Abstract
Background
There is an increasing desire for contralateral prophylactic mastectomy (CPM) among patients with unilateral breast cancer. It is unknown if risk assessment and genetic testing at the time of diagnosis will aid women in their surgical choice. We report on the uptake and predictors of CPM in women receiving a negative genetic test result for BRCA1 and BRCA2 mutations before surgery.
Methods
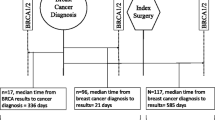
Women diagnosed with breast cancer between June 2013 and May 2018 were recruited from four academic health sciences centers in Toronto, Canada. Genetic counseling (risk assessment) and genetic testing was performed prior to surgery. Women were asked about their surgical preference before surgery. At 1 year post-surgery we asked what surgery was completed. This study reports on women who received a negative BRCA1/BRCA2 result.
Results
A total of 766 women with a mean age of 46 years (range 21–82) were included in the analysis. Before genetic counseling and testing, 37% of the women were undecided or leaning towards CPM; however, after receiving a negative BRCA test, 15% of the women opted for CPM. Thirty percent of women whose mother died of breast cancer elected for CPM, compared with 15% of women whose mother did not die of breast cancer (p = 0.03).
Conclusions
Women receiving a risk assessment and negative BRCA1/BRCA2 genetic test result before surgery use this information to guide their surgical decision. Uptake of CPM for women who were planning on CPM before genetic testing decreases after receiving a negative BRCA1/BRCA2 genetic test result.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
For women diagnosed with unilateral breast cancer, the choice of contralateral prophylactic mastectomy (CPM) is a personal one. For breast cancer patients as a whole, a survival advantage has not been reported in association with CPM. National and international guidelines do not support the use of CPM in average-risk women;1,2 nevertheless, the uptake of CPM has increased in recent years in many countries; in the United States, reported CPM rates have ranged between 4% and 25%.3,4,5,6
The 25-year lifetime risk of contralateral breast cancer is approximately 30% for women who have a BRCA1 or BRCA2 mutation and 10% for women without a mutation.7 For women with a BRCA1 or BRCA2 mutation, CPM reduces the risk of a contralateral breast cancer8 and may reduce long-term mortality.9 However, most women are unaware of their BRCA1/ BRCA2 mutation status at the time of breast cancer diagnosis. We have recently reported that among women with breast cancer who are aware that they carry a BRCA1 or BRCA2 mutation, the uptake of CPM is 78%.10 These high-risk women reported that knowledge of the positive genetic test influenced their decision for contralateral mastectomy; however, it is unclear to what extent women who receive a negative BRCA1 and BRCA2 genetic test result use this information when making their decision.
Women often overestimate the risk of contralateral cancer and the survival advantage associated with CPM;11 this highlights the need for presurgical education and counseling. Genetic counsellors have the opportunity to communicate the risk of contralateral breast cancer and to help women understand their risk in the context of the genetic test result, including those who test negative. Genetic counseling can lead to increased knowledge, perceived personal control, more accurate risk perception accuracy, and decreased anxiety and cancer-related distress.12
To better understand the motivation behind a woman’s decision to undergo CPM, it is helpful to identify predictors of uptake of CPM. These factors may or may not relate to the actual risk of contralateral breast cancer. Younger age, higher education, insurance coverage, and White race have all been associated with higher rates of CPM.3,4,13,14,15 Psychosocial factors that predict uptake of CPM include anxiety, distress, and concern about body image.16,17
The implications of having a positive genetic test result on CPM have been well-studied and, in general, most surgeons endorse CPM for BRCA mutation carriers. However, it is less common for physicians to recommend CPM for their patients with a positive family history but a negative genetic test result. In this case, the patient’s wish to have the operation is the determining factor. It is unclear if women who are told that they do not carry a BRCA mutation use this information to make surgical choices, or if there are predictors of uptake of CPM in women who receive a negative genetic test result. In the current study, we report on the uptake of CPM in women who received a negative BRCA1 and BRCA2 genetic test result at the time of surgical decision making.
Methods
Study Population
Participants included women diagnosed with invasive breast cancer at one of four academic health sciences centers in Toronto, Canada (Women’s College Hospital, Sunnybrook Health Sciences Centre, St. Michael’s Hospital, and University Health Network) between June 2013 and May 2018. Inclusion criteria to be offered study participation and rapid genetic testing for BRCA1 and BRCA2 were first primary invasive breast cancer, no previous prophylactic breast surgery, age 18 years or older, able to read and understand English, and no previous testing for BRCA1 or BRCA2 mutations. In addition, women also had to meet at least one of the following criteria: Jewish ethnicity; triple-negative breast cancer; age of diagnosis ≤50 years; synchronous bilateral breast cancer or a family history of breast cancer. A positive family history was defined as a first- or second-degree relative with breast cancer diagnosed at age 50 years or younger, ovarian cancer at any age, or male breast cancer at any age.
Study Procedures
The study protocol received ethics approval from all participating institutions. At the time of breast cancer diagnosis, potentially eligible women were referred to the study by their breast surgeon and were contacted by telephone within 24 business hours. The genetic counsellor assessed eligibility. All participants provided written consent for participation in the study. Participants received standard pretest genetic counseling and were offered rapid genetic testing for BRCA1 and BRCA2 mutations. Genetic testing was performed at one of three laboratories (Mount Sinai Hospital, North York General Hospital, or Women’s College Hospital). Genetic test results were disclosed by the genetic counsellor via telephone prior to surgery and results were faxed to the referring surgeon.
Measures
Participants completed baseline questionnaires prior to genetic counseling and a follow-up questionnaire at 1 week after receipt of the genetic test results.
Study-Specific Baseline Questionnaire: Sociodemographic variables included age, marital status, education, and parity. Women were also asked what surgery (lumpectomy, unilateral mastectomy, bilateral mastectomy, or unsure) they were leaning towards. The study personnel took a complete three-generation family history from each participant. Data collected included information on relatives’ cancer diagnoses, including type of cancer, age at cancer diagnosis, and vital status.
Cancer-related distress was measured at baseline using the Impact of Event Scale (IES),18 a validated 15-item questionnaire that assesses subjective distress surrounding a stressful event (specified as ‘having a breast cancer diagnosis’). Each item is rated on a 5-point scale from 0 (‘not at all’) to 5 (‘often’). The sum of the ratings on each item is the total distress score. Higher total scores represent greater distress: 0–8, subclinical range; 9–25, mild; 26–43, moderate; and 44+ severe.
Anxiety was measured at baseline using the anxiety subscale of the Hospital Anxiety and Depression Scale (HADS),19,20 a validated, 14-item questionnaire that assesses anxiety (7 items) and depression (7 items), with subscale scores ranging from 0 to 21. Scores of 0–7 indicate normal symptoms, 8–10 indicate mild symptoms, 11–14 indicate moderate symptoms, and 15–21 indicate severe symptoms.20
A Study-Specific One Week Follow-up Questionnaire was completed by participants at 1 week following the disclosure of the genetic test result. Women were asked if the genetic test result changed their surgical decision.
Medical Chart Review
A medical chart review was completed at 1 year by the study genetic counsellor. Diagnostic, pathological, and treatment data were abstracted. Data were abstracted on tumor size, axillary nodal status, estrogen receptor (ER) status, progesterone receptor (PR) status, human epidermal growth factor receptor 2 (HER2) status, initial surgery (lumpectomy, unilateral mastectomy, bilateral mastectomy), hormonal therapy, chemotherapy (yes/no), and radiotherapy (yes/no).
Statistical Analysis
The Chi-square test was used to compare frequencies of categorical variables, and the t-test was used to compare the mean values of continuous variables. The p-values in Tables 1, 2, and 3 are the test of differences between subjects with or without contralateral mastectomy. In Tables 2 and 3, we also performed tests between the two groups by adjusting some variables. All statistical tests were performed using statistical software SAS version 9.4 (TS1M3; SAS Institute, Inc., Cary, NC, USA).
Results
Study Sample
Overall, a total of 1007 women underwent rapid genetic testing for BRCA1 and BRCA2 at the time of breast cancer diagnosis. For the current analysis, we included the 850 women with a negative genetic test result. Of these 850 women with a negative BRCA result, we excluded 28 women with stage IV breast cancer and 56 women with bilateral breast cancer. A total of 766 women were included in the current analysis.
The mean age of participants was 46.2 years (range 21–82). The majority (90.8%) had a college education or higher; 71.5% were married or cohabitating; 70.5% had children; 11.2% had triple-negative breast cancer; 46.4% had positive lymph nodes; and 32% had stage I, 50.0% had stage II, and 18.0% had stage III breast cancer. The demographic and clinical characteristics of the sample are presented in Table 1. Overall, 378 women (49.3%) had breast-conserving therapy, 274 (35.8%) had unilateral mastectomy, and 114 women (14.9%) had CPM.
Demographic and Clinical Predictors
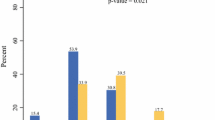
Women with CPM were significantly younger than those who did not elect for CPM (mean age 42.9 years vs. 46.8 years; p = 0.0002). Forty-three (20.9%) women aged 40 years or younger at diagnosis elected for CPM compared with 71 (12.7%) women over the age of 40 years. There were no significant differences in education (p = 0.90), marital status (p = 0.35), or having children (p = 0.66) between those with and without CPM.
Women with ER-positive tumors were more likely to have CPM compared with women with ER-negative tumors (16% vs. 8%; p = 0.01). Women with triple-negative tumors were significantly less likely to have CPM compared with women without triple-negative tumors (5.9% vs. 16.0%; p = 0.01). There were no significant differences in the uptake of CPM by stage (p = 0.94).
Psychosocial Predictors
There were no significant differences in mean scores for any of the psychosocial predictors in women who elected for or against CPM (Table 2).
Family History Predictors
Overall, 24.4% of women reported having one or more first-degree relative with breast cancer; 16.6% of women had a mother with breast cancer and 8.9% had at least one sister with breast cancer. Women who had a mother with breast cancer were significantly more likely to have a CPM compared with women without a mother with breast cancer (23.2% vs. 13.5%; p = 0.006); 29.6% of women with a mother who died of breast cancer elected for CPM, compared with 14.6% of women with a mother who had not died of breast cancer (p = 0.03). There were no significant differences in the uptake of CPM in relation to having a sister diagnosed with (p = 0.96) or dying of (p = 0.10) breast cancer.
Surgical Choices
Of the 638 women who responded to the question about surgical preference prior to surgery and genetic testing, 405 women (63.5%) were leaning against having a CPM, 70 (11.0%) were leaning towards CPM, and 163 women (25.5%) were unsure. Of the 70 women who were leaning towards CPM prior to genetic testing, 42 (60.1%) had CPM after learning of their negative BRCA genetic test. Of the 163 women who were unsure about CPM, 24 (14.7%) elected for CPM. Of the 405 women leaning against having a CPM, 29 (7.2%) elected for a CPM.
Overall, 34.0% of the women reported that their surgical decision changed after receipt of a negative genetic test result.
Discussion
In the current study, we have reported on surgical decision making in women who received genetic counseling and a negative BRCA1 and BRCA2 genetic test result at the time of breast cancer diagnosis and before surgery. Prior to genetic counseling and testing, 37% of women were unsure of or leaning towards having a CPM. However, after receipt of pre- and post-test genetic counseling, 15% of high-risk women without a BRCA1 or BRCA2 mutation elected for CPM. Forty percent of women who were planning on CPM prior to genetic testing did not have a CPM after receiving negative genetic test results. Seven percent of women who initially preferred not to have CPM did have CPM despite receiving a negative genetic test result.
We recently reported on the uptake of CPM in a large Canadian prospective cohort of women with no documented BRCA1 or BRCA2 mutation.17 The mean age of the women at breast cancer diagnosis was 55 years, and 22% of the women elected for CPM. Previous research has shown that young age is a predictor of CPM.3,4,5 The average age of women in the current study was relatively young, at 46 years. We therefore would have expected the uptake of CPM in this cohort to be higher that what has been reported in previous studies with older participants. However, in the current study where women had genetic counseling and testing and received a negative BRCA genetic test result, only 15% of the women elected for CPM despite this being a relatively young cohort.
Having a mother with breast cancer or a mother dying of breast cancer were among the most significant predictors of uptake of CPM. Thirty percent of women who had a mother who died of breast cancer elected for CPM. In most previous research, family history has been defined as yes or no, and there has not been an examination of family history with regard to specific relatives and mortality associated with the cancer in the relative.
Women who have experienced the death of a mother from breast cancer experience elevated levels of cancer-related distress and high cancer risk perception.21 For women without breast cancer, this often translates into high rates of cancer screening adherence, including mammography.22,23 Interestingly, although family history of cancer is associated with higher screening adherence, the death of a relative due to breast cancer may be a more significant predictor than a cancer diagnosis alone.24 It has been hypothesized that women with a mother who survived breast cancer may be more optimistic than women who have a mother who died of breast cancer.24 Less is known about how the death of mother from breast cancer may impact on breast cancer treatment decisions. Previous research has shown that uptake of CPM is associated with greater worry about recurrence.25 For women who witnessed a breast cancer recurrence and death in a mother, they may have greater worry about recurrence, which could explain the high uptake of CPM in this group of women.
Family history of breast cancer also impacts on women’s decision making related to preventive surgery. We have previously reported on uptake of prophylactic surgery in 517 Canadian women with a BRCA1 or BRCA2 mutation.26 Women with a first-degree relative with breast cancer were significantly more likely to elect for prophylactic mastectomy, and women with a first-degree relative with ovarian cancer were more likely to elect for prophylactic oophorectomy. Although all women with a BRCA1 or BRCA2 mutation are at a high risk of both breast and ovarian cancers, those who have not experienced a cancer diagnosis in a relative are less likely to elect for preventive surgery.
Unlike previous research, we did not observe that psychosocial functioning predicted uptake of CPM. We and others have previously reported that women who elected for CPM had higher levels of cancer worry and cancer-related distress, and lower levels of body satisfaction and optimism.16,17,27 However, in the previous studies, the women did not have genetic counseling and testing at the time of surgical decision making. There may be a role for genetic counseling at the time of breast cancer diagnosis, specifically in using genetic testing to assist women to understand their risk of a contralateral breast cancer, and also to provide psychosocial support during the treatment decision period. Christie and collegues reported that genetic counseling is associated with a decrease in distress for women with breast cancer,28 and also reported that women who had genetic counseling at the time of treatment decision making had the largest decline in distress compared with women who had genetic counseling after treatments were completed. Future research is needed to evaluate the impact of genetic counseling on psychosocial and decision outcomes in women at the time of breast cancer diagnosis.
There are limitations to the current study. Women in the current study were all recruited from academic health science centers, which may not be representative of the Canadian population, which limits the generalizability of the findings to women who are being treated in non-academic centers. In addition, all Canadian women have access to universal healthcare, therefore access to surgery is not limited as it may be in other countries, and insurance status does not have an impact on surgical choices. We did not collect data on surgeon recommendations. Furthermore, we did not have a control group and relied on historical cohorts. Studies with a control group that does not receive rapid genetic testing are needed. Furthermore, testing was limited to the analysis of the BRCA1 and BRCA2 genes. There is less evidence of the effectiveness of various treatments for women with mutations in genes other than BRCA1 and BRCA2.
Conclusion
Women who receive genetic counseling and a negative BRCA1 and BRCA2 genetic test result at the time when breast cancer treatment choices are being made use this information to inform surgical decisions. The uptake rate of 15% for CPM is lower than what has been reported previously, despite this being a young group of breast cancer patients. The American Society of Breast Surgeons has recently recommended that all women with breast cancer receive genetic testing.29 The results of this study support this recommendation, in that negative genetic test results can also be informative when making treatment decisions.
References
Boughey JC, Attai DJ, Chen SL, et al. Contralateral prophylactic mastectomy (CPM) consensus statement from the american society of breast surgeons: data on CPM outcomes and risks. Ann Surg Oncol. 2016;23:3100–5.
Wright FC, Look Hong NJ, Quan ML, et al. Indications for contralateral prophylactic mastectomy: a consensus statement using modified delphi methodology. Ann Surg. 2018;267:271–9.
Tuttle TM, Habermann EB, Grund EH, Morris TJ, Virnig BA. Increasing use of contralateral prophylactic mastectomy for breast cancer patients: a trend toward more aggressive surgical treatment. J Clin Oncol. 2007;25:5203–9.
Yao K, Stewart AK, Winchester DJ, Winchester DP. Trends in contralateral prophylactic mastectomy for unilateral cancer: a report from the National Cancer Data Base, 1998–2007. Ann Surg Oncol. 2010;17:2554–62.
Dragun AE, Pan J, Riley EC, et al. Increasing use of elective mastectomy and contralateral prophylactic surgery among breast conservation candidates: a 14-year report from a comprehensive cancer center. Am J Clin Oncol. 2013;36:375–80.
Grimmer L, Liederbach E, Velasco J, Pesce C, Wang CH, Yao K. Variation in contralateral prophylactic mastectomy rates according to racial groups in young women with breast cancer, 1998 to 2011: a report from the National Cancer Data Base. J Am Coll Surg. 2015;221:187–96.
Metcalfe K, Lynch HT, Ghadirian P, et al. Contralateral breast cancer in BRCA1 and BRCA2 mutation carriers. J Clin Oncol. 2004;22:2328–35.
Metcalfe K, Gershman S, Lynch HT, et al. Predictors of contralateral breast cancer in BRCA1 and BRCA2 mutation carriers. Br J Cancer. 2011;104:1384–92.
Metcalfe K, Gershman S, Ghadirian P, et al. Contralateral mastectomy and survival after breast cancer in carriers of BRCA1 and BRCA2 mutations: retrospective analysis. BMJ. 2014;348:g226.
Metcalfe KA, Eisen A, Poll A, et al. Rapid genetic testing for BRCA1 and BRCA2 mutations at the time of breast cancer diagnosis: an observational study. Ann Surg Oncol. 2021;28(4):2219–26.
Soran A, Kamali Polat A, Johnson R, McGuire KP. Increasing trend of contralateral prophylactic mastectomy: What are the factors behind this phenomenon? Surgeon. 2014;12:316–22.
Madlensky L, Trepanier AM, Cragun D, Lerner B, Shannon KM, Zierhut H. A rapid systematic review of outcomes studies in genetic counseling. J Genet Couns. 2017;26:361–78.
Yi M, Meric-Bernstam F, Middleton LP, et al. Predictors of contralateral breast cancer in patients with unilateral breast cancer undergoing contralateral prophylactic mastectomy. Cancer. 2009;115:962–71.
Bedrosian I, Hu CY, Chang GJ. Population-based study of contralateral prophylactic mastectomy and survival outcomes of breast cancer patients. J Natl Cancer Inst. 2010;102:401–9.
Sorbero ME, Dick AW, Beckjord EB, Ahrendt G. Diagnostic breast magnetic resonance imaging and contralateral prophylactic mastectomy. Ann Surg Oncol. 2009;16:1597–605.
Parker PA, Peterson SK, Shen Y, et al. Prospective study of psychosocial outcomes of having contralateral prophylactic mastectomy among women with nonhereditary breast cancer. J Clin Oncol. 2018;36:2630–8.
Metcalfe KA, Retrouvey H, Kerrebijn I, et al. Predictors of uptake of contralateral prophylactic mastectomy in women with nonhereditary breast cancer. Cancer. 2019;125:3966–73.
Horowitz M, Wilner N, Alvarez W. Impact of event scale: a measure of subjective stress. Psychosom Med. 1979;41:209–18.
Snaith RP, Zigmond AS. The hospital anxiety and depression scale. Br Med J. 1986;292:344.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 1983;67:361–70.
Zakowski SG, Valdimarsdottir HB, Bovbjerg DH, et al. Predictors of intrusive thoughts and avoidance in women with family histories of breast cancer. Ann Behav Med. 1997;19:362–9.
Carney PA, O’Malley JP, Gough A, et al. Association between documented family history of cancer and screening for breast and colorectal cancer. Prev Med. 2013;57:679–84.
Bostean G, Crespi CM, McCarthy WJ. Associations among family history of cancer, cancer screening and lifestyle behaviors: a population-based study. Cancer Causes Control. 2013;24:1491–503.
Tracy KA, Quillin JM, Wilson DB, et al. The impact of family history of breast cancer and cancer death on women’s mammography practices and beliefs. Genet Med. 2008;10:621–5.
Hawley ST, Jagsi R, Morrow M, et al. Social and clinical determinants of contralateral prophylactic mastectomy. JAMA Surg. 2014;149(6):582–9.
Metcalfe KA, Foulkes WD, Kim-Sing C, et al. Family history as a predictor of uptake of cancer preventive procedures by women with a BRCA1 or BRCA2 mutation. Clin Genet. 2008;73:474–9.
Parker PA, Peterson SK, Bedrosian I, et al. Prospective study of surgical decision-making processes for contralateral prophylactic mastectomy in women with breast cancer. Ann Surg. 2016;263:178–83.
Christie J, Quinn GP, Malo T, et al. Cognitive and psychological impact of BRCA genetic counseling in before and after definitive surgery breast cancer patients. Ann Surg Oncol. 2012;19:4003–11.
Manahan ER, Kuerer HM, Sebastian M, et al. Consensus guidelines on genetic testing for hereditary breast cancer from the American Society of Breast Surgeons. Ann Surg Oncol. 2019;26:3025–31.
Funding
This study was funded by a CIHR Grant awarded to KAM.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Metcalfe, K.A., Eisen, A., Poll, A. et al. Frequency of Contralateral Prophylactic Mastectomy in Breast Cancer Patients with a Negative BRCA1 and BRCA2 Rapid Genetic Test Result. Ann Surg Oncol 28, 4967–4973 (2021). https://doi.org/10.1245/s10434-021-09855-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-09855-6