantz’s tumor: a case report. Int J Surg Case Rep. 2020;71:66–9.
Distler M, Ruckert F, Hunger M, et al. Evaluation of survival in patients after pancreatic head resection for ductal adenocarcinoma. BMC Surg. 2013;13:12.
Cusworth BM, Krasnick BA, Nywening TM, et al. Whipple-specific complications result in prolonged length of stay not accounted for in ACS-NSQIP Surgical Risk Calculator. HPB. 2017;19(2):147–53.
Pugalenthi A, Protic M, Gonen M, et al. Postoperative complications and overall survival after pancreaticoduodenectomy for pancreatic ductal adenocarcinoma. J Surg Oncol. 2016;113(2):188–93.
Zhang C, Liu F, Chang H, et al. Less aggressive surgical procedure for treatment of solid pseudopapillary tumor: limited experience from a single institute. PLoS ONE. 2015;10(11):e0143452.
Wu L, Nahm CB, Jamieson NB, et al. Risk factors for development of diabetes mellitus (Type 3c) after partial pancreatectomy: a systematic review. Clin Endocrinol. 2020;92(5):396–406.
Burkhart RA, Gerber SM, Tholey RM, et al. Incidence and severity of pancreatogenic diabetes after pancreatic resection. J Gastrointest Surg. 2015;19(2):217–25.
Lee LC, Grant CS, Salomao DR, et al. Small, nonfunctioning, asymptomatic pancreatic neuroendocrine tumors (PNETs): role for nonoperative management. Surgery. 2012;152(6):965–74.
Gaujoux S, Partelli S, Maire F, et al. Observational study of natural history of small sporadic nonfunctioning pancreatic neuroendocrine tumors. J Clin Endocrinol Metab. 2013;98(12):4784–9.
Bettini R, Partelli S, Boninsegna L, et al. Tumor size correlates with malignancy in nonfunctioning pancreatic endocrine tumor. Surgery. 2011;150(1):75–82.
Gallotti A, Johnston RP, Bonaffini PA, et al. Incidental neuroendocrine tumors of the pancreas: MDCT findings and features of malignancy. AJR Am J Roentgenol. 2013;200(2):355–62.
Yoon HJ, Lim JH. Solid pseudopapillary tumor of the pancreas with hepatic metastasis: spontaneous regression over 10-year follow-up period. Korean J Radiol. 2012;13(5):648–51.
Hachiya M, Hachiya Y, Mitsui K, Tsukimoto I, Watanabe K, Fujisawa T. Solid, cystic and vanishing tumors of the pancreas. Clin Imaging. 2003;27(2):106–8.
Suzuki M, Shimizu T, Minowa K, Ikuse T, Baba Y, Ohtsuka Y. Spontaneous shrinkage of a solid pseudopapillary tumor of the pancreas: CT findings. Pediatr Int. 2010;52(2):335–6.
Tanaka M, Fernandez-del Castillo C, Adsay V, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012;12(3):183–97.
Vege SS, Ziring B, Jain R, Moayyedi P, Clinical Guidelines C, American Gastroenterology A. American gastroenterological association institute guideline on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology. 2015;148(4):819–22.
(NCCN) NCCN. NCCN Clinical Practice Guidelines in Oncology. Neuroendocrine Adrenal Tumor (Version 1.2022). 2022.
Partelli S, Ramage JK, Massironi S, et al. Management of asymptomatic sporadic nonfunctioning pancreatic neuroendocrine neoplasms (ASPEN) ≤ 2 cm: study protocol for a prospective observational study. Front Med. 2020;7:598438.
Funding
There was no outside funding or influence in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
There are no conflicts of interest for any of the authors listed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Standring, O., Benitez Sanchez, S., Pasha, S. et al. Potential Role for Observation in Small Solid Pseudopapillary Neoplasm (SPN). Ann Surg Oncol 30, 5105–5112 (2023). https://doi.org/10.1245/s10434-023-13496-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-13496-2