Abstract
Background
Current national guidelines do not include hyperthermic intraperitoneal chemoperfusion (HIPEC) as treatment for gastric cancer, and there are no completed clinical trials of cytoreduction, gastrectomy, and HIPEC from the US.
Methods
Patients with gastric adenocarcinoma and positive peritoneal cytology or carcinomatosis who had completed systemic chemotherapy and laparoscopic HIPEC underwent cytoreduction, gastrectomy, and HIPEC with 30 mg mitomycin C and 200 mg cisplatin. The primary endpoint was overall survival (OS), with a secondary endpoint of postoperative complications (NCT02891447).
Results
We enrolled 20 patients from September 2016 to March 2019. Six patients had positive cytology only and 14 had carcinomatosis. All patients were treated with systemic chemotherapy with a median of eight cycles (range 5–11 cycles) and at least one laparoscopic HIPEC. The median peritoneal carcinomatosis index at cytoreduction/gastrectomy/HIPEC was 2 (range 0–13). After surgery, the 90-day morbidity and mortality rates were 70% and 0%, respectively. Median length of hospital stay was 13 days (range 7–23 days); median follow-up was 33.5 months; median OS from the date of diagnosis of metastatic disease was 24.2 months; and median OS from the date of cytoreduction, gastrectomy, and HIPEC was 16.1 months. 1-, 2-, and 3-year OS rates from the diagnosis of metastatic disease were 90%, 50%, and 28%, respectively.
Conclusions
Survival rates for patients with gastric adenocarcinoma and peritoneal disease treated with cytoreduction, gastrectomy, and HIPEC are encouraging; our early results are similar to those of recent prospective registry studies. Multi-institutional and cooperative group trials should be supported to confirm survival and safety outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Patients with gastric cancer and peritoneal metastases are reported to have median survival rates of 6–15 months.1 Current National Comprehensive Cancer Network Guidelines recommend systemic chemotherapy only or best supportive care.2 Chemotherapy has been shown to improve survival in patients with peritoneal disease, but only at a median of 4 months.3
Peritoneal disease is clearly an important target for improving survival in metastatic gastric cancer. First, the peritoneum is the most common site of metastases when stage IV disease is identified at diagnosis.4 Second, carcinomatosis or positive cytology is identified in over 30% of patients with potentially resectable disease, based on imaging, who undergo staging laparoscopy.5 Third, peritoneal disease is identified in 11% of patients who progress during preoperative therapy.6 Fourth, the peritoneum is the most common site of recurrence after potentially curable resection.7
Hyperthermic intraperitoneal perfusion with chemotherapy (HIPEC), in combination with cytoreduction, is a treatment modality considered standard of care for some tumors metastatic to the peritoneum. However, there are only a few clinical trials of cytoreduction and HIPEC in gastric cancer, and no completed clinical trials from the US.8,9 Therefore, the purpose of this clinical trial is to determine the overall survival and safety of cytoreduction, gastrectomy, and hyperthermic intraperitoneal chemotherapy with mitomycin C and cisplatin in patients with stage IV gastric cancer limited to the peritoneum.
Methods
Patients
This phase II, single-arm trial (ClinicalTrials.gov identifier: NCT02891447) was conducted at MD Anderson Cancer Center between September 2016 and March 2019. Patients who were aged 18 years or older, with gastric or gastroesophageal adenocarcinoma diagnosed as stage IV based on histologic confirmation of positive peritoneal cytology or carcinomatosis, were eligible. Inclusion criteria included completion of systemic chemotherapy, with type and duration at the discretion of the treating medical oncologist. Patients were also required to undergo diagnostic laparoscopy with laparoscopic HIPEC prior to enrollment. Patients with distant metastases other than peritoneal or ovarian location were not included in this study. Additional inclusion criteria included Eastern Cooperative Oncology Group performance status ≤ 2, leukocyte count ≥ 3000/μL, absolute neutrophil count ≥ 1500/μL, platelet count ≥ 60,000/μL, serum creatinine ≤ 1.5 mg/dL, and aspartate transaminase and alanine transaminase levels ≤ 5 times the institutional upper limit of normal.
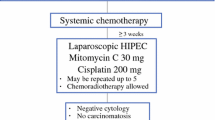
Treatment Design
The design of this single-center, investigator-initiated phase II trial is shown in Fig. 1. The type and duration of systemic chemotherapy was left to the discretion of the treating medical oncologist. Patients may have also received treatment with chemoradiation therapy. Duration and frequency of preoperative laparoscopic HIPEC procedures was left to the discretion of the treating surgical oncologist. A minimum of 4 weeks between laparoscopic HIPEC and cytoreduction, gastrectomy, and HIPEC was required. All participants provided written informed consent prior to surgery. The study was approved by the MD Anderson Institutional Review Board.
Cytoreduction, Gastrectomy, Hyperthermic Intraperitoneal Chemoperfusion
Cytoreduction of any suspicious lesions was performed, and subtotal or total gastrectomy was performed according to standard surgical principles. Once the cytoreduction and gastrectomy portion of the procedure were concluded, inflow and outflow catheters were placed. Crystalloid perfusate was circulated using an extracorporeal circulation device at a flow rate of 700–1500 mL/min. Once the heated perfusion was established per standard of care, mitomycin 30 mg and cisplatin 200 mg were instilled. A loading dose and 12-h continuous infusion of sodium thiosulfate was administered to limit the systemic toxicity of cisplatin. A loading dose of 7.5 g/m2 of sodium thiosulfate was diluted in 20 mL/kg of 0.9% normal saline up to 500 mL. The total loading dose was not to exceed 12.5 g. A maintenance infusion of sodium thiosulfate 25.56 g/m2 was then delivered by continuous infusion pump over approximately 12 h as per standard of care, until the infusion was complete. The target inflow temperature was 41–42 °C, with a target outflow of 39–40 °C. The perfusion was performed for 60 min and all perfusate was removed. Physical manipulation of the abdomen was maintained for 60 min to ensure even distribution of the perfusate. Postoperative hydration included maintenance intravenous fluids, and urine output was maintained and monitored as per standard of care.
Endpoints and Statistical Methods
The primary endpoint was OS, measured from the time of diagnosis of metastatic peritoneal disease. Secondary endpoints included OS from the date of cytoreduction, gastrectomy, and HIPEC, as well as complications. The probabilities of OS were estimated using the Kaplan–Meier method.10 The study was designed to improve OS from 11 to 15 months with the experimental therapy. A Bayesian interim futility monitoring rule was implemented such that the trial would be stopped early if, at any time during the study, there was a < 2% chance that OS was improved by at least 4 months. Death within 30 days was also monitored for early stopping of the trial. A recent series of patients undergoing this procedure reported a postoperative mortality rate of 5%.11 The stopping boundaries for the trial were if ≥ 2/10 or 3/20 patients died within 30 days from surgery. Ninety-day complications were also recorded and graded according to the Clavien–Dindo classification system.12 All statistical analyses were performed using Splus software (TIBCO Software Inc., Palo Alto, CA, USA).
Results
Patient Characteristics and Treatments
Twenty patients were treated on the trial (see Table 1 for a summary of the baseline characteristics). The median age was 58 years (range 20–75) and six patients were aged 65 years or older. Most tumors were poorly differentiated (85%) with signet ring cell histology (65%). Tumor location was cardia/body in 3 patients, antrum in 6 patients, and overlapping or total involvement in 11 patients. Linitis plastica was identified in 35% of patients. Peritoneal carcinomatosis was present in 70% of patients, while 30% of patients had positive cytology only. Seventeen patients received 5-fluorouracil and oxaliplatin (one with trastuzumab), while three patients received triplet therapy (doxorubicin/cisplatin/5-fluorouracil, epirubicin/oxaliplatin/xeloda, and docetaxel/carboplatin/5-fluorouracil). Two patients received second-line therapy prior to enrollment (ramicurimab/paclitaxel and 5-fluorouracil/irinotecan). Most patients (75%) were treated with 8–10 cycles of chemotherapy. Fifteen patients had a single laparoscopic HIPEC and five patients had two laparoscopic HIPECs prior to enrollment. Nine patients underwent total gastrectomy and 11 patients underwent subtotal gastrectomy. The median peritoneal carcinomatosis index at cytoreduction, gastrectomy, and HIPEC was 2 (range 0–13). Resection of other organs, beyond peritoneal cytoreduction, was required in nine patients, which included transverse colon in one patient, transverse mesocolon in three patients, partial or complete splenectomy in two patients, and bilateral salpingoophorectomy in four patients (once in combination with transverse mesocolon). Chest tube placement was performed in two patients at the time of surgery.
Surgical Pathology, Outcomes, and Complications
American Joint Commission on Cancer T-stage classification included ypT1b (n = 2), ypT2 (n = 1), ypT3 (n = 6), and ypT4 (n = 11).13 N-stage classification included ypN0 (n = 6), ypN1 (n = 6), ypN2 (n = 2), and ypN3 (n = 6). The median number of examined nodes was 31. An R1 margin was present in three patients.
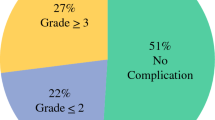
The median length of stay for patients undergoing surgery was 13 days (range 7–23), with readmission occurring in 50% of patients. Twenty-two surgical complications occurred in 14 patients (70%), and seven grade III/IV complications occurred in five patients (25%), with one patient experiencing three grade III complications representing multiple separate percutaneous drainage procedures. Four patients who had undergone subtotal gastrectomy experienced grade III/IV complications, while only one total gastrectomy patient experienced a grade III complication. Fifteen grade I/II complications occurred in 10 patients (50%), with three patients experiencing two grade II complications and one patient experiencing three grade II complications. All complications within 90 days, graded according to an accepted classification system, are outlined in Table 2. Isolated grade I complications were infrequent and included a single patient with severe nausea requiring antiemetic treatment. Grade II complications were the most common and included pulmonary embolization (n = 1), acute kidney injury requiring medical management (n = 1), cellulitis requiring antibiotics (n = 1), gastrointestinal leakage controlled with a drain placed at initial operation (n = 2), clostridium difficile infection (n = 2), inability to tolerate tube feeds requiring total parenteral nutrition (n = 4), and blood transfusion (n = 3). There were six grade III complications of anastomotic leakage or symptomatic abdominal fluid collection requiring a percutaneous drain. One patient had a grade IV complication with abdominal compartment syndrome and multi-organ system failure, also requiring reoperation. There were no grade V complications (mortality) within 90 days of surgery.
Overall Survival
The median follow-up duration was 33.5 months (95% confidence interval [CI] 30.3 months–not estimable); the median OS from the date of diagnosis of metastatic disease was 22.1 months; median OS from the date of first laparoscopic HIPEC was 17.4 months; and median OS from the date of cytoreduction, gastrectomy, and HIPEC was 16.1 months. 1-, 2, and 3-year OS rates from the diagnosis of metastatic disease were 90%, 50%, and 28%, respectively (Fig. 2), and 1-, 2-, and 3-year OS rates from the date of cytoreduction, gastrectomy, and HIPEC were 60%, 25%, and 25%, respectively (Fig. 3). The peritoneum was identified as the most common site of recurrence in 10 patients, with distant lymph nodes (n = 1), brain (n = 1), liver (n = 1), lung (n = 1), and undocumented (n = 2) accounting for the remaining sites. There are currently four patients alive without evidence of disease, at a range of 32–49 months after diagnosis of metastatic disease: three patients with positive cytology who converted to negative, and one patient with carcinomatosis that macroscopically resolved after systemic chemotherapy.
Discussion
In this single-arm, phase II trial, we enrolled patients with gastric adenocarcinoma metastatic to the peritoneum who had completed systemic chemotherapy and at least one laparoscopic HIPEC. This selective and multidisciplinary approach to the investigation of HIPEC in metastatic gastric cancer resulted in OS rates that were favorable when compared with reports of outcomes for patients with carcinomatosis or positive cytology.1
There are multiple clinical trials and cohort studies supporting the investigation of HIPEC in gastric adenocarcinoma. Initial work from Japan and China evaluated HIPEC as adjuvant treatment for patients at high risk of peritoneal disease. These studies have been compiled multiple times in reviews that document a significant improvement in OS with adjuvant HIPEC; 14,15,16,–17 however, these studies are now approximately 20 years old and adjuvant HIPEC is not a standard of care in these or other countries. Currently in Japan, most research is focused on non-heated intraperitoneal paclitaxel for stage IV disease, in combination with systemic therapy.18 The role of adjuvant HIPEC in Western populations will be best addressed by the ongoing GASTRICHIP trial.19
There are multiple retrospective cohort studies that demonstrate promising survival rates in select patients treated with HIPEC with established carcinomatosis.20 A recent French registry retrospective report of prospective data, the CYTOCHIP study, compared patients undergoing cytoreduction and gastrectomy alone with patients undergoing cytoreduction, gastrectomy, and HIPEC.11 The patients in this study who received HIPEC had improved median OS rates compared with cytoreduction alone and, most notably, a 5-year OS rate of 20%. The authors acknowledge the highly selective nature of the 25-year study, with, on average, less than one patient treated per center per year.11 Ongoing randomized clinical trials that will continue to evaluate the benefit of HIPEC include the GASTRIPEC trial, comparing gastrectomy and cytoreduction with gastrectomy, cytoreduction, and HIPEC in patients who have completed systemic chemotherapy.21 Although this study was terminated early due to low accrual, which is partly attributed to the high progressive disease rate during the preoperative systemic chemotherapy phase, it should provide some comparative data in the context of a randomized controlled trial. The PERISCOPE II trial is a recently activated randomized trial that will compare cytoreduction, gastrectomy, and HIPEC with standard of care systemic chemotherapy, addressing the most prominent question in the role of HIPEC in patients with gastric cancer and peritoneal disease.22
The current trial is the culmination of a peritoneal program reflecting our concerns over the risks associated with combining gastrectomy, cytoreduction, and HIPEC. Our initial investigation in HIPEC was a phase II trial of repeated laparoscopic HIPEC without cytoreduction or gastrectomy, after completion of systemic chemotherapy, to attempt to clear the peritoneum of disease.23 Only in the setting of no visible carcinomatosis and negative peritoneal washings were patients offered gastrectomy alone, without HIPEC. This trial demonstrated promising survival rates and low morbidity, but many patients had persistent peritoneal disease that did not respond to this approach.
The results reported here represent a more aggressive approach of combining cytoreduction, gastrectomy, and HIPEC, and appear to improve upon our previous phase II trial of repeated laparoscopic HIPEC. However, the importance of systemic chemotherapy is clearly evident in that all long-term survivors had had an excellent response with either conversion of cytology or macroscopic resolution of carcinomatosis. Surgery, and HIPEC, in the setting of peritoneal disease should always be approached in a multidisciplinary fashion, and appears to work best as an adjuvant procedure after maximal effect of chemotherapy.24 These findings also provide equipoise for future studies with a comparative arm including either resection alone or standard of care systemic therapy. As long-term survivors are identified after extended chemotherapy with locoregional treatment of either chemoradiotherapy or surgery without HIPEC, multi-institutional randomized trials will be critically important in determining a causative effect between HIPEC and OS.25,26 There is also increasing evidence that combination intraperitoneal and systemic paclitaxel may convert peritoneal disease to an undetectable level, perhaps then allowing for more effective surgical interventions.18,27,28 These studies, primarily from Japan, have provided the rationale for a current phase I trial of intraperitoneal paclitaxel at our institution (NCT04220827).29
The strength of this trial is that it provides further evidence regarding the safety outcomes related to cytoreduction, gastrectomy, and HIPEC, while supporting the feasibility of a cooperative group trial. National Surgical Quality Improvement Program data reporting 30-day complications of gastrectomy for cancer note a serious morbidity rate of 24%, mortality rate of 4%, and reoperation rate of 8%, which is similar to our 90-day grade III/IV complication rate of 25% without mortality.30 There are several limitations that require discussion, most prominently the selection bias of accruing patients after the completion of systemic therapy. We did not define the systemic therapy administered prior to enrollment, as patients are often started on chemotherapy prior to referral. Our institutional preference is treatment with 5-fluorouracil and oxaliplatin for eight cycles. The small sample size and lack of correlative studies also prevent us from identifying predictors of response to HIPEC, other than stressing the importance of a response to chemotherapy. Future work will benefit greatly from translational studies identifying biomarkers of response and the most beneficial chemotherapeutic agents.
Conclusion
Survival rates for patients with gastric adenocarcinoma and peritoneal disease treated with cytoreduction, gastrectomy, and HIPEC are encouraging; our early results are similar to those of recent prospective registry studies. There are ongoing efforts within the cooperative group system to develop randomized trials to confirm survival and safety outcomes, which should be supported.
References
Badgwell B, Cormier JN, Krishnan S, et al. Does neoadjuvant treatment for gastric cancer patients with positive peritoneal cytology at staging laparoscopy improve survival? Ann Surg Oncol. 2008;15(10):2684–2691.
National Comprehensive Cancer Network Guidelines Version 4.2019, Gastric Cancer. Available at: www.nccn.org. Accessed 31 Jan 2020.
Thomassen I, Bernards N, van Gestel YR, et al. Chemotherapy as palliative treatment for peritoneal carcinomatosis of gastric origin. Acta Oncol. 2014;53(3):429–432.
Badgwell B, Das P, Ajani J. Treatment of localized gastric and gastroesophageal adenocarcinoma: the role of accurate staging and preoperative therapy. J Hematol Oncol. 2017;10(1):149.
Ikoma N, Blum M, Chiang YJ, et al. Yield of staging laparoscopy and lavage cytology for radiologically occult peritoneal carcinomatosis of gastric cancer. Ann Surg Oncol. 2016;23(13):4332–4337.
Thiels CA, Ikoma N, Fournier K, et al. Repeat staging laparoscopy for gastric cancer after preoperative therapy. J Surg Oncol. 2018;118(1):61–7.
Ikoma N, Chen HC, Wang X, et al. Patterns of initial recurrence in gastric adenocarcinoma in the era of preoperative therapy. Ann Surg Oncol. 2017;24(9):2679–2687.
Yang XJ, Huang CQ, Suo T, et al. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy improves survival of patients with peritoneal carcinomatosis from gastric cancer: final results of a phase III randomized clinical trial. Ann Surg Oncol. 2011;18(6):1575–81.
Rudloff U, Langan RC, Mullinax JE, et al. Impact of maximal cytoreductive surgery plus regional heated intraperitoneal chemotherapy (HIPEC) on outcome of patients with peritoneal carcinomatosis of gastric origin: results of the GYMSSA trial. J Surg Oncol. 2014;110(3):275–284.
Kaplan EMP. Nonparametric estimator from incomplete observations. J Am Stat Assoc. 1958;53:457–481.
Bonnot PE, Piessen G, Kepenekian V, et al. Cytoreductive surgery with or without hyperthermic intraperitoneal chemotherapy for gastric cancer with peritoneal metastases (CYTO-CHIP study): a propensity score analysis. J Clin Oncol. 2019;37(23):2028–2040.
Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–196.
AJCC (2017) Stomach cancer In: Ajani JA, In H, Sano T (Eds.) Cancer staging manual 8. Springer, New York, pp 203–220.
Yan TD, Black D, Sugarbaker PH, et al. A systematic review and meta-analysis of the randomized controlled trials on adjuvant intraperitoneal chemotherapy for resectable gastric cancer. Ann Surg Oncol. 2007;14(10):2702–13.
Coccolini F, Cotte E, Glehen O, et al. Intraperitoneal chemotherapy in advanced gastric cancer. Meta-analysis of randomized trials. Eur J Surg Oncol. 2014;40(1):12–26.
Sun J, Song Y, Wang Z, et al. Benefits of hyperthermic intraperitoneal chemotherapy for patients with serosal invasion in gastric cancer: a meta-analysis of the randomized controlled trials. BMC Cancer. 2012;12:526.
Brenkman HJF, Paeva M, van Hillegersberg R, Ruurda JP, Haj Mohammad N. Prophylactic hyperthermic intraperitoneal chemotherapy (HIPEC) for gastric cancer: a systematic review. J Clin Med. 2019;8(10):1685.
Ishigami H, Fujiwara Y, Fukushima R, et al. Phase III trial comparing intraperitoneal and intravenous Paclitaxel Plus S-1 Versus Cisplatin Plus S-1 in patients with gastric cancer with peritoneal metastasis: PHOENIX-GC Trial. J Clin Oncol. 2018;36(19):1922–29.
Glehen O, Passot G, Villeneuve L, et al. GASTRICHIP: D2 resection and hyperthermic intraperitoneal chemotherapy in locally advanced gastric carcinoma: a randomized and multicenter phase III study. BMC cancer. 2014;14:183.
Glehen O, Gilly FN, Arvieux C, et al. Peritoneal carcinomatosis from gastric cancer: a multi-institutional study of 159 patients treated by cytoreductive surgery combined with perioperative intraperitoneal chemotherapy. Ann Surg Oncol. 2010;17(9):2370–77.
Brandl A, Pachmayr E, Gul-Klein S, Alberto M, Thuss-Patience P, Rau B. Surgical treatment of peritoneal metastases of gastric cancer. Chirurg. 2018;89(9):669–77.
Koemans WJ, van der Kaaij RT, Boot H, et al. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy versus palliative systemic chemotherapy in stomach cancer patients with peritoneal dissemination, the study protocol of a multicentre randomised controlled trial (PERISCOPE II). BMC Cancer. 2019;19(1):420.
Badgwell B, Blum M, Das P, et al. Phase II trial of laparoscopic hyperthermic intraperitoneal chemoperfusion for peritoneal carcinomatosis or positive peritoneal cytology in patients with gastric adenocarcinoma. Ann Surg Oncol. 2017;24(11):3338–44.
Newhook TE, Agnes A, Blum M, et al. Laparoscopic hyperthermic intraperitoneal chemotherapy is safe for patients with peritoneal metastases from gastric cancer and may lead to gastrectomy. Ann Surg Oncol. 2019;26(5):1394–400.
Badgwell B, Roy-Chowdhuri S, Chiang YJ, et al. Long-term survival in patients with metastatic gastric and gastroesophageal cancer treated with surgery. J Surg Oncol. 2015;111(7):875–81.
Mizrak Kaya D, Wang X, Harada K, et al. 101 Long-term survivors who had metastatic gastroesophageal cancer and received local consolidative therapy. Oncology. 2017;93(4):243–48.
Ishigami H, Yamaguchi H, Yamashita H, Asakage M, Kitayama J. Surgery after intraperitoneal and systemic chemotherapy for gastric cancer with peritoneal metastasis or positive peritoneal cytology findings. Gastric cancer. 2017;20 (Suppl 1):128–34.
Ishigami S, Natsugoe S, Nakajo A, et al. Salvage gastrectomy following a combination of biweekly paclitaxel and S-1 for stage IV gastric cancer. J Gastrointestinal. 2008;12(8):1370–5.
MD Anderson Cancer Center. Paclitaxel for the treatment of gastric or gastroeosphageal cancer. ClinicalTrials.gov identifier NCT04220827. Available at: https://clinicaltrials.gov. Accessed 19 May 2020.
Papenfuss WA, Kukar M, Oxenberg J, et al. Morbidity and mortality associated with gastrectomy for gastric cancer. Ann Surg Oncol. 2014;21(9):3008–14.
Acknowledgment
This trial was supported by the Holy Clegg Gastric Cancer Research Fund, the No Stomach for Cancer Award for Gastric Cancer Research, and the University Cancer Foundation via the Institutional Research Grant program at the University of Texas MD Anderson Cancer Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Prajnan Das has received honorarium from Adlai Nortye USA Inc.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Badgwell, B., Ikoma, N., Murphy, M.B. et al. A Phase II Trial of Cytoreduction, Gastrectomy, and Hyperthermic Intraperitoneal Perfusion with Chemotherapy for Patients with Gastric Cancer and Carcinomatosis or Positive Cytology. Ann Surg Oncol 28, 258–264 (2021). https://doi.org/10.1245/s10434-020-08739-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08739-5