Abstract
Background
Esophageal neuroendocrine carcinoma (ENEC) has a poor prognosis, and predicting the prognosis by examining various markers may contribute to the determination of treatment strategies. Therefore, a multiple-institution retrospective study was performed to identify biomarkers using diagnostic immunohistochemistry and serum tumor markers that predict the prognosis of patients with ENEC.
Methods
The results of immunohistochemical examination and serum tumor markers were extracted from the data of 141 ENEC patients at 39 institutions certified by the Japan Esophageal Society. The study then examined correlations between these data and prognosis or treatment effects.
Results
The ENEC patients with positively for all expression of synaptophysin (Syn), chromogranin A (CgA), and CD56 had a significantly worse prognosis than the patients with other expression patterns. Additionally, surgery and chemoradiotherapy were significantly more effective treatments than chemotherapy for the patients who were not positive for all expressions of Syn, CgA, and CD56. In terms of serum tumor markers, the patients with a high neuron-specific enolase (NSE) value had a significantly worse prognosis than the patients with a normal NSE value, and complete response (CR) cases treated with chemotherapy were significantly fewer in the high-NSE group. The results of multivariate analysis demonstrated that high NSE levels were an independent poor prognostic factor for esophageal endocrine cell carcinoma.
Conclusion
This study showed that positivity for all expressions of Syn, CgA, and CD56, and a high NSE value were significantly worse prognostic factors for ENEC patients than other expression patterns and may be important prognostic biomarkers of ENEC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Esophageal neuroendocrine carcinoma (ENEC) is an extremely rare type of malignant tumor characterized by high malignant potential, rapid growth, and poor prognosis.1 Compared with other types of esophageal cancer, ENEC is more malignant, and due to the lack of sufficient clinical data, no fixed treatment guidelines currently exist.2
We previously reported a large-scale nationwide survey of ENEC in Japan, demonstrating that the malignant potential of ENEC is greater than that of other histologic types of esophageal cancer. Additionally, we reported that the survival benefit of surgery is limited, especially for stages 3 and 4 ENEC.3 Patients with ENEC have a poor prognosis, and predicting the prognosis by examining various markers may contribute to the determination of treatment strategies.
Using immunostaining for diagnosis, the World Health Organization (WHO) definition of neuroendocrine carcinoma (NEC) includes positive endocrine markers such as chromogranin A (CgA), synaptophysin (Syn), and CD56. In addition, the diagnosis of NEC requires Ki67 or a mitotic index of 20/10 high-power fields or more, and tumors with a Ki67-positive rate of fewer than 20/10 high-power fields are diagnosed as neuroendocrine tumors.4
The most common markers for confirming tumor cell endocrine properties are CgA and Syn. Generally, CgA is slightly expressed in poorly differentiated NEC, but Syn is expressed in all neuroendocrine tumors (NETs).5,6 In this study, immunohistochemical data of CgA, Syn, and CD56 were extracted and analyzed.
In terms of serum tumor markers, squamous cell carcinoma antigen (SCC-Ag), carbohydrate antigen 19-9 (CA19-9), carcinoembryonic antigen (CEA), and cytokeratin 19 fragment antigen 21-1 are reported to be commonly used in diagnosis and as prognostic predictors of esophageal squamous cell carcinoma.7,8,9 Although no known prognostic biomarkers of ENEC have been found, Yan et al.10 reported that a low pretreatment serum level of neuron-specific enolase (NSE) is the most significant independent predictor of good overall survival for patients with esophageal small cell carcinoma.
In this study, we extracted immunostaining results and serum tumor marker data from the large dataset of the aforementioned nationwide survey and analyzed prognostic factors and treatment effects. We performed this multiple-institution retrospective study to identify biomarkers that predict the prognosis for patients with ENEC.
Patients and Methods
From January 2010 to December 2015, 141 patients with ENEC were treated at 39 institutions certified by the Japan Esophageal Society. We reviewed the patient records using a questionnaire form.3 The following data were extracted from the database: demographic data, pathologic findings, tumor progression, tumor location, macroscopic type, serum tumor marker levels (CEA, SCC-Ag, NSE, CA19-9, and ProGRP), and immunohistochemical profiles (synaptophysin, chromogranin A, and CD56). For serum tumor marker levels, data for 127 cases of SCC-Ag, 125 cases of CEA, 60 cases of CA19-9, 79 cases of NSE, and 45 cases of ProGRP were included. The serum tumor markers were divided into normal and high ranges and classified as normal and high groups. Moreover, 81 patients who underwent all immunohistochemical examinations were included in this study. The results of the immunohistochemical examinations were assessed as positive or negative at each facility.
Clinical staging and pathologic examination of resected specimens were performed according to the Guidelines for Clinical and Pathological Studies on Carcinoma of the Esophagus of the Japanese Society for Esophageal Diseases.11 Standard clinical measurements and radiologic examinations were performed to assess the tumor response according to the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1.12 Overall survival (OS) was calculated from the first day of initial treatment to the date of death or the last follow-up day of survivors. The ethics committee of each institution approved our retrospective analysis.
Statistical Analysis
All statistical analyses were performed using JMP Pro Version 14 software (SAS Institute Japan, Tokyo, Japan). Continuous data were assessed using Student’s t test or the Mann-Whitney U test, whereas categorical data were assessed using Person’s chi-square test, Fisher’s exact test, or the Mann-Whitney U test as appropriate. Kaplan-Meier analysis and log-rank tests were used to estimate the association between eligible variables and survival time. Independent prognostic factors were evaluated using Cox hazard regression models. All p values lower than 0.05 were considered statistically significant.
Results
Prognosis by Immunostaining in ENEC Patients
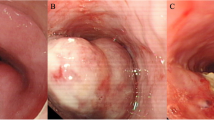
Figure 1a shows a comparison of prognosis by each immunostaining (synaptophysin, chromogranin A, and CD56) for the ENEC patients. No significant differences were observed in prognosis between positivity and negativity for each immunostaining.
A Comparison of prognosis by each immunostaining for the patients with esophageal neuroendocrine carcinoma (ENEC). No significant differences in prognosis between positivity and negativity were found for any of the immunostaining methods. B Comparison of prognosis between positivity for all and others in ENEC patients. The 5-year overall survival rates of the positivity for all and others were respectively 45.46% and 23.38%.
Subgroup Analysis of All Positive Cases by Immunostaining
In the examination performed under the condition that all the results of immunostaining for diagnosis were positive, the prognosis was significantly poor in all positive cases compared with other cases (Fig. 1b). Based on this result, a comparison of the background between all positive cases and other cases by immunostaining results was performed to investigate the factor influencing the poor prognosis (Table 1). However, no significant differences were observed between all the positive cases and the other cases in terms of patient characteristics and disease progression.
Additionally, we performed comparative analysis of prognosis by treatment type in all the positive cases and other cases by immunostaining (Fig. 2). Regarding the number of treatments in each group among all the positive cases, 13 patients had surgery, 7 patients had chemoradiotherapy (CRT), and 11 patients had chemotherapy (CT). On the other hand, among the other cases, 26 patients had surgery, 13 patients had CRT, and 11 patients had CT.
Comparison of prognosis by treatment type in all positive cases and other cases by immunostaining. a The 5-year overall survival rate for the operation group was 24.6%. The CRT group had a short observation period and was unevaluable, and even the 2-year survival period was not obtained for the CT group. b The 5-year overall survival rate was 55.1% for the surgery group, 47.2% for the CRT group, and 0% for the CT group.
None of the positive cases showed a significant difference in prognosis by treatment type (p = 0.263). However, surgery and CRT were significantly more effective treatments than CT in the other cases (p = 0.028). Moreover, concerning the treatment effect by treatment type, none of the positive cases differed significantly from the other cases (data not shown).
Comparison of Prognosis by Each Serum Tumor Marker in ENEC Patients
Figure 3 shows the comparison of prognosis by each tumor marker in ENEC patients. The patients in the high-NSE group had a significantly worse prognosis than those in the normal-NSE group (p = 0.0003), although there was no significant difference between prognosis and the other tumor marker levels.
Comparison of prognosis by each serum tumor marker for the patients with esophageal neuroendocrine carcinoma (ENEC). The high neuron-specific enolase (NSE) group had a significantly worse prognosis than the normal NSE group. However, no significant difference was observed between prognosis and other serum tumor markers.
Based on the aforementioned result, the backgrounds of the high- and normal-NSE groups were compared to investigate the factors influencing a poor prognosis (Table 2). There were significant differences between the high-NSE group and depth of invasion (p = 0.019), lymph node metastasis (p = 0.038), distant metastasis (p < 0.001), and stage (p = 0.002).
Regarding the correlation between the NSE level and therapeutic effect, there was no significant difference in prognosis by treatment type in each group (Fig. 4). However, as shown in Fig. 4, non-operative treatment may be recommended for normal-NSE patients. Conversely, operative treatment may be recommended for high-NSE patients.
Comparison of prognosis by treatment type for the patients of each neuron-specific enolase (NSE) group. a The 5-year overall survival rates for the normal NSE patients were 33.9% in the surgery group and 53.2% in the non-surgery groups (CRT/CT). b The 5-year overall survival rates for the high NSE patients were 40.0% for the surgery group and 0% for the non-surgery (CRT/CT) (insufficient observation period).
Additionally, we performed correlation analysis between treatment effects by the NSE value in each treatment type. There was no significant difference between treatment effects by the NSE value in the surgery or CRT group. However, there was a significant difference between treatment effects by the NSE value in the CT group. CR The high-NSE group had significantly fewer cases (Fig. 5). Table 3 details the factors that contributed to survival, as identified in the multivariate analysis. Accordingly, multivariate analysis identified high NSE levels (>16.3 ng/mL) as an independent factor of poor prognosis for esophageal neuroendocrine cell carcinoma.
Discussion
In the current study, we extracted the results of immunostaining and serum tumor marker data from a previous large-scale study of esophageal NEC and examined the prognosis and effect of each treatment. Our study included a large sample and analyzed protein expression of specific markers determined by diagnostic immunohistochemistry and pretreatment levels of several serum tumor markers as well as their prognostic value for ENEC patients.
Zhang et al.13 showed the favorable prognostic value of Syn, CgA, NSE, and TTF-1 for patients with esophageal small cell carcinoma. Conversely, our data on Syn, CgA, and CD56 implied an unfavorable prognostic value, although no significant difference between each marker and prognosis was found. These differences are difficult to explain because the two studies did not differ significantly. The background factors were different, and there was insufficient information such as the degree of differentiation. However, our data showed that the positivity of patients for all expression of Syn, CgA, and CD56 immunostaining had a significantly worse prognosis than that of patients with the other staining pattern. This result is new data showing a significant difference and a new finding that approaches the pathology of ENEC. Moreover, it was interesting that no correlation was found between all expression of Syn, CgA, and CD56 immunostaining and tumor progression or various treatment effects. The ability to predict prognosis by immunostaining for diagnosis is an important finding, and it may be an important biomarker.
Regarding the serum tumor marker examination, the high-NSE group had a significantly worse prognosis than the normal-NSE group (Fig. 3). The results were similar to those of a previous report10 indicating that NSE is an important prognostic predictive marker for ENEC. Our data showed that this result is attributable to the significant correlation between the high NSE level and depth of invasion, lymph node metastasis, distant metastasis, and stage. Examination of the other tumor markers also showed a good prognosis in the normal group, but no significant difference (Fig. 3).
Our study also showed that CRT may be recommended for normal-NSE patients and that surgery may be recommended for high-NSE patients, although the study had insufficient cases to determine treatment strategy based on NSE results alone. This report is not only a description detailing the prognosis of NSE, but also the first report to show that treatment policy is determined by the value of NSE, and future case accumulation will further prove this.
Additionally, Yan et al.10 reported that the effectiveness of CRT was significantly associated with the serum levels of NSE before treatment. Our data did not show a significant difference between treatment effects by NSE value in the CRT group. However, treatment effects differed significantly by the NSE value in the CT group. Among the high-NSE cases, CR cases were significantly fewer. Our data showed that NSE may be a reliable surrogate marker of CT efficacy for patients with ENEC. In previous reports, including our previous report, CT did not show a sufficient prognostic effect in ENEC patients.3 Therefore, CT should be avoided, especially for patients with high NSE, although systemic CT has been recommended as a treatment for ENEC.14 The high NSE group was correlated with tumor progression, and local treatment such as surgery or CRT cannot be applied in many cases. Furthermore, given that multivariate analysis showed high preoperative NSE to be an independent poor prognosis factor, the development of effective treatment methods for patients with esophageal neuroendocrine carcinoma presenting with high preoperative NSE is imperative for further improvement of the prognosis for overall esophageal endocrine cell carcinoma.
This study showed that positivity for all expression of Syn, CgA, and CD56 and a high NSE value were significantly worse prognostic factors for ENEC patients and may be important prognostic biomarkers of ENEC. A large-scale study is necessary because our study had many limitations such as an insufficient number of cases in each study and difficulty examining the details of each case due to the questionnaire survey. However, because ENEC is a disease with a small number of cases and a poor prognosis, it is important to continue study of prognostic markers to provide more effective treatment and prevent ineffective treatment.
References
Ma Z, Cai H, Cui Y. Progress in the treatment of oesophageal neuroendocrine carcinoma. Tumour Biol. 2017. https://doi.org/10.1177/1010428317711313.
Cai W, Ge W, Yuan Y, et al. A 10-year population-based study of the differences between NECs and carcinomas of the esophagus in terms of clinicopathology and survival. J Cancer. 2019;10:1520–1527. https://doi.org/10.7150/jca.29483.
Sohda M, Kuwano H, Saeki H, et al. Nationwide survey of neuroendocrine carcinoma of the esophagus: a multicenter study conducted among institutions accredited by the Japan Esophageal Society. J Gastroenterol. 2021;56:350–359. https://doi.org/10.1007/s00535-020-01756-x
Arnold R, Capella C, Klimstra DS. Neuroendocrine neoplasms of the oesophagus. Bosman FT, Car nerio F, Hruban RH, Theise ND, editors. Lyons, France: IARC press; 2010.
Hirabayashi K, Zamboni G, Nishi T, Tanaka A, Kajiwara H, Nakamura N. Histopathology of gastrointestinal neuroendocrine neoplasms. Front Oncol. 2013;3:2. https://doi.org/10.3389/fonc.2013.00002.
Capelli P, Fassan M, Scarpa A. Pathology - grading and staging of GEP-NETs. Best Pract Res Clin Gastroenterol. 2012;26:705–717. https://doi.org/10.1016/j.bpg.2013.01.003.
Cao X, Zhang L, Feng GR, et al. Preoperative Cyfra21-1 and SCC-ag serum titers predict survival in patients with stage II esophageal squamous cell carcinoma. J Transl Med. 2012;10:197. https://doi.org/10.1186/1479-5876-10-197.
Zhang HQ, Wang RB, Yan HJ, et al. Prognostic significance of CYFRA21-1, CEA, and hemoglobin in patients with esophageal squamous cancer undergoing concurrent chemoradiotherapy. Asian Pac J Cancer Prev. 2012;13:199–203. https://doi.org/10.7314/apjcp.2012.13.1.199.
Ikeguchi M, Kouno Y, Kihara K, et al. Evaluation of prognostic markers for patients with curatively resected thoracic esophageal squamous cell carcinomas. Mol Clin Oncol. 2016;5:767–772. https://doi.org/10.3892/mco.2016.1073.
Yan H, Wang R, Jiang S, et al. NSE can predict the sensitivity to definitive chemoradiotherapy of small cell carcinoma of esophagus. Med Oncol. 2014;31:796. https://doi.org/10.1007/s12032-013-0796-0.
Japanese Society for Esophageal Disease. [Guidelines for the Clinical and Pathological Studies on Carcinoma of the Esophagus 11th edn.]. Kanehara, Tokyo, 2015.
Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–247. https://doi.org/10.1016/j.ejca.2008.10.026.
Zhang Y, Li C, Chen M. Prognostic value of immunohistochemical factors in esophageal small cell carcinoma (ESCC): analysis of clinicopathologic features of 73 patients. J Thorac Dis. 2018;10:4023–4031. https://doi.org/10.21037/jtd.2018.06.26.
Lv J, Liang J, Wang J, et al. Primary small cell carcinoma of the esophagus. J Thorac Oncol. 2008;3:1460–1465. https://doi.org/10.1097/JTO.0b013e31818e1247.
Acknowledgments
We thank Edanz Group (https://en-author-services.edanzgroup.com/) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
There are no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sohda, M., Saeki, H., Kuwano, H. et al. Diagnostic Immunostaining and Tumor Markers Predict the Prognosis of Esophageal Neuroendocrine Cell Carcinoma Patients. Ann Surg Oncol 28, 7983–7989 (2021). https://doi.org/10.1245/s10434-021-09872-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-09872-5