Abstract
Clinical practice guidelines in oncology have typically focused on workup, disease staging, and medical management. Although recommendations for surgical care have been included in these guidelines, those recommendations have primarily addressed issues such as the role of surgery or the incorporation of surgery into multidisciplinary treatment strategies, not the technical performance of the operative procedures themselves. Therefore, the quality of surgery, the only component of multidisciplinary cancer care proven to be potentially curative, has been poorly controlled. During the past decade, the American College of Surgeons (ACS) cancer programs have attempted to fill this gap by developing “operative standards” for cancer surgery. This report discusses the history of the operative standards, highlights evidence to demonstrate their efficacy, and describes the activities of the ACS Commission on Cancer and Cancer Surgery Standards Program toward disseminating and implementing them.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The Institute of Medicine defines clinical practice guidelines as “statements that include recommendations, intended to optimize patient care, that are informed by a systematic review of evidence and an assessment of the benefits and harms of alternative care options.”1 In the field of oncology, several practice guidelines and critical pathways are used to inform the care of patients with cancer. Evidence exists to show that compliance with these guidelines improves metrics including length of stay, adverse events, financial outcomes, and in certain cases, long-term oncologic outcomes including disease-free and overall survival.2
Clinical practice guidelines such as those published by the American Society of Clinical Oncology3 and the National Comprehensive Cancer Network4 have typically focused on workup, disease staging, and medical management. Although recommendations for surgical care have been included in these guidelines, those recommendations have primarily addressed issues such as the role of surgery or the incorporation of surgery into multidisciplinary treatment strategies, not the technical performance of the operative procedures themselves. Indeed, that surgical operations are performed identically by all surgeons (similar procedure names and coding) might appear to have been assumed by some, especially non-surgeons, although the way operations are performed is highly variable. In a study of patients who had undergone pulmonary resection for non-small cell lung cancer, for example, fewer than half of the operations included an adequate lymphadenectomy of the mediastinal and hilar lymph nodes.5
Technical standards that do exist have historically been represented largely by outcome metrics, such as the number of nodes harvested during colon cancer resection.6,7,8 In contrast, process standards informing the performance of surgical procedures have been relatively few. Historically, the quality of surgery, the only component of multidisciplinary cancer care proven to be potentially curative, has been poorly controlled.
During the past decade, the American College of Surgeons (ACS) cancer programs have attempted to fill this gap by developing “operative” or “technical” standards for cancer surgery. In this review, we discuss the history of these standards, highlight evidence to suggest their efficacy, and describe the activities of the ACS Commission on Cancer (ACS-CoC) and Cancer Surgery Standards Program (ACS-CSSP) geared toward disseminating and implementing them.
Background and Development of Operative Standards for Cancer Surgery Manuals
The operative standards developed by the ACS were first published through a collaboration between the ACS-Cancer Research Program (ACS-CRP) and the Alliance for Clinical Trials in Oncology in 2015. The first volume of Operative Standards for Cancer Surgery aimed to explicitly educate surgeons and surgical trainees, to provide quality controls within the context of clinical research protocols, to identify and target knowledge gaps for further study, and to enhance the quality of surgical oncology as practiced in the United States.9
In this initial publication, which focused on surgery for cancers of the breast, pancreas, colon, and lung, “critical elements” for various operative procedures were defined as specific technical steps perceived to have a direct impact on long-term oncologic outcomes such as overall survival and quality of life. Critical elements (e.g., lymphadenectomy at pancreatoduodectomy or high vascular ligation at colectomy) were separated from other technical aspects of surgery that do not as clearly influence these outcomes (e.g., access incision, mobilization) and/or that do not occur from skin incision to skin closure (e.g., disease staging or use of perioperative antibiotics). Recommendations for the performance of each critical element were generated by diverse teams of disease-site experts following literature reviews. The quality of each recommendation was graded per the American College of Physicians guideline grading system based on the strength of the recommendation and the quality of the evidence supporting it.10 A second manual describing the operative care of patients with esophageal, rectal, gastric, thyroid and skin (melanoma) cancer was published in 2019,11 and a third volume that includes adrenal, hepatobiliary, and urothelial cancers; neuroendocrine tumors; sarcoma; and peritoneal malignancies is nearing publication.
Significance and Impact of Operative Standards on Patient Care
Significant variability exists in the way these critical elements are performed nationwide. A systematic review examining the role that periadventitial dissection of the superior mesenteric artery plays in pancreatoduodenectomy evaluated 43 articles addressing the influence of this critical technical element on margin status and survival. Although 33 of these studies concluded that a positive resection margin was associated with decreased overall survival, the operative technique used to manage the most commonly positive margin was addressed in only 11 of the studies.12 Another study of operative reports on patients enrolled in a trial of adjuvant therapy after pancreatoduodenectomy found that skeletonization of the right lateral aspect of the superior mesenteric artery had been performed in only 25% of cases.13
Data exist to suggest that widespread adoption of operative standards may reduce this variability and improve oncologic outcomes. In a study of more than 500,000 patients in the National Cancer Database who had undergone surgery for breast cancer between 2004 and 2015, only about 75% of the patients had care adhering to oncologic standards that included some of the ACS operative standards. The patients whose care met the standards had 5- and 10-year overall survival rates significantly longer than those of patients whose care did not.14 Similar findings also exist to inform the care of patients with other malignancies, including malignancies of the stomach,15 colon16 and lung.5,17 It is important to recognize that adherence to technical standards may improve outcomes, at least in part, by improving precision in cancer staging and can lead to “upstaging” of patients, thereby informing the role and delivery of postoperative systemic and adjuvant therapies.18
Integration of Operative Standards into ACS-CoC Accreditation Standards
In 2020, the ACS-CoC published the latest edition of its accreditation manual, Optimal Resources for Cancer Care.19 For the first time, the accreditation manual included technical standards for cancer surgery. Surgeons and pathologists in ACS-CoC-accredited facilities currently are required to adhere to and document compliance with six new evidence-based best practices for operations performed for breast cancer, colon cancer, lung cancer, melanoma, and rectal cancer (Table 1). Each of these standards was derived from critical elements described in the Operative Standards for Cancer Surgery manuals.
Rationale: Sentinel Node Biopsy for Breast Cancer (Standard 5.3)
Sentinel nodes are defined as nodes having uptake of radioactive tracer and/or colored dye previously injected into the affected breast nodes to which a colored lymphatic travels or to dominant lymph nodes palpable or otherwise suspicious on intraoperative evaluation. Nodes with radioactive counts at least 10% that of the most radioactive node also are considered sentinel nodes. All sentinel nodes must be identified, removed, and subjected to histopathologic analysis to ensure that sentinel lymph node mapping and sentinel lymphadenectomy provide accurate staging information.20
Sentinel nodes are typically found within level 1 or 2 of the axilla. The median number of nodes removed at a well-performed sentinel lymphadenectomy is two or three. The risk for a false-negative biopsy increases when fewer nodes are removed.21,22 Although the procedure can be performed using either a radioactive tracer (e.g., technetium sulfur colloid) or colored dye, most surgeons use both.23 In such cases, some nodes may be identified using only one of the tracers, and use of both tracers increases the likelihood that all sentinel nodes will be identified.
Rationale: Axillary Lymph Node Dissection for Breast Cancer (Standard 5.4)
Axillary lymph node dissection provides important staging information used to inform treatment decisions, and it also may improve locoregional control in some settings. A properly performed axillary lymph node dissection removes all levels 1 and 2 lymph nodes that lie within an anatomic triangle defined by the axillary vein, chest wall, and latissimus dorsi muscle while preserving the important long thoracic nerve, thoracodorsal nerve, and branches of the intercostobrachial nerves. Most often, axillary metastases are identified in level 1 nodes. Metastases that occur in level 2 or 3 nodes in the absence of level 1 nodes are rare and found in level 3 nodes in less than 1% of patients.24 Furthermore, no survival advantage is associated with levels 1, 2, and 3 lymphadenectomies versus a more limited level 1 or 2 dissection.25,26 Thus, level 3 nodes generally need not be removed unless clinically suspicious.
The long thoracic nerve innervates the serratus anterior muscle, and transection of the nerve can lead to pain, weakness, limited shoulder elevation, and scapular winging. The thoracodorsal nerve innervates the latissimus dorsi muscle, and transection results in weakness or atrophy of that muscle.
Rationale: Wide Local Excision for Primary Cutaneous Melanoma (Standard 5.5)
The recommended clinical margin width for wide local excision of melanoma is based on the original Breslow thickness of the primary tumor.27 The margin should be measured circumferentially at the level of the skin from either residual gross tumor or the previous biopsy scar. For invasive melanomas, the wide local excision width should be 1 cm for lesions less than 1 mm thick, 1 to 2 cm for lesions 1 to 2 mm thick, and 2 cm for lesions more than 2 mm thick.28,29,30,31 In all cases, the depth of resection should include the skin and all underlying subcutaneous tissue to the level of the underlying fascial plane. When performed for melanoma in situ, the width of wide local excisions should be at least 5 mm, and the depth need include only the skin and superficial subcutaneous fat.
Rationale: Colon Resection (Standard 5.6)
For patients with colon cancer, proper resection of the tumor-bearing bowel segment should include complete lymphadenectomy. Lymphatics within the mesocolon parallel the arterial supply. The lymphatic drainage of the right and proximal transverse colon occurs through lymphatics along the branches of the superior mesenteric artery. The lymphatic drainage of the distal transverse, descending, and distal colon occurs through lymphatics along the course of the inferior mesenteric artery.
In general, lymphatic drainage is continuous and sequential, from the pericolonic nodes to the intermediate nodes along the right, middle, left, and sigmoid colic arteries, then to the nodes at the origins of the superior and inferior mesenteric arteries. Proximal vascular ligation with en bloc lymphadenectomy ensures complete resection of the associated lymph nodes for pathologic evaluation.
Rationale: Total Mesorectal Excision (Standard 5.7)
Total mesorectal excision (TME) of rectal cancer leverages existing tissue planes to perform a complete resection of the tumor and the associated lymph nodes. By maintaining the intact fascia propria of the rectum and operating in the space between the mesorectum and the endopelvic fascia, surgeons can achieve R0 resection margins, preserve key neurovascular structures, reduce locoregional recurrence, and prolong patient survival.32
Importantly, a negative microscopic margin alone is not enough to maximize outcomes. The quality of the TME specimen also is important. The quality of TME is assessed by the pathologist after resection using the most disrupted part of the resected specimen. The TME is classified as complete when there is an intact, bulky mesorectum with a smooth surface, only minor irregularities, and no coning toward the distal specimen. Near-complete specimens are those that have an irregular mesorectal surface and defects larger than 5 mm. Incomplete specimens are those that have defects down to the muscularis propria and little to no bulk of the mesorectum.
A complete mesorectum after TME is associated with lower rates of local and distant cancer recurrence compared with an incomplete mesorectum.33 Although surgeons should strive to perform a complete TME, a near-complete TME yields similar rates of local recurrence and survival as a complete TME.
Rationale: Pulmonary Resection (Standard 5.8)
For patients with lung cancer, prognosis and management depend on accurate pathologic nodal staging. However, nodal staging is highly susceptible to variability in the techniques used to remove tumors and evaluate them pathologically.34 Accurate pathologic lymph node staging requires appropriate dissection of hilar and mediastinal lymph node stations by the surgeon, transfer of these nodes to the pathologist, and appropriate processing and evaluation.35 The current consensus is that pulmonary resections should be accompanied by examination of hilar and intrapulmonary lymph nodes as well as examination of three or more mediastinal lymph node stations. Data show that patients whose operations conform to these standards live longer than those whose operations do not.5
Implementation of ACS-CoC Standards 5.3–5.8
Institutions implementing ACS-CoC Standards 5.3–5.8 are using a phased approach that began in 2020. Because these standards apply to any operation conducted with curative intent, the operating surgeon should preoperatively assign the intent of each operation and clearly document it postoperatively based on preoperative evaluation and intraoperative management.
Curative operations generally include complete resection of the primary tumor and nodal evaluation for therapeutic or staging purposes. It is acknowledged that the word “curative” is at least to some degree ambiguous and subjective. But the goal is that the specific techniques the surgeon uses to perform a cancer operation are logically aligned with the intent the surgeon has in performing it. If the surgeon performs an operation with the purported goal of curing the patient of cancer, that operation should then be performed in accordance with the operative standards. Any operation in which a surgeon deliberately deviates from these standards, as may occur in the setting of patient frailty or comorbidity, for example, would not be considered curative. Intended deviations should be reported as part of the narrative.
According to ACS-CoC Standards 5.7 and 5.8, pathology reports are required to include specific elements in synoptic format for the operations performed, starting 1 January 2021. The elements required for Standards 5.7 and 5.8 also are required by the College of American Pathology. Starting in 2022, ACS-CoC site visits will evaluate documentation from 2021 to determine whether the site meets the specified compliance criteria for Standards 5.7 and 5.8, with an expected compliance rate of 70% for 2021. The mandatory compliance rate increases to 80% for cases starting 1 January 2022.36
Standards 5.3–5.6 require operative reports to include specific elements in synoptic format for operations starting 1 January 2023, with an expected compliance rate of 70% in 2023. Operative reports will be assessed for compliance with these standards, starting with site visits taking place in 2024. In 2022, ACS-CoC-accredited cancer programs must document their plan for how they will achieve compliance with Standards 5.3 to 5.6, including the mechanism the facility will use to capture the required data elements in a synoptic format, how they are educating surgeons about these requirements, and when they are going to start requiring surgeons to use the synoptic reporting to ensure that the relevant breast, colon, and melanoma procedures performed in 2023 are documented using synoptic format.
It is important to note that compliance with ACS-CoC Standards 5.3 to 5.8 will be assessed on the basis of an attestation made by the operating surgeon, not on the basis of videos, operative photographs, or other clinical or pathologic “evidence.” It is thus possible that the operative report may not accurately or completely reflect all intraoperative events. Although this represents, to some degree, a limitation in implementation, it should be emphasized to all surgeons and programs that the goal of these standards is not to punish, but instead to educate and encourage process improvement.
Site reviewers will review seven charts for each operative standard. If a program has fewer than seven patients who meet the criteria for a specific standard, then all patient charts meeting the inclusion criteria will be reviewed by the site reviewer.
Educational Resources
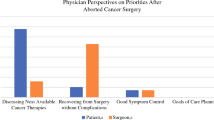
The mission of ACS-CSSP is to improve the quality of surgical care provided to people with cancer. One important aim of this program is to support ACS-CoC-accredited cancer programs in implementation and adherence to ACS-CoC Standards 5.3–5.8. To this end, ACS-CSSP members have disseminated surveys to measure surgeon awareness and knowledge of the operative standards, and have developed educational resources to close identified gaps.37
In 2020, for example, a survey was sent to contacts at CoC-accredited sites to understand site and surgeon preparedness for implementation of ACS-CoC Standards 5.3 to 5.8. The survey results suggested that existing practices would translate to a 50–60% compliance rate for the operative standards (Vreeland T., unpublished data). It was unclear whether gaps were related to the technical or the documentation component. To address the lack of clarity around the standards, the ACS-CSSP was launched to promote the purpose, value, and supporting evidence for the operative standards, and to help implement them.
In 2021, another survey was sent to CoC-accredited cancer programs to understand surgeon knowledge and perception of the standards. The results from the survey showed that surgeons could demonstrate a thorough knowledge of the technical aspects of cancer surgery underlying the ACS-CoC operative standards, but that they were relatively unaware of the details of the standards themselves. Most surgeons (75%), however, stated that adhering to the standards would have “little” or “no” effect on their current practice (Vreeland T., unpublished data).
The ACS-CSSP has focused development of educational resources on the technical aspects and documentation details for the operative standards, including webinars, guidelines documents, toolkits, videos, and visual abstracts.36 (Figs. 1 and 2). These resources have been and will continue to be promoted through ACS channels and through external societies, with the goal of reaching general surgeons in practice across the country as well as trainees. Together with the ACS-CRP, the ACS-CSSP also is developing new operative standards for incorporation into future ACS-CoC accreditation manuals.
Implementation Resources
Because synoptic reporting is an important part of tracking compliance with the standards, the ACS-CSSP has developed comprehensive synoptic operative reports and other resources to support integration into the electronic health record. Comprehensive synoptic operative reports for breast cancer, colon cancer, and melanoma surgery are complete and available, and reports for thyroid, pancreas, and lung operations are in development. The companion to this article, “Technical Standards for Cancer Surgery: Improving Patient Care through Synoptic Operative Reporting,”38 discusses the background and benefits of synoptic reporting and its incorporation into the ACS-CoC Standards.
The Accreditation Committee of the ACS-CoC evaluates and monitors the value of its standards over time. Because implementation of College of American Pathology synoptic reporting tools during the past decade was successful,39 we anticipate synoptic operative reporting will likewise be well-accepted over time. The ACS-CSSP will work with the ACS-CoC and other cancer programs to evaluate the utility of synoptic reporting and to determine whether it should be more broadly adapted, limited to specific areas of cancer surgery, or discontinued. This will be a continuous process of evaluation across the cancer programs as the field changes. If the benefits of synoptic operative reporting are strong, beginning in 2026, the ACS-CoC will implement expanded requirements for synoptic operative reporting with the goal of transitioning all institutions to full synoptic operative reports for all cancer-related operations.
Summary
Technical standards to control the quality of oncologic surgery have long been needed. The standards developed by the ACS during the past decade have been designed to reduce variability of care in oncologic surgery and improve the therapeutic outcomes for patients with cancer.
References
Graham R, et al (eds). Clinical Practice Guidelines We Can Trust. Institute of Medicine Committee on Standards for Developing Trustworthy Clinical Practice Guidelines, 2011. National Academies Press, Washington, D.C.
Smith TJ, Hillner BE. Ensuring quality cancer care by the use of clinical practice guidelines and critical pathways. J Clin Oncol. 2001;19:2886–97.
Guidelines by clinical area 2021 Retrieved 3 October 2021 at https://www.asco.org/practice-patients/guidelines.
NCCN Guidelines 2021 Retrieved 3 October at https://www.nccn.org/guidelines/category_1.
Osarogiagbon RU, et al. Prognostic value of National Comprehensive Cancer Network lung cancer resection quality criteria. Ann Thorac Surg. 2017;103:1557–65.
Williams AD, et al. Comparison of open and minimally invasive approaches to colon cancer resection in compliance with 12 regional lymph node harvest quality measure. J Surg Oncol. 2021;123:986–96.
CoC Quality of Care measures 2020 surveys. 2020 Retrieved 3 October 2021 at https://www.facs.org/quality-programs/cancer/ncdb/qualitymeasurescocweb.
Shulman LN, et al. Building data infrastructure to evaluate and improve quality: the National Cancer Data Base and the Commission on Cancer’s Quality Improvement Programs. J Oncol Pract. 2015;11:209–12.
Nelson H. American College of Surgeons, and Alliance for Clinical Trials in Oncology. Oper Stand Cancer Surg. 2015, Xxxiii:332.
Qaseem A, et al. The development of clinical practice guidelines and guidance statements of the American College of Physicians: summary of methods. Ann Intern Med. 2010;153:194–9.
Hunt K, editor. Operative Standards for Cancer Surgery. vol 2, Philadelphia: Walters Kluwer; 2019.
Butler JR, et al. A systematic review of the role of periadventitial dissection of the superior mesenteric artery in affecting margin status after pancreatoduodenectomy for pancreatic adenocarcinoma. HPB Oxford. 2016;18:305–11.
Katz MH, et al. Standardization of surgical and pathologic variables is needed in multicenter trials of adjuvant therapy for pancreatic cancer: results from the ACOSOG Z5031 trial. Ann Surg Oncol. 2011;18:337–44.
Zhao B, et al. Adherence to surgical and oncologic standards improves survival in breast cancer patients. J Surg Oncol. 2019;120:148–59.
Zhao B, et al. Adherence with operative standards in the treatment of gastric cancer in the United States. Gastric Cancer. 2020;23:550–60.
Shulman LN, et al. Compliance with cancer quality measures over time and their association with survival outcomes: the Commission on Cancer’s experience with the quality measure requiring at least 12 regional lymph nodes to be removed and analyzed with colon cancer resections. Ann Surg Oncol. 2019;26:1613–21.
Osarogiagbon RU, et al. Institutional-level differences in quality and outcomes of lung cancer resections in the United States. Chest. 2021;159:1630–41.
Chang GJ, et al. Lymph node evaluation and survival after curative resection of colon cancer: systematic review. J Natl Cancer Inst. 2007;99:433–41.
Optimal Resources for Cancer Care. Standards. Chicago: American College of Surgeons; 2020. p. 2019.
Boughey JC, et al. Sentinel lymph node surgery after neoadjuvant chemotherapy in patients with node-positive breast cancer: the ACOSOG Z1071 (Alliance) clinical trial. JAMA. 2013;310:1455–61.
Krag DN, et al. Sentinel lymph node resection compared with conventional axillary lymph node dissection in clinically node-negative patients with breast cancer: overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol. 2010;11:927–33.
Pesek S, et al. The false-negative rate of sentinel node biopsy in patients with breast cancer: a meta-analysis. World J Surg. 2012;36:2239–51.
Quan ML, et al. Beyond the false-negative rate: development of quality indicators for sentinel lymph node biopsy in breast cancer. Ann Surg Oncol. 2010;17:579–91.
Boova RS, Bonanni R, Rosato FE. Patterns of axillary nodal involvement in breast cancer: predictability of level one dissection. Ann Surg. 1982;196:642–4.
Tominaga T, Takashima S, Danno M. Randomized clinical trial comparing level II and level III axillary node dissection in addition to mastectomy for breast cancer. Br J Surg. 2004;91:38–43.
Kodama H, et al. Ten-year follow-up results of a randomised controlled study comparing level I vs level III axillary lymph node dissection for primary breast cancer. Br J Cancer. 2006;95:811–6.
Balch CM, et al. Efficacy of 2-cm surgical margins for intermediate-thickness melanomas (1 to 4 mm): results of a multi-institutional randomized surgical trial. Ann Surg. 1993;218:262–7.
Veronesi U, et al. Thin stage I primary cutaneous malignant melanoma: comparison of excision with margins of 1 or 3 cm. N Engl J Med. 1988;318:1159–62.
Cohn-Cedermark G, et al. Long-term results of a randomized study by the Swedish Melanoma Study Group on 2-cm versus 5-cm resection margins for patients with cutaneous melanoma with a tumor thickness of 08–20 mm. Cancer. 2000;89:1495–501.
Balch CM, et al. Long-term results of a multi-institutional randomized trial comparing prognostic factors and surgical results for intermediate thickness melanomas (10 to 40 mm). Intergroup Melanoma Surgical Trial. Ann Surg Oncol. 2000;7:87–97.
Balch CM, et al. Long-term results of a prospective surgical trial comparing 2 cm vs. 4 cm excision margins for 740 patients with 1–4 mm melanomas. Ann Surg Oncol. 2001;8:101–8.
Kapiteijn E, et al. Impact of the introduction and training of total mesorectal excision on recurrence and survival in rectal cancer in The Netherlands. Br J Surg. 2002;89:1142–9.
Nagtegaal ID, et al. Macroscopic evaluation of rectal cancer resection specimen: clinical significance of the pathologist in quality control. J Clin Oncol. 2002;20:1729–34.
Allen JW, et al. Quality of surgical resection for nonsmall cell lung cancer in a US metropolitan area. Cancer. 2011;117:134–42.
Osarogiagbon RU, D’Amico TA. Improving lung cancer outcomes by improving the quality of surgical care. Transl Lung Cancer Res. 2015;4:424–31.
Timeline and Compliance Information 2021 Retrieved 3 October 2021 at https://www.facs.org/quality-programs/cancer/coc/standards/2020/operative-standards/implementation.
Operative Standards Toolkit 2021 Retrieved 3 October 2021 at https://www.facs.org/quality-programs/cancer/cssp/resources/operative-standards-toolkit.
Hieken TJ, Burns WR, Francescatti AB, Morris AM, Wong SL. Cancer Surgery Standards Program of the American College of Surgeons. Ann Surg Oncol. 2022. https://doi.org/10.1245/s10434-022-11330-9
King S, Dimech M, Johnstone S. Structured pathology reporting improves the macroscopic assessment of rectal tumour resection specimens. Pathology. 2016;48:349–52.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Disclosure
Kelly K. Hunt reports relationships with Armada Health (Medical Advisory Board), Merck & Co. (Medical Advisory Board), and Research funding to MD Anderson Cancer Center–Eli Lilly & Co., Lumicell, Cairn Surgical. Matthew H. G. Katz and Amanda Francescatti have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Katz, M.H.G., Francescatti, A.B., Hunt, K.K. et al. Technical Standards for Cancer Surgery: Commission on Cancer Standards 5.3–5.8. Ann Surg Oncol 29, 6549–6558 (2022). https://doi.org/10.1245/s10434-022-11375-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-11375-w