Abstract
Background
Patients undergoing oncologic surgery are at risk for persistent postoperative opioid use. As a quality improvement initiative, this study sought to characterize provider perceptions regarding opioid-prescribing after oncologic procedures.
Methods
Surgical oncology attending physicians, clinical fellows, and advanced practice providers (APPs) at a high-volume cancer center were surveyed before and after educational sessions focusing on the opioid epidemic with review of departmental data.
Results
The pre-education response rates were 72 (70%) of 103: 22 (65%) of 34 attending physicians, 19 (90%) of 21 fellows, and 31 (65%) of 48 APPs. For five index operations (open abdominal resection, laparoscopic colectomy, wide local excision, thyroidectomy, port), the fellows answered that patients should stop receiving opioids sooner than recommended by the attending surgeons or APPs. For four of five procedures, the APPs recommended higher discharge opioid prescriptions than the attending surgeons or fellows. Almost half of the providers (n = 46, 45%) responded to both the pre- and post-education surveys. After the intervention, the providers recommended lower numbers of opioid pills and indicated that patients should be weaned from opioids sooner for all the procedures. Compared with pre-education, more providers agreed post-education that discharge opioid prescriptions should be based on a patient’s last 24 h of inpatient opioid use (83 vs 91%; p = 0.006). The providers who did not attend a session showed no difference in perceptions or recommendations at the repeat assessment.
Conclusions
Variation exists in perioperative opioid-prescribing among provider types, with those most involved in daily care and discharge processes generally recommending more opioids. After education, providers lowered discharge opioid recommendations and thought patients should stop receiving opioids sooner. The next steps include assessing for quantitative changes in opioid-prescribing and implementing standardized opioid prescription algorithms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The death rate from prescription opioid use has quadrupled in the last 20 years.1 It is estimated that 1 of every 25 Americans currently uses opioids daily, a trend that started more than a decade ago as the number of opioid prescriptions began increasing by 35% annually from 2000 to 2009.2 Surgeons and surgical care providers play a critical role in this epidemic because opioids are frequently prescribed to alleviate postoperative pain. Prescribing opioids to naïve patients in the perioperative period can lead to long-term use, with rates of new persistent opioid use as high as 6.5%.3,4 For cancer patients undergoing oncologic resection, up to 15% of previously opioid-naïve patients become persistent users.5,6
Efforts such as Enhanced Recovery After Surgery (ERAS) have been shown to decrease inpatient postoperative opioid use,7,8,–9 but have done little to address the volume of opioids prescribed at discharge.10 Recent trends in postoperative opioid prescriptions show considerable variation in the quantity of opioids prescribed for a given procedure and that surgeons often over-prescribe.11,12,–13 This likely translates to increased rates of chronic opioid use and, more directly, results in excess opioid dissemination to the public. These and related findings have led to the development of opioid-prescribing guidelines for providers.14,15 Currently, few guidelines apply specifically to patients undergoing oncologic resection despite the increased risk of long-term opioid use for this patient population.
As a quality improvement effort with the ultimate goal of creating opioid-prescribing guidelines for surgical oncology, we aimed to evaluate provider understanding of the current opioid epidemic and perceptions surrounding opioid use. Furthermore, we sought to educate providers about both the national opioid crisis and our own institutional practices and to assess the effectiveness of our educational session via pre- and post-education surveys.
Methods
Study Population
Study participants were recruited from the Department of Surgical Oncology at the University of Texas MD Anderson Cancer Center in August 2018. All attending surgeons, clinical fellows, and advanced practice providers (APPs) within the department were surveyed. This study was approved by the Quality Improvement Assessment Board (QIAB).
Study Design and Survey Development
The study consisted of two online surveys administered via Research Electronic Data Capture (REDCap) before and after an educational intervention specific to perioperative opioid practices (Supplemental Appendices A and B).16 Both surveys addressed opioid-prescribing habits, perceptions surrounding perioperative pain management, and general knowledge related to the opioid epidemic. Five oncologic operations were included in the survey to assess opioid-prescribing habits: open abdominal resection, laparoscopic colectomy, wide local excision with sentinel lymph node biopsy, total thyroidectomy, and port placement. The post-intervention survey repeated these questions and included additional fields regarding plans to change prescribing habits.
The survey tool was developed by the research team (authors H.A.L., T.E.N., T.J.V., C.D.T.), then vetted by an additional attending surgeon, a Complex General Surgical Oncology (CGSO) fellow, and an APP. The first survey was administered during a 2-week period preceding the intervention. The educational sessions took place during 1 week, and the follow-up survey was sent approximately 2 weeks after the intervention during a 2-week period. All surveys and educational sessions took place during the month of August 2018.
Educational Intervention
The intervention consisted of an educational session held in three different settings to ensure adequate availability and exposure to each provider group. Because the intervention took place at the beginning of the academic year, one session was directed toward incoming fellows. A second educational session was given at the monthly Surgical Physician Assistant Continuing Education (SPACE) conference. The final session was a departmental grand rounds presentation. A video recording of the grand rounds presentation was subsequently disseminated to the department via email.
Presentations were given by a CGSO fellow (author T.E.N.) and an attending surgical oncologist (author C.D.T.). Each 1-h interactive session included background information on the extent of the opioid epidemic, both generally and specific to the cancer population. A retrospective cohort study of opioid discharge practices using departmental data was a key component of each presentation so that providers could quantify, for the first time, our actual current practice.17 Finally, future prospective quality improvement and research projects targeting perioperative opioid practices were discussed.
Statistical Analyses
Categorical variables, shown as numbers and percentages, were compared using Chi square or Fisher’s exact test, as appropriate. Continuous variables, shown as median and interquartile range (IQR), were compared using the Wilcoxon rank-sum or the Kruskal–Wallis test. Paired pre- versus post-intervention data were compared with the Wilcoxon signed-rank test or McNemar’s test. All p values were two-sided, and p values lower than 0.05 were statistically significant. All statistical analyses were performed using JMP Pro software (version 12; SAS Institute Inc., Cary, NC, USA).
Results
Study Participants: Pre-education Cohort
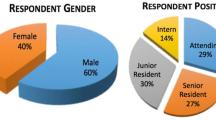
For the pre-education survey, 72 of 103 providers participated, for an overall response rate of 70%. The breakdown of provider types showed 43% APPs, 31% attending surgeons, and 26% fellows. The response rates based on clinical role were 22 (65%) of 34 attending surgeons, 19 (90%) of 21 fellows, and 31 (65%) of 48 APPs.
The details regarding the participants’ clinical role, subspecialty, and years in practice are shown in Fig. 1. The participants were well distributed among the surgical oncology disease-site subspecialties. Among the fellows, 15 (79%) were CGSO fellows and 4 (21%) were non-CGSO subspecialty fellows.
Pre-educational intervention survey participants. A breakdown of respondents’ clinical role, clinical specialty,* and years in practice* are shown. *Clinical specialty and years in practice apply only to attending surgeons and advanced practice practitioners (APPs). Respondents could select more than one specialty if appropriate
Pre-education Opioid Practices, Perceptions, and Knowledge
Before any educational sessions, the participants were surveyed about opioid-prescribing habits and perceptions surrounding opioid use for common oncologic procedures (Table 1). The APPs recommended a higher number of opioid pills than the fellows or the attending surgeons for all procedures except open abdominal resection. The fellows indicated that patients should be weaned from opioids at a shorter postoperative interval than attending surgeons and APPs for all procedures. The fellows also responded with higher perceived patient-reported pain scores at the time of discharge for open abdominal resection. For other procedures, the providers responded similarly regarding pain scores.
A high proportion of all provider types agreed that nonopioid adjuncts decrease opioid use (median total agreement, 100%; IQR, 92–100%) and that regional nerve blocks are useful adjuncts for postoperative pain (96%; IQR, 84–100%). The attending surgeons and fellows had greater agreement than the APPs regarding regional blocks (Table 2). Agreement was slightly lower for basing discharge opioid prescriptions on the last 24 h of inpatient opioid use (80%; IQR, 67–100%). The median agreement was lowest for the statement that patients who do not require opioids in the 24 h before discharge should not receive a discharge opioid prescription (56%; IQR, 30–85%).
When asked which non-opioid adjuncts they use for inpatient management, 62 providers (86%) indicated acetaminophen, 45 (63%) indicated ketorolac, 30 (42%) indicated gabapentin and/or pregabalin, 48 (67%) indicated ibuprofen or another oral NSAID, 26 (36%) indicated celecoxib, and 43 (60%) indicated methocarbamol or cyclobenzaprine. For outpatient management, 60 (83%) of the providers indicated using acetaminophen, 14 (19%) indicated using gabapentin and/or pregabalin, 55 (76%) indicated using ibuprofen or another oral NSAID, 10 (14%) indicated using celecoxib, and 25 (35%) indicated using methocarbamol or cyclobenzaprine.
General knowledge questions also were asked of the providers. Before the intervention, most of the providers correctly classified fentanyl (93%) and oxycodone (100%) as opioids. However, 29% of the providers failed to identify tramadol as an opioid. Two of the providers (3%) thought ketorolac is an opioid. Regarding new persistent opioid use among patients undergoing potentially curative oncologic resection, 71 of 72 providers responded, and 34 (48%) chose the correct answer: 10%.5 For the question pertaining to drug overdose deaths, 35 of the providers (49%) chose correctly: 50 to 75%.1
Pre- Versus Post-education Survey Responses
Forty-five percent of providers (46/103) completed both the pre- and post-education surveys. Comparative analysis was performed using only these providers. The group was composed of 39% APPs, 28% attending surgeons, and 33% fellows. The individual provider response rates were 13 (38%) of 34 attending surgeons, 15 (71%) of 21 fellows, and 18 (38%) of 48 APPs. The distribution of clinical specialty and years in practice was similar to that of the larger pre-education cohort. Of the fellows, 11 (73%) were CGSO and 4 (27%) were training in another oncologic subspecialty. Of this group, 27 (46%) attended the grand rounds session, 5 (8%) watched the grand rounds video but did not attend in person, 14 (24%) attended the SPACE session, and 6 (10%) attended the orientation session. Seven of the providers (12%) did not attend any session. Several of the providers attended more than one session.
After education, the respondents answered the same questions regarding opioid needs and prescribing habits for common oncologic procedures. Compared with pre-education, the post-education responses recommended lower numbers of opioid pills for all procedures (Table 3). After the intervention, the providers also responded that patients should be off of opioids sooner for every procedure type. The perceived patient pain scores at discharge were similar. A post hoc subgroup analysis performed for the seven participants who indicated that they did not attend an educational session showed similar pre- versus post-education responses (p > 0.05) for each question for all five procedures.
As in the pre-education survey, most of the providers agreed with the statements regarding non-opioid adjuncts and regional nerve blocks in the post-education survey. When asked about basing discharge opioid prescriptions on the last 24 h of inpatient use, the median agreement for the 46 providers who took both surveys increased from 83% (IQR, 69–100%) to 91% (IQR, 77–100%; p = 0.006). Agreement that patients should not receive a discharge opioid prescription if they did not require opioids during the previous 24 h increased from 58% (IQR, 32–85%) to 77% (IQR, 52–90%; p = 0.008).
Analysis performed on the subgroup of providers who did not attend any session showed that agreement did not change for any of the questions before versus after education. Comparison of those who did and those who did not attend the sessions is shown in Fig. 2. For those who participated in the educational intervention, 96% reported plans to decrease opioid prescriptions compared with only 54% of the non-participants.
Pre- versus post-educational intervention agreement questions based on participation, including responses from only those participants who responded to both the pre- and post-education surveys. Median agreement is shown for each agreement question, with comparisons of pre- and post-intervention values using Wilcoxon’s signed-rank test. Question stems are abbreviated from original survey (Supplementary Appendix B)
For those who completed both surveys, the responses to the repeated knowledge questions were similar (McNemar’s test, p > 0.05). Although not statistically significant, more of the providers responded correctly to both multiple choice questions. Similarly, more of the providers responded correctly that tramadol is an opioid medication on the post-education survey (76–85%; p = 0.157).
Discussion
Given the current opioid crisis, efforts must be made to reduce opioid prescriptions. The perioperative period is an important time for prescribing opioids, with patients undergoing oncologic resection at increased risk for long-term opioid use after surgery.5,6 To acquire a better understanding of provider perceptions related to opioid use after cancer surgery, we surveyed surgical oncology providers at a high-volume comprehensive cancer center and informed the providers about the extent of the opioid problem, focusing on actual institutional data and prospective plans for improvement in a learning health care system model. We found variation in perioperative opioid-prescribing habits among provider types, with those most involved in the daily care and the discharge process recommending more opioids. After educational interventions, the same providers lowered recommended discharge opioid amounts and believed that patients should stop receiving opioids sooner.
Our pre-intervention data regarding provider perceptions of patient-reported postoperative pain and the duration of opioid requirements after various oncologic procedures showed variation among provider types. Specifically, the fellows indicated that patients should be weaned off of opioids sooner than attending surgeons and APPs, whereas APPs recommended higher numbers of opioid pills after every procedure type. This may reflect the amount of time the provider spends with patients at various time points of their perioperative care. For example, APPs generally spend the most time with patients during the index hospitalization (responding to inpatient requests), on the day of discharge (educating patients), and in clinic (responding to refill requests). Fellows perform these tasks less frequently, with requests rarely reaching attending surgeons. Perhaps the increased pill number at discharge indicated by the APPs reflects a more patient-centric prescribing pattern given the increased direct patient contact during this time, erring on the side of overprescription. Also, APPs are more likely to be the providers actually writing the discharge prescriptions. Fellows have the least long-term follow-up with surgical patients given the monthly rotation schedule. This may account for fellows’ perception of shorter postoperative durations of opioid requirement because they deal with refill requests and medicine reconciliations during outpatient visits less frequently. While different patterns were seen in a recent study assessing quantitative opioid discharge prescriptions after general surgery procedures, variation between attending surgeons, trainees, and APPs was also found.18 This variation highlights the importance of involving all types of surgical care providers in educational initiatives. Specific focus on inter-provider communication also would be beneficial. Finally, the key to understanding why provider-prescribing habits differ is determining what motivates providers to prescribe more opioids (e.g., perceived empathy for patients or pragmatic worry for refill requests) and what barriers exist that hinder implementation of opioid reduction strategies.
After our intervention, the providers indicated that they would prescribe lower amounts of discharge opioids and that patients should require them for shorter intervals after surgery for every procedure type. We attribute these findings to our educational sessions.
A unique feature of our presentations was the incorporation of data from our own department in addition to general information regarding the opioid epidemic. Anecdotally, sharing this institution-level data led to increased discussion among the surgical providers on the topic of opioids during this period. Specifically, there was sharing of opioid weaning strategies between services with low opioid use and those on the higher end of the spectrum. This was thought to be clinically relevant given that before the intervention, there was very little general group discussion on this topic. Meanwhile, although small in number, the providers indicating that they did not attend a session showed no change in their opioid-prescribing habits or agreement with opioid-related questions in the post-education survey.
Future planned steps include a repeat survey assessment to understand the long-term effect of our educational intervention. Additionally, we are assessing for quantitative changes in actual opioid-prescribing habits based on procedure type in order to implement standardized multimodal pain management protocols for index operations.
We must acknowledge the possibility of response bias because participants could have answered questions in a manner they thought would be pleasing to the research group. Similarly, the increased publicity that the opioid epidemic has received from the media and in the surgical literature may have played a synergistic role. However, the sessions themselves appeared to have an impact on the participants given that no difference was seen in the perceptions of the nonparticipants. Notably, the nonparticipating providers reported only 54% agreement regarding plans to decrease their opioid-prescribing practices compared with nearly 100% for the participants. Although the relatively small number of participants may have limited this comparison, the provider group that responded to both surveys was representative of our entire cohort with regard to subspecialty and years in practice, and significant differences between the responses still were found. Despite these limitations, this study represents an important step forward in understanding opioid-prescribing patterns and offers a successful example of department-wide opioid education having a clinically relevant impact on provider perceptions.
Conclusions
Perioperative opioid-prescribing habits vary considerably among surgical provider types, with those most involved in daily patient care and discharge processes recommending more opioids. After educational interventions, all provider types lowered the quantity of opioids recommended at discharge and indicated shorter durations of postoperative opioid use. The next steps include assessing for quantitative changes in opioid prescriptions at our institution and implementing inpatient weaning strategies and standardized discharge opioid prescription algorithms.
References
Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths–United States, 2000–2014. MMWR Morb Mortal Wkly Rep. 2016;64:1378–82.
Kenan K, Mack K, Paulozzi L. Trends in prescriptions for oxycodone and other commonly used opioids in the United States, 2000–2010. Open Med. 2012;6:e41–7.
Hah JM, Bateman BT, Ratliff J, Curtin C, Sun E. Chronic opioid use after surgery: implications for perioperative management in the face of the opioid epidemic. Anesth Analg. 2017;125:1733–40.
Brummett CM, Waljee JF, Goesling J, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg. 2017;152:e170504.
Lee JS-J, Hu HM, Edelman AL, et al. New persistent opioid use among patients with cancer after curative-intent surgery. J Clin Oncol. 2017;35:4042–9.
Tuminello S, Schwartz R, Liu B, et al. Opioid use after open resection or video-assisted thoracoscopic surgery for early-stage lung cancer. JAMA Oncol. 2018;4:1611–3.
Alvarez MP, Foley KE, Zebley DM, Fassler SA. Comprehensive enhanced recovery pathway significantly reduces postoperative length of stay and opioid usage in elective laparoscopic colectomy. Surg Endosc. 2015;29:2506–11.
King AB, Spann MD, Jablonski P, Wanderer JP, Sandberg WS, McEvoy MD. An enhanced recovery program for bariatric surgical patients significantly reduces perioperative opioid consumption and postoperative nausea. Surg Obes Relat Dis. 2018;14:849–56. https://doi.org/10.1016/j.soard.2018.02.010.
Grant MC, Sommer PM, He C, et al. Preserved analgesia with reduction in opioids through the use of an acute pain protocol in enhanced recovery after surgery for open hepatectomy. Regional Anesth Pain Med. 2017;42:451–7.
Brandal D, Keller MS, Lee C, et al. Impact of enhanced recovery after surgery and opioid-free anesthesia on opioid prescriptions at discharge from the hospital: a historical-prospective study. Anesth Analg. 2017;125:1784–92.
Thiels CA, Anderson SS, Ubl DS, et al. Wide variation and overprescription of opioids after elective surgery. Ann Surg. 2017;266:564–73.
Hill MV, McMahon ML, Stucke RS, Barth RJ Jr. Wide variation and excessive dosage of opioid prescriptions for common general surgical procedures. Ann Surg. 2017;265:709–14.
Eid AI, DePesa C, Nordestgaard AT, et al. Variation of opioid-prescribing patterns among patients undergoing similar surgery on the same acute care surgery service of the same institution: time for standardization? Surgery. 2018;164:926–30.
Overton HN, Hanna MN, Bruhn WE, Hutfless S, Bicket MC, Makary MA. Opioid-prescribing guidelines for common surgical procedures: an expert panel consensus. J Am Coll Surg. 2018;227:411–8.
Thiels CA, Ubl DS, Yost KJ, et al. Results of a prospective, multicenter initiative aimed at developing opioid-prescribing guidelines after surgery. Ann Surg. 2018;268:457–68.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Informat. 2009;42:377–81.
Newhook TE, Vreeland TJ, Dewhurst WL, et al. Clinical factors associated with practice variation in discharge opioid prescriptions after pancreatectomy. Ann Surg. 2018. https://doi.org/10.1097/SLA.0000000000003112.
Lev R, Lee O, Petro S, et al. Who is prescribing controlled medications to patients who die of prescription drug abuse? Am J Emerg Med. 2016;34:30–5.
Funding
Dr. Heather Lillemoe is supported by National Institutes of Health Grant T32CA009599 and the MD Anderson Cancer Center support Grant P30 CA016672.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lillemoe, H.A., Newhook, T.E., Vreeland, T.J. et al. Educating Surgical Oncology Providers on Perioperative Opioid Use: Results of a Departmental Survey on Perceptions of Opioid Needs and Prescribing Habits. Ann Surg Oncol 26, 2011–2018 (2019). https://doi.org/10.1245/s10434-019-07321-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-019-07321-y