Abstract
Background
The American Society of Clinical Oncology guidelines recommend early referral to reproductive endocrinology and infertility (REI) specialists for young women diagnosed with breast cancer. Current practice patterns demonstrate an increased utilization of neoadjuvant chemotherapy (NAC). We evaluated premenopausal women with breast cancer after consultation with a Fertility Nurse Specialist (FNS) and determine factors associated with referral to REI specialists.
Methods
This retrospective review included all premenopausal women diagnosed at our institution with stage 0–III unilateral breast cancers between 2009 and 2015 who completed an FNS consultation. Clinicopathologic features and factors associated with referral to REI after FNS consultation were analyzed.
Results
A total of 334 women were identified. Median age was 35 years (interquartile range 32–38). The majority of women were single (n = 198, 59.3%) and nulliparous (n = 239, 71.6%). REI referrals were common (n = 237, 71.0%). The Breast Surgery service was the most frequent referring service (n = 194, 58.1%), with significantly more REI referrals compared to Breast Medicine and Genetics services (p = 0.002). Nulliparity was associated with REI referral (p < 0.0001). Adjuvant chemotherapy (p = 0.003) was associated with pursuing REI referral, whereas NAC (p < 0.001) was associated with declining REI referral.
Conclusions
Most women elected to consult with an REI specialist, confirming strong interest in fertility preservation among premenopausal women with breast cancer. However, women receiving NAC more frequently declined referral to REI, suggesting that the need to start NAC may influence decisions regarding fertility preservation. With increasing utilization of NAC, our study supports the need for further counseling and education regarding fertility preservation for women undergoing NAC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Breast cancer is the most commonly diagnosed malignancy in women of reproductive age.1 Although prevalence of breast cancer in young women is low, 6.6% of all breast cancers are diagnosed in women 40 years of age or younger.2,3 Recent advances in treatment regimens over the past several decades have dramatically improved disease-free and overall survival, prompting providers to focus more attention on optimizing patient quality of life.4 As women increasingly delay childbearing for personal and professional reasons, it is likely that many women will be diagnosed with breast cancer before completion of childbearing.5,6 These intersecting trends help to explain the heightened awareness and concern regarding fertility after breast cancer treatment.
Breast cancer treatment is associated with infertility.7,8 Cytotoxic chemotherapeutic agents induce fibrosis, apoptosis of primordial follicles, and vascular damage, compromising stromal function and depleting ovarian reserve.9 In addition to inciting direct toxicity to the ovary and accelerating natural declines in ovarian function, adjuvant therapies can impose temporal delays on childbearing, further compromising fertility.
Current practice patterns demonstrate a trend toward increasing NAC utilization in women with invasive breast cancer.10,11,–12 Use of NAC has historically been limited to treatment of locally advanced disease, but recommendations for NAC in early-stage breast cancer are increasing, especially in the setting of high-risk molecular tumor subtypes.13,14 Young women are more likely to have delays in diagnosis and to harbor these aggressive subtypes with higher rates of high-grade, triple negative, and HER2 overexpressing tumors, compared with their older counterparts.4,15,16 The benefits of NAC include both prognostic and predictive information as well as potentially minimizing surgical intervention, particularly for women with nodal involvement.17 Thus, for women of reproductive age, the use of NAC has significant implications for future fertility.7,8
Previous studies have indicated that chemotherapy-induced infertility is associated with negative quality of life as well as increased anxiety and psychological burden.18,19 Indeed, significant interest in and concerns regarding fertility have been reported in premenopausal women with breast cancer.8,20,21,22,–23 The American Society of Clinical Oncology (ASCO) has recognized the need for fertility counseling in the setting of a new cancer diagnosis and has implemented recommendations that emphasize the paramount importance of accurate reproductive counseling and timely referral to reproductive endocrinologists.24 Despite these recommendations, studies have consistently demonstrated that women do not receive adequate counseling regarding potential impact on future fertility and options for fertility preservation.21,25,26,27,–28
In an effort to meet this need, Memorial Sloan Kettering Cancer Center (MSKCC) established the MSKCC Cancer and Fertility Program in 2009 with the goal of educating women about treatment-related fertility risks, as well as fertility preservation and family building options, and facilitating referrals to reproductive endocrinologists and infertility (REI) specialists. This study evaluates the factors associated with referral to REI specialists for women with breast cancer and the effect of NAC on the decision to pursue REI consultation.
Methods
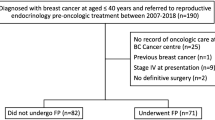
We performed an Institutional Review Board-approved retrospective review of a prospectively maintained breast cancer database to identify all women with stage 0-III breast cancer between 2009 and 2015 who consulted with a Fertility Nurse Specialist (FNS) in the MSKCC Cancer and Fertility Program. Clinicopathologic features, treatment variables, referring service, and outcome of FNS consultation were collected. FNS consultation outcomes were prospectively recorded as REI consult accepted or declined. Women who accepted REI referral were compared with those who declined REI referral following FNS consultation. Women with bilateral cancer or women who were missing information on REI referral status were excluded.
Continuous characteristics were summarized with the median and interquartile range (IQR), whereas categorical characteristics were summarized with the frequency and percentage. Comparisons between those accepting and declining REI referral, and between those receiving NAC or not, were made with the Wilcoxon rank-sum test for continuous variables, and the Chi square test or Fisher’s exact test, as appropriate, for categorical variables. A p value ≤ 0.05 was considered statistically significant. All statistical analyses were conducted in R software version 3.2.5 (R Core Development Team, Vienna, Austria).
MSKCC Cancer and Fertility Program
MSKCC established its Cancer and Fertility Program in 2009 to address the growing need for comprehensive patient education about the impact of cancer diagnosis and treatments on subsequent fertility and family planning. An FNS provides counseling regarding potential reproductive toxicities of proposed cancer treatments as well as opportunities for fertility preservation before initiation of cancer therapy, including facilitating referrals to REI specialists. All premenopausal women who are diagnosed with breast cancer are offered consultation with an FNS before beginning treatment.
Results
Patient Demographics
A total of 334 women who underwent FNS referral were identified. During this time period, 3242 premenopausal women were evaluated at MSKCC with a new diagnosis of breast cancer. Patient demographics are detailed in Table 1. Median age was 35 years (interquartile [IQR] 32–39). Most women were Caucasian (n = 210, 62.8%) and had private insurance (n = 296, 88.6%). The majority of women were single (n = 198, 59.3%), nulligravid (n = 185, 55.4%), and nulliparous (n = 239, 71.6%). Previous oral contraceptive use was common (n = 232, 69.5%), whereas previous fertility treatment was rare (n = 28, 8.4%). Germline mutations were detected in 13.8% (n = 46) of women, and family history of a first-degree family member with breast or ovarian cancer was uncommon (n = 38, 11.4%; and n = 5, 1.5%, respectively).
Tumor Characteristics
The predominant histology was invasive ductal carcinoma (n = 309, 92.5%) with a median tumor size of 2.0 cm (IQR 1.2–2.8 cm; Table 1). Stage II was the most common stage at diagnosis (n = 158, 47.3%), followed by stage I (n = 121, 36.2%), and stage III (n = 45, 13.5%). Stage 0 cancers comprised only 3% (n = 10) of the entire cohort. The majority of tumors were high grade (n = 177, 53.0%), expressed estrogen receptor (ER) (n = 257, 76.9%), and did not demonstrate HER2 amplification (n = 267, 79.9%). Triple negative tumors comprised 17.4% (n = 58) of tumors.
Treatment Characteristics
Table 1 summarizes treatment characteristics. The most common surgical approach was mastectomy (n = 208, 62.3%). Of women who underwent mastectomy, 66.3% (n = 138) elected to undergo contralateral prophylactic mastectomy for risk reduction. Almost all patients underwent axillary staging (n = 326, 97.6%), the majority with sentinel lymph node biopsy alone (n = 216, 64.7%). The eight women who did not undergo axillary staging had pure ductal carcinoma in situ. Axillary lymph node dissection (ALND) was performed in 32.9% (n = 110) of patients.
The majority of women received systemic therapy. Adjuvant chemotherapy was administered to 195 (58.4%) women, whereas a neoadjuvant approach was less common (n = 63, 18.9%). Endocrine therapy was prescribed to 73.1% (244 of 334) of all patients and to 91.1% (234 of 257) of those who were ER positive.
Fertility Nurse Specialist Consults
All women met with an FNS (either in-person or via phone consultation) to discuss fertility concerns and the option to obtain an REI referral. The Breast Surgery Service was the most common source of referral to the FNS team (n = 194, 58.1%; Table 2). The majority of FNS consultations were performed over the phone (n = 268, 80.2%), whereas the minority (n = 66, 19.8%) were performed as office-based consultations. After FNS consultation, 237 (71.0%) women proceeded with an REI referral, and 97 (29.0%) declined REI referral.
Factors Associated with REI Referral
Nulliparity was associated with more frequent acceptance of REI referral (p < 0.0001); however, there was no association between age, marital status, gravida status, race, or insurance type with REI referral (Table 2). Referral from the Breast Surgery Service was associated with higher frequency of acceptance of REI referral (p = 0.002) as was early-stage disease (p < 0.001). Additionally, timing of chemotherapy administration was associated with outcome of FNS consultation; adjuvant chemotherapy was associated with REI referral (p = 0.003), whereas NAC was associated with declining REI referral (p < 0.001). Of the 195 women who received adjuvant chemotherapy, 151 (77.4%) pursued REI referral compared with 25 (39.7%) of 63 women who received NAC (Table 3). On multivariate analysis, only referring service and receipt of NAC were associated with decision of whether to pursue REI referral or not.
NAC Versus Adjuvant Chemotherapy
Women in our study group receiving chemotherapy received anthracycline-based regimens in the majority of cases (n = 210, 81.4% of women receiving chemotherapy). The majority of women were treated before 2015 before the results of the POEMS (Prevention of Early Menopause Study) trial were published. As a result, use of GnRH agonists for fertility preservation was only routinely offered to patients starting in 2015.
To investigate the finding that women who received NAC were more likely to decline REI referral (p < 0.001), we performed a subset analysis comparing women who received NAC (n = 63) with those who received adjuvant chemotherapy (n = 195). The two subsets of women were similar with regard to demographics (Table 3). Although the distribution of tumor histology was similar, tumor molecular profiles differed between groups. Women receiving NAC had more advanced disease, with larger tumor size and a higher proportion of adverse molecular subtypes (ER negative and HER2 positive), compared with those who received adjuvant chemotherapy (all p < 0.05). Women receiving NAC also had a higher frequency of clinically node-positive disease (NAC n = 43, 68.3% vs. adjuvant chemotherapy n = 93, 47.7%; p = 0.006) and more frequently received ALND at the time of surgery. The receipt of endocrine therapy was similar between groups.
A total of 97 women who received chemotherapy declined REI consultation (n = 44 in the adjuvant chemotherapy group and n = 38 in the NAC group) (Table 4). There was no statistical difference in molecular profile, but among women who declined REI consultation, women who received NAC did have more advanced disease compared with those who received adjuvant chemotherapy (p = 0.03).
Treatment delays, defined as initiating chemotherapy more than 6 weeks after initial diagnosis in the NAC setting, and more than 12 weeks in the adjuvant setting, were uncommon. In the women undergoing NAC, a total of four (6.3%) women receiving NAC started chemotherapy ≥ 6 weeks after initial diagnosis; of those, three women had pursued an REI referral. Similarly, a total of seven (3.5%) women receiving adjuvant chemotherapy failed to initiate chemotherapy by 12 weeks after surgery; of those, six women pursued an REI referral. Overall, the number of women who had delays in receiving chemotherapy is too small to make any statistical comparisons.
Discussion
More than 70% of consultations with the FNS resulted in an REI referral, confirming previous findings of significant interest in future fertility among premenopausal women with breast cancer. Women who pursued an REI referral tended to be nulliparous, in agreement with existing studies.21 We noted an interesting relationship between REI referral and timing of chemotherapy; despite similar demographic characteristics, women who received NAC declined REI referral more frequently compared with those who received adjuvant chemotherapy. This relationship persisted on multivariate analysis, while early stage of disease, which was significantly associated with REI referral, failed to be associated with REI referral on multivariate analysis. This finding suggests that it is the receipt of NAC rather than advanced disease that drives the trend to decline REI referral among premenopausal women who receive NAC.
NAC offers a range of potential benefits, ranging from downstaging the breast and axilla, allowing for breast conservation and potential obviation of ALND, to providing a measure of histologic response to chemotherapeutic agents.17,30 Oncologists also can tailor adjuvant therapies according to degree of pathologic response.17,30 Despite these advantages, recommendation for NAC is associated with a potential “scare factor” that may indicate increased severity and urgency to a patient.31 Indeed, women who received NAC in our study had more advanced disease and higher incidence of unfavorable molecular subtypes (ER negative and HER2 positive subtypes ). Internalization of this fear and anxiety could partially explain our study finding that only 40% of patients undergoing NAC sought an REI referral and that receipt of NAC was associated with a decision to decline consultation with an REI specialist. Additionally, NAC has been associated with higher levels of psychological distress, which have been linked to anxiety and depression.32 A study of infertile women demonstrated that patients who screened positive for depression were less likely to initiate fertility treatments, highlighting the complexity of potential factors that enter into the decisional calculus regarding fertility treatment.33
While the finding that receipt of NAC was associated with less-frequent acceptance of REI referral is novel and significant on its own, it becomes even more important in the context of a recent multicenter study that demonstrated that NAC was an independent negative predictor of completing ovarian stimulation following REI consultation.34 The less-frequent referral to REI and higher odds of not completing ovarian stimulation makes the NAC setting particularly challenging for women who are interested in fertility preservation.
Although current advances in fertility preservation techniques are associated with favorable outcomes and include a range of options, such as administration of ovarian suppression with gonadotropin-releasing hormone analogs during chemotherapy, ovarian tissue, oocyte, and embryo cryopreservation strategies, potential concerns may lead to clinician and patient reluctance to pursue these options before NAC.29,35 These concerns include estradiol level elevations during ovarian stimulation treatment as well as temporal delays in starting NAC because of pursuit of these options. Ovarian stimulation is associated with a tenfold increase in baseline estradiol levels, which could promote mitogenic effects on ER positive tumors, especially in the neoadjuvant setting, in which the tumor remains in situ.36 Although the exposure is limited, the concept of intentionally generated hormonal milieus with elevated levels of estradiol before or during breast cancer treatment is difficult to reconcile and has led to increased interest in alternative strategies, including cryopreservation of ovarian tissue.37 Research leading to refinement of ovarian stimulation cycles to maximize oocyte yield while minimizing serum estradiol levels is ongoing.38,39,40,41,42,43,–44 However, it is reassuring that several studies have reported equivalent rates of recurrence and survival in patients with breast cancer electing to undergo ovarian stimulation compared to those who do not undergo ovarian stimulation.30,45,46,–47
Regarding concerns about treatment delay, traditional protocols require ovarian stimulation to commence during the follicular phase, which can lead to patients waiting 6 weeks to complete a single cycle.43 The introduction of random-start protocols has revolutionized the timing of ovarian stimulation cycles, allowing patients to complete a single cycle within 2 weeks.5,48 The time between surgery and initiation of adjuvant chemotherapy is a preferred time to pursue cryopreservation cycles, as waiting up to 12 weeks to start chemotherapy does not adversely impact survival outcomes.49,50 Timing of fertility treatment certainly becomes more complex in the setting of NAC; however, recent studies have suggested that use of ovarian stimulation is not associated with clinically meaningful delays in initiation of NAC or deleterious oncologic outcomes.51,52 Similarly, our study demonstrated that REI referral rarely delayed initiation of chemotherapy in both the neoadjuvant and adjuvant settings.
Current recommendations for prolonged endocrine therapy (10 years) also may affect decisions for pursuit of fertility preservation options in young women with ER-positive breast cancer.53,54,–55 Although the need for endocrine therapy was not associated with patient acceptance of referral to an REI in our study, it is important to note recent studies have shown that up to 40% of women receiving endocrine therapy for breast cancer are interested in interruption of endocrine therapy to pursue pregnancy.56 The POSITIVE (Pregnancy Outcome and Safety of Interrupting Therapy for women with endocrine responsIVE breast cancer) trial is ongoing, and may answer questions regarding oncologic safety of endocrine therapy interruption. In the future, the use of prolonged endocrine therapy without interruption may change REI referral uptake and pursuit of fertility preservation options.
In our study, Breast Surgery was the most common referring service, responsible for 58% of referrals to the FNS, and was associated with uptake of REI consultation. Indeed, along with receipt of NAC, referral to an FNS from the Breast Surgery service was one of only two factors that remained associated with decisions regarding REI consultation. Previous studies from our institution have suggested that breast surgical oncologists are uniquely positioned to facilitate early referrals to fertility specialists, because they often are the initial point of contact for women with a new breast cancer diagnosis.21 Timely referral to REI specialists is of paramount importance, as early referral has been shown to permit multiple cryopreservation cycles without delaying initiation of neoadjuvant or adjuvant chemotherapy.49,51
This study is limited by its single-institution retrospective design, which may compromise its generalizability. Another important limitation is that this study did not capture the outcome of the REI consultations. At a tertiary care cancer center without an REI department, all consultations were performed at different outside institutions; as a result, this retrospective review was unable to identify the rate of uptake of ovarian stimulation or other forms of fertility preservation in the study population. Additionally, our study focuses on decision making and use of REI consultation at time of diagnosis, and thus subsequent pregnancy after breast cancer (including successful pregnancy after pursuing advanced reproductive techniques) is beyond the scope of this study. Additionally, although we were able to capture some differences in demographics, clinicopathologic features, and treatments between women who pursued REI referral and those who declined, the study lacks the granularity to understand patient-level decision making. Additional studies are planned to evaluate trends in uptake of fertility options in women who elect to pursue formal fertility consultation.
Despite these limitations, this study indicates interest in fertility preservation among premenopausal women with breast cancer and suggests that NAC may affect decisions regarding pursuit of fertility preservation options. With increasing utilization of NAC in breast cancer, our study supports the need for further counseling and education regarding fertility preservation for women undergoing NAC. Future studies evaluating the impact of both FNS education programs and clinician counseling on choice of fertility preservation options are necessary in the NAC setting.
References
Hery C, Ferlay J, Boniol M, Autier P. Changes in breast cancer incidence and mortality in middle-aged and elderly women in 28 countries with Caucasian majority populations. Ann Oncol. 2008;19(5):1009–18.
Anders CK, Johnson R, Litton J, Phillips M, Bleyer A. Breast cancer before age 40 years. Semin Oncol. 2009;36(3):237–49.
Merlo DF, Ceppi M, Filiberti R, et al. Breast cancer incidence trends in European women aged 20–39 years at diagnosis. Breast Cancer Res Treat. 2012;134(1):363–70.
Murphy BL, Day CN, Hoskin TL, Habermann EB, Boughey JC. Adolescents and young adults with breast cancer have more aggressive disease and treatment than patients in their forties. Ann Surg Oncol. 2019;26(12):3920–30.
Cakmak H, Rosen MP. Random-start ovarian stimulation in patients with cancer. Curr Opin Obstet Gynecol. 2015;27(3):215–21.
Mathews TJ, Hamilton BE. Mean Age of Mothers is on the Rise: United States, 2000–2014. NCHS Data Brief. 2016;232:1–8.
Letourneau JM, Ebbel EE, Katz PP, et al. Acute ovarian failure underestimates age-specific reproductive impairment for young women undergoing chemotherapy for cancer. Cancer. 2012;118(7):1933–9.
Partridge AH, Ruddy KJ. Fertility and adjuvant treatment in young women with breast cancer. Breast. 2007;16 Suppl 2:S175–81.
Soleimani R, Heytens E, Darzynkiewicz Z, Oktay K. Mechanisms of chemotherapy-induced human ovarian aging: double strand DNA breaks and microvascular compromise. Aging (Albany NY). 2011;3(8):782–93.
Mougalian SS, Soulos PR, Killelea BK, et al. Use of neoadjuvant chemotherapy for patients with stage I to III breast cancer in the United States. Cancer. 2015;121(15):2544–52.
Murphy BL, Day CN, Hoskin TL, Habermann EB, Boughey JC. Neoadjuvant chemotherapy use in breast cancer is greatest in excellent responders: triple-negative and HER2 + subtypes. Ann Surg Oncol. 2018;25(8):2241–8.
Puig CA, Hoskin TL, Day CN, Habermann EB, Boughey JC. National trends in the use of neoadjuvant chemotherapy for hormone receptor-negative breast cancer: a national cancer data base study. Ann Surg Oncol. 2017;24(5):1242–50.
Alberro JA, Ballester B, Deulofeu P, et al. Long-term outcomes for neoadjuvant versus adjuvant chemotherapy in early breast cancer: meta-analysis of individual patient data from ten randomised trials. Lancet Oncol. 2018;19(1):27–39.
von Minckwitz G, Untch M, Blohmer JU, et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol. 2012;30(15):1796–804.
Chen HL, Zhou MQ, Tian W, Meng KX, He HF. Effect of age on breast cancer patient prognoses: a population-based study using the SEER 18 Database. PLoS ONE. 2016;11(10):e0165409.
Kollias J, Elston CW, Ellis IO, Robertson JF, Blamey RW. Early-onset breast cancer–histopathological and prognostic considerations. Br J Cancer. 1997;75(9):1318–23.
Mamtani A, Barrio AV, King TA, et al. How often does neoadjuvant chemotherapy avoid axillary dissection in patients with histologically confirmed nodal metastases? Results of a prospective study. Ann Surg Oncol. 2016;23(11):3467–74.
Howard-Anderson J, Ganz PA, Bower JE, Stanton AL. Quality of life, fertility concerns, and behavioral health outcomes in younger breast cancer survivors: a systematic review. J Natl Cancer Inst. 2012;104(5):386–405.
Ruddy KJ, Gelber SI, Tamimi RM, et al. Prospective study of fertility concerns and preservation strategies in young women with breast cancer. J Clin Oncol. 2014;32(11):1151–6.
Dunn J, Steginga SK. Young women’s experience of breast cancer: defining young and identifying concerns. Psychooncology. 2000;9(2):137–46.
Goldfarb SB, Kamer SA, Oppong BA, et al. Fertility preservation for the young breast cancer patient. Ann Surg Oncol. 2016;23(5):1530–6.
Lambertini M, Fontana V, Massarotti C, et al. Prospective study to optimize care and improve knowledge on ovarian function and/or fertility preservation in young breast cancer patients: Results of the pilot phase of the PREgnancy and FERtility (PREFER) study. Breast. 2018;41:51–6.
Partridge AH, Gelber S, Peppercorn J, et al. Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol. 2004;22(20):4174–83.
Loren AW, Mangu PB, Beck LN, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013;31(19):2500–10.
Duffy CM, Allen SM, Clark MA. Discussions regarding reproductive health for young women with breast cancer undergoing chemotherapy. J Clin Oncol. 2005;23(4):766–73.
Jukkala AM, Azuero A, McNees P, Bates GW, Meneses K. Self-assessed knowledge of treatment and fertility preservation in young women with breast cancer. Fertil Steril. 2010;94(6):2396–8.
Peate M, Meiser B, Friedlander M, et al. It’s now or never: fertility-related knowledge, decision-making preferences, and treatment intentions in young women with breast cancer—an Australian fertility decision aid collaborative group study. J Clin Oncol. 2011;29(13):1670–7.
Ruddy KJ, Gelber S, Ginsburg ES, et al. Menopausal symptoms and fertility concerns in premenopausal breast cancer survivors: a comparison to age- and gravidity-matched controls. Menopause. 2011;18(1):105–8.
Moore HC, Unger JM, Phillips KA, et al. Goserelin for ovarian protection during breast-cancer adjuvant chemotherapy. N Engl J Med. 2015;372(10):923–32.
King TA, Morrow M. Surgical issues in patients with breast cancer receiving neoadjuvant chemotherapy. Nat Rev Clin Oncol. 2015;12(6):335–43.
Hershlag A, Mullin C, Bristow SL. Is fertility preservation feasible and safe with neoadjuvant therapy for breast cancer? J Glob Oncol. 2018;4:1–5.
Magno S, Carnevale S, Dentale F, Belella D, Linardos M, Masetti R. Neo-adjuvant chemotherapy and distress in breast cancer patients: The moderating role of generalized self-efficacy. 2017;35(15_suppl):e21570–70.
Crawford NM, Hoff HS, Mersereau JE. Infertile women who screen positive for depression are less likely to initiate fertility treatments. Hum Reprod. 2017;32(3):582–7.
Kim J, Oktay K, Gracia C, Lee S, Morse C, Mersereau JE. Which patients pursue fertility preservation treatments? A multicenter analysis of the predictors of fertility preservation in women with breast cancer. Fertil Steril. 2012;97(3):671–6.
Taylan E, Oktay KH. Current state and controversies in fertility preservation in women with breast cancer. World J Clin Oncol. 2017;8(3):241–8.
Joo BS, Park SH, An BM, Kim KS, Moon SE, Moon HS. Serum estradiol levels during controlled ovarian hyperstimulation influence the pregnancy outcome of in vitro fertilization in a concentration-dependent manner. Fertil Steril. 2010;93(2):442–6.
Oktay K, Taylan E, Kawahara T, Cillo GM. Robot-assisted orthotopic and heterotopic ovarian tissue transplantation techniques: surgical advances since our first success in 2000. Fertil Steril. 2019;111(3):604–6.
Azim AA, Costantini-Ferrando M, Oktay K. Safety of fertility preservation by ovarian stimulation with letrozole and gonadotropins in patients with breast cancer: a prospective controlled study. J Clin Oncol. 2008;26(16):2630–5.
Oktay K, Turan V, Bedoschi G, Pacheco FS, Moy F. Fertility preservation success subsequent to concurrent aromatase inhibitor treatment and ovarian stimulation in women with breast cancer. J Clin Oncol. 2015;33(22):2424–9.
Turan V, Bedoschi G, Moy F, Oktay K. Safety and feasibility of performing two consecutive ovarian stimulation cycles with the use of letrozole-gonadotropin protocol for fertility preservation in breast cancer patients. Fertil Steril. 2013;100(6):1681–5 e1681.
Martinez M, Rabadan S, Domingo J, Cobo A, Pellicer A, Garcia-Velasco JA. Obstetric outcome after oocyte vitrification and warming for fertility preservation in women with cancer. Reprod Biomed Online. 2014;29(6):722–8.
Cavagna F, Pontes A, Cavagna M, et al. A specific controlled ovarian stimulation (COS) protocol for fertility preservation in women with breast cancer undergoing neoadjuvant chemotherapy. Contemp Oncol (Pozn). 2017;21(4):290–4.
Cavagna F, Pontes A, Cavagna M, et al. Specific protocols of controlled ovarian stimulation for oocyte cryopreservation in breast cancer patients. Curr Oncol. 2018;25(6):e527–32.
Pereira N, Kelly AG, Stone LD, et al. Gonadotropin-releasing hormone agonist trigger increases the number of oocytes and embryos available for cryopreservation in cancer patients undergoing ovarian stimulation for fertility preservation. Fertil Steril. 2017;108(3):532–8.
Meirow D, Raanani H, Maman E, et al. Tamoxifen co-administration during controlled ovarian hyperstimulation for in vitro fertilization in breast cancer patients increases the safety of fertility-preservation treatment strategies. Fertil Steril. 2014;102(2):488–95 e483.
Moravek MB, Confino R, Smith KN, et al. Long-term outcomes in cancer patients who did or did not pursue fertility preservation. Fertil Steril. 2018;109(2):349–55.
Oktay K, Buyuk E, Libertella N, Akar M, Rosenwaks Z. Fertility preservation in breast cancer patients: a prospective controlled comparison of ovarian stimulation with tamoxifen and letrozole for embryo cryopreservation. J Clin Oncol. 2005;23(19):4347–53.
von Wolff M, Capp E, Jauckus J, Strowitzki T, Germeyer A, Ferti Psg. Timing of ovarian stimulation in patients prior to gonadotoxic therapy: an analysis of 684 stimulations. Eur J Obstet Gynecol Reprod Biol. 2016;199:146–9.
Lee S, Ozkavukcu S, Heytens E, Moy F, Oktay K. Value of early referral to fertility preservation in young women with breast cancer. J Clin Oncol. 2010;28(31):4683–6.
Lohrisch C, Paltiel C, Gelmon K, et al. Impact on survival of time from definitive surgery to initiation of adjuvant chemotherapy for early-stage breast cancer. J Clin Oncol. 2006;24(30):4888–94.
Letourneau JM, Sinha N, Wald K, et al. Random start ovarian stimulation for fertility preservation appears unlikely to delay initiation of neoadjuvant chemotherapy for breast cancer. Hum Reprod. 2017;32(10):2123–9.
Letourneau JM, Wald K, Sinha N, et al. Fertility preservation before breast cancer treatment appears unlikely to affect disease-free survival at a median follow-up of 43 months after fertility-preservation consultation. Cancer. 2019.
Davies C, Pan H, Godwin J, et al. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet. 2013;381(9869):805–16.
Gray RG, Rea D, Handley K, et al. aTTom: Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years in 6,953 women with early breast cancer. J Clin Oncol. 2013;31(15).
Rosenberg SM, Gelber S, Gelber RD, et al. Oncology physicians’ perspectives on practices and barriers to fertility preservation and the feasibility of a prospective study of pregnancy after breast cancer. J Adolesc Young Adult Oncol. 2017;6(3):429–34.
Braems G, Denys H, De Wever O, Cocquyt V, Van den Broecke R. Use of tamoxifen before and during pregnancy. Oncologist. 2011;16(11):1547–51.
Acknowledgment
This study was accepted for presentation in poster format at the 21st Annual Meeting of the American Society of Breast Surgeons, April 29–May 3, 2020, Las Vegas, NV.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The preparation of this manuscript was funded in part by NIH/NCI Cancer Center Support Grant No. P30 CA008748 to Memorial Sloan Kettering Cancer Center. Dr. Shari B. Goldfarb discloses research funding from Sprout Pharmaceuticals and Paxman Coolers Ltd, and consulting and advisory roles to Sermonix Pharmaceuticals, Bayer Healthcare, and Procter and Gamble. All other authors have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Crown, A., Muhsen, S., Zabor, E.C. et al. Does Use of Neoadjuvant Chemotherapy Affect the Decision to Pursue Fertility Preservation Options in Young Women with Breast Cancer?. Ann Surg Oncol 27, 4740–4749 (2020). https://doi.org/10.1245/s10434-020-08883-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08883-y