Abstract
Introduction
Managing postoperative pain requires an individualized approach in order to balance adequate pain control with risk of persistent opioid use and narcotic abuse associated with inappropriately outsized narcotic prescriptions. Shared decision-making has been proposed to address individual pain management needs. We report here the results of a quality improvement initiative instituting prescribing guidelines using shared decision-making and preoperative pain expectation and management education to decrease excess opioid pills after surgery and improve patient satisfaction.
Methods
Pre-intervention prescribing habits were obtained by retrospective review perioperative pharmacy records for patients undergoing general surgeries in the 24 months prior to initiation of intervention. Patients scheduled to undergo General Surgery procedures were given a survey at their preoperative visit. Preoperative education was performed by the surgical team as a part of the Informed Consent process using a standardized handout and patients were asked to choose the number of narcotic pills they wished to obtain within prescribing recommendations. Postoperative surveys were administered during or after their 2-week postoperative visit.
Results
131 patients completed pre-intervention and post-intervention surveys. The average prescription size decreased from 12.29 oxycodone pills per surgery prior to institution of pathway to 6.80 pills per surgery after institution of pathway (p < 0.001). The percentage of unused pills after surgery decreased from an estimated 70.5% pre-intervention to 48.5% (p < 0.001) post-intervention. 61.1% of patients with excess pills returned or planned to return medication to the pharmacy with 16.8% of patients reporting alternative disposal of excess medication. Patient-reported satisfaction was higher with current surgery compared to prior surgeries (p < 0.001).
Conclusion
Institution of procedure-specific prescribing recommendations and preoperative pain management education using shared decision-making between patient and provider decreases opioid excess burden, resulting in fewer unused narcotic pills entering the community. Furthermore, allowing patients to participate in decision-making with their provider results in increased patient satisfaction.
Graphical abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Managing postoperative pain for outpatient procedures is a difficult art form. In 1995, the American Pain Society introduced “pain as a fifth vital sign.” In the decade that followed, the sale of opioids increased fourfold with a parallel increase in opioid overdose deaths [1]. Opioids have become a mainstay of the postoperative pain regimen.
Deriving an algorithm for narcotic prescription has proved to be an elusive task. Understanding a patient’s postoperative pain management needs requires a thorough evaluation of inherent pain of the procedure as well as the patient’s prior sensitization, expectation and tolerance of pain, and response to medication. This difficult calculus is exacerbated by a push to increase outpatient surgery, requiring surgeons to predict postoperative pain requirements preoperatively. This has historically resulted in vast overprescription of narcotic pain medication. Development of prescribing guidelines and preoperative patient education has been recommended by the American College of Surgery and the Michigan Opioid Prescribing Engagement Network [2, 3]. Vilkins et al. found that using a visual aid for standardized preoperative education and a shared decision-making model resulted in significantly fewer morphine equivalents prescribed upon discharge following hysterectomy at their institution [4].
We hypothesized that this novel model could be extended to common general surgery procedures within our institution and that engaging patients in their pain management with preoperative education and allowing them to choose the number of narcotic pills they would receive postoperatively would decrease the number of opioid pills prescribed and increase patient satisfaction. The goals of this Quality Improvement project were to develop standardized maximum narcotic prescribing guidelines for common general surgery procedures, decrease our overall narcotic prescribing and use, increase patient satisfaction through shared decision-making and improved preoperative counseling, and to set a standard that can be modified and applied to other surgical departments within our institution and hospital system. We report here results of a Quality Improvement project after instituting patient-centered perioperative pain management planning.
Methods
The primary intention of this project was Quality Improvement with the collection of data serving to monitor the process and effectiveness of the intervention. According to institutional guidance at the time of the initiation of this project, under these circumstances, an Institutional Review Board (IRB) determination was not required. Per institutional policy, after initiation of a project no further IRB determination will be granted.
Pre-intervention prescribing habits
Prior to instituting the quality improvement intervention, the scope of the problem was evaluated by determining the pre-intervention prescribing habits of the Department of General Surgery. A list of cases performed by staff General Surgeons from 12/31/2018 to 12/11/2020 was obtained from the hospital’s Surgical Scheduling System (S3; Eisenhower Army Medical Center; 2.3). Surgeries with perioperative pain management pathways such as bariatric surgery and Enhanced Recovery After Surgery (ERAS) were excluded. Additional exclusion criteria were anorectal cases, endoscopic procedures, and multiple procedures performed on separate body parts unless commonly paired (such as breast and axillary surgery or bilateral inguinal hernias). Perioperative pain medication prescriptions were obtained from the Pharmacy Data Transaction Service (PDTS) through the Defense Health Agency (DHA) Pharmacy Analytics Support Section (PASS) using AHFS codes 280804 (non-steroidal anti-inflammatory agents), 280812 (opiate partial agonists), 280892 (analgesics and antipyretics, misc), and 280808 (opiate agonists) for 636 patients. The perioperative period was defined as 7 days prior to surgery to 30 days following surgery. Prescriptions with non-analgesic indications, such as aspirin 81 mg, were excluded. Number of pills and dosages were recorded for all narcotic and non-narcotic perioperative medications as well as any refills or additional pain medications prescribed by outside providers within the perioperative period.
The number of pills prescribed was then evaluated by individual procedure to determine median, mode, and range as well as rate of additional prescriptions or refills required.
Perioperative pain expectations and management
A preoperative survey was offered to general surgery patients scheduled for elective surgery at a preoperative appointment to elicit pain history and expectations. Satisfaction with pain control from prior surgeries was measured using a 5-point Likert scale ranging from very dissatisfied to very satisfied. Exclusion criteria were undergoing surgery for which narcotics were not typically prescribed including lipoma excision and endoscopy, or where the procedure was unknown preoperatively, such as exam under anesthesia. General Surgery residents and staff surgeons counseled patients on postoperative pain expectations and management using a standardized handout during the informed consent process. The standardized handout included information on non-narcotic medications such as acetaminophen and ibuprofen, cold and heat therapy, and mindfulness techniques. Patients were offered the opportunity to choose the number of oxycodone pills they would be prescribed postoperatively within a range based on the type of procedure and expected pain levels. Prescribing recommendations were determined using the University of Michigan Department of Surgery guidelines and best available literature sources. These guidelines were approved by a quorum of Department of General Surgery staff surgeons. The number of pills that each patient elected to receive was annotated in their history and physical and on a Pain Management Plan that was included in their perioperative chart. The Pain Management Plan was given to the patient in the post-anesthesia care unit (PACU) upon discharge. The number of oxycodone pills chosen was prescribed at time of discharge as well as a standard prescription of acetaminophen and ibuprofen as long as there were no medical contraindications. A second survey was then administered at their postoperative appointment or via telephone following their postoperative appointment (median day 16; range postoperative day 5–97) regarding postsurgical pain experience and satisfaction. The number of pills prescribed was confirmed through electronic health record pharmacy records. Postoperative pain management concerns were recorded by patient admission on the postoperative survey and through review of records for clinic appointments, emergency department visits/hospital readmissions, and telephone consult encounters dated within 30 days of the procedure. Areas of concern regarding to patient care were reported to the surgical team to address. As a Quality Improvement initiative, the intervention, the institution of the standardized Pain Management Plan, was recommended for providers to use in all patients, regardless of their intent to answer the surveys.
Statistical analysis
The primary outcome was average prescription size before and after institution of the quality improvement pathway. Secondary outcomes were the percentages of unused pills after surgery reported by patients post-intervention compared to a theoretical model that was based on the department’s historical pre-intervention prescribing habits by surgery, percentage of patients who returned or planned to return excess narcotic pills to the pharmacy, and patient-reported satisfaction. Analysis was done using R programming software and all p values less than 0.05 were considered statistically significant. Wilcoxon signed-rank test with continuity correction testing was used to compare pre- and post-intervention prescription size as well as excess pills prescribed pre- and post-intervention and satisfaction. This was used due to the non-parametric nature of the variables as determined by Shapiro–Wilk test demonstrating significant departure from normality of the data. Pearson’s χ2 test with Yate’s continuity correction was used to compare rate of additional narcotic prescriptions required in pre- and post-intervention populations.
Results
Pre-intervention prescribing habits
Over the period of 12/31/2018 to 12/11/2020, 638 General Surgery cases were evaluated. Prescription records were available for 629 cases. Narcotics were prescribed postoperatively by General Surgery residents and attendings in 88.55% (557/629 patients) and 89.83% (565/629) of patients were written for a narcotic prescription by any provider in the perioperative period (defined as 7 days before surgery to 30 days after surgery).
The most commonly prescribed narcotic was oxycodone, which was prescribed after 84.58% of surgeries (532/629). The number of pills prescribed postoperatively ranged from 3 to 260 pills. After removing two patients with documented sole provider contracts whose pain regimen was prescribed by or in conjunction with the sole provider the number of pills prescribed postoperatively ranged from 3 to 30 pills. When liquid oxycodone was prescribed the range was 60–300 ml (equivalent to 12–60 pills). The median number of pills prescribed was 12 oxycodone pills with 10 pills most commonly prescribed. The median liquid oxycodone prescription was 180 ml (equivalent to 36 pills) with 300 ml (equivalent to 60 pills) most commonly prescribed.
Post-intervention prescribing habits
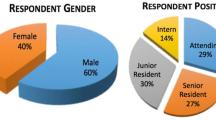
Overall 131 patients responded to both preoperative and postoperative surveys (68 female, 51.5% vs 63 male, 48.5%). Median prescription size decreased from 12 oxycodone pills per surgery prior to institution of pathway to 5 pills per surgery after institution of the pathway (p < 0.001, Table 1, Fig. 1). The percentage of unused pills after surgery decreased from 70.5% pre-intervention to 48.5% post-intervention (p < 0.001). Furthermore, patient-reported satisfaction with pain management was higher with current surgery compared to prior surgeries they had experienced, with median score of 5 (very satisfied) after current surgery compared to median score of 4 (satisfied) with prior surgeries (p < 0.001, Fig. 2). There was no increase in the number of patients who required refill or additional narcotic prescription within the perioperative period (14.67% pre-intervention vs 6.10% post-intervention, p = 0.013). While 6 patients (4.6%) required an unplanned visit to the General Surgery clinic or Emergency Department for postoperative issues, only 3 (2.3%) patients cited surgical pain as the reason for their return. 90.1% and 75.6% of patients reported taking acetaminophen and ibuprofen as a non-narcotic adjunct, respectively (6.1% and 19.8% report not taking or being prescribed. 3.8% did not answer.).
Discussion
Opioids, such as oxycodone, are mainstays of postoperative pain management with 76–92% of patients receiving narcotic prescription following surgery [5]. This is consistent with the pre-intervention prescribing habits at our institution, in which we found that 10% of patients received no narcotics within the perioperative period. Prescription of opioids postoperative and the size of the prescription are known risk factors for development of prolonged opioid use, with reported rates of prolonged use of 0.4–14%. However, the definition of prolonged use is controversial, ranging from continuous use greater than 90 days to single additional prescription within 60 days of one year anniversary of surgery, which makes understanding the true extent of the issue difficult [6,7,8,9,10].
Reasons for opioid overprescribing are likely multifactorial, with proposed reasons including a desire to avoid readmission or repeat presentation for refill, knowledge that patients rate overall care based on the level of postsurgical pain and awareness of publically available physician ratings, restrictions on opioid prescribing leading to larger initial prescriptions due to increased time and effort associated with writing refills, and early inadequate pain control as a risk factor for the development of persistent postsurgical pain [7, 11, 12]. Due to the increased emphasis of pain control since the 1990s and patient satisfaction as a measure of the quality of medical care provided, opioids have become a central component of postoperative pain regimens. However, very little emphasis is placed on medical education to inform providers about prescription size.
A survey of surgical attending physicians and residents at one institution found that 32% of residents report that they received formal education on postoperative prescribing in medical school and only 16% reported training in residency [13]. The most influential factor that residents cited as affecting their prescribing habits were staff surgeons. Yet, only 12% of staff surgeons reported comfort with their own prescribing habits [11].
A tendency towards overprescribing is further exacerbated by a greater push towards same-day surgery to decrease cost and preserve valuable hospital resources. This results in shorter period of time for surgeons to determine a patient’s individual pain response to surgery. As a result, postoperative narcotic prescriptions have historically been oversized, with 67–92% of patients reporting having unused opioids [1, 14, 15], which results in 43–72% of prescribed opioid pills being leftover after surgery [2].
Excess opioids after surgery both contributes to long-term use and creates unused opioids for diversion [1]. Among patients who report excess narcotics, few reported actual or anticipated disposal of extra medications. Historically, 60–70% of patients report saving extra narcotic medication for future use [1, 14, 15]. A self-administered survey in a pediatrician office found that 9.5% of patients kept excess pills for future use of others with 7.1% reporting they would give leftover opioid pills to adolescents to manage pain [15]. In our study, we found that we saved 32.8% of leftover pills from being distributed and decreased the percentage of unused opioids after surgery by 53.7%.
Compared to our department’s historical average, instituting prescribing recommendations and preoperative education decreased our overall opioid prescription significantly with improved patient satisfaction and without increasing the burden on the Emergency or General Surgery departments. This is consistent with Anderson et al. who found that opioid-sparing protocols do not decrease patient satisfaction compared to standard of care [16]. We also hypothesize that this improvement in satisfaction is related to preoperative emphasis on pain expectations and patient autonomy due to institution of shared decision-making. This is in alignment with Vilkins et al., which found that shared decision-making led to decreased narcotic prescription without compromising on patient satisfaction [4]. Barry and Edgman-Levitan wrote in 2012 that shared decision-making is “the pinnacle of patient-centered care” highlighting that “the most important attribute of patient-centered care is the active engagement of patients” [17]. Patient autonomy is well established as one of the 4 key medical ethical principles and patients desire to be allowed to participate in this decision-making. In our experience, when asked who should choose the number of pills prescribed 78% of patients believed it should be a joint decision between their surgeon and themselves compared to 17% who thought the decision should be made by the surgeon and 5% who thought the decision should be made by the patient (Fig. 3). Allowing patients to contribute to their prescription size can further contribute to decreasing excess narcotics, as 55.5% of patients in our study chose fewer than the maximum number of pills allotted.
Despite this significant improvement, 48.5% of prescribed pills remained unused. However, 77.9% of patients reported that they had disposed or had a plan for disposal of excess narcotic pills. This is in stark contrast to the reported literature, where nearly 70% of patients kept or planned to keep excess pills [1, 14, 15].
Limitations of this study include lack of a true control group and potential recall bias, especially for the patients who reached at the extreme of the postoperative survey window. Observer bias may be of particular concern as some patients were reached via phone encounter by a provider rather than given directly to the patients to complete independently as originally intended. In order to institute this quality improvement project to all patients, the pre-intervention cohort was evaluated retrospectively as a theoretical model based on historical prescribing habits rather than individually measured.
Conclusion
Preoperative pain education and prescribing recommendations with shared decision-making significantly decreases opioid prescription without decreasing patient satisfaction, resulting in significantly fewer unused opioid pills available in the community. However, further work can be done to refine prescribing guidelines in order to decrease excess narcotics. Our study demonstrates a novel approach that can be instituted in a wide variety of elective surgical procedures.
References
Feinberg AE, Chesney TR, Srikandarajah S, Acuna SA, McLeod RS (2018) Opioid use after discharge in postoperative patients: a systemic review. Ann Surg 267(6):1056–1062
Michigan-open.org/prescribing-recommendations. Viewed 2/21/2021. Last updated 2/25/2020
Statement on the Opioid Abuse Epidemic. Approved by ACS Board of Regents June 2017. Online August 2, 2017. https://www.facs.org/about-acs/statements/100-opioid-abuse.
Vilkins AL, Sahara M, Till SR et al (2019) The effect of shared decision-making on opioid prescribing after hysterectomy. Obstet Gynecol 134(4):823–833
Fuji MH, Hodges AC, Russell RL, Roensch K, Beynnon B, Ahern TP, Holoch P, Moore JS, Ames SE, MacLean CD (2018) Post-discharge opioid prescribing and use after common surgical procedures. J Am Coll Surg 226(6):1004–1012
Waljee JF, Li L, Brummett CM, Englesbee MJ (2017) Iatrogenic opioid dependence in the United States: are surgeons the gatekeepers? Ann Surg 265:728–730
Clarke H, Soneji N, Ko DT, Yun L, Wijeysundera DM (2014) Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ 348:g1251
Alam A, Gomes T, Zheng H, Mamdani MM, Jurrlink DN, Bell CM (2012) Long-term analgesic use after low-risk surgery: a retrospective cohort study. Arch Intern Med 172(5):425–430
El-Kafraoui C, Olleik G, Chay MA, Kouyoumdjian A, Nguyen-Powanda P, Rajabiyazdi F, Do U, Derksen A, Landry T, Amar-Zifkin A, Ramanakumar AV, Martel MO, Baldini G, Feldman L, Fiore JF (2020) Opioid versus opioid-free analgesia after surgical discharge: protocol for systematic review and meta-analysis. BMJ Open 10(1):e035443
Soneji N, Clarke HA, Ko DT, Wijeysundera DM (2016) Risks of developing persistent opioid use after major surgery. JAMA Surg 151(11):1083–1084
Goel A, Feinberg A, McGuiness B, Brar S, Srikandarajah S, Pearsall E, McLeod R, Clarke H (2020) Postoperative opioid-prescribing patterns among surgeons and residents at university-affiliated hospitals: a survey study. Can J Surg 68(1):E1-8
Hsia H, Takemoto S, Raghunathan K (2018) Acute pain is associated with chronic opioid use after total knee arthroplasty. Reg Anesth Pain Med 43(7):705–711
Hunyh V, Colborn K, Christian N, Rojas K, Nehler M, Bronsert M, Cumbler E, Ahrendt G, Tevis S (2020) Resident opioid prescribing habits do not reflect best practices in the post-operative pain management: an assessment of the knowledge and education gap. J Surg Educ S1931–7204(20):30484
Bicket MC, Long JJ, Pronovost PJ, Alexander GC, Wu CL (2017) Prescribing opioid analgesics commonly unused after surgery: a systemic review. JAMA Surg 157(11):1066–1071
Garbutt JM, Kulka K, Dodd S, Sterkel R, Plax R (2019) Opioids in adolescent’s homes: prevalence, caregiver attitudes, and risk reduction opportunities. Acad Pediatr 19(1):103–108
Anderson M, Hallway A, Brummett C, Waljee J, Englesbe M, Howard R (2021) Patient-reported outcomes after opioid-sparing surgery compared with standard of care. JAMA Surg 156(3):286–287
Barry MJ, Edgman-Levitan S (2012) Shared decision-making—the pinnacle of patient-centered care. NEJM 366:780–781
Acknowledgements
We would like to thank Dr. Amer Mujkanovic, Dr. Reginald Swift, and Stacy Arrazcaeta of Rubix Life Sciences for their statistical analysis. We would also like to thank the employees of the Dwight D Eisenhower Army Medical Center, including Hospital Command, Same Day Surgery/Preoperative Clinic, Post-Anesthesia Care Unit, and General Surgery clinic. We would especially like to thank the General Surgery attending surgeons and residents for their significant effort to institute this intervention.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The authors Dr. Ciampa, Dr. Sherman, Dr. Liang, Dr. O’Hara, and Dr. Joel have no conflicts of interest or financial ties to disclose and no affiliations with or involvement in any organization with financial interest in the subject matter or materials discussed in this presentation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The views expressed in this publication are those of the authors and do not necessarily reflect the official policy or position of the Department of the Army, the Department of Defense, nor the U.S. Government.
Rights and permissions
About this article
Cite this article
Ciampa, M.L., Liang, J., O’Hara, T.A. et al. Shared decision-making for postoperative opioid prescribing and preoperative pain management education decreases excess opioid burden. Surg Endosc 37, 2253–2259 (2023). https://doi.org/10.1007/s00464-022-09464-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09464-8