Abstract
Background
Recent studies have reported a beneficial role of trastuzumab in neoadjuvant treatment (NAT) among resectable gastric cancer (GC) patients; however, the effect of adjuvant treatment (AT) combined with trastuzumab is understudied. We performed a retrospective cohort study to compare chemotherapies with or without trastuzumab among human epidermal growth factor receptor 2-positive (HER2 +) locally advanced GC patients in the AT and NAT settings, respectively.
Methods
We enrolled 208 HER2 + resected GC patients who underwent perioperative/postoperative treatment in 2010–2019 in a single-centered hospital, including 135 AT patients and 73 NAT patients. We used inverse probability of treatment weighting (IPTW) to balance potential confounding factors between the treatment groups, and estimated the treatment effect of trastuzumab. Pathological and survival outcomes were evaluated.
Results
The number of trastuzumab-exposed patients in the AT and NAT cohorts was 31 (23.0%) and 34 (46.6%), respectively. After IPTW adjustment, AT combined with trastuzumab showed a better overall survival (OS) over chemotherapy alone (p = 0.023). In IPTW-adjusted NAT analysis, trastuzumab-exposed patients had an improvement in tumor pathological regression and downstaging, with lower tumor regression grade scores (p = 0.002), ypTNM stages (p < 0.001), ypN stages (p = 0.035), and ypT stages (p < 0.001). Loss of HER2 positivity following trastuzumab treatment was observed in NAT patients; however, we did not observe any significant effect of trastuzumab on OS (p = 0.126).
Conclusions
Given the improvement in tumor regression and downstaging among NAT patients, and the OS benefit in AT patients, trastuzumab could be considered a promising treatment for locally advanced HER2 + GC patients. In particular, re-evaluation of HER2 status should be considered following NAT combined with trastuzumab.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Gastric cancer (GC), which is separated anatomically into true gastric adenocarcinomas and gastroesophageal junction (GEJ) adenocarcinomas, is one of the most common malignant tumors and one of the leading causes of cancer mortality in both China and the world.1,2 Surgery combined with either adjuvant or neoadjuvant chemotherapy is the recommended approach in the treatment of locally advanced disease, as these therapies have been shown to improve disease-free survival and overall survival (OS).3,4,-5 However, among locally advanced GC patients, the effect of the recommended treatment among locally advanced GC patients is not satisfactory enough, with a reported 5-year OS rate of 36–78%.6,7,-8 Therefore, additional treatment, such as radiotherapy, targeted treatment, or novel immune checkpoint inhibitors, is proposed as a supplement to the current therapeutic regimen in an attempt to gain further benefits.3
Human epidermal growth factor receptor 2 (HER2) is an important biomarker and critical driver of GC tumorigenesis.9 Between 10% and 20% of GC patients are HER2-positive (HER2 +).10,11 Trastuzumab, a targeted drug against HER2, can play an antitumor role by directly blocking HER2-mediated signaling pathways and indirectly inducing antibody-dependent cellular cytotoxicity.9 The international phase III Trastuzumab for Gastric Cancer (ToGA) study showed that trastuzumab combined with chemotherapy, compared with chemotherapy alone, improved the overall tumor response rate and OS among HER2 + GC patients in the advanced/metastatic setting.12,13 However, only 3% of patients included in the ToGA study were diagnosed with locally advanced GC, with evidence on HER2 + locally advanced GC remaining uncertain. Given the survival benefit of trastuzumab in the management of advanced/metastatic GC,12 it is worthwhile to evaluate the clinical effect of adjuvant and neoadjuvant trastuzumab for locally advanced GC. Some case reports14,15,16,-17 and small scale studies18,19,-20 have reported that neoadjuvant chemotherapy and trastuzumab showed a beneficial effect on tumor regression, R0 resection rate, and short-term survival. However, the treatment strategy of trastuzumab implemented in the postoperative adjuvant treatment (AT) setting only has not been reported. Furthermore, previous studies found that trastuzumab therapy could lead to a change in HER2 status, from positive to negative, in both resectable HER2 + breast cancer and metastatic GC patients.21,22,23,24,-25 However, a potential change in HER2 status following trastuzumab therapy in neoadjuvant treatment (NAT) for resectable GC remains unclear.
Statistical studies demonstrated that an inverse probability of treatment weighting (IPTW) approach exhibited higher statistical power than traditional logistic regression to control confounding factors, especially when the sample size is small.26,27 We therefore employed the IPTW method among a retrospective cohort of HER2 + locally advanced GC patients to (1) investigate the tumor pathological regression and survival probability following NAT with or without trastuzumab; and (2) compare the survival probability between patients undergoing adjuvant chemotherapy plus trastuzumab and adjuvant chemotherapy alone. In addition, we described the probability of loss of HER2 positivity after NAT combined with trastuzumab.
Methods
Patients
We retrospectively collected information of eligible locally advanced GC patients who underwent gastrectomy from 1 January 2010 to 1 December 2019, from the hospital’s patient database, which is prospectively recorded and maintained at the Gastrointestinal Cancer Center of Peking University Cancer Hospital (PUCH). The study was approved by the PUCH Ethics Committee, and all participants included in the present study provided informed consent.
A patient was included in the current study if he/she met the following criteria: (1) was diagnosed with locally advanced GC or GEJ cancer; (2) underwent gastrectomy with primary D2 lymph node dissection; (3) tested positive for HER2 immunohistochemistry (IHC) 3 + or IHC 2 + with fluorescence in situ hybridization (FISH), defined as HER2 +;11 and (4) received perioperative chemotherapy (including neoadjuvant and adjuvant chemotherapy) or postoperative adjuvant chemotherapy, with or without trastuzumab. Patients were excluded if they were (1) diagnosed with stage I or IV disease according to the 8th edition of the American Joint Committee on Cancer (AJCC) Staging Manual;28 (2) diagnosed with non-gastric adenocarcinomas before treatment; (3) experienced perioperative death (occurring within 1 month after surgery); (4) received perioperative radiotherapy, other targeted therapies except for trastuzumab, immunotherapy, or unknown/absent perioperative therapies; and (5) the patient was diagnosed with other simultaneous malignancies (Fig. 1).
In total, we identified 314 HER2 + patients who underwent surgery, from the patient database. After the exclusion procedure, 208 eligible patients were enrolled in the present study, including 135 patients undergoing adjuvant therapy (AT cohort) and 73 patients receiving NAT (NAT cohort).
Exposure, Covariates, and Outcomes
Exposure was defined as the receipt of trastuzumab by intravenous infusion during the perioperative period for at least one cycle of trastuzumab. Patients who received trastuzumab preoperatively in the NAT cohort and postoperatively in the AT cohort were included in the exposed group, while those who only underwent chemotherapy without trastuzumab were considered the control group.
Patient demographic, clinicopathological, and treatment data were obtained from the hospital’s patient database. Patient-related variables included age at diagnosis, sex, and Charlson–Deyo Comorbidity Score (0, 1, or 2 +). Clinicopathological measures assessed tumor site (GEJ or gastric primary), cancer cellular differentiation grade (poorly or not poorly), presence of signet-ring cells (yes or no), prechemotherapy TNM stage, prechemotherapy T stage, and prechemotherapy N stage. Treatment-related information took into account the number of regional lymph nodes dissected (1–14, 15–29, or ≥ 30), microscopic residual tumor status (R0 or R1 [positive resection margin]),29 and year of surgery (2010–2014 or 2015–2019). Additional information, including the number of neoadjuvant chemotherapy cycles and whether paclitaxel was introduced, was documented for NAT patients. Among NAT patients who underwent trastuzumab treatment, data on whether HER2 positivity changed and whether the regimen changed were also collected and recorded. The cTNM classification and pTNM stage were treated as the prechemotherapy TNM stage for NAT patients and AT patients, respectively.
Two types of outcomes, pathological outcomes and OS, were considered for the NAT cohort, whereas OS was the single outcome for AT patients. Pathologists evaluated resected specimens and reported pathological outcomes, which consisted of tumor regression grade (TRG; 0, 1, 2, or 3),30 ypTNM stage (0, I, II, III, or IV), ypT stage (1, 2, 3, or 4), ypN stage (0, 1, 2, or 3), and the degree of tumor downstaging (cTNM stage minus ypTNM stage; continuous value). The survival outcome was all-cause death or censorship from the date of treatment (surgery date for the AT cohort, or the date of the first chemotherapy cycle for the NAT cohort) to the date of death, loss to follow-up, or the last follow-up occasion. The most recent follow-up interview was carried out in March 20. The additional details of data collection and follow-up are provided in the electronic supplementary Methods.
Statistical Analysis
Continuous variables were summarized by means (standard deviations) or medians (interquartile ranges), and group differences were tested using t-tests or Mann–Whitney tests whenever appropriate. Categorical variables were described as frequencies (percentages), and the Chi square or Fisher’s exact tests were performed.
To minimize the effect of selection bias and balance potential confounding factors between the treatment groups, we performed the IPTW method. The IPTW model is an approach attempting to mimic a randomized situation where exposed and control groups are allocated in balance by sample weighting. Exposed and control patients in the IPTW model were weighted by the inverse probability of being assigned to the exposed and control groups based on propensity score (PS).31 We calculated the PS through multivariable logistic regression models, with variables significantly different between the control and exposed groups (p < 0.1) in the present analysis and factors that were previously reported to be significantly associated with outcomes.32
Inverse probability weights calculated from the PS were constructed for NAT and AT patients separately, as cohort sample sizes and included independent variables were different. To calculate PS in the NAT cohort, we only accounted for the number of neoadjuvant chemotherapy cycles, differentiation grade, prechemotherapy TNM stage, regimens with or without paclitaxel, tumor site, and year of surgery.30 For AT cohort, we generated the weights to balance 12 variates, including age, sex, Charlson–Deyo comorbidity score, tumor site, cancer cellular differentiation grade, signet-ring cells, prechemotherapy TNM stage, prechemotherapy T stage, prechemotherapy N stage, number of lymph nodes dissected, microscopic residual tumor, and year of surgery.33,34,-35
We computed the Kaplan–Meier curves and log-rank test based on inverse probability weights to compare OS between the trastuzumab-exposed and control groups. Furthermore, we employed inverse probability-weighted linear regression, weighted ordinal logistic regressions, and weighted Cox proportional hazard regression to estimate the treatment effect of trastuzumab on continuous outcome (tumor downstaging degree), ordinal categorical outcomes (ypTNM, ypT, and ypN stage), and time-to-event outcome (OS). Time since treatment (in months) was used as the time scale in Cox regression. We further performed subgroup analyses to investigate the IPTW-adjusted hazard ratio (HR) in subcohorts stratified by AT patients’ tumor location, pT stage, pN stage, differentiation grade, microscopic residual tumor, and the year of surgery. The robustness of the IPTW model was tested in the sensitivity analyses by performing conventional multivariate analysis and PS matching (PSM) analysis. Statistical analyses were performed using R software version 3.6.0 (The R Foundation for Statistical Computing, Vienna, Austria), with a two-sided p value < 0.05 defined as a statistical significance level.
Results
Patient Characteristics
Among 208 included patients, 104, 31, 39, and 34 patients underwent a treatment of AT without trastuzumab, AT with trastuzumab, NAT without trastuzumab, and NAT with trastuzumab, respectively (Fig. 1). Table 1 shows patient-, tumor-, and treatment-related characteristics of the unweighted sample, by treatment groups. Among the AT patients, there were 135 HER + GC patients with an average age of 62.0 years, of whom 78.5% were male. The AT trastuzumab-exposed group displayed a higher proportion of patients with a pT1-2 stage (p = 0.026) and those who received surgery between 2015 and 2019 (p = 0.002), relative to the control group.
In the NAT cohort, 84.6% were males and the average age was 61.6 years. Compared with patients in the control group (NAT without trastuzumab), trastuzumab-exposed patients were more likely to undergo higher numbers of chemotherapy cycles (p = 0.002). Furthermore, a greater proportion of trastuzumab-exposed patients were treated in the more recent time period, i.e. 2015–2019 (p < 0.001).
To balance baseline characteristics between the exposed and control groups, we weighted each subject by their inverse probability of treatment. After being weighted, all significant differences observed in the unweighted AT cohorts between the control and exposed groups no longer existed (electronic supplementary Table S1). Electronic supplementary Table S2 displays the covariate differences among the NAT patients after IPTW adjustment. Similarly, no covariates between the two NAT groups were significantly different after being weighted.
Survival Outcome in the Adjuvant Treatment Cohort
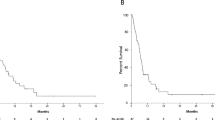
The median follow-up time for the whole, control, and exposed AT cohorts was 43.9, 46.7, and 28.5 months, respectively. The crude rates at the 3rd and 5th year were 85.9% and 76.4%, respectively, among the trastuzumab-exposed patients, and 69.6% and 58.8%, respectively, among patients in the control group. After IPTW adjustment, 3- and 5-year OS rates were 87.6% and 84.1%, respectively, in the exposed group, which was significantly better than 71.7% and 58.7%, respectively, in the control group (weighted HR [wHR] 0.24, 95% confidence interval [CI] 0.07–0.82; p = 0.023). Figure 2a shows the Kaplan–Meier survival curves of OS before and after IPTW-adjusted analysis in AT patients. We checked the results using multiple procedures. Similar results (HR < 1) are reported in electronic supplementary Table S3, which indicated a protective effect was consistent across different methods regardless of the relatively small samples.
Kaplan–Meier survival curves of overall survival before and after the IPTW analysis among HER2 + gastric cancer patients with (a) AT and (b) NAT. IPTW inverse probability of treatment weighting, HER2 +human epidermal growth factor receptor 2-positive, AT adjuvant treatment, NAT neoadjuvant treatment
To test the robustness of our findings, we further performed subgroup analyses to investigate the IPTW-adjusted HR in subcohorts. We found that the effect of trastuzumab was mostly consistent across subgroups stratified by tumor site, differentiation grade, pT stage, pN stage, and microscopic residual tumor status (electronic supplementary Fig. S1).
Pathological and Survival Outcomes in the Neoadjuvant Treatment Cohort
We found that trastuzumab-exposed patients showed better short-term pathological outcomes with respect to tumor regression and downstaging. Patients taking trastuzumab harbored lower TRG scores (weighted odds ratio [wOR] 0.35, 95% CI 0.15–0.79; p = 0.013), lower ypN stages (wOR 0.10, 95% CI 0.04–0.23; p < 0.001), lower ypTNM stages (wOR 0.23, 95% CI 0.05–0.86; p = 0.035), lower ypT stages (wOR 0.12, 95% CI 0.05–0.26; p < 0.001), and higher degrees of tumor downstaging (weighted β 1.08, 95% CI 0.62–1.54; p < 0.001) (Table 2). Among the 34 trastuzumab-exposed NAT patients, 23 patients re-evaluated their HER2 status, six patients did not have their HER2 status re-evaluated, and five patients achieved a complete pathomorphological response (TRG0) and were not able to re-evaluate their HER2 status (Table 3). Of the 23 patients who re-evaluated their HER2 status after treatment, six (26.9%) lost HER2 positivity, and only one patient stopped anti-HER2 treatment due to the loss of HER2 positivity.
The median follow-up time for all patients, control patients, and trastuzumab-exposed NAT patients was 31.0, 45.3, and 26.4 months, respectively. In respect of long-term survival outcomes, we did not observe any significant evidence (wHR 0.38, 95% CI 0.10–1.57; p = 0.126) after IPTW adjustment (Fig. 2b). Electronic supplementary Table S3 lists the pathological and survival results of sensitivity analyses, showing consistent results after using different strategies to control group imbalance.
Discussion
We retrospectively evaluated the effect of trastuzumab among locally advanced HER2 + GC patients who underwent AT and NAT. Adjuvant chemotherapy in combination with trastuzumab was associated with a 76% (1-wHR) decreased risk of mortality compared with chemotherapy alone. Neoadjuvant chemotherapy with trastuzumab increased the possibility of tumor regression response by a factor of 4 (1/wOR), and trastuzumab-exposed patients were more likely to report a lower ypT, ypN, and ypTNM stage compared with traditional neoadjuvant chemotherapy. Moreover, 26.9% of patients who received neoadjuvant trastuzumab lost HER2 positivity, suggesting a re-evaluation of HER2 status after NAT with trastuzumab. The present study provided promising evidence to support trastuzumab use in the adjuvant and neoadjuvant therapy settings for locally advanced GC.
Postoperative chemotherapy has become a standard treatment for curatively D2-resected GC in east Asia since the ACTS-GC and CLASSIC trials reported the superiority of adjuvant chemotherapy in improving survival outcomes compared with surgery alone.8,36 Furthermore, the ToGA trial also observed the protective effect of trastuzumab in combination with chemotherapy on survival among HER2 + advanced GC patients.12 However, the evidence of adjuvant chemotherapy plus trastuzumab in the treatment of resectable GC after D2 dissection is still lacking, especially in East Asian countries where curative D2 resection plus postoperative therapy is popular. The present study enrolled GC patients with D2 dissection and evaluated the effect of trastuzumab in the postoperative AT setting. We found that trastuzumab plus chemotherapy could significantly improve the survival outcome among locally advanced GC patients. The survival rates of the adjusted AT control group at the 3rd and 5th years were 71.7% and 58.7%, respectively. In contrast, the trastuzumab-exposed group in the adjusted AT cohort was associated with a 76% decreased risk of death, with 3- and 5-year survival rates of 87.6% and 84.1%, respectively. Our results provided the first direct evidence for the effect of postoperative therapy with additional trastuzumab for locally advanced GC after D2 lymph node dissection.
Subgroup analyses tested the robustness of our findings in the IPTW-adjusted AT cohort. The results showed that HR values were still < 1 across subgroups stratified by tumor site, differentiation grade, pT stage, pN stage, and microscopic residual tumor status. Interestingly, we found that HER2 + GC patients with higher pT, pN, and pTNM stages might have a higher possibility of benefiting from adjuvant therapy containing trastuzumab (electronic supplementary Fig. S1). However, since each subgroup only included a limited number of patients, such findings need to be verified and supported by future studies.
Moreover, we performed a sensitivity analysis by using multiple statistical methods, such as multiple regression and PSM. Compared with conventional multivariate analysis and PSM, IPTW tends to report a result with a similar point estimate but a narrower CI (electronic supplementary Table S3), which suggests the robustness of our results and the advantage of using the IPTW method in a study with a small sample size.
Besides the protective effect of trastuzumab on survival in the AT group, we also found the advantageous effect of trastuzumab on tumor regression and downstaging among NAT patients, which is in line with recent studies.19,20 Tong et al. reported that the transition probability from cN + to ypN0 was 53.8% in the group with trastuzumab plus chemotherapy; at the same time, the rate was only 35.7% in the group with chemotherapy20. Similarly, we also found the addition of trastuzumab to NAT contributed to the decrease in ypN stage, with 50% ypN0 stage in the trastuzumab-exposed group and 23.1% in the control group. Furthermore, in our study, 50% of patients receiving traditional neoadjuvant chemotherapy in the control group had TRG 3, comparable with a previous report on preoperative chemotherapy among 480 surgical patients with GC,37 which found that more than 50% of patients treated with neoadjuvant chemotherapy had either a minimal or no pathological response (TRG 3) to this treatment. In contrast, we found that neoadjuvant chemotherapy with trastuzumab increased the possibility of tumor regression response by a factor of 4, with only 25% remaining as TRG 3 and 25% achieving TRG 0 or 1. This finding was in agreement with a recent report from the multicenter, randomized, controlled, PETRARCA clinical trial (NCT02581462),20 in which the addition of anti-HER2 antibodies to neoadjuvant chemotherapy significantly improved the pathological complete response rate compared with chemotherapy alone.
Even though trastuzumab presented benefits regarding a tumor’s pathological regression, we did not observe statistically significant evidence on the survival outcome, partly due to the relatively small sample size and short follow-up time (median: 31 months). Similarly, the study by Tong et al. and the PETRARCA trial reported the short-term benefits on tumor pathological response, but no survival benefit, with a median follow-up of 24.3 and 22.0 months, respectively.19,20 Since the two studies, along with our results, suggested a higher survival rate among the trastuzumab group near the end of the follow-up period, it is possible that trastuzumab could influence the long-term survival outcome. Further investigations with a large sample size or longer follow-up time are needed to elucidate the effect of trastuzumab on long-term survival outcomes within the NAT strategy.
Interestingly, we found an occurrence of loss of HER2 positivity in the trastuzumab-exposed NAT group, which indicated that the HER2 amplification clone might have been eliminated after NAT, resulting in resistance to trastuzumab. In the present clinical practice as well as the above trials, not all HER2 + patients underwent a re-evaluation of HER2 status. Moreover, only 16.7% of patients with loss of HER2 positivity changed the regimen according to the results of re-evaluation. Currently, the preoperative use of trastuzumab among GC patients is dependent on the HER2 status of the primary tumor at initial diagnosis. The same postoperative therapy would often be maintained, with an assumption that the pre-and postoperative HER2 status is stable. However, our findings cast doubt on the stability of HER2 status. Our results recommended a re-evaluation of HER2 status using surgical specimens after NAT with trastuzumab, and a subsequent adjustment to the anti-HER2 postoperative treatment strategy when loss of HER2 positivity is observed.
This study has several limitations. First, the present sample size was relatively small, which limited us to detect trastuzumab effects in subgroups and effects in small magnitudes. As the prevalence of HER2 positivity among GC patients is only approximately 10–20%, it is challenging to enroll many resectable HER2 + GC patients. Our sample size is by far the largest examining the trastuzumab effect among resectable HER2 + GC patients within the AT setting. Furthermore, to decrease the influence due to the small sample size, we used an IPTW adjustment based on the PS, which has the potential advantage of retaining all the samples over matched-pairs analyses. Second, inherent selection bias and limited information exist on account of the retrospective nature of this study. We obtained limited data on the toxicity of trastuzumab and time to recurrence, which could better explain the safety and prognosis of trastuzumab. Despite these problems, we thought this study had its merit, as we included a relatively large number of HER2 + GC resectable patients, provided the first evidence on AT containing trastuzumab for GC, and made use of the IPTW method to balance the treatment factors.
Conclusions
Given the improved pathological outcomes of tumor regression and downstaging in the NAT group, and the survival benefit among AT patients, trastuzumab could be considered a promising treatment for patients diagnosed with HER2 + locally advanced GC. As loss of HER2 positivity was observed, we recommend a re-evaluation of HER2 status using surgical specimens following NAT with trastuzumab. Prospective studies with a longer follow-up and large sample sizes are still warranted to validate these findings and guide the use of trastuzumab in the treatment for locally advanced GC.
References
Freddie B, Jacques F, Isabelle S, Rebecca LS, Lindsey AT, Ahmedin J. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;6:394–424.
Lei Y, Rongshou Z, Ning W, et al. Incidence and mortality of stomach cancer in China, 2014. Chin J Cancer Res. 2018;3:291–8.
Hiroyuki A, Takako EN. Recent developments of systemic chemotherapy for gastric cancer. Cancers. 2020;5:10–3390.
Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2018 (5th edition). Gastric cancer. Epub 14 Feb 2020. https://doi.org/10.1007/s10120-020-01042-y.
National Health Commission of the People’s Republic of China. Chinese guidelines for diagnosis and treatment of gastric cancer 2018 (English version). Chin J Cancer Res. 2019;5:707–37.
Eric VC, Xavier S, Baki T, Karin H, Hans P. Gastric cancer. Lancet. 2016;388(10060):2654–2664.
Cunningham D, Allum WH, Stenning SP, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med. 2006;355(1):11–20.
Sung HN, Sook RP, Han-Kwang Y, et al. Adjuvant capecitabine plus oxaliplatin for gastric cancer after D2 gastrectomy (CLASSIC): 5-Year follow-up of an open-label, randomised phase 3 trial. Lancet Oncol. 2014;12:1389–96.
Gravalos C, Jimeno A. HER2 in gastric cancer: A new prognostic factor and a novel therapeutic target. Ann Oncol. 2008;9:1523–9.
Rüschoff J, Hanna W, Bilous M, et al. HER2 testing in gastric cancer: A practical approach. Mod Pathol. 2012;5:637–50.
Hofmann M, Stoss O, Shi D, et al. Assessment of a HER2 scoring system for gastric cancer: Results from a validation study. Histopathology. 2008;7:797–805.
Bang YJ, Van Cutsem E, Feyereislova A, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): A phase 3, open-label, randomised controlled trial. Lancet. 2010;376(9742):687–97.
Kurokawa Y, Sugimoto N, Miwa H, et al. Phase II study of trastuzumab in combination with S-1 plus cisplatin in HER2-positive gastric cancer (HERBIS-1). Br J Cancer. 2014;5:1163–8.
Sueoka S, Ito A, Kawanishi J, Sakakima Y. A case of gastric cancer that responded to a preoperative combination therapy of S-1/CDDP plus trastuzumab. Gan To Kagaku Ryoho. 2014;9:1155–7.
Nishino M, Hosoda Y, Okano M, et al. A case of HER2-Positive advanced gastric cancer with a pathological complete response to neoadjuvant chemotherapy with S-1/CDDP/Trastuzumab. Gan To Kagaku Ryoho. 2015;12:2043–5.
Kanaya N, Arata T, Tanakaya K, Yamasaki R, Aoki H, Takeuchi H. A case of HER2-positive esophagogastric junction cancer treated by using a neoadjuvant chemotherapy regimen consisting of trastuzumab [in Japanese]. Gan To Kagaku Ryoho. 2014;41(12):2285–6.
Wang J, Saukel GW, Garberoglio CA, Srikureja W, Hsueh CT. Pathological complete response after neoadjuvant chemotherapy with trastuzumab-containing regimen in gastric cancer: A case report. J Hematol Oncol. 2010;3:31.
Hoffmann-La Roche. An open-label, multicenter study to evaluate the disease free survival rate of a perioperative combination of capecitabine (Xeloda), trastuzumab (Herceptin) and oxaliplatin (XELOX-trastuzumab) in patients with resectable gastric or gastroesophageal junction adenocarcinoma. (2015). Available at: https://clinicaltrials.gov/ct2/show/study/NCT01130337. Accessed 3 Sep 2020.
Gangling T, Shuluan L, Lin L, et al. Trastuzumab with FLOT regimen for the perioperative treatment of resectable HER2 + advanced gastric cancer: A retrospective study. Cancer Manag Res. 2020;12:2481–2489.
Hofheinz RD Haag GM, Ettrich TJ, et al. Perioperative trastuzumab and pertuzumab in combination with FLOT versus FLOT alone for HER2-positive resectable esophagogastric adenocarcinoma: Final results of the PETRARCA multicenter randomized Phase II trial of the AIO. J Clin Oncol. 2020;38 Suppl. 15:4502.
Pietrantonio F, Caporale M, Morano F, et al. HER2 loss in HER2-positive gastric or gastroesophageal cancer after trastuzumab therapy: implication for further clinical research. Int J Cancer. 2016;12:2859–64.
Seo S, Ryu M, Park YS, et al. Loss of HER2 positivity after anti-HER2 chemotherapy in HER2-positive gastric cancer patients: Results of the GASTric cancer HER2 reassessment study 3 (GASTHER3). Gastric Cancer. 2019;3:527–35.
Ishimine Y, Goto A, Watanabe Y, et al. Loss of HER2 positivity after trastuzumab in HER2-Positive gastric cancer: Is change in HER2 status significantly frequent? Case Reports in Gastrointestinal Medicine. 2015;2015:132030.
Guarneri V, Dieci MV, Barbieri E, et al. Loss of HER2 positivity and prognosis after neoadjuvant therapy in HER2-positive breast cancer patients. Ann Oncol. 2013;12:2990–4.
Kijima T, Arigami T, Uenosono Y, et al. Comparison of HER2 status before and after trastuzumab-based chemotherapy in patients with advanced gastric cancer. Anticancer Res. 2020;40(1):75–80.
Pirracchio R, Resche-Rigon M, Chevret S. Evaluation of the propensity score methods for estimating marginal odds ratios in case of small sample size. BMC Med Res Methodol. 2012;12:70.
Cepeda MS, Boston R, Farrar JT, Strom BL. Comparison of logistic regression versus propensity score when the number of events is low and there are multiple confounders. Am J Epidemiol. 2003;3:280–7.
Jaffer AA, Haejin I, Takeshi S, et al. Stomach. In: Mahul BA (ed). AJCC Cancer Staging Manual. 8th ed. New York: Springer; 2016. pp. 203–215.
Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;2:101–12.
Becker K, Langer R, Reim D, et al. Significance of histopathological tumor regression after neoadjuvant chemotherapy in gastric adenocarcinomas: A summary of 480 cases. Ann Surg. 2011;253(5):934–9.
Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;28:3661–79.
Lonjon G, Porcher R, Ergina P, Fouet M, Boutron I. Potential pitfalls of reporting and bias in observational studies with propensity score analysis assessing a surgical procedure: A methodological systematic review. Ann Surg. 2017;265(5):901–909.
Piessen G, Messager M, Leteurtre E, Jean-Pierre T, Mariette C. Signet ring cell histology is an independent predictor of poor prognosis in gastric adenocarcinoma regardless of tumoral clinical presentation. Ann Surg. 2009;6:878–87.
Bollschweiler E, Breckheimer S, Monig SP, Holscher AH. The prognostic relevance of age and comorbidity in patients with resected gastric cancer. Zentralbl Chir. 2009;1:71–6.
van den Ende T, Ter Veer E, Mali R, et al. Prognostic and predictive factors for the curative treatment of esophageal and gastric cancer in randomized controlled trials: a systematic review and Meta-Analysis. Cancers (Basel). 2019;11(4):530.
Sakuramoto S, Sasako M, Yamaguchi T, et al. Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. N Engl J Med. 2007;18:1810–20.
Becker K, Mueller JD, Schulmacher C, et al. Histomorphology and grading of regression in gastric carcinoma treated with neoadjuvant chemotherapy. Cancer-Am Cancer Soc. 2003;7:1521–30.
Acknowledgements
The authors thank all of the patients, their families, and medical staff members, especially the radiologists, who participated in this study.
Funding
This study was supported by the Peking University Clinical Scientist Program (BMU2019LCKXJ011), San Ming Project of Shenzhen city, China (No. SZSM201612051), National Science Foundation for Young Scientists of China (81802735), and China Postdoctoral Science Foundation (2019M650399).
Author information
Authors and Affiliations
Contributions
Conceptualization: QH, ZB, and JJ. Data collection and check: JC, CJ, and KZ. Methodology: QH, JC, and XL. Formal analysis and investigation: QH, KZ, AW, XJ, and KJ. Writing—original draft preparation: QH and XL. Writing—review and editing: XJ, JC, ZB, and JJ. Funding acquisition: QH, AW, and JJ. Resources: QH, JZ, and XW. Validation: JZ, and XW. Supervision: ZB and JJ.
Corresponding authors
Ethics declarations
Disclosure
Qifei He, Jiahui Chen, Kai Zhou, Chenggen Jin, Anqiang Wang, Ke Ji, Xin Ji, Ji Zhang, Xiaojiang Wu, Xia Li, Zhaode Bu, and Jiafu Ji report no potential conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
He, Q., Chen, J., Zhou, K. et al. Effect of Additional Trastuzumab in Neoadjuvant and Adjuvant Treatment for Patients with Resectable HER2-Positive Gastric Cancer. Ann Surg Oncol 28, 4413–4422 (2021). https://doi.org/10.1245/s10434-020-09405-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09405-6