Abstract
Purpose
Trastuzumab plus chemotherapy is an effective therapy in HER2 positive advanced gastric cancer (AGC). However, the clinicopathologic factors that predict the outcome of routine trastuzumab therapy remain unclear.
Methods
The outcome and safety profile of trastuzumab therapy in untreated HER2 positive AGC was evaluated in this prospective observational study. Clinical and pathological data including demographics, treatment profiles, expression level of HER2 were analyzed to identify predictive factors of trastuzumab-based first-line therapy for their progression-free survival (PFS).
Results
Overall, 107 patients were eligible. The median number of treatment cycles was 9 (range 1–44), the median PFS and median overall survival (OS) were 7.7 months (95% CI 6.5–8.9) and 16.0 months (95% CI 13.2–18.8), respectively. The confirmed response rate was 58.9%, and the disease control rate was 82.2%. Patients with liver metastasis (HR 1.616) and poor performance status (PS, HR 2.518) were independently associated with a worse PFS, while the other clinicopathological factors including demographics, treatment profiles and some other clinical characteristics did not predict the survival.
Conclusions
In routine clinical practice, the addition of trastuzumab to chemotherapy was effective and safe in real-world setting in Chinese patients with HER2 positive AGC, regardless of most of the clinicopathological factors. Further studies are needed to improve the prognosis of HER2 positive patients with liver metastasis or poor PS.
Trial Registration clinicaltrials.gov Identifier: NCT03024450
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer is one of the leading causes of cancer-related death worldwide [1]. More than 70% cases occur in developing countries, and 50% new cases originate in eastern Asia (mainly in China) [2]. Human epidermal growth factor receptor-2 (HER2) overexpression/amplification is accounted for 6.0–29.5% in advanced gastric cancer [3,4,5,6,7]. Trastuzumab is a humanized monoclonal antibody that targets HER2. The ToGA study demonstrated the beneficial effect of trastuzumab in gastric cancer patients with HER2 overexpressing tumors: the addition of trastuzumab resulted in a longer overall survival (OS, 13.8 months versus 11.1 months) and progression-free survival (PFS, 6.7 months versus 5.5 months) than cisplatin plus capecitabine or fluorouracil [3]. In the subgroup analysis of ToGA study, adding trastuzumab significantly improved OS of 16.0 months in patients with HER2 immunohistochemistry (IHC) 3+ or IHC 2+ plus the positive result of fluorescence in situ hybridization (FISH); it was more prominent than the whole patients. Trastuzumab in combination with other chemotherapy regimen was also effective [6, 8,9,10,11]. According to the different studies available, the median PFS ranged from 6.7 to 9.8 months and median OS was from 11.8 to 24.7 months [6, 8,9,10,11]. It implies that a different regimen or characteristic feature may affect the outcome in trastuzumab-treating patients. The valid predictive factors of trastuzumab treatment are still unknown.
The purpose of this study was to identify predictive factors affecting the PFS in AGS patients with high level of HER2 who received trastuzumab-based first-line therapy, as well as to evaluate the efficacy and safety of trastuzumab.
Patients and methods
Patients
From January 2012 to December 2016, patients diagnosed with HER2 positive advanced or metastatic gastric adenocarcinoma in Shanghai Zhongshan Hospital, Fudan University were prospectively collected. HER2 expression was assessed by IHC first. In the cases with IHC 2+, fluorescence in situ hybridization (FISH) was used to detect HER2/neu amplification levels. HER2 status was determinate according to the gastric cancer scoring system for HER2 [12]. Due to the subset analysis of ToGA study patients, only patients with high levels of HER2 expression (IHC 3+ or IHC 2+ plus FISH positive) were eligible in this study. The additional principal inclusion criteria were as follows: (1) pathology and medical imageology proven advanced gastric adenocarcinoma, inoperable; (2) received trastuzumab plus chemotherapy as the first-line palliative chemotherapy; (3) with measurable lesion with a diameter more than 20 mm using conventional computed tomography (CT) or magnetic resonance imaging (MRI) scans or 10 mm using spiral CT scans; (4) Eastern Cooperative Oncology Group performance status (ECOG PS) of 0–2; (5) left ventricular ejection fraction(LVEF) more than 50 percent; (6) sufficient bone marrow, liver and renal function. The main exclusion criteria included: (1) received previous systemic therapy for advanced disease (except adjuvant/neoadjuvant chemotherapy completed at least 6 months before enrollment); (2) trastuzumab-based adjuvant/neoadjuvant therapy; (3) treatment with any other anticancer therapy (lapatinib, immunotherapy, etc.); (4) patients with heart failure, coronary artery disease or myocardial infarction within the previous 6 months. (5) Trastuzumab-based first-line therapy started beyond 4 weeks from the first diagnosis of AGC.
Treatment
Trastuzumab was administrated every 3 weeks with a dose of 6 mg/kg (8 mg/kg for first dose). There were no protocol-specified chemotherapy regimens. Fluoropyrimidine (5-FU, S1 or capecitabine), platinum (cisplatin or oxaliplatin), taxane (docetaxel or paclitaxel), irinotecan were allowed to be used as the first-line chemotherapy for the AGC in our study. If LVEF was below 45% and dropped by ten points from baseline or LVEF was below 40%, trastuzumab was withheld and an extra LVEF assessment was performed after 3 weeks. Trastuzumab was discontinued permanently if the following occurred: LVEF did not recover to 45% or 40–45% but dropped within ten points in 3 weeks, symptomatic significant heart failure, and severe infusion reactions. Dosage adjustment and treatment delay were also made by the physician as usual clinical practice if the toxicities were mainly caused by chemotherapy, but trastuzumab was administrated as scheduled.
All patients have signed written informed consents in our study. This study was approved by the Research Ethics Committees of Zhongshan hospital, Fudan University.
Follow-up and evaluation
Clinical and pathological characteristics including age, gender, tumor location, ECOG PS, Lauren classification, previous gastrectomy, metastasis and first-line treatment were collected at baseline, while toxicity according to version 4.0 of Common Terminology Criteria for Adverse Events (AEs) was recorded at every cycle. Patients received CT/MRI for response evaluation every 9 weeks according to Response Evaluation Criteria in Solid Tumors (RECIST) (version 1.1) or earlier if there were indications of treatment failure. LVEF was assessed at baseline and at least every 12 weeks.
OS was defined as time from the beginning of first-line therapy to death; PFS was measured from the start of first-line therapy to the date of progressive disease or death, with censoring of patients who were lost to follow-up. Response rate (RR) was defined as complete response (CR) plus partial response (PR); disease control rate (DCR) was defined as CR plus PR plus stable disease (SD). CR and PR were confirmed > 4 weeks after the initial identification of response. All patients were followed up every three months after disease progression (PD). The last date of follow-up was 20th June, 2017.
Statistical analysis
Statistical analyses were performed with SPSS 16.0 statistical software (IBM SPSS Statistics, Chicago, IL, USA). PFS and OS curve was estimated by the Kaplan–Meier method. Clinicopathologic factors and variables of treatment information were evaluated by univariate analysis using the log-rank test and a multivariate analysis using a Cox proportional hazards model and presented as an HR and a 95% CI. Differences between values were regarded as statistically significant if the P value was less than 0.05.
Results
Patients and characteristics
A total of 136 HER2 positive AGC were registered and 107 patients were eligible. The consort diagram was summarized in Fig. 1. The median age was 64 years (range 26–87). 95 patients (88.8%) received platinum plus fluoropyrimidine (FP) or taxane plus fluoropyrimidine (DF) as the first-line chemotherapy. In other patients, two patients were treated with irinotecan plus cisplatin, and ten patients received mono-chemo-agent therapy. Patients’ baseline characteristics including demographics, treatment profiles, and clinical characteristics were shown in Table 1.
Efficacy and multivariate analysis
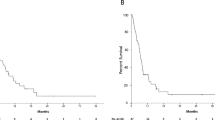
At the last patient visit, the disease had progressed in 96 patients. Among them, 83 patients died of disease progression. The median number of treatment cycles given was 9 (range 1–44, total 1104 cycles) and the median follow-up time was 14.0 months, with a median PFS of 7.7 months (95% CI 6.5–8.9, Fig. 2a) and a median OS was 16.0 months (95% CI 13.2–18.8, Fig. 2b). The confirmed response rate was 58.9% and the disease control rate was 82.2%: 3 CR (2.8%), 60 PR (56.1%), 25 SD (23.4%), and 19 PD (17.8%).
Kaplan–Meier curves of progression-free survival and overall survival in patients. a Kaplan–Meier curves of progression-free survival in all enrolled patients. b Kaplan-Meier curves of overall survival in all enrolled patients. c PFS in patients with liver metastasis (liver +), and without liver metastasis (liver−). d PFS in patients with ECOG PS 0–1, and PS 2
Univariate analyses were performed to determine the independent influences of gender, age, ECOG PS, HER2 expression level, metastasis status, chemotherapy regimen and other characteristic features on PFS. The results showed that only ECOG PS (P < .001), and liver metastasis (P = .003) were related to the prognosis. PFS was significantly prolonged in patients without liver metastases (12.0 months versus 7.0 months for patients with liver metastases, Fig. 2c) and patients with ECOG PS 0–1 (9.0 months versus 4.0 months for ECOG PS 2, Fig. 2d). The P values for metastasis and ECOG PS in the multivariate analysis were .044 (HR 1.616, 95% CI 1.014–2.577) and .000 (HR 2.518, 95% CI 1.522–4.167), which were therefore also the independent factors influencing PFS.
Whether it was platinum plus fluoropyrimidine or taxane plus fluoropyrimidine, different standard chemotherapy regimens made no difference of efficacy for HER2 positive AGC based on trastuzumab first-line therapy. There were 88 patients who did not have disease progression after six cycles of initial treatment. Among them, 40 patients switched to maintenance therapy of trastuzumab alone and other 48 patients received trastuzumab plus chemotherapy. Further analysis was carried out in these patients and the median PFS of trastuzumab maintenance therapy was similar with trastuzumab plus chemotherapy (7.3 months versus 8.0 months, P = 0.625, Fig. 3a). The same result was obtained in OS analysis (16.0 months versus 17.8 months, P = 0.946, Fig. 3b).
Kaplan–Meier curves of progression-free survival and overall survival in patients with different therapy. a PFS in patients who received maintenance trastuzumab without chemotherapy (H), and those who received trastuzumab with chemotherapy (CT + H). b OS in patients who received maintenance trastuzumab without chemotherapy (H), and those who received trastuzumab with chemotherapy (CT + H)
Safety
The incidences of hematological and non-hematological adverse events (AEs) were shown in Table 2. The leucopenia/neutropenia and anorexia were the most common hematological and non-hematological AEs, respectively. Three patients experienced grade 1/2 infusion reaction related to trastuzumab when they accepted the first trastuzumab infusion, one patient stopped trastuzumab therapy due to asymptomatic left ventricular ejection fractions. No heart failure, arrhythmia or any other cardiac adverse event occurred. There was no treatment-related death in this observational study. All the AEs are reversible.
Discussion
This was the first study to analyse the prognostic factor in HER2 positive AGC treated with trastuzumab in real-world setting in China. In our study, median PFS (7.7 months) and OS (16.0 months) was comparable with the results of the subgroup with high HER2 expression analysis in ToGA and the study reported by Kurokawa et al. that verified the high efficacy of trastuzumab in the clinical practice of Chinese population [3, 10].
Compared with breast cancer, fewer patients presented HER2 overexpression in gastric cancer. HER2 overexpressed more frequently in patients with these characteristics: male agenda, esophageal gastric junction adenocarcinoma or with intestinal type [13,14,15]. Elevated serum carcinoembryonic antigen concentration, differentiated histology, pulmonary metastasis, and distant lymph node metastasis were significant predictive factors for HER2 positivity in recurrent or metastatic disease [16]. However, whether these clinicopathological factors associated with HER2 positivity also have the prognostic significance on anti-HER2 therapy in gastric cancer continue to be an issue of debate. So, we conducted univariate and multivariate analyses to identify the predictor in trastuzumab-treated patients.
Our study showed poor ECOG PS and liver metastasis associated with poor outcome in trastuzumab therapy, while other factors such as old age, gastrectomy, peritoneal metastases, small number of metastasis which were predictors of prognosis in AGC did not influence the outcome in HER2 positive AGC [17,18,19,20]. Further analysis also demonstrated that median OS in patients with ECOG PS ≤ 1 (17.8 months versus 8.0 months, P = 0.000) or patients without liver metastasis (24 months versus 14 months, P = 0.007) were more longer than those with ECOG PS = 2 or liver metastasis. Liver metastasis was more common in HER2 positive AGC and HER2 was a predictor of worse survival in AGC with liver metastasis [21, 22]. In ToGA study, patients with visceral metastasis (including liver) benefit less from trastuzumab [3]. But it did not indicate that trastuzumab was totally ineffective in these patients. Takuya Saito’s study found that HER2 positivity of the primary tumor and liver metastases had good concordance in patients with liver metastases. It suggested liver metastasis was a potential target for anti-HER2 molecular therapy [23]. Moreover, our previous study demonstrated that adding trastuzumab to chemotherapy could significantly reverse the poor prognosis in HER2 positive AGC with liver metastasis patients [24]. Recently, a randomized phase III study was designed to investigate whether high-dose trastuzumab improved the OS compared with standard dosing regimen in patients with risk factors associated with more rapid disease progression and/or shorter survival duration. The main inclusion criteria included ECOG PS 2, at least two organs involved in metastatic gastric tumor (at least lung or liver or both), no prior gastrectomy. However, high-dose regimen failed to show the benefits on OS [25]. Thus, much more attempts were warranted to improve the prognosis in patients with liver metastasis or ECOG 2.
We retrospectively reviewed the FISH status in patients with HER2 IHC 3+ after our study. All patients with IHC 3+ were FISH +. There was no statistical significance of PFS (7.7 months vs. 7.5 months) or OS (17.8 months vs. 15.0 months) in 70 patients with HER2 IHC 3 +/FISH + and 37 patients with IHC 2 +/FISH + (Fig. 4). The previous studies showed that HER2 expression was the independent prognostic biomarker [3, 8, 26, 27], which seemed to be in conflict with ours. Actually, there was a portion of enrolled patients with low HER2 expression (IHC +/FISH +) in those studies [3, 8, 26]. Gomez et al. reported that HER2 positive patients with HER2 IHC 3+ showed significantly longer OS than patients with HER2 ≤ 2+. Further analysis in that study demonstrated HER2/CEP 17 ratio ≥ 4.48 was the optimal cutoff value for predicting longer OS in patients treated with trastuzumab [26]. Patients with a HER2/CEP 17 ratio greater than 5 also achieved better OS in GCOG1001 study [8]. Considering our results, HER2 gene amplification level instead of IHC level might be an appropriate predictive factor for response to trastuzumab-based treatment and survival benefit in patients with HER2 high expression.
Trastuzumab in combination with chemotherapy was the standard therapy for HER2 positive AGC. New chemotherapy agents such as S1, capecitabine, paclitaxel, docetaxel was more effective or less toxicity than the chemotherapy regimen in ToGA. Trastuzumab combined with XELOX/SP/cisplatin has been reported as an effective first-line therapy for HER2 positive AGC in some phase II clinical trials [8,9,10,11]. Therefore, chemotherapy was not confined to a certain regimen in this observational study. To find out the optimal regimen with trastuzumab, we evaluated the efficacy of different regimens by univariate analysis. The result showed similar outcomes in patients treated with different chemotherapy regimen; it might indicate that the anti-tumor activity of trastuzumab was not dependent on the chemotherapy regimen.
Gravalos et al. reported the first trial in HER2 positive AGC: trastuzumab with cisplatin monotherapy was an active regimen and has a favorable toxicity profile [11]. There were also nine patients who were elderly or presented low tumor load that accepted mono-chemotherapy as their first-line therapy in our study. Their survival was similar with others, which indicated mono-chemotherapy was also an active regimen. If patients did not have disease progression after six cycles of first-line therapy, there were two maintenance treatment options that depended on the physician’s choice: one was remaining in trastuzumab with chemotherapy; the other was stopping chemotherapy but using trastuzumab treatment alone. In contrast to ToGA, chemotherapy was required to be continued until disease progression in some phase II studies [8, 9, 11]. Median PFS reported in these studies seemed to be longer than that in ToGA, so we analyzed the prognosis in 88 patients who had SD/PR/CR after six cycles of initial therapy. There was no significant difference on OS or PFS of different maintenance therapy. Therefore, trastuzumab in combination with single chemotherapy drug or trastuzumab maintenance alone after six cycles might be both promising options with less toxicity in clinical practice, which were deserved to be verified in randomized clinical trials.
However, there were always limitations for this single-arm observational study. Explanatory analyses of subgroups of patients were post hoc, but not pre-planned. The baseline data might not be perfectly balanced. The other is the limitation of most single-center studies. We analyzed 107 patients who received trastuzumab-based therapy in one center, which lead to a small sample scale in some subgroups in univariate and multivariate analysis and some other bias compared with multicenter studies. All these might impair the statistical efficiency. A large sample of prospective control study in multicenter was warranted to verify the results in our study, especially to evaluate the efficacy of different treatment interventions in trastuzumab-based therapy.
In conclusion, the efficacy of trastuzumab in combination with chemotherapy in real-world setting in Chinese patients was similar with the outcome in the subgroup patients with high expression of HER2 in ToGA. Chemotherapy regimen and the maintenance therapy were not predictive factors influencing the outcome of trastuzumab-based therapy. ECOG PS scored 2 and liver metastasis were associated with a poor prognosis. Further exploration is warranted to improve the survival in these patients. More intensive, dual HER2 block, new drugs or regimens might be novel and promising approaches.
References
Siegel RL, Miller KD, Jemal A. Cancer Statistics. CA Cancer J Clin. 2017;67(1):7–30.
Dulak AM, Schumacher SE, van Lieshout J, Imamura Y, Fox C, Shim B, et al. Gastrointestinal adenocarcinomas of the esophagus, stomach, and colon exhibit distinct patterns of genome instability and oncogenesis. Cancer Res. 2012;72(17):4383–93.
Bang YJ, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet. 2012;376(9742):687–97.
Halon A, Donizy P, Biecek P, Rudno-Rudzinska J, Kielan W, Matkowski R. HER-2 expression in immunohistochemistry has no prognostic significance in gastric cancer patients. Sci World J. 2012;2012:941259.
Kim MA, Jung EJ, Lee HS, Lee HE, Jeon YK, Yang HK, et al. Evaluation of HER-2 gene status in gastric carcinoma using immunohistochemistry, fluorescence in situ hybridization, and real-time quantitative polymerase chain reaction. Hum Pathol. 2007;38(9):1386–93.
Shitara K, Yatabe Y, Matsuo K, Sugano M, Kondo C, Takahari D, et al. Prognosis of patients with advanced gastric cancer by HER2 status and trastuzumab treatment. Gastric Cancer. 2013;16(2):261–7.
Gomez-Martín C, Lopez-Rios F, Aparicio J, Barriuso J, García-Carbonero R, Pazo R, et al. A critical review of HER2-positive gastric cancer evaluation and treatment: from trastuzumab, and beyond. Cancer Lett. 2014;351(1):30–40.
Gong J, Liu T, Fan Q, Bai L, Bi F, Qin S, et al. Optimal regimen of trastuzumab in combination with oxaliplatin/capecitabine in first-line treatment of HER2-positive advanced gastric cancer (CGOG1001): a multicenter, phase II trial. BMC Cancer. 2016;16:68. doi:10.1186/s12885-016-2092-9.
Ryu MH, Yoo C, Kim JG, Ryoo BY, Park YS, Park SR, et al. Multicenter phase II study of trastuzumab in combination with capecitabine and oxaliplatin for advanced gastric cancer. Eur J Cancer. 2015;51(4):482–8.
Kurokawa Y, Sugimoto N, Miwa H, Tsuda M, Nishina S, Okuda H, et al. Phase II study of trastuzumab in combination with S-1 plus cisplatin in HER2-positive gastric cancer (HERBIS-1). Br J Cancer. 2014;110(5):1163–8.
Grávalos C, Gómez-Martín C, Rivera F, Alés I, Queralt B, Márquez A, et al. Phase II study of trastuzumab and cisplatin as first-line therapy in patients with HER2-positive advanced gastric or gastroesophageal junction cancer. Clin Transl Oncol. 2011;13(3):179–84.
Gómez-Martin C, Garralda E, Echarri MJ, Ballesteros A, Arcediano A, Rodríguez-Peralto JL, et al. HER2/neu testing for anti-HER2-based therapies in patients with unresectable and/or metastatic gastric cancer. J Clin Pathol. 2012;65(8):751–7.
Kataoka Y, Okabe H, Yoshizawa A, Minamiguchi S, Yoshimura K, Haga H, et al. HER2 expression and its clinicopathological features in resectable gastric cancer. Gastric Cancer. 2013;16(1):84–93.
Grabsch H, Sivakumar S, Gray S, Gabbert HE, Muller W. HER2 expression in gastric cancer: rare, heterogeneous and of no prognostic value—conclusions from 924 cases of two independent series. Cell Oncol. 2010;32(1–2):57–65.
Aizawa M, Nagatsuma AK, Kitada K, Kuwata T, Fujii S, Kinoshita T, et al. Evaluation of HER2-based biology in 1,006 cases of gastric cancer in a Japanese population. Gastric Cancer. 2014;17(1):34–42.
Park JS, Rha SY, Chung HC, Jung M, Kim KH, Jun HJ, et al. Clinicopathological features and prognostic significance of HER2 expression in gastric cancer. Oncology. 2015;88(3):147–56.
Zhang W, Yu Y, Fang Y, Wang Y, Cui Y, Shen K, et al. Systemic chemotherapy as a main strategy for liver metastases from gastric cancer. Clin Transl Oncol. 2015;17(11):888–94.
Chau I, Norman AR, Cunningham D, Waters JS, Oates J, Ross PJ. Multivariate prognostic factor analysis in locally advanced and metastatic esophago-gastric cancer-pooled analysis from three multicenter, randomized, controlled trials using individual patient data. J Clin Oncol. 2004;22(12):2395–403.
Yoshida M, Ohtsu A, Boku N, Miyata Y, Shirao K, Shimada Y, et al. Long-term survival and prognostic factors in patients with metastatic gastric cancers treated with chemotherapy in the Japan Clinical Oncology Group (JCOG) study. Jpn J Clin Oncol. 2004;34(11):654–9.
Koo DH, Ryoo BY, Kim HJ, Ryu MH, Lee SS, Moon JH, et al. A prognostic model in patients who receive chemotherapy for metastatic or recurrent gastric cancer: validation and comparison with previous models. Cancer Chemother Pharmacol. 2011;68(4):913–21.
Matsusaka S, Nashimoto A, Nishikawa K, Miki A, Miwa H, Yamaguchi K, et al. Clinicopathological factors associated with HER2 status in gastric cancer: results from a prospective multicenter observational cohort study in a Japanese population (JFMC44-1101). Gastric Cancer. 2016;19(3):839–51.
Dang HZ, Yu Y, Jiao SC. Prognosis of HER2 over-expressing gastric cancer patients with liver metastasis. World J Gastroenterol. 2012;18(19):2402–7.
Saito T, Nakanishi H, Mochizuki Y, Ito S, Ito Y, Misawa K, et al. Preferential HER2 expression in liver metastases and EGFR expression in peritoneal metastases in patients with advanced gastric cancer. Gastric Cancer. 2015;18(4):711–9.
Jiang H, Li Q, Yu S, Yu Y, Wang Y, Li W, et al. Impact of HER2 expression on outcome in gastric cancer patients with liver metastasis. Clin Transl Oncol. 2017;19(2):197–203.
Shah MA, Xu RH, Bang YJ, Hoff PM, Liu T, Herráez-Baranda LA, et al. HELOISE: phase IIIb randomized multicenter study comparing standard-of-care and higher-dose trastuzumab regimens combined with chemotherapy as first-line therapy in patients with human epidermal growth factor Receptor 2-positive metastatic Gastric or gastroesophageal junction adenocarcinoma. J Clin Oncol. 2017;. doi:10.1200/JCO.2016.71.6852.
Gomez-Martin C, Plaza JC, Pazo-Cid R, Salud A, Pons F, Fonseca P, et al. Level of HER2 gene amplification predicts response and overall survival in HER2-positive advanced gastric cancer treated with trastuzumab. J Clin Oncol. 2013;31(35):4445–52.
Ock CY, Lee KW, Kim JW, Kim JS, Kim TY, Lee KH, et al. Optimal patient selection for trastuzumab treatment in HER2-Positive advanced gastric cancer. Clin Cancer Res. 2015;21(11):2520–9.
Acknowledgements
Dr. Qian Li, Hong Li and Huiqin Jiang share first authorship in this work.
Funding
This work was supported by a grant from Shanghai Science and Technology Committee (Grant No. 15411961900). Thanks for offering financial supports for related clinical and pathological tests.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical standard
This study was approved by the Research Ethics Committee of Zhongshan Hospital, Fudan University. The study was conducted in full accordance with the 1964 Declaration of Helsinki and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Li, Q., Li, H., Jiang, H. et al. Predictive factors of trastuzumab-based chemotherapy in HER2 positive advanced gastric cancer: a single-center prospective observational study. Clin Transl Oncol 20, 695–702 (2018). https://doi.org/10.1007/s12094-017-1772-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12094-017-1772-5