Abstract
Background
Multifocal papillary thyroid microcarcinoma (PTMC) has been associated with poor outcomes; however, we often encounter pathologically confirmed unilateral multifocal PTMC after surgery. To date, no consensus on the proper surgical extent for patients with this form of PTMC has been reported.
Objective
The aim of this study was to analyze the effect of the type of surgical treatment on disease recurrence in patients with unilateral multifocal PTMC.
Methods
We retrospectively analyzed data from 255 patients with unilateral, multifocal, node-negative PTMC between March 1999 and December 2012. We evaluated two groups of patients: those who underwent unilateral lobectomy (Group I, n = 127) and those who underwent total thyroidectomy (Group II, n = 128). During the follow-up period, which lasted a median of 94.8 months, we assessed locoregional recurrence (LRR).
Results
There was no statistically significant difference between the two groups with regard to LRR at follow-up (3.15% for Group I vs. 0.78% for Group II; p = 0.244). The association between the type of surgical treatment and LRR remained nonsignificant after adjusting for potential confounders such as age, tumor size, microscopic extrathyroidal extension, and lymphovascular invasion (p = 0.115). During follow-up, the incidence of transient hypocalcemia (0% vs. 8.6%; p = 0.001) and vocal fold paralysis (1.6% vs. 9.4%; p = 0.011) was higher in Group II than in Group I.
Conclusions
Even though randomized controlled trials are the only option to obtain a definitive answer to this question, unilateral lobectomy may be a safe operative option for selected patients with unilateral, multifocal, node-negative PTMC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Papillary thyroid microcarcinoma (PTMC) is defined as papillary thyroid carcinoma (PTC) that is ≤ 1 cm in greatest diameter, in accordance with the classification of the World Health Organization.1 The incidence of PTMC has been rapidly increasing, mainly due to the widespread use of high-resolution ultrasonography.2
Tumor multifocality is not an unusual finding in PTMC. Multifocality has been associated with an increased risk of gross extrathyroidal extension (ETE), cervical lymph node (CLN) metastasis, persistent local disease after initial treatment, regional recurrence, and distant metastasis in patients with PTMC.3,4,5 The frequency of multifocal PTMC has been reported to be 20–40%, and patients with multifocal PTMC are frequently managed with more aggressive treatment than those with solitary PTMC].5,6,7,8,9
The local surgical treatment options for PTMC are total thyroidectomy or unilateral lobectomy. According to the American Thyroid Association (ATA) guidelines published in 2016, the extent of initial thyroid surgery probably has little impact on disease-specific survival in properly selected low- to intermediate-risk patients (low-risk patients may have intrathyroidal PTMC with solitary or multifocal tumors, and intermediate-risk patients may have multifocal PTMC ETE).10 However, for multifocal PTMC, although total thyroidectomy is obviously associated with the lowest rates of recurrence during long-term follow-up, unilateral lobectomy is also a reasonable management strategy since completion surgery is quite effective in patients who experience recurrence after unilateral lobectomy.10
In many PTMC patients, multiple tumor foci in the unilateral thyroid gland are diagnosed on preoperative radiologic evaluation. However, in clinical practice, we often encounter pathologically confirmed unilateral multifocal PTMC that has been missed by preoperative radiologic evaluation after unilateral lobectomy in patients with PTMC. Although several studies have reported a higher rate of contralateral tumors when unilateral multifocality is present,6,11,12 if the pathological analysis reveals unilateral, multifocal, node-negative PTMC, the surgeon cannot make a strong recommendation for completion thyroidectomy because of the excellent prognosis and potential lifelong discomfort from associated complications. Furthermore, in the latest guidelines from the ATA, the extent of surgery has still not been clearly determined for unilateral, multifocal, node-negative PTMC.10 Therefore, the aim of this study was to analyze the effect of the type of surgical treatment (unilateral lobectomy vs. total thyroidectomy) on disease recurrence in patients with unilateral, multifocal, node-negative PTMC.
Methods
Patient Identification
This retrospective study was approved by the Institutional Review Board at our institution (VC15RISI0004). Patients with PTMC who had undergone curative thyroid cancer surgery (unilateral lobectomy vs. total thyroidectomy) were identified at the Department of Surgery, St. Vincent’s Hospital, The Catholic University, between March 1999 and December 2012.
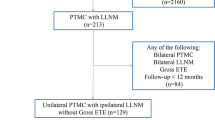
All patients had a diagnosis of unilateral multifocal PTMC. Unilateral multifocality was defined as two or more PTMC lesions present within only the ipsilateral lobe, which was confirmed by a head and neck pathologist at St. Vincent’s Hospital, The Catholic University, Korea. Patients were ineligible if they met the following criteria: tumor size > 1 cm, bilateral multifocality, non-PTC carcinomas (follicular, medullary, anaplastic), high-risk histological subtypes (tall cell, columnar, and solid variants of PTC), gross ETE, CLN (central and lateral) metastasis according to the final pathological reports, postoperative radioactive iodine (RAI) therapy, and the presence of distant metastasis. Figure 1 provides a detailed list of the exclusion cases.
Preoperative Assessment and Surgical Methods
All patients underwent preoperative ultrasonography to determine the presence of tumor multiplicity and central or lateral CLN metastasis. Preoperative ultrasound-guided fine needle aspiration cytology was performed for any clinically suspicious thyroid nodules, CLNs, and contralateral nodules.
Based on the inclusion criteria for this cohort, all patients had stage I disease (T1N0M0) according to the 7th Edition of the American Joint Committee on Cancer (AJCC) staging system13 and had a low- to intermediate-risk of recurrence according to the ATA guidelines.10 Since patients were eligible for unilateral lobectomy or total thyroidectomy, the choice of surgical method was determined by the patient after discussion with a surgeon regarding other individualized risk factors, such as follow-up compliance, family history, sex, and tumor multiplicity. Therapeutic CLN dissection was performed whenever abnormal lymphadenopathy was suspected during the preoperative or intraoperative examination.
Postoperative Follow-Up
After the initial surgical treatment, all patients underwent regular follow-up every 6–12 months. Follow-up studies consisted of physical examinations; cervical ultrasonography; thyroid function testing; measurement of total serum calcium (Ca), intact parathyroid hormone (iPTH), and thyroglobulin (Tg) levels; computed tomography of the neck; or an RAI scan.
Transient hypocalcemia was defined as complete recovery from symptomatic and biochemical hypocalcemia within 12 months of thyroidectomy, mandating the use of transient Ca supplementation. Permanent hypocalcemia means failure of recovery from the hypocalcemia more than 12 months from thyroidectomy. Transient vocal fold paralysis was defined as satisfactory regain of vocal quality determined by vocal cord visualization with indirect laryngoscope or functional evaluation of voice quality within 6 months after thyroidectomy. Permanent vocal fold paralysis was defined as the complete and irreversible loss of vocal fold function.
The primary endpoint of the study was recurrence-free survival (RFS), defined as the time from the initial surgery for primary PTMC to the first event of locoregional recurrence (LRR). During follow-up, LRR was defined as a newly detected malignant lesion in the thyroid bed or the contralateral lobe or metastatic lymph nodes > 6 months after the initial surgery that was proven to be malignant by cytology and surgical excision.
Statistical Analysis
Descriptive statistics were used to summarize the study data. Associations among categorical variables were evaluated using the independent t test and Fisher’s exact or Chi square tests as appropriate. A logistic regression model was developed to examine the association between the surgical method and recurrence after adjusting for multiple confounders, such as age, tumor size, surgery type, microscopic ETE, and lymphovascular invasion. The cumulative risk of RFS was estimated using the Kaplan–Meier method. Log-rank tests were performed to compare the recurrence curves. The analyses were performed using SPSS software version 17.0.1 (SPSS Inc., Chicago, IL, USA). In all statistical analyses, a two-tailed p value < 0.05 was considered statistically significant. The follow-up time was calculated from the time of surgery to the date of the last follow-up.
Results
Patients and Baseline Clinicopathologic Characteristics
Between March 1999 and December 2012, 1602 patients with PTMC underwent curative thyroid cancer surgery at out institution. Multifocal PTMC, which was defined as two or more PTMC lesions being presented within an ipsilateral lobe in one or both lobes, was reported in 428 patients (26.72%). According to the inclusion criteria, 255 patients with unilateral multifocal PTMC were included in the cohort. Of 255 patients, 127 (49.80%) underwent unilateral lobectomy with ipsilateral CLN dissection (Group I), and 128 patients (50.20%) underwent total thyroidectomy with ipsilateral CLN dissection (Group II) (Fig. 1). Occult multifocality that was discovered on final pathology preoperatively undetected multifocal lesions in the ipsilateral lobe, was present in 67/255 patients (26.3%) (Table 1).
The characteristics of patients in Groups I and II are shown in Table 1. Among all patients, the median age was 49 years (range 25–76), and the median diameter of the thyroid cancer was 6.49 mm (range 1–10). There were no statistically significant differences in the size of the primary or secondary tumor or in the total tumor diameter. The proportions of patients with tumors ≤ 1 cm (55.9 vs. 53.9%; p = 0.802) or ≤ 2 cm (94.5 vs. 92.1%; p = 0.617) in total tumor diameter were not statistically significant between the groups.
Patients who underwent total thyroidectomy were older and more commonly had microscopic ETE than those who underwent unilateral lobectomy. However, there were no statistically significant differences in the histological papillary carcinoma subtype between the groups. Furthermore, there were no statistically significant differences in tumor laterality, number of tumors in one lobe, lymphovascular invasion, or duration of follow-up (Table 1).
Follow-Up and Tumor Recurrence
At the final follow-up, the median follow-up duration was 94.8 months (range 24–209). Among the entire cohort, LRR developed in five patients (1.96%). In Group I, 4 (3.15%) of the 127 patients developed LRR during follow-up, including 3 patients with contralateral lobe recurrence and 1 patient with contralateral lobe, ipsilateral lateral neck lymph node recurrence. In these patients, the median time to recurrence was 43 months (range 24–172). In Group II, only one patient (0.78%) of the 128 patients developed local operative bed recurrence at 55 months after primary curative thyroid cancer surgery. Distant metastases were not identified in any of the five patients with LRR, either at the time of recurrence or during subsequent or ongoing follow-up. There were no cases of mortality.
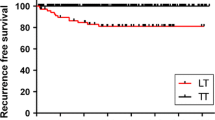
Kaplan–Meier curves were plotted to investigate the differences in RFS between the two groups. Figure 2 shows that there was no statistically significant difference between the two groups with regard to LRR during follow-up (p = 0.244).
Univariate and multivariate analyses were performed to determine whether the type of surgical treatment (unilateral lobectomy vs. total thyroidectomy) was associated with RFS in patients with unilateral, multifocal PTMC. The association between the type of surgical treatment and RFS remained nonsignificant after adjusting for potential confounders (hazard ratio [HR] 0.153, 95% confidence interval [CI] 0.015–1.578; p = 0.115). Furthermore, this result was consistent when the primary tumor size was > 0.5 cm (HR 0.166, 95% CI 0.014–1.936; p = 0.152) and the total tumor diameter was > 1.0 cm (HR 0.200, 95% CI 0.017–2.335; p = 0.199) (Table 2).
During follow-up, the incidence of transient hypocalcemia (0% vs. 8.6%; p = 0.001) and vocal fold paralysis (1.6% vs. 9.4%; p = 0.011) was significantly higher in Group II than in Group I. However, we found only one patient with permanent hypocalcemia in Group II, and permanent vocal fold paralysis was not represented in both groups.
Discussion
In this study, we investigated the relationship between the extent of surgery and prognosis in unilateral, multifocal, node-negative PTMC. The results of this retrospective study suggest that unilateral lobectomy may be a safe operative option for these patients.
Multifocality is the unique feature of PTC, and the rate of multifocality is reported to be 50–78%.14,15 Previous studies have suggested that multiple tumor foci are the result of intraglandular metastasis from a single primary tumor spread via intraglandular lymphatics.16,17 Although the clonal origin of multifocal PTCs has not been completely settled, recent modern molecular techniques have reported that multifocal PTCs are multiple synchronous primary tumors arising from independent clones.18,19 However, many studies have reported that multifocal PTCs are associated with increased risks of CLN metastasis, distant metastasis, and persistent local disease after initial treatment.20,21,22 Therefore, aggressive treatment, such as total thyroidectomy, central neck dissection, or postoperative RAI ablation, is suggested as an adequate treatment for multifocal PTCs. Concordantly, in PTMC, multifocality has been reported in 20–40% of patients and has been associated with increased risks of gross ETE, CLN metastasis, LRR, or distant metastasis in studies evaluating PTMC alone.5,6,7,8,9
However, the definition of multifocality is obscure and different according to each study.3,4,20,21 For example, if multifocality is defined as the presence of two or more tumor foci in the resected thyroid gland, the meaning can be subdivided into either unilateral multifocality (two or more lesions within the ipsilateral lobe only), bilateral multifocality (two or more lesions within the ipsilateral lobe and one or more lesions within the contralateral lobe) or bilaterality (one lesion within each lobe) according to the tumor location. In this regard, even the recent international consensus guidelines do not define multifocality by laterality as either ipsilateral (unilateral) or bilateral.10 Although total thyroidectomy is the only surgical treatment for bilateral multifocal PTMC, unilateral lobectomy may be an additional surgical option for unilateral multifocal PTMC. In particular, if there are no other serious risk factors, such as CLN metastasis, unilateral lobectomy may be a more reasonable treatment option for patients with unilateral multifocal PTMC with no clinical burden of potential CLN metastasis.
Recently, several studies have tried to uncover the optimal surgical extent for PTMC including multifocality.4,6,9,11,23,24 However, due to the following limitations, no conclusions have been reached through these studies regarding the optimal surgical extent for unilateral multifocal PTMC. First, no randomized controlled trial has been performed that can definitively delineate the benefits of one approach over the other for patients with unilateral multifocal PTMC patients in terms of recurrence/survival. However, such randomized controlled trials seem to be almost impossible because the majority of PTMC patients have excellent survival with very low LRR rates, even if they have unilateral multifocal PTMC. Furthermore, these studies included multiple confounding factors (such as CLN metastasis, gross ETE, an obscure definition of multifocality, and RAI ablation) that can affect recurrence/survival.
We focused our attention on unilateral, multifocal, node-negative PTMC because the indolent course of this type of PTMC requires that the question of optimal surgical treatment be addressed. We reported only four patients who developed a contralateral lobe recurrence in Group I (3.15%), and one patient in Group II (0.78%), after a median follow-up of 94.8 months (range 24–209). However, we would like to emphasize that although both groups presented excellent results in terms of RFS, transient hypocalcemia and vocal fold paralysis, which are the most important complications, were, as expected, higher among those who underwent total thyroidectomy than those who underwent unilateral lobectomy. Considering these results, patients with unilateral, multifocal, node-negative PTMC represent a very low-risk cluster and may benefit from a less aggressive surgical approach to avoid unnecessary morbidity. However, considering that most recurrences are on the contralateral lobe, meticulous preoperative evaluation using ultrasonography for the contralateral lobe is important to determine the optimal extent of surgery for these patients.
In this study, the association between the type of surgical treatment and RFS remained nonsignificant in patients with a primary tumor size > 0.5 cm or a total tumor diameter > 1.0 cm. Although previous studies have reported that a primary tumor size > 0.5 cm or a total tumor diameter > 1.0 cm may be used for predicting CLN metastasis,3,25 these results were not in accordance with the findings of our study including patients with unilateral, multifocal, node-negative PTMC.
Our study has some limitations due to its retrospective design. The number of patients with recurrent disease during follow-up was relatively small because we only included patients with unilateral, multifocal, node-negative PTMC. However, this approach was inevitable because we wanted to enroll patients who did not have any of several confounding factors (such as CLN metastasis, gross ETE, and RAI ablation) that can affect recurrence/survival. In addition, the follow-up period of our study may not have been sufficient to evaluate patients with late recurrences, which can occur up to 10 years after the initial treatment. Thus, multicenter research and long-term follow-up are needed to better understand the optimal surgical extent for unilateral, multifocal, node-negative PTMC. Nevertheless, this is the first report to evaluate the effect of the type of surgical treatment (unilateral lobectomy vs. total thyroidectomy) on disease recurrence in patients with unilateral, multifocal, node-negative PTMC. We believe this finding provides important insights into the optimal surgical extent for unilateral, multifocal, node-negative PTMC.
Conclusions
The decision regarding the optimal extent of surgery for patients with multifocal PTMC should be made after careful deliberation. However, we found that the type of surgical treatment (unilateral lobectomy vs. total thyroidectomy) was not associated with RFS in patients with unilateral, multifocal PTMC. Because recurrence in the contralateral remnant lobe can be safely managed by completion thyroidectomy, unilateral lobectomy may be a safe operative option for patients with unilateral, multifocal, node-negative PTMC.
References
Hedinger C, Williams ED, Sobin LH. The WHO histological classification of thyroid tumors: a commentary on the second edition. Cancer. 1989;63:908–11.
Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA. 2006; 295:2164–67.
Kim SK, Park I, Woo JW, et al. Predictive factors for lymph node metastasis in papillary thyroid microcarcinoma. Ann Surg Oncol. 2016;23:2866–73.
So YK, Kim MW, Son YI. Multifocality and bilaterality of papillary thyroid microcarcinoma. Clin Exp Otorhinolaryngol. 2015;8:174–8.
Mercante G, Frasoldati A, Pedroni C, et al. Prognostic factors affecting neck lymph node recurrence and distant metastasis in papillary microcarcinoma of the thyroid: results of a study in 445 patients. Thyroid. 2009;19:707–16.
Connor MP, Wells D, Schmalbach CE. Variables predictive of bilateral occult papillary microcarcinoma following total thyroidectomy. Otolaryngol Head Neck Surg. 2011;144:210–5.
Dunki-Jacobs E, Grannan K, McDonough S, Engel AM. Clinically unsuspected papillary microcarcinomas of the thyroid: a common finding with favorable biology? Am J Surg. 2012;203:140–4.
Siassakos D, Gourgiotis S, Moustafellos P, Dimopoulos N, Hadjiyannakis E. Thyroid microcarcinoma during thyroidectomy. Singap Med J. 2008;49:23–5.
Ciuffreda L, De Martino D, Bonfitto N, Scaramuzzi R. Our experience on surgical treatment of papillary thyroid microcarcinoma. G Chir. 2011;32:41–4 (in Italian).
Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26:1–133.
Kim ES, Kim TY, Koh JM, et al. Completion thyroidectomy in patients with thyroid cancer who initially underwent unilateral operation. Clin Endocrinol (Oxf). 2004;61:145–8.
Pasieka JL, Thompson NW, McLeod MK, Burney RE, Macha M. The incidence of bilateral well-differentiated thyroid cancer found at completion thyroidectomy. World J Surg. 1992;16:711–6 (discussion 716–7).
Edge SB, American Joint Committee on Cancer 2010. AJCC Cancer Staging Manual. 7th edn. New York: Springer; 2010.
Katoh R, Sasaki J, Kurihara H, Suzuki K, Iida Y, Kawaoi A. Multiple thyroid involvement (intraglandular metastasis) in papillary thyroid carcinoma. A clinicopathologic study of 105 consecutive patients. Cancer. 1992;70:1585–90.
Gerfo PL, Chabot J, Gazetas P. The intraoperative incidence of detectable bilateral and multicentric disease in papillary cancer of the thyroid. Surgery. 1990;108:958–62 (discussion 962–53).
Iida F, Yonekura M, Miyakawa M. Study of intraglandular dissemination of thyroid cancer. Cancer. 1969;24:764–71.
Russell WO, Ibanez ML, Clark RL, White EC. Thyroid carcinoma. Classification, intraglandular dissemination, and clinicopathological study based upon whole organ sections of 80 glands. Cancer. 1963;16:1425–60.
Shattuck TM, Westra WH, Ladenson PW, Arnold A. Independent clonal origins of distinct tumor foci in multifocal papillary thyroid carcinoma. N Engl J Med. 2005;352:2406–12.
Park SY, Park YJ, Lee YJ, et al. Analysis of differential BRAF(V600E) mutational status in multifocal papillary thyroid carcinoma: evidence of independent clonal origin in distinct tumor foci. Cancer. 2006;107:1831–8.
Kim HJ, Sohn SY, Jang HW, Kim SW, Chung JH. Multifocality, but not bilaterality, is a predictor of disease recurrence/persistence of papillary thyroid carcinoma. World J Surg. 2013;37:376–84.
Kim KJ, Kim SM, Lee YS, Chung WY, Chang HS, Park CS. Prognostic significance of tumor multifocality in papillary thyroid carcinoma and its relationship with primary tumor size: a retrospective study of 2,309 consecutive patients. Ann Surg Oncol. 2015;22:125–31.
Joseph KR, Edirimanne S, Eslick GD. Multifocality as a prognostic factor in thyroid cancer: a meta-analysis. Int J Surg. 2018;50:121–5.
Donatini G, Castagnet M, Desurmont T, Rudolph N, Othman D, Kraimps JL. Partial thyroidectomy for papillary thyroid microcarcinoma: is completion total thyroidectomy indicated? World J Surg. 2016;40:510–5.
Kim SK, Park I, Woo JW, Lee JH, Choe JH, Kim JH, et al. Total thyroidectomy versus lobectomy in conventional papillary thyroid microcarcinoma: analysis of 8,676 patients at a single institution. Surgery. 2017;161:485–92.
Zhao Q, Ming J, Liu C, Shi L, Xu X, Nie X, Huang T. Multifocality and total tumor diameter predict central neck lymph node metastases in papillary thyroid microcarcinoma. Ann Surg Oncol. 2013;20:746–52.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Ye Won Jeon, Hong Gi Gwak, Seung Taek Lim, Jean Schneider, and Young Jin Suh have no conflicts of interest to report in relation to this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jeon, Y.W., Gwak, H.G., Lim, S.T. et al. Long-Term Prognosis of Unilateral and Multifocal Papillary Thyroid Microcarcinoma After Unilateral Lobectomy Versus Total Thyroidectomy. Ann Surg Oncol 26, 2952–2958 (2019). https://doi.org/10.1245/s10434-019-07482-w
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07482-w