Abstract
Background
The peritoneum frequently is the only recurrence site after radical resection of gastric cancer. Data suggest that hyperthermic intraperitoneal chemotherapy (HIPEC) and intraoperative radiotherapy (IORT) reduce peritoneal recurrence and possibly improve survival for patients with resected gastric and serosal involvement. This study aimed to evaluate the efficacy of combining prophylactic HIPEC and IORT after radical resection of localized gastric cancer.
Methods
In this retrospective study, the medical records of adult patients with histologically proven gastric/gastroesophageal adenocarcinoma who underwent radical resection with curative intent were evaluated for recurrence and survival according to whether they received prophylactic HIPEC and IORT.
Results
The eligibility criteria were met by 58 patients, 33 of whom underwent prophylactic HIPEC and IORT after radical surgery. Overall, 91% the HIPEC/IORT group and 72% of the surgery-only group had ≤pT3 disease. The median follow-up period was 26.6 months for the HIPEC/IORT group and 50.6 months for the surgery group. Locoregional recurrence occurred for six patients (18.1%) in the HIPEC/IORT group and five patients (20%) in the surgery-only group, with peritoneal metastasis (PM) occurring in respectively three (9%) and six (24%) patients. The median recurrence-free survival (RFS) duration was 23.2 months (95% confidence interval [CI] 6.5–39.9 months) for the HIPEC/IORT group versus 24.8 months (95% CI 0.0–51.1 months) for the surgery-only group (p = 0.88), and the corresponding 5-year overall survival (OS) estimates were 69% and 58%.
Conclusion
Prophylactic HIPEC and IORT after radical surgery for localized gastric or gastroesophageal cancer did not improve RFS or OS for an unselected group of patients at risk for peritoneal recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Gastric cancer (GC) is one leading cause of cancer-related mortality worldwide.1 Approximately 55% of patients present with locoregional disease, which usually is treated by surgical resection ± neoadjuvant and/or adjuvant chemotherapy.2 Despite this, more than 50% of these patients relapse and die of GC.3
Peritoneal carcinomatosis (PC) represents 40–50% of the cases of treatment failure after perioperative systemic chemotherapy and radical surgery among patients with localized GC.4,5 Furthermore, findings have shown PC to be a poor prognostic feature for patients with metastatic GC.6 The median overall survival (OS) is reported to be 4.6 months for GC patients with peritoneal metastases alone and 3.3 months for those with other organ metastasis.7
The pathogenesis of PC after curative surgery for GC might be explained by the “tumor cell entrapment hypothesis” suggested by Sugarbaker et al.,8 which proposes that intraperitoneal free cancer cells (IFCCs) adhere to the raw surgical area within minutes through fibrin entrapment. This is assisted by cytokine release as part of the wound-healing mechanism. The hypoxic environment renders the trapped cancer cells relatively immune to the effects of systemic chemotherapy. Intraperitoneal chemotherapy is therefore intended to clear these free cancer cells that persist after curative resection.9,10 Both hyperthermia and intraperitoneal chemotherapy have synergistic cytotoxic effects on IFCCs.11
The role of prophylactic hyerthermic intraperitoneal chemotherapy (HIPEC) for high-risk localized GC is controversial. Both retrospective and small-sample prospective studies suggest that survival is improved and peritoneal recurrence is decreased with prophylactic HIPEC for localized GC patients who have high-risk features for peritoneal recurrence.12,13,14
The role of radiation therapy in managing GC is not well defined. Several trials have failed to show improvements in survival by adding external beam radiotherapy to the perioperative treatment.15,16
On the other hand, intraoperative radiotherapy (IORT) has led to a reduction in local recurrence for patients who have advanced locoregional disease, with no apparent OS benefit.17,18
In our study, we analyzed the impact of combining prophylactic HIPEC with IORT, performed as part of standard treatment, and compared the results with those of patients who underwent surgical resection alone.
Patients and Methods
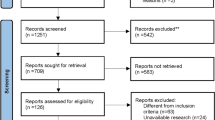
This retrospective study reviewed the medical records of patients with a confirmed diagnosis of gastric or gastroesophageal junction adenocarcinoma managed at a tertiary care institution. The inclusion criteria specified adult patients 18 years of age or older, localized disease at presentation, laparotomy performed for definitive surgery, no evidence of peritoneal or other metastasis intraoperatively, and surgical resection with curative intent. Pre- or postoperative chemotherapy was allowed.
Staging evaluations were performed using computed tomography (CT) of the chest, abdomen, and pelvis as well as positron emission tomography (PET). No endoscopic ultrasound was performed for staging.
The patients were divided into two groups: those who underwent curative gastrectomy only (surgery-only group) and those who underwent curative gastrectomy with prophylactic HIPEC and IORT (HIPEC/IORT group). All the treatments were considered standard at that time and performed by different operating surgeons.
The data collected included age, sex, clinical stage, pathologic stage, histologic subtype, human epidermal growth factor receptor 2 (HER2)/neu overexpression, margin, and use of pre- and postoperative chemotherapy.
The surgical procedure was either total or subtotal gastrectomy with D2 lymphadenectomy. In addition, patients treated with the HIPEC procedure underwent additional total peritonectomy.
The chemotherapy agents used for the HIPEC procedure were mitomycin C and cisplatin, or melphalan. The perfusate was heated. Thermal probes continuously monitored the intraperitoneal temperature in the abdominopelvic cavity to ensure that the temperature remained at 41–42.2 °C.
At the end of the HIPEC procedure, the abdominopelvic cavity was lavaged with copious volumes of normal saline. The HIPEC drains were removed intraoperatively, and Jackson–Pratt drains were inserted as indicated. The median operative time was 270 min (range 240–360 min).
The IORT procedure was performed using the Mobetron self-shielded electron beam linear accelerator machine (IntraOp Medical Corporation; Sunnyvale, CA, USA). The patients underwent IORT before undergoing anastomosis and after lymphadenectomy. The dose given was 10–12 Gray (Gy) for negative resection margins (R0), 12–15 Gy for microscopic positive resection margins (R1), and 15–20 Gy for macroscopic/gross residual tumors (R2). Unaffected organs were shielded by lead bars to reduce radiation exposure. The indications, dose, and technique for IORT were decided case by case after review by the surgeon, radiation oncologist, clinical pharmacist, and medical oncologist according to the aforementioned criteria.
The patient characteristics are summarized as frequencies with percentages for categorical variables and as medians with interquartile ranges for continuous variables. Overall survival was defined as the time to death from any cause. The patients alive at the last follow-up visit were censored. Recurrence-free survival (RFS) was defined as the time to disease recurrence or death. The patients alive and free of recurrence at the last follow-up visit were censored.
The probabilities of OS and RFS were summarized using a Kaplan–Meier estimator, with variance calculated using the Greenwood formula. Survival curves were compared using the log-rank test. A p value lower than 0.05 was considered significant. Statistical analysis was performed using RStudio, version 1.4.1717 2009–2021 (Rstudio, PBC, Boston, MA).
This study was approved by the hospital research ethics committee (approval no. RAC 2181165). In addition, the research ethics committee granted a waiver for patient consent given the study’s retrospective nature.
Results
From January 2009 to the end of 2018, 58 patients met the inclusion criteria. Of the 58 patients, 25 underwent gastrectomy without HIPEC/IORT, and 33 underwent gastrectomy followed by prophylactic HIPEC and IORT. The patient characteristics are summarized in Table 1. Interestingly, the median age for the surgery-only group was significantly younger than for the HIPEC/IORT group (54 vs. 64 years; p = 0.02).
The number of patients with diffuse and intestinal subtypes of disease was significantly lower in the surgery-only group than in the HIPEC/IORT group (12% and 20% vs. 33.3% and 39.4%; p < 0.001). Additionally, HER2/neo was overexpressed in 8% of the surgery-only group and 18% of the HIPEC/IORT group (p < 0.001). The median number of preoperative chemotherapy cycles was higher in the HIPEC/IORT group than in the surgery-only group (5 vs. 3; p = 0.006).
All the patients in the surgery-only group received neoadjuvant chemotherapy (20 received EOX, 4 received FOLFOX, and 1 received docetaxel). One patient in the HIPEC/IORT group did not receive neoadjuvant chemotherapy. Two patients received concurrent chemoradiotherapy with paclitaxel and carboplatin (CROSS protocol), and the other preoperative chemotherapy regimens were as follows: 12 EOX, 12 FOLFOX, 3 XELOX, and 3 FLOT regimens. The adjuvant therapies in the surgery-only group were as follows: 11 EOX, 1 FOLFOX/XELOX, and 1 capecitabine. In the HIPEC/IORT group, six patients received EOX, eight patients received FOLFOX/XELOX, and two patients received FLOT.
In the HIPEC/IORT group, 3 patients underwent subtotal gastrectomy, and 30 patients underwent total gastrectomy, whereas in the surgery-only group, 6 patients underwent subtotal and 19 patients underwent total gastrectomy. All the patients in the HIPEC/IORT group underwent D2 lymphadenectomy compared with only 13 patients in the surgery-only group.
The surgical complications in the surgery-only group included wound infection in one patient, infected abdominal collection in two patients, central line infection in one patient, intestinal obstruction secondary to adhesions in one patient, iatrogenic splenic injury and postoperative bleeding in one patient, and postoperative sepsis and death in one patient. The complications in the HIPEC/IORT group included an infected abdominal collection in one patient, an infected abdominal collection in one patient, myocardial infarction in one patient, deep vein thrombosis in one patient, and leakage in one patient.
The median follow-up duration was 50.6 months (95% confidence interval [CI] 42.2–58.9 months) for the surgery-only group and 26.6 months (95% CI 13.1–40.0 months) for the HIPEC/IORT group. Locoregional recurrence occurred for five patients (20%) in the surgery-only group, and six (18.1%) patients in the HIPEC/IORT group. Peritoneal carcinomatosis occurred for six patients (24%) in the surgery-only group and three patients (9%) in the HIPEC/IORT group.
The median RFS duration was 24.8 months (95% CI 0.0–51.1 months) for the surgery-only group and 23.2 months (95% CI 6.5–39.9 months) for the HIPEC/IORT group (p = 0.88). The 5-year OS estimate was 58% for the surgery-only group and 69% for the HIPEC/IORT group (p = 0.77; Figs. 1, 2).
The RFS duration for the subgroup with pathologic T4 disease/node positivity was 10.6 months (95% CI 0.0–32.3 months) for the surgery-only group and 22.2 months (95% CI 14.8–29.6 months) for the HIPEC/IORT group (p = 0.826). The study end point for OS was not reached in either group for the subgroup that had high-risk features (T4/node-positive disease), with no significant difference between the groups (p = 0.614).
The univariate analysis of age, sex, and clinical and pathologic node status as factors affecting OS is summarized in Table 2. Only pathologic nodal status was found to have a significant effect on survival (p = 0.001).
Discussion
To our knowledge, this is the first study to examine the benefit of combining prophylactic HIPEC and IORT for the management of localized GC. Prophylactic HIPEC for localized GC has been studied extensively. Free cancer cells have been demonstrated in the peritoneal lavage of 14–27% of patients undergoing gastrectomy.19
The most common risk factors for peritoneal metastasis are serosal involvement and regional lymph node metastasis.19,20 It is believed that cells exfoliate from the lymphatic vessels during the lymphadenectomy procedure. The peritoneum is the most common site of recurrence after radical gastric surgery,21 with an incidence of approximately 40–50%.5,22 Once developed, PC has a poor prognosis, with an average median survival duration of 3–4 months.7
Several studies have demonstrated that prophylactic HIPEC after gastrectomy reduces the incidence of peritoneal recurrence. Most of these studies have come from the Asian-Pacific region and have been either randomized or nonrandomized comparative studies. Feingold et al.23 reported a systematic review of prophylactic HIPEC for patients with localized GC. Unfortunately, they excluded studies in which perioperative systemic chemotherapy was given, which currently is a standard procedure. The review identified 17 studies with 2029 patients. However, the studies were inappropriately performed, with up to 31% of some studies having patients with stage 4 disease. Additionally, 250 of the 1083 patients receiving prophylactic intraperitoneal chemotherapy received the treatment in the postoperative setting. A subgroup analysis of 10 randomized controlled studies reporting 5-year OS rates showed a significant difference in mortality between the intraperitoneal chemotherapy arm and the surgery-alone arm of the analysis (odds ratio [OR 0.65; 95% CI 0.52–0.81; p < 0.005).
A more recent meta-analysis of 22 trials involving 2097 patients was reported by Zhuang et al.24 Of these 22 trials, 12 were randomized. This meta-analysis included patients who received postoperative chemotherapy and excluded patients with peritoneal metastasis. The meta-analysis showed better 1-, 3- and 5-year OS rates in the HIPEC group than in the control group, with respective odds ratios of 5.10, 2.07, and 1.96.
A recent randomized phase 2 study of prophylactic HIPEC for a small, unselected group of 50 patients did not show benefits for the prophylactic HIPEC group compared with the control group. The HIPEC group had a 3-year relapse-free survival rate of 84.8% compared with 88% for the control group (p = 0.986).24 Notably, all the patients received adjuvant chemotherapy. In a multivariate analysis, pathologic T stage was the only independent risk factor for relapse-free survival (p = 0.012; hazard ratio [HR] 5.071).
The data on IORT are less solid. The reason behind local therapy lies in the fact that 50–90% of patients with localized disease experience locoregional recurrence after curative resection.25,26 Additionally, despite the efficacy of concurrent postoperative chemoradiotherapy demonstrated in the Intergroup 0116 trial, 19% of the patients in the investigational arm experienced local recurrence, and 65% experienced regional recurrence.27
A recent meta-analysis of patients with resectable gastric and esophageal cancers who received IORT (570 patients in the IORT group and 1011 in the control group) showed no significant difference in OS between the two groups (HR 0.91; 95% CI 0.73–1.13; p = 0.38).18 However, the patients with stage 2 or 3 cancer exhibited favorable effects, with improved locoregional control.
Another meta-analysis published in 2014 included eight studies that examined the benefit of IORT for resectable GC.17 In the four studies that included OS, the addition of IORT had no significant impact on OS. The pooled HR was 0.97 (95% CI 0.75–1.26; Z = 0.21; p = 0.837). In contrast, three studies reported subgroups of patients with stage 3 disease and showed a significantly improved OS with IORT (HR 0.60; 95% CI 0.40–0.89; Z = 2.53; p = 0.011).
To our knowledge, no other study has combined prophylactic HIPEC and IORT. The patient characteristics in our study were slightly unbalanced, with more favorable numbers for the HIPEC/IORT group (more intestinal histology [39.4% vs. 20%], a lower rate of pathologic T4 primary tumors [9% vs. 20%], and less lymph node involvement [39.4% vs. 56%]). On the other hand, the median age was in favor of the surgery-only group (54 vs. 64 years). The two groups showed no difference in OS or RFS, likely due to the unselected patient population, with only 9% of the HIPEC group having T4 disease and 39.4% having lymph node involvement. Interestingly, only three patients (9%) in the HIPEC/IORT group had peritoneal recurrence, and only six patients (18%) had locoregional recurrence. Locoregional recurrence occurred for five patients (20%) in the surgery-only group, similar to the HIPEC/IORT group. However, the peritoneal recurrence rate was slightly higher, with six patients experiencing peritoneal metastasis (24%).
Our subgroup analysis with pathologically confirmed T4 disease or node positivity (38 patients) confirmed our hypothesis. The RFS duration more than doubled in the HIPEC/IORT group compared with the surgery-only group (median of 22.2 months in the HIPEC/IORT group vs 10.6 months in the surgery-only group). However, this difference was not significant due to the small number of patients. No difference in OS was found. These data support the lack of benefits with prophylactic HIPEC and IORT in an unselected group of patients. The univariate analysis in our study showed that pathologic nodal status was the only prognostic factor of significance for survival.
Our study had several limitations. The greatest limitations were the small sample size, the study’s retrospective nature, and the nonrandomized comparison. In addition, the inclusion of all different stages of disease in the HIPEC/IORT group also limited observation of a difference between the two groups.
Conclusion
Our study showed that the addition of prophylactic HIPEC combined with IORT after curative resection of GC for an unselected group of patients did not improve RFS or OS. The benefits of combining both methods may be observed with better patient selection, including those with high-risk features for local and peritoneal recurrence. Further studies are required.
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71:7–33. https://doi.org/10.3322/caac.21654.
Pelcovits A, Almhanna K. Locoregional gastric cancer: a narrative review of multidisciplinary management. Ann Translat Med. 2020;8:1108–13. https://doi.org/10.21037/atm-20-3509.
Al-Batran SE, Homann N, Pauligk C, et al. Perioperative chemotherapy with fluorouracil plus leucovorin, oxaliplatin, and docetaxel versus fluorouracil or capecitabine plus cisplatin and epirubicin for locally advanced, resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4): a randomized, phase 2/3 trial. Lancet. 2019;393:1948–57. https://doi.org/10.1016/S0140-6736(18)32557-1.
Ji ZH, Peng KW, Yu Y, et al. Current status and future prospects of clinical trials on CRS + HIPEC for gastric cancer peritoneal metastases. Int J Hyperthermia. 2017;33:562–70. https://doi.org/10.1080/02656736.2017.1283065.
Reutovich MY, Krasko OV, Sukonko OG. Hyperthermic intraperitoneal chemotherapy in serosa-invasive gastric cancer patients. Eur J Surg Oncol. 2019;45:2405–11. https://doi.org/10.1016/j.ejso.2019.07.030.
Reutovich I, Krasko OV, Sukonko OG. Hyperthermic intraperitoneal chemotherapy in prevention of gastric cancer metachronous peritoneal metastases: a systematic review. J Gastrointest Oncol. 2021;12:S5–17. https://doi.org/10.21037/jgo-20-129.
Thomassen I, van Gestel YR, van Ramshorst B, et al. Peritoneal carcinomatosis of gastric origin: a population-based study on incidence, survival, and risk factors. Int J Cancer. 2014;134:622–8. https://doi.org/10.1002/ijc.28373.
Sugarbaker PH, Yu W, Yonemura Y. Gastrectomy, peritonectomy, and perioperative intraperitoneal chemotherapy: the evolution of treatment strategies for advanced gastric cancer. Semin Surg Oncol. 2003;21:233–48. https://doi.org/10.1002/ssu.10042.
Ji ZH, Peng KW, Li Y. Intraperitoneal free cancer cells in gastric cancer: pathology of peritoneal carcinomatosis and rationale for intraperitoneal chemotherapy/hyperthermic intraperitoneal chemotherapy in gastric cancer. Translat Gastroenterol Hepatol. 2016;1:69–80. https://doi.org/10.21037/tgh.2016.08.03.
González-Moreno S. Hyperthermic intraperitoneal chemotherapy: rationale and technique. World J Gastrointest Oncol. 2010;2:68. https://doi.org/10.4251/wjgo.v2.i2.68.
Sticca RP, Dach BW. Rationale for hyperthermia with intraoperative intraperitoneal chemotherapy agents. Surg Oncol Clin N Am. 2003;12:689–701. https://doi.org/10.1016/S1055-3207(03)00029-2.
Yonemura Y, de Aretxabala X, Fujimura T, et al. Intraoperative chemohyperthermic peritoneal perfusion as an adjuvant to gastric cancer: final results of a randomized controlled study. Hepatogastroenterology. 2001;48:1776–82.
Hamazoe R, Maeta M, Kaibara N. Intraperitoneal thermochemotherapy for prevention of peritoneal recurrence of gastric cancer: final results of a randomized controlled study. Cancer. 1994;73:2048–52. https://doi.org/10.1002/1097-0142(19940415)73:8%3c2048::AID-CNCR2820730806%3e3.0.CO;2-Q.
Kim JY, Bae HS. A controlled clinical study of serosa-invasive gastric carcinoma patients who underwent surgery plus intraperitoneal hyperthermo-chemo-perfusion (IHCP). Gastric Cancer. 2001;4:27–33. https://doi.org/10.1007/s101200100013.
Lee J, Lim DH, Kim S, et al. Phase III trial comparing capecitabine plus cisplatin versus capecitabine plus cisplatin with concurrent capecitabine radiotherapy in completely resected gastric cancer with D2 lymph node dissection: the ARTIST trial. J Clin Oncol. 2012;30:268–73. https://doi.org/10.1200/JCO.2011.39.1953.
Cats A, Jansen EPM, van Grieken NCT, et al. Chemotherapy versus chemoradiotherapy after surgery and preoperative chemotherapy for resectable gastric cancer (CRITICS): an international, open-label randomizedsed phase 3 trial. Lancet Oncol. 2018;19:616–28. https://doi.org/10.1016/S1470-2045(18)30132-3.
Yu WW, Guo YM, Zhang Q, Fu S. Benefits from adjuvant intraoperative radiotherapy treatment for gastric cancer: a meta-analysis. Mol Clin Oncol. 2015;3:185–9. https://doi.org/10.3892/mco.2014.444.
Gao P, Tsai C, Yang Y, et al. Intraoperative radiotherapy in gastric and esophageal cancer: meta-analysis of long-term outcomes and complications. Minerva Med. 2017;108:74–83. https://doi.org/10.23736/S0026-4806.16.04628-0.
Marutsuka T, Shimada S, Shiomori K, Hayashi N, Yagi Y, Yamane T. Mechanisms of peritoneal metastasis after operation for non-serosa-invasive gastric carcinoma: an ultrarapid detection system for intraperitoneal free cancer cells and a prophylactic strategy for peritoneal metastasis. https://pubmed.ncbi.nlm.nih.gov/12576435/.
Yul CW, Levison D, Dunn J, et al. Pathological prognostic factors in the second British Stomach Cancer Group trial of adjuvant therapy in resectable gastric cancer. Br J Cancer. 1995;71:1106–10.
Wu CW, Lo SS, Shen KH, et al. Incidence and factors associated with recurrence patterns after intended curative surgery for gastric cancer. World J Surg. 2003;27:153–8. https://doi.org/10.1007/s00268-002-6279-7.
Kang LY, Mok KT, Liu SI, et al. Intraoperative hyperthermic intraperitoneal chemotherapy as adjuvant chemotherapy for advanced gastric cancer patients with serosal invasion. J Chin Med Assoc. 2013;76:425–31. https://doi.org/10.1016/j.jcma.2013.04.004.
Feingold PL, Kwong MLM, Davis JL, Rudloff U. Adjuvant intraperitoneal chemotherapy for the treatment of gastric cancer at risk for peritoneal carcinomatosis: a systematic review. J Surg Oncol. 2017;115:192–201. https://doi.org/10.1002/jso.24476.
Zhuang X, He Y, Ma W. Prophylactic hyperthermic intraperitoneal chemotherapy may benefit the long-term survival of patients after radical gastric cancer surgery. Sci Rep. 2022. https://doi.org/10.1038/s41598-022-06417-y.
Landry J, Tepper JE, Wood WC, Moulton EO, Koerner F, Sullinger J. Patterns of failure following curative resection of gastric carcinoma. Int J Radiat Oncol Biol Phys. 1990;19(6):1357–62. https://doi.org/10.1016/0360-3016(90)90344-j.
Gunderson LL, Sosin H. Adenocarcinoma of the stomach: areas of failure in a re-operation series (second or symptomatic look) clinicopathologic correlation and implications for adjuvant therapy. Int J Radiat Oncol Biol Phys. 1982;8:1–11. https://doi.org/10.1016/0360-3016(82)90377-7.
Macdonald JS, Smalley SR, Benedetti J, et al. Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction. N Engl J Med. 2001;345:725–30. https://doi.org/10.1056/NEJMoa010187.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bazarbashi, S., Badran, A., Gad, A.M. et al. Combined Prophylactic Hyperthermic Intraperitoneal Chemotherapy and Intraoperative Radiotherapy for Localized Gastroesophageal Junction and Gastric Cancer: A Comparative Nonrandomized Study. Ann Surg Oncol 30, 426–432 (2023). https://doi.org/10.1245/s10434-022-12467-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12467-3