Abstract
Patients with esophageal small cell carcinoma undergoing definitive chemoradiotherapy (CRT) seem to have disparity in tumor response. The identification of CRT sensitivity-related tumor markers would be helpful for selecting patients most likely to benefit from CRT. The aim of this study was to examine the predictive value of biological markers in small cell carcinoma of the esophagus (SCEC) patients treated with definitive CRT. Pretreatment serum levels of neurone-specific enolase (NSE), cytokeratin 19 fragment antigen 21-1 (CYFRA21-1), and carcinoembryonic antigen (CEA) were measured by immunoradiometric assays, while the tumor responses were evaluated according to the World Health Organization response criteria. The relationships between pretreatment expression of NSE, CYFRA21-1, CEA, and the tumor response to CRT were analyzed. The effective rates (complete response + partial response) in NSE high and low groups were 10.80 % (9/82) and 37.98 % (31/82), respectively (P = 0.003).The results from statistical analysis indicated that the effectiveness of CRT was significantly associated with the serum levels of NSE before treatment (P = 0.002). The overall survival (OS) of the patients with high NSE levels was worse than that of those with low NSE levels (P = 0.004). In multivariate analysis, low level of NSE was the most significant independent predictor of good OS (P = 0.003). The result showed a promising predictive value of NSE regarding to the sensitivity of tumors to CRT. NSE may be a reliable surrogate marker of CRT efficacy in patients with SCEC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary small cell carcinoma of the esophagus (SCEC) is a rare disease, which was first described in 1952 by McKeown [1]. SCEC is characterized by high malignancy, distant metastasis, and poor prognosis [2]. The disappointing rates of survival and local control associated with single modality therapy, and the need for effective non-surgical management led to the development of definitive chemoradiotherapy (CRT) paradigms for esophageal cancer [3, 4]. A retrospective comparison of surgical resection and definitive CRT showed survival rates that were comparable to surgical results, suggesting that CRT was useful as an alternative treatment [5]. However, the response of individual tumors to CRT is not uniform. Therefore, it would be significant to identify biomarkers in predicting responsiveness to CRT and prognosis, which would be extremely helpful in selecting optimal treatment protocols for patients. However, there are no studies about biomarkers associated with sensitivity to CRT on the primary lesions of SCEC. Hence, we performed this single-institution and retrospective study to identify biomarkers that predict tumor response in patients with SCEC who received definitive CRT.
Materials and methods
Eighty-two patients diagnosed with SCEC and treated with definitive CRT between February 1992 and December 2012 in our institution were recruited from our database on the basis of the following criteria: (1) pathologically confirmed and previously untreated SCEC; (2) Karnofsky performance status (KPS) scale 80–100; (3) clinical stage T1–T4, N0, or N1, and M0 or M1 according to the International Union Against Cancer tumor-node-metastasis (TNM) classification; (4) adequate bone marrow, renal, and hepatic function; (5) no severe medical complications. Informed consents were obtained from all patients.
Pretreatment evaluation
Pretreatment evaluation included barium swallow, endoscopy of the esophagus, and computed tomography (CT) of the neck, chest, and abdomen. Endoscopic ultrasound of the esophagus, ultrasound of the neck, and PET-CT were optional. The T-factor in patients with <T4 was determined by endoscopic ultrasound or endoscopy (or both). Metastatic lymph nodes were defined if they were ≥1 cm in their greatest diameter on any imaging technique. We collected blood by venipuncture and obtained serum samples after clotting and centrifugation which were then stored at −80 °C. Serum levels of neurone-specific enolase (NSE), cytokeratin 19 fragment antigen 21-1 (CYFRA21-1), and carcinoembryonic antigen (CEA) were measured by immunoradiometric assays (Boehringer Mannheim GmbH, Mannheim, Germany). The cutoff points were at 17 ng/ml of NSE, 3.4 ng/ml of CYFRA21-1, and 3.3 ng/ml of CEA, respectively, according to the 95 % confidence intervals of non-cancer Chinese patients.
Treatment schedule
The treatment consisted of two cycles of etoposide (100 mg/m2 intravenously on Days 1–3) and cisplatin (25 mg/m2 intravenously on Days 1–3), combined with radiotherapy of 60 Gy in 30 fractions over 8 weeks, including a 2-week break. Radiation therapy was delivered with megavoltage equipment using anterior–posterior opposed fields up to 40 Gy, including the primary tumor, the metastatic lymph nodes, and the regional nodes. A booster dose of 20 Gy was given to the primary tumor and the metastatic lymph nodes for a total dose of 60 Gy, using bilateral oblique or multiple fields.
Response assessment
The clinical response to CRT was evaluated by the findings of barium esophagogram, esophagoscopy, endoscopic ultrasonography, and CT. Tumor response was assessed according to the RECIST (response evaluation criteria in solid tumors) response criteria: complete response (CR), disappearance of all target lesions, confirmed at 4 weeks; partial response (PR), at least a 30 % decrease in the sum of the longest diameter of target lesions, taking as reference the baseline sum longest diameter; stable disease (SD), neither PR nor progressive disease (PD) criteria are met, taking as reference the smallest sum of the longest diameter recorded since treatment started; PD, at least 20 % increase in the sum of the longest diameter of target lesions, taking as reference the smallest sum longest diameter recorded since treatment started or appearance of new lesions. For statistical analysis, the clinical effect was divided into two groups: effective group consisted of patients with CR and PR, while ineffective group included patients with SD and PD.
Statistical analysis
Chi-square or Fisher exact tests were performed to determine significant univariate predictors of early efficacy of CRT. Then, a logistic regression analysis was used to identify the significant multivariate predictors. Receiver operating characteristic (ROC) curves were constructed to determine the discriminatory capacity of biomarkers for prediction, and the area under the curve (AUC) was analyzed by χ 2 test. Overall survival (OS) was calculated using the Kaplan–Meier method. OS was defined as the time from start of treatment to death; data on survivors were censored at the last follow-up. The differences between the survival curves were tested by using the log-rank test. The Cox proportional hazards regression model was used to determine the joint effects of several variables on survival. For all statistical analysis, Statistica13.0 was used. Values of P < 0.05 or 95 % were considered as having a statistical significance.
Results
Tumor response
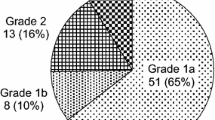
A total of 40 patients (48.78 %) with CR or PR were judged as effective, whereas 42 patients (51.22 %) with SD or PD were judged as ineffective. The effective rates (CR + PR) in NSE high and low groups were 10.98 % (9/82) and 37.80 % (31/82), in CYFRA21-1 high and low groups were 23.17 % (19/82) and 25.61 % (21/82), while in CEA high and low groups, they were 20.73 % (17/82) and 28.05 % (23/82), respectively. The effective rates (CR + PR) in different T stage of tumor were 3.66 % (3/82), 3.66 % (3/82), 24.39 % (20/82), and 17.07 % (14/82), respectively (Table 1).
Correlation between pretreatment clinicopathological characteristics and tumor response
The effectiveness of CRT was significantly associated with the serum levels of NSE before treatment. The differences of the effective rates between NSE high and low groups were significant (P = 0.003). The differences of the effective rates between CYFRA21-1 high and low groups were significant (P = 0.042).The univariate analysis also indicated that the efficacy of CRT was significantly associated with the pretreatment T stage of tumor (P = 0.024) (Table 1). The other variables that were evaluated (age, gender, tumor length, KPS, CEA, tumor location, clinical N and M stage) were not associated significantly with tumor response (Table 1). There was no significant association between the serum levels of NSE, CYFRA21-1, CEA levels, and TNM stage (Table 2). The multivariate logistic regression analysis showed that the efficacy of CRT was significantly associated with the levels of NSE before treatment (P = 0.002) (Table 3). That is to say patients with low NSE were sensitive to CRT. We then applied the ROC curve analysis method to explore the predictive value of serum levels of NSE CYFRA21-1 and CEA in the group of patients with CR + PR in relation to the effectiveness of CRT (Figs. 1, 2, 3). The AUC of using NSE as predictive value for the sensitivity of tumors to CRT was 0.803 (95 % CI = 0.701–0.911, P = 0.001), in contrast to an AUC for CYFRA21-1 and CEA of 0.649 (95 % CI = 0.571–0.698, P = 0.053) and 0.577 (95 % CI = 0.513–0.599, P = 0.134), respectively (Table 4).
Association of pretreatment clinicopathological characteristics with patient long outcome
In univariate analysis, low level of NSE was associated with good OS (P = 0.004) in addition to acquiring of good efficacy (Fig. 4; Table 5). Low level of CYFRA21-1 and CEA was not correlated with patient outcome (P > 0.05) (Table 6). In multivariate analysis, low level of NSE was the most significant independent predictor of good OS (P = 0.003) followed by acquire of good efficacy (Table 6). The result showed a promising predictive value of NSE regarding to the sensitivity of tumors to CRT.
Discussion
Serum NSE is a key enzyme involved in glycolysis; there are three subunits including α, β, and γ that compose five isoenzymes [6]. NSE is a well-established tumor marker for SCLC, and is produced by other neuroendocrine tumors too. Although the prognostic value of NSE in SCLC had been widely accepted [7, 8], a high level of NSE also could be observed in some NSCLC and might be correlated with poor prognosis [9, 10]. The results in the present study indicated that preoperative serum NSE levels could be used as a biomarker for outcome prediction in non-small cell lung cancer. Elevated serum NSE levels were correlated with worse prognosis in NSCLC patients [11, 12]. The histology and clinical characteristics of SCEC are similar to SCLC. However, little is known about its usefulness for the early prediction of therapy response in patients with SCEC. We firstly analyzed the pretreatment levels of NSE and reported the correlation between NSE and tumor response to chemoradiation in SCEC. In our study, we found that the effective rates in NSE high and low groups were significantly different (P = 0.003). We also found that there was no correlation between the pretreatment serum NSE levels and TNM stage. Meanwhile, the effectiveness rates of CRT were significantly associated with the pretreatment levels of NSE by logistic regression analysis. By ROC curve analysis, we could detect that NSE showed a significant predictive value for the sensitivity of tumors to CRT. The overall survival of the patients with high NSE levels was worse than that of those with low NSE levels (P = 0.004). In multivariate analysis, a low level of NSE was the most significant independent predictor of good OS (P = 0.003). Our study showed that lowering this cutoff point to 3.4 ng/ml might be more useful in current clinical practice. It showed that NSE may be an independent predictor for definitive CRT sensitivity in SCEC.
CYFRA21-1 is an epitope of a polypeptide, which recognizes soluble cytokeratin-19 fragments [13, 14]. There have been many reports on the relationship between pretreatment levels of CYFRA21-1 and clinical response for ESCC. A study showed that CYFRA21-1 appears to be a useful marker for human squamous cell carcinoma of the esophagus [15]. Kunisaki et al. [16] reported only the serum cytokeratin (CYFRA) level independently predicted the responsiveness to treatment. Previous studies showed a positive correlation between the serum CYFRA21-1 levels before treatment and TNM stage in patients with squamous cell carcinoma of the esophagus [17]. The predictive value of CYFRA21-1 has been reported in NSCLC and ESCC. However, the prediction of CYFRA21-1 in SCEC remains unknown. In our study, we found that there was no correlation between the serum CYFRA21-1 levels before treatment and TNM stage. In our study, the logistic regression analysis indicated a statistically significant difference was not found between pretreatment levels of CYFRA21-1 and tumor response. This may partly be because the sample was relatively small. This result should be confirmed by study of larger and more homogeneous samples.
CEA is the most widely used and readily available tumor marker for the management of colorectal carcinoma [18]. It is helpful in the diagnosis, prediction of prognosis, and monitor of postoperative recurrence in patients with ESCC [19, 20]. A study showed significant relationship between elevated serum CEA levels and distant metastases in esophageal cancer [21]. Yi et al. [22] reported that CEA may be helpful in predicting the responsiveness in ESCC of primary lesions to CRT. However, there were no studies about CEA associated with sensitivity to CRT on the primary lesions of SCEC. In our study, the efficacy of CRT was not significantly associated with pretreatment levels of CEA (P = 0.339).
In our univariate analysis, we also found that there is a significant correlation between tumor response and T stage. The correlation of tumor response with T stage, however, has not been extensively studied. Although molecular markers and gene expression profiling are likely to play increasing roles in predicting [23, 24], the role of clinical predictive factors, such as NSE and CYFRA21-1, should not be overlooked. Moreover, we need to assess carefully how much additional information molecular markers provide compared with cheap, easily measurable clinical predictors. Such factors may promote the development of individualized, risk-adapted treatment strategies for patients. Above-mentioned clinical predictive factors also should be synthesized to consider to obtain a very exact result.
In conclusion, this retrospective study firstly demonstrated that NSE may be useful predictor of sensitivity of SCEC to CRT. It is important to analyze the pretreatment serum levels of NSE for predicting the response to the treatment. These predictive factors may conduce to predict outcomes for patients and also may be used to guide individualized and targeting treatment for patients who receive newer therapies for SCEC. However, the results should be further confirmed in larger, more homogeneous studies.
References
Coia LR. Chemoradiation as primary management of esophageal cancer. Semin Oncol. 1994;21(4):483–92.
Forastiere AA, Orringer MB, Perez-Tamayo C, Urba SG, Zahurak M. Preoperative chemoradiation followed by transhiatal esophagectomy for carcinoma of the esophagus: final report. J Clin Oncol. 1993;11(6):1118–23.
Ohtsu A, et al. Concurrent chemotherapy and radiation therapy for locally advanced carcinoma of the esophagus. Jpn J Clin Oncol. 1995;25(6):261–6.
Hironaka S, et al. Nonrandomized comparison between definitive chemoradiotherapy and radical surgery in patients with T(2-3)N(any)M(0) squamous cell carcinoma of the esophagus. Int J Radiat Oncol Biol Phys. 2003;57(2):425–33.
Stahl M, et al. Chemoradiation with and without surgery in patients with locally advanced squamous cell carcinoma of the esophagus. J Clin Oncol. 2005;23(10):2310–7.
Jørgensen LG, et al. Serum neuron-specific enolase (S-NSE) and the prognosis in small-cell lung cancer (SCLC): a combined multivariable analysis on data from nine centres. Br J Cancer. 1996;74(3):463–7.
Schneider J, Philipp M, Salewski L, Velcovsky HG. Pro-gastrin-rel easing peptide (ProGRP) and neuron specific enolase (NSE) in therapy control of patients with small-cell lung cancer. Clin Lab. 2003;49(1–2):35–42.
Pujol JL, et al. Neuroendocrine and cytokeratin serum markers as prognostic determinants of small cell lung cancer. Lung Cancer. 2003;39(2):131–8.
Barlesi F, et al. Prognostic value of combination of Cyfra 21–1, CEA and NSE in patients with advanced non-small cell lung cancer. Respir Med. 2004;98(4):357–62.
Nisman B, Heching N, Biran H, Barak V, Peretz T. The prognostic significance of circulating neuroendocrine markers chromogranin a, pro-gastrin-releasing peptide and neuron-specific enolase in patients with advanced non-small-cell lung cancer. Tumour Biol. 2006;27(1):8–16.
Pujol JL, Boher JM, Grenier J, Quantin X. Cyfra 21–1, neuron specific enolase and prognosis of non-small cell lung cancer: prospective study in 621 patients. Lung Cancer. 2001;31(2–3):221–31.
Jacot W, et al. Brain metastases at the time of presentation of non-small cell lung cancer: a multi-centric AERIO analysis of prognostic factors. Br J Cancer. 2001;84(7):903–9.
Stieber P, et al. Comparison of cytokeratin fragment 19 (CYFRA 21-1), tissue polypeptide antigen (TPA) and tissue polypeptide specific antigen (TPS) as tumour markers in lung cancer. Eur J Clin Chem Clin Biochem. 1993;31(2):689–94.
Bodenmüller H, Donié F, Kaufmann M, Banauch D. The tumor markers TPA, TPS, TPACYK and CYFRA 21-1 react differently with the keratins 8, 18 and 19. Int J Biol Markers. 1994;9(2):70–4.
Yamamoto K, et al. CYFRA 21-1 is a useful marker for esophageal squamous cell carcinoma. Cancer. 1997;79(9):1647–55.
Kunisaki C, et al. Prognostic factors after chemoradiotherapy for patients with inoperable esophageal squamous cell carcinoma. Hepatogastroenterology. 2006;53(69):366–71.
Kawaguchi H, et al. CYFRA 21-1 determination in patients with esophageal squamous cell carcinoma: clinical utility for detection of recurrences. Cancer. 2000;89(7):1413–7.
Das P, et al. Predictors of tumor response and downstaging in patients who receive preoperative chemoradiation for rectal cancer. Cancer. 2007;109(9):1750–5.
Mao YS, et al. Significance of CEA, SCC and Cyfra21-1 serum test in esophageal cancer. Zhonghua Zhong Liu Za Zhi. 2003;25(5):457–60.
Mroczko B, et al. The diagnostic value of the measurement of matrix metalloproteinase 9 (MMP-9), squamous cell cancer antigen (SCC) and carcinoembryonic antigen (CEA) in the sera of esophageal cancer patients. Clin Chim Acta. 2008;389(1–2):61–6.
Kosugi S, et al. Clinical significance of serum carcinoembryonic antigen, carbohydrate antigen 19-9, and squamous cell carcinoma antigen levels in esophageal cancer patients. World J Surg. 2004;28(7):680–5.
Yi Y, et al. CYFRA21-1 and CEA are useful markers for predicting the sensitivity to chemoradiotherapy of esophageal squamous cell carcinoma. Biomarkers. 2009;14(7):480–5.
Gotoh M, et al. Epidermal growth factor receptor is a possible predictor of sensitivity to chemoradiotherapy in the primary lesion of esophageal squamous cell carcinoma. Jpn J Clin Oncol. 2007;37(9):652–7.
Hildebrandt MA, et al. Genetic variations in the PI3 K/PTEN/AKT/mTOR pathway are associated with clinical outcomes in esophageal cancer patients treated with chemoradiotherapy. J Clin Oncol. 2009;27(6):857–71.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yan, H., Wang, R., Jiang, S. et al. NSE can predict the sensitivity to definitive chemoradiotherapy of small cell carcinoma of esophagus. Med Oncol 31, 796 (2014). https://doi.org/10.1007/s12032-013-0796-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-013-0796-0