Abstract
Background
Surgical resection is associated with the best long-term results for intrahepatic cholangiocarcinoma (ICC); however, long-term outcomes are still poor.
Objective
The primary aim of this study was to validate the recently proposed MEGNA score and to identify additional prognostic factors influencing short- and long-term survival.
Patients and Methods
This was a retrospective analysis of a German multicenter cohort operated at 10 tertiary centers from 2004 to 2013. Patients were clustered using the MEGNA score and overall survival was analyzed. Cox regression analysis was used to identify prognostic factors for both overall and 90-day survival.
Results
A total of 488 patients undergoing liver resection for ICC fulfilled the inclusion criteria and underwent analysis. Median age was 67 years, 72.5% of patients underwent major hepatic resection, and the lymphadenectomy rate was 86.9%. Median overall survival was 32.2 months. The MEGNA score significantly discriminated the long-term overall survival: 0 (68%), I (48%), II (32%), and III (19%) [p <0.001]. In addition, anemia was an independent prognostic factor for overall survival (hazard ratio 1.78, 95% confidence interval 1.29–2.45; p <0.01).
Conclusion
Hepatic resection provides the best long-term survival in all risk groups (19–65% overall survival). The MEGNA score is a good discriminator using histopathologic items and age for stratification. Correction of anemia should be attempted in every patient who responds to treatment. Perioperative liver failure remains a clinical challenge and contributes to a relevant number of perioperative deaths.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Cholangiocarcinoma is a tumor with a great regional variance in prevalence, and is increasingly prevalent worldwide. In Germany, the number of cholangiocarcinoma cases have more than doubled during the last 15 years, from approximately 5000 newly diagnosed and treated patients in the year 2000 to over 10,000 patients per year in 2015.1 The median age at diagnosis was 71 years for male patients and 74 years for female patients. Notably, the long-term survival data at 5 and 10 years was still very poor (13% and 7%).1 The overall survival data after curative surgery varies in the literature and is difficult to assess because most studies only consider small cohorts of patients; thus, the range is considerably wide, with 32–64% 5-year overall survival rates in highly selected populations. For a German cohort of 4667 patients operated between 2010 and 2015, the Federal Statistical Office data reveal a hospital mortality rate of 11.0%.2 Factors associated with outcome analysis on specific subgroups show that patients with extraordinarily good prognosis do exist.3,4,–5 Undoubtedly, surgical resection is the gold standard and leads to the best long-term survival rates.4,6 Although surgery imposes the highest risk of dying in the perioperative period, when compared with interventional and chemotherapeutic treatments, it outnumbers both these treatment options because of the advantage in overall survival.6 In this project, we established a cooperative of German centers, which is a unique first accomplishment and is therefore worthwhile mentioning. Our primary aim was to validate the recently proposed MEGNA score,3 which is based on histopathological factors plus patient age, and has been shown to be of higher predictive value than the AJCC classification for intrahepatic cholangiocarcinoma (ICC). As a secondary aim, prognostic factors influencing short- and long-term survival should be identified.
Patients and methods
Study Design
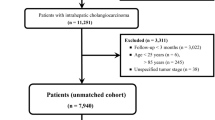
This was a retrospective analysis of a multicenter cohort of patients who were operated for ICC at 10 German tertiary care centers from 1 January 2004 to 31 December 2013. The primary objective was to validate the MEGNA score, which is based on tumor number, T classification, grading, nodal status, and patient age.3 The Institutional Review Board of the Medical Faculty Mannheim of the University of Heidelberg provided permission for the study on 4 April 2016 (2016-816R-MA). The data were retrospectively collected from patient charts and tumor databases. Each patient was followed up until 5 years after surgery, death, or to the date of last contact.
Inclusion and Exclusion Criteria
Adult patients (> 18 years) with a histologic diagnosis of ICC and who were operated with curative intent were included in this study. Patients with metastatic tumors prior to resection and who had undergone exploratory laparotomies or laparoscopies were excluded from the analysis, as were patients who had limited peritoneal spread or extra regional lymph node metastases. Follow-up data were obtained from local patient charts, tumor databases, and by phone calls to the general practitioner or requests to the national registration offices to obtain the most recent survival status.
Variables and Statistical Analysis
The data were evaluated and analyzed in a dichotomous binary fashion. The age groups were defined as 18–60 years and > 60 years. Information regarding sex and concomitant disease, including diabetes, smoking, cardiovascular risk, liver disease and ascites, were collected. Imaging modalities included ultrasound, computed tomography (CT) scan and magnetic resonance imaging (MRI). The extent of resection was divided into major and minor resections in accordance with the Brisbane classification,7 while complications were classified in accordance with the Dindo–Clavien classification.8 Perioperative biliary leakage, post-hepatectomy hemorrhage, and post-hepatectomy liver failure were classified in accordance with the International Study Group for Liver Surgery (ISGLS) definitions.9,10,–11 Additionally, data on preoperative pathologic work-up, the requirement for the transfusion of packed red blood cells within the first 24 h after resection, and their number, were collected. Preoperative laboratory values included serum albumin, serum bilirubin, and serum creatinine. Serum creatinine values > 1.2 mg/dL were defined as pathologic and indicating renal damage in accordance with the study by Chawla et al., which found a correlation of a 50% increase in odds for chronic kidney disease following surgery for every increase in serum creatinine unit.12 Preoperative hemoglobin values were collected to detect anemia, which was defined as hemoglobin values lower than 11.5 g/dL for female patients and lower than 13.5 g/dL for male patients, in accordance with the recommendations from the German Patient Blood Management Network.13,14,–15 Tumor-specific data were classified in accordance with the 8th edition of the American Joint Committee on Cancer (AJCC) classification of ICC.16
In the initial request to the centers, we asked for data on all consecutive patients operated in the defined period; however, selection bias cannot be ruled out completely. Statistical analysis was performed using SPSS version 25 (IBM Corporation, Armonk, NY, USA). Data were analyzed for frequency and were reported as total numbers with percentages. Differences among groups and the univariable analyses were tested using the Chi square test. Multivariable analysis was performed using a Cox regression model for survival with stepwise backward elimination. The binary data revealing a p value of < 0.1 were entered into the multivariable analysis. Variables with a p value < 0.05 were considered relevant for the prognosis after resection of ICC. Patients who were lost to follow-up prior to 5 years after resection were censored at the day of last contact. The ELM (extrahepatic extension, large tumors, multiple tumors) and ISS (intrahepatic, small, single tumors) groups were defined in accordance with the studies by Spolverato et al.17 and Hyder et al.18 The MEGNA risk score was calculated as outlined in the study by Raoof et al.3 Patients with more than 25% of data missing were excluded from the analysis.
Results
Demographics and Tumor Characteristics
The 10 German sites identified a total of 793 patients at their sites who were eligible due to their diagnosis of ICC. A total of 305 patients were excluded from the analysis; 280 patients either had irresectable tumors on imaging (n =168) or they underwent exploratory laparotomy or laparoscopy and showed signs of diffuse intrahepatic spread or peritoneal carcinomatosis (n =112). For 25 patients, more than 25% of data were missing. Finally, a total of 488 patients undergoing liver resection for ICC fulfilled the inclusion criteria and were included in the analysis, of whom 250 (51.2%) were male and 348 (71.3%) were older than 60 years.
Diabetes, smoking, and cardiovascular disease (19.3%, 17.8%, and 34.0%, respectively) were the most common concomitant diseases, and approximately 38% of patients had a biopsy prior to surgery. Importantly, 43 patients (8.8%) had a slightly increased serum creatinine level and 124 patients (25.4%) had anemia prior to resection. Most patients (72.5%) underwent major resection and 17.8% required a blood transfusion within the first 24 perioperative hours. Tumor characteristics in accordance with the 8th edition of the AJCC showed the following distribution in Union for International Cancer Control (UICC) stages: Ia (15.6%), Ib (9.2%), II (19.5%), IIIa (11.1%), and IIIb (44.7%). Patients with stage IV cancer were excluded from the analysis. A total of 9% of patients had T4-staged tumors, 28.9% of patients had N + tumors, and 13.1% of patients had an Nx situation in pathologic work-up. More than 40% of patients had G3 tumors. Multifocal tumors were present in 43.3% of patients, and the tumor diameter of the largest tumor was 4.7 cm (median).
Resection margins were positive in one-quarter of the resected patients, accounting for 223 patients in the ELM group and 265 patients in the ISS group. Based on this, the MEGNA classification classified patients as 0 in 7.4% of patients, I in 25.8% of patients, II in 28.5% of patients, and III in 38.3% of all patients. Each patient was followed up for a median of 18 months.
Complications and Mortality
Of the 511 analyzed patients, 215 (44.1%) experienced at least one complication. Major complications occurred in 119 patients, representing > 50% of all complications and 24.4% of all patients. Severe post-hepatectomy liver failure, grades 2 and 3 biliary leakage, and grades 2 and 3 hemorrhage occurred in 21 (4.3%), 80 (16.4%), and 22 (4.5%) patients, respectively. Another 16 patients died due to various infectious complications following biliary complications. A total of 15 patients required intensive care treatment with reversible problems during the hospital stay, which led to a 90-day overall survival rate of 90.0% in all patients. The median overall survival for all patients was 32.2 months, showing significant differences between MEGNA risk groups, UICC stages, and ELM and ISS categories (Table 1). The MEGNA risk groups had an overall survival of 68% (0), 48% (I), 32% (II), and 19% (III), while UICC stages had an overall survival of 70% (Ia), 54% (Ib), 42% (II), 28% (IIIa), and 25% (IIIb). Data are displayed in Figs. 1 and 2, and the supplementary figures highlight stratification by T and N status.
Univariable and Multivariable Analysis and Risk Groups
For the univariable analysis, 28 items were tested using the Chi square test. Three different analyses were performed identifying predictors for 90-day survival, overall survival, and the occurrence of severe (grade II and III) post-hepatectomy liver failure (Table 2). The items that delivered a p value< 0.1 were regarded as good predictors and were entered into the multivariable analysis. By multivariable analysis, post-hepatectomy liver failure was detected as a significant predictor for 90-day survival (hazard ratio [HR] 10.3, 95% confidence interval [CI] 3.97–26.7; p <0.01). Overall survival was predicted by post-hepatectomy liver failure (HR 5.07, 95% CI 2.93–8,78; p <0.01) and anemia prior to surgery (HR 1.54, 95% CI 0.61–3.87; p <0.01), and severe liver failure was predicted by the necessity for transfusion within 24 h of surgery (HR 4.33. 95% CI 1.22–15.4; p = 0.02), reflecting post-hepatectomy hemorrhage (HR 29.2, 95% CI 6.82–124.6; p <0.01). Data are displayed in Table 2.
Discussion
To the best of our knowledge, this is currently the largest ever published multicentric German cohort in hepatobiliary surgery. By classifying the operated patients with the MEGNA score that was proposed by Raoof et al., we confirmed their findings and usefulness of the MEGNA sore in a cohort of 488 patients in a non-US cohort of patients undergoing surgery for ICC.3 Overall survival data at 5 years were slightly better in the German cohort (0: 68%; I: 48%; II: 32%; III: 19%) when compared with the US cohort (0: 61%; I: 35%; II: 20%; III: 0%). However, data in the original publication were classified in accordance with the 6th and 7th editions of the AJCC for ICC, whereas in this study, the 8th edition of the AJCC for ICC was applied, which may have led to the slight shift in prognosis.16 The MEGNA score, which scores 1 point each for patients over 60 years of age, multifocal tumors, G3 tumor, and T4 and N + tumors, delivers a good discrimination for the patient’s long-term prognosis. As guidelines recommend that a patient should be operated, when surgically resectable,4,6 the MEGNA score adds up tumor-specific items and a patient-specific item (age) that can be used in the decision-making process of an elderly population.
In addition to the above findings, the present analysis helped to identify prognostic factors for early outcome (severe liver failure) and the reasons for severe liver failure (severe hemorrhage, transfusion, and biliary leakage), as well as long-term predictors (anemia prior to surgery). Although various items were significantly associated with short-term outcome after resection, only liver failure remained as a determinant of 90-day survival. However, the only risk factors for severe liver failure were biliary leakage and hemorrhage. These findings are in major agreement with a recent systematic review by Ray et al.,19 which highlighted, in particular, perioperative blood loss and intra-abdominal infections, such as biliary leakages and renal impairment, as driving factors for post-hepatectomy liver failure.
Importantly, anemia was associated with long-term, but not short-term, outcome. In a recent publication by our group, Keding et al. found a strong correlation of pretreatment anemia with late outcome.13 Basically, anemia leads to late-term effects that are currently not well understood. However, the findings of the previously published data were reproducible in another independent cohort of patients, which supports the validity of the data. Correction of presurgical anemia is currently recommended by an expert panel in patient blood management, but further academic exploration is required to identify cohorts that have modifiable anemia.20
Notably, we excluded nodal status from the multivariable analysis, although there was a strong association with survival. However, nodal status is part of the MEGNA score and thus may interact during analysis. The MEGNA score was a strong predictor of overall survival when excluded from the analysis. In one of their recent publications, Pawlik and coworkers found that the lymphadenectomy rate had increased from 44 to 82% over the last years and that systematic lymphadenectomy is associated with better prediction of the prognosis. In the current publication, the lymphadenectomy rate was over 85% for a time period of more than 10 years, which reflects the long-term established surgical oncological quality at German academic centers for hepatobiliary surgery.5
Critically reviewing the literature, network publishing cooperation among German academic surgical hepatobiliary centers is rare and is mostly achieved by cooperation of the transplanting centers.21,22 Therefore, this detail is one of our major accomplishments and is a model for future sustainability in national publication strategies. To cooperate creates transparency and scalability, and creates knowledge about treatment patterns in a particular environment.23 It helps to put the data into a context on any scale (e.g. the center, (inter-)nationally, highly vs. normally specialized centers, etc.), enables the detection of weaknesses, and displays particular strengths. It promotes future cooperation, fosters new research ideas, and creates working groups.
Limitations
This was a retrospective analysis of risk factors from multiple sites in Germany without external data audit; thus, selection bias cannot be excluded. However, this study constitutes a protocol-based collection of all consecutive cases. A structured database for data entry reduced the heterogeneity of data collection. Moreover, the first-time formation of a dedicated surgical group with international leaders in hepatobiliary surgery suggests high motivation for high-quality output.
Conclusions
This analysis confirmed the validity of the MEGNA score to estimate prognosis in ICC patients in a German cohort. Long-term survival of more than 65% of patients can be achieved in selected groups. If a patient is surgically, oncologically, and functionally resectable, resection should be performed. Importantly, patients in this analysis had a twofold longer median overall survival (32 vs. 15 months) than palliatively treated patients in the ABC 01-03 clinical trials with liver-limited disease. Moreover, the worst prognostic group (MEGNA 3, 19% at 5 years) still had a better overall survival than the palliative chemotherapy group at 3 years (0%).24 Correction of anemia may be of further benefit for patients undergoing liver resection for ICC. Systematic lymphadenectomy has a pivotal role for estimation of the long-term prognosis of patients. Perioperative liver failure remains a clinical challenge and contributes to a relevant number of perioperative deaths.
References
Statistisches Bundesamt. Krankenhausstatistik-Diagnosedaten der Patienten und Patientinnen in Krankenhäusern, Statistisches Bundesamt.
Filmann N, Walter D, Schadde E, et al. Mortality after liver surgery in Germany. Br J Surg. 2019;106(11):1523–9.
Raoof M, Dumitra S, Ituarte PHG, et al. Development and validation of a prognostic score for intrahepatic cholangiocarcinoma. JAMA Surg. 2017;152:e170117.
Khan SA, Davidson BR, Goldin RD, et al. Guidelines for the diagnosis and treatment of cholangiocarcinoma: an update. Gut. 2012;61:1657–69.
Zhang X-F, Chakedis J, Bagante F, et al. Trends in use of lymphadenectomy in surgery with curative intent for intrahepatic cholangiocarcinoma. Br J Surg. 2018;105:857–66.
Bridgewater J, Galle PR, Khan SA, et al. Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma. J Hepatol. 2014;60:1268–89.
Belgihiti J, Clavien PA, Gadzijev E, et al. The Brisbane 2000 terminology of liver anatomy and resections. HPB (Oxford). 2000;2:333–9.
Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Rahbari NN, Garden OJ, Padbury R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011;149:713–24.
Koch M, Garden OJ, Padbury R, et al. Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 2011;149:680–8.
Rahbari NN, Garden OJ, Padbury R, et al. Post-hepatectomy haemorrhage: a definition and grading by the International Study Group of Liver Surgery (ISGLS). HPB (Oxford). 2011;13:528–35.
Chawla LS, Amdur RL, Amodeo S, et al. The severity of acute kidney injury predicts progression to chronic kidney disease. Kidney Int. 2011;79:1361–9.
Keding V, Zacharowski K, Bechstein WO, et al. Patient Blood Management improves outcome in oncologic surgery. World J Surg Oncol. 2018;16:159.
Meybohm P, Fischer DP, Geisen C, et al. Safety and effectiveness of a Patient Blood Management (PBM) program in surgical patients: the study design for a multi-centre prospective epidemiologic non-inferiority trial. BMC Health Serv Res. 2014;14:576.
Meybohm P, Herrmann E, Steinbicker AU, et al. Patient blood management is associated with a substantial reduction of red blood cell utilization and safe for patient’s outcome: a prospective, Multicenter cohort study with a noninferiority design. Ann Surg. 2016;264:203–11.
Kim Y, Moris DP, Zhang X-F, et al. Evaluation of the 8th edition American Joint Commission on Cancer (AJCC) staging system for patients with intrahepatic cholangiocarcinoma: a Surveillance, Epidemiology, and End Results (SEER) analysis. J Surg Oncol. 2017;116:643–50.
Spolverato G, Kim Y, Alexandrescu S, et al. Is hepatic resection for large or multifocal intrahepatic cholangiocarcinoma justified? Results from a Multi-Institutional Collaboration. Ann Surg Oncol. 2015;22:2218–25.
Hyder O, Marques H, Pulitano C, et al. A nomogram to predict long-term survival after resection for intrahepatic cholangiocarcinoma: an Eastern and Western experience. JAMA Surg. 2014;149:432–8.
Ray S, Mehta NN, Golhar A, et al. Post hepatectomy liver failure—a comprehensive review of current concepts and controversies. Ann Med Surg. 2018;34:4–10.
Mueller MM, Van Remoortel H, Meybohm P, et al. Patient blood management: recommendations from the 2018 Frankfurt Consensus Conference. JAMA. 2019;321:983–97.
Hildebrand T, Pannicke N, Dechene A, et al. Biliary strictures and recurrence after liver transplantation for primary sclerosing cholangitis: a retrospective multicenter analysis. Liver Transplant. 2016;22:42–52.
Krawczyk M, Grąt M, Adam R, et al. Liver transplantation for hepatic trauma: a study from the European Liver Transplant Registry. Transplantation. 2016;100:2372–81.
Guise J-M, Savitz LA, Friedman CP. Mind the gap: putting evidence into practice in the era of learning health systems. J Gen Intern Med. 2018;33:2237–9.
Lamarca A, Ross P, Wasan HS, et al. Advanced intrahepatic cholangiocarcinoma: post hoc analysis of the ABC-01, -02 and -03 clinical trials. J Natl Cancer Inst. Epub 11 May 2019. https://doi.org/10.1093/jnci/djz071.
Funding
No funding was received for this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Andreas A. Schnitzbauer, Johannes Eberhard, Fabian Bartsch, Stefan M. Brunner, Güralp O. Ceyhan, Dirk Walter, Helmut Fries, Sabine Hannes, Andreas Hecker, Jun Li, Karl Oldhafer, Nuh Rahbari, Falk Rauchfuss, Hans J. Schlitt, Utz Settmacher, Gregor Stavrou, Jürgen Weitz, Hauke Lang, Wolf O. Bechstein and Felix Rückert declare they have no conflict of interests.
Approval
The Institutional Review Board of the Medical Faculty Mannheim of the University of Heidelberg provided approval for this project in April 2016 (2016-816R-MA).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Schnitzbauer, A.A., Eberhard, J., Bartsch, F. et al. The MEGNA Score and Preoperative Anemia are Major Prognostic Factors After Resection in the German Intrahepatic Cholangiocarcinoma Cohort. Ann Surg Oncol 27, 1147–1155 (2020). https://doi.org/10.1245/s10434-019-07968-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07968-7