Abstract
Background
Moderately and poorly differentiated adenocarcinoma of the appendix represents an aggressive histological variant with a high risk of recurrence and death.
Methods
Overall, 178 patients with moderately and poorly differentiated appendiceal adenocarcinoma were identified from a prospective database. Clinical, pathologic, and treatment factors were analyzed for outcomes.
Results
Diagnostic laparoscopy (DL) identified radiographic occult peritoneal metastasis in 25 (42%) patients. These patients had a significantly lower peritoneal carcinomatosis index (PCI) and improved overall survival (OS) compared with those with radiographic disease. Twenty-seven (41%) patients were excluded from cytoreductive surgery (CRS) because of findings on DL, while 116 (65%) patients underwent CRS and hyperthermic intraperitoneal chemotherapy (HIPEC), with a median disease-free survival (DFS) of 23 months. Mucinous histology (hazard ratio [HR] 0.52, p = 0.04) and PCI (HR 1.054, p = 0.02) were independent predictors of DFS. The median OS following CRS and HIPEC was 48 months. Mucinous histology (HR 0.352, p = 0.018), signet ring cells (HR 3.34, p = 0.02), positive peritoneal cytology (HR 0.081, p = 0.04), and PCI (HR 1.076, p = 0.004) were independently associated with OS. Eight-five (73.3%) patients received neoadjuvant chemotherapy, and 40 (47.1%) patients achieved a radiographic response; 36 (42.3%) had stable disease, while 9 (10.6%) had progressive disease. Stable or responsive disease was associated with improved median OS of 44 months, compared with 21 months for those with progressive disease (p = 0.011).
Conclusions
In selected patients, long-term survival can be obtained. Mucinous histology, absence of signet ring cells, negative peritoneal cytology, PCI ≤ 20, and response/stable disease after neoadjuvant chemotherapy are important selection criteria for CRS and HIPEC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The primary treatment for patients with peritoneal dissemination from appendiceal adenocarcinoma is cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC). In multiple studies, this aggressive approach has been demonstrated to result in improved disease control and long-term survival compared with systemic chemotherapy alone;1,2,3,4,5 however, satisfactory outcomes are not universal and are highly dependent on the biological aggressiveness of the tumor.6 As such, histological grade and the presence of signet ring cells are commonly demonstrated to be adverse prognostic factors.6,7,8 The higher grade is associated with a higher proliferative capacity, as well as desmoplastic and destructive tissue invasion, leading to difficulty in obtaining complete cytoreduction and shorter disease-free intervals.9,10
An aggressive multimodality approach is necessary to best manage this aggressive histological variant. While not particularly effective for the well-differentiated appendiceal adenocarcinoma, systemic chemotherapy has been previously demonstrated to result in a significant but modest improvement in progression-free survival (PFS) and overall survival (OS) for patients with moderately and poorly differentiated appendiceal adenocarcinoma.9,11,12 When this systemic chemotherapy is then followed with CRS and HIPEC, we have previously demonstrated a median PFS of 1.2 years and OS of 4.2 years in patients who are able to obtain a complete cytoreduction.9 Others have found similarly improved PFS (median 19–20 months) and OS (median 52–57 months) for complete cytoreduction of high-grade disease.10
Previous reports have been limited by small case sizes and frequently grouping moderately and poorly differentiated appendiceal adenocarcinomas with other high-grade gastrointestinal primary sites.13 As such, there is no consensus on the role of perioperative systemic chemotherapy or CRS and HIPEC for the management of moderately and poorly differentiated appendiceal adenocarcinoma. We therefore sought to review our experience and critically evaluate our current treatment algorithm in order to optimize outcomes and clarify patient selection criteria.
Methods
Patient Selection
Between January 2004 and December 2014, consecutive patients with moderately and poorly differentiated appendiceal adenocarcinoma were identified from a prospectively maintained database. Written informed consent was obtained from all patients, and permission for data analysis and publication was granted by the Institutional Review Board. All pathology was reviewed by our gastrointestinal subspecialty pathologists and histological grade was classified as moderately differentiated or poorly differentiated based on tumor cellularity, architectural features, and cytologic abnormalities. Poorly differentiated tumors were defined as cellular tumors with clusters of tumor cells within mucin pools. The neoplastic epithelium was characterized by cytologic atypia (enlarged nuclei, open chromatin, apoptotic bodies, loss of polarity) and/or architectural complexity, and/or loss of cohesion (clusters of neoplastic cells and/or abundant single cells). In contrast, moderately differentiated tumors were less cellular, with little complexity and cytologic atypia. If signet ring cells were not a significant component of the tumor (i.e. < 10% of the neoplastic cells), these were not incorporated into the grade but were annotated.
Our institutional algorithm for the management of patients with moderately and poorly differentiated appendiceal adenocarcinoma is outlined in Fig. 1a. Neoadjuvant chemotherapy most commonly consisted of four to six cycles of FOLFOX ± bevacizumab, although other agents and durations have been utilized. Radiographic response was defined as a decrease in diameter of measurable disease on post-treatment computed tomography (CT) scan following therapy, compared with pretherapy CT scan as assessed by the reading radiologist. Progressive disease was defined as the appearance of new lesions or an increase in the size of any peritoneal lesions (no minimum amount of increase), while stable disease was defined as no substantial change in peritoneal disease or a mixed response, with some lesions responding and some lesions demonstrating progression; stable disease was combined with responsive disease for analysis. Our technique for CRS and HIPEC has been previously described.14 A peritoneal carcinomatosis index (PCI) was calculated at the time of surgery for all patients,15 and the completeness of cytoreduction (CC) score was used to assess the extent of residual macroscopic disease at the end of surgical resection.15
a Institutional Algorithm for the complex evaluation and management of patients with moderately and poorly differentiated appendiceal adenocarcinoma. b Flowchart illustrating the breakdown of patients (number and percentage) within each clinical context of the evaluation and management algorithm of figure (a)
Data Analysis
Descriptive statistics were reported as number and frequency, or median and interquartile range unless specified. Associations between categorical variables were compared using the Chi square and Fisher’s exact tests, while continuous variables were compared using a Wilcoxon rank-sum test. OS was estimated using the Kaplan–Meier method and compared with the log-rank test, and was calculated from the date of first treatment to the date of death or last follow-up. Disease-free survival (DFS) was calculated from the date of CRS and HIPEC to the time of first recurrence identified on imaging. Only patients with a CC score of 0–1 (CC0 or CC1) were included in the DFS analysis. Multivariate analysis was performed with Cox regression analysis in which a backward elimination process was used for variable selection, with an entry and removal limit of p < 0.1 and p < 0.05, respectively. All analyses were performed using SPSS 22 (released 2013; SPSS Statistics for Windows, version 22.0; IBM Corporation, Armonk, NY, USA), and all graphs were made using GraphPad Prism version 6.00 for Windows (GraphPad Software, La Jolla, CA, USA; www.graphpad.com). All p-values were two-sided and a p value ≤ 0.05 was considered statistically significant.
Results
During the study period, we evaluated 178 patients with moderately or poorly differentiated appendiceal adenocarcinoma. The pathology and operative parameters were stratified according to disease presentation/treatment strategy (Table 1). Sixty patients were referred to our institution after an initial diagnostic appendectomy or right hemicolectomy at an outside facility, and no suspicion of peritoneal disease on the operative report and imaging (Fig. 1b). All of these patients underwent a diagnostic laparoscopy (DL) within 1 year of diagnosis, with 35 (58%) patients having a negative DL. Two (5.7%) of these patients developed peritoneal recurrence during a median follow-up of 47 months (36.0–72.0); one recurrence occurred 25 months after, and the other 44 months after, a negative DL. The patient with relapse at 25 months had a negative peritoneal biopsy on DL and was followed expectantly until carcinoembryonic antigen (CEA) level had risen and a solitary pelvic nodule on surveillance imaging warranted a complete CRS and HIPEC, with a PCI of 15. The patient remains without evidence of disease after an additional 57 months of follow-up. The patient with recurrence at 44 months initially had extension of the appendiceal primary into the bladder wall at the time of right hemicolectomy, but no obvious peritoneal disease. She was lost to follow-up and presented back 44 months later with advanced disease not amenable to CRS and HIPEC. Unfortunately, the patient is deceased 55 months from DL. The remaining 33 (94.3%) patients remain alive without evidence of disease at a median follow-up of 47 months (35.5–69.5) from a negative DL.
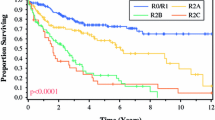
Overall, 116 patients were recommended to undergo CRS and HIPEC: 25 with radiographic occult disease identified on DL, and 91 with radiographic evidence of disease (Fig. 1b). The median DFS for the 83 patients who underwent a CC0 or CC1 CRS was 23 months, and 1-, 3-, and 5-year DFS estimates were 86.4, 29.0, and 16.8%, respectively. On multivariate analysis, mucinous histology (hazard ratio [HR] 0.52, 95% CI 0.277–0.975, p = 0.04) and PCI (HR 1.054, 95% CI 1.009–1.102, p = 0.02) were the only independent predictors of DFS. The median OS for all 116 patients undergoing CRS and HIPEC was 48 months, and the 1-, 3-, and 5-year OS estimates were 95.7, 65.1, and 40.7%, respectively. On multivariate analysis, mucinous histology (HR 0.352, 95% CI 0.148–0.836, p = 0.018), signet ring cells (HR 3.34, 95% CI 1.21–9.211, p = 0.02), positive peritoneal cytology (HR 0.081, 95% CI 0.007–0.890, p = 0.04), and PCI (HR 1.076, 95% CI 1.023–1.31, p = 0.004) were independently associated with OS (Table 2). A PCI ≤ 20 was associated with an improved median OS of 65 months, compared with 28 months for PCI > 20 (p < 0.001) (Fig. 2).
Kaplan Meier graph illustrating the statistically significant difference in overall survival (OS) for patients with moderately- and poorly-differentiated appendiceal adenocarcinoma undergoing cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) as stratified by the Peritoneal carcinomatosis index (PCI) with the cut-off of ≤ 20 and > 20 (p < 0.001)
The 25 (42%) patients without radiographic evidence of peritoneal disease were found to have peritoneal disease at the time of DL [median PCI 8 (4–11)]. A complete cytoreduction was obtained in all of these patients, with a CC0 in 23 (92%) patients and a CC1 in 2 (8%) patients. The 3- and 5-year OS from the time of surgery for this cohort was 83% and 56%, respectively. Median survival has not yet been reached.
Ninety-one patients had radiographic disease at the time of CRS and HIPEC. The median PCI was 14.5 (9–20.75) in these patients, significantly greater than those with radiographic occult disease on DL (p < 0.001). The 3- and 5-year OS from the time of surgery for this cohort was 60.7 and 37.3%, respectively, significantly shorter than those who underwent DL with radiographic occult disease (p = 0.04). Median survival was 44 months.
Of the 64 patients who had a pre-CRS DL, 20 had peritoneal cytology performed; nine (45%) were positive and 11 (55%) were negative. The median OS for cytology-positive cases was 39 months, compared with 55 months for those in whom cytology was not performed and 45 months for those with negative cytology. All patients with positive cytology were deceased by 49 months.
Eighty-five (73.3%) of the 116 patients undergoing CRS and HIPEC had neoadjuvant chemotherapy. No significant difference in OS was observed between those treated with neoadjuvant chemotherapy and those with a surgery-first approach. However, patients treated with neoadjuvant chemotherapy were significantly more likely to have poorly differentiated tumors (p < 0.001), nonmucinous tumors (p = 0.001), presence of signet ring cells (p = 0.019), presence of lymphovascular invasion (p = 0.001), and lymph node involvement (p = 0.008). Forty (47.1%) patients had a radiographic response, 36 (42.3%) had stable disease, and only 9 (10.6%) had progressive disease. Patients with radiographic evidence of stable or responsive disease had a significantly improved median OS of 44 months, compared with 21 months for those with progressive disease on restaging imaging after neoadjuvant chemotherapy (p = 0.011) (Fig. 3). In multivariate analysis of the 85 patients undergoing neoadjuvant chemotherapy, mucinous histology (HR 0.257, 95% CI 0.111–0.587, p = 0.002), presence of signet ring cells (HR 4.079, 95% CI 1.674–9.94, p = 0.002), peritoneal cytology (HR 0.17, 95% CI 0.0047–0.626, p = 0.008), PCI (HR 1.124, 95% CI 1.067–1.184, p < 0.001), and radiographic response/stable disease (HR 17.967, 95% CI 1.745–184.99, p = 0.01) were independent predictors of OS.
Kaplan Meier graph illustrating the statistically significant difference in overall survival (OS) for patients with moderately- and poorly-differentiated appendiceal adenocarcinoma undergoing cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC) as stratified by the radiographic response to neoadjuvant chemotherapy (p = 0.01)
Twenty-seven (40.9%) patients were evaluated with DL and were not found to be candidates for CRS and HIPEC. The most common reason was extensive small bowel serosal or mesenteric involvement that precluded resection in 12 (44.4%) patients, followed by extensive disease/high PCI in 5 (18.5%) patients, and rapid disease progression from the time of last imaging to DL in 4 (14.8%) patients. Other reasons included extensive pelvic (n = 2, 7.4%) or epigastric/portal (n = 2, 7.4%) disease and the infiltrative nature of the disease (n = 2, 7.4%). In this cohort, the 1- and 3-year OS was 69.9 and 32.6%, respectively, with a median survival of 24 months after DL, which was significantly less than those undergoing CRS and HIPEC (p < 0.001).
Discussion
The management of patients with moderately and poorly differentiated appendiceal adenocarcinoma is challenging. Evidence-based treatment algorithms are necessary but are currently unavailable. We have therefore reviewed our institutional experience with this aggressive biologic variant. Similar to previous studies, we found DL to be a safe and feasible method of identifying patients with high-grade appendiceal adenocarcinoma who will benefit from CRS/HIPEC, and to avoid an unnecessary laparotomy in those who will not.16,17,18 Our rate of DL findings prohibiting CRS and HIPEC is only marginally higher than the 20–40% reported in the literature.16,17 This likely reflects the fact that previous studies have grouped all histologies together when considering unnecessary laparotomies, and are likely biased by the large number of low-grade appendiceal tumors that are more likely to result in complete CRS. Unlike low-grade appendiceal adenocarcinoma, where a simplified preoperative assessment score can be calculated based on preoperative imaging, and predict the ability to obtain a complete cytoreduction with near 100% sensitivity, high-grade appendiceal adenocarcinoma requires direct visualization of the peritoneal surfaces in order to determine the likelihood of complete cytoreduction.19 Even high-quality imaging underestimates the extent and distribution of high-grade peritoneal disease, which we and others have demonstrated is an important determinant of outcome.20 Given the poor outcomes for patients with extensive disease (PCI > 20), aggressive organ resection in these patients leads to considerable morbidity with limited benefit.21,22,23 High-grade appendiceal adenocarcinoma is more invasive, and involvement of the small bowel, pelvis, epigastrium, and porta make complete resection difficult. Incomplete resections are of little benefit in patients with high-grade appendiceal adenocarcinoma and should be avoided.1,22 In those patients deemed amenable to complete CRS and HIPEC on DL, we report a high, but not universal, rate of complete cytoreduction. In our experience, this was due to limitation of inspection of the entire abdomen by adhesions. Moreover, we found DL to be helpful in identifying radiographically occult disease in patients who have previously undergone resection elsewhere and have no suspicion of residual disease on review of the outside operative report and imaging. In this group of patients, we found peritoneal disease in just under half of the patients. Identifying low-volume peritoneal disease is critical as these were the patients most likely to obtain a CC0 resection and most likely to have long-term survival. In this group of patients with low-volume disease, we reported 5-year OS exceeding 50%. Likewise, a negative DL was associated with excellent, but not universal, long-term survival, underscoring the continued need for surveillance in this population.
Although we have previously demonstrated disease control in over half of the patients with unresectable appendiceal adenocarcinoma,24 and a significant improvement in OS11,12 with systemic chemotherapy, the perioperative use of systemic chemotherapy remains controversial. Older studies have failed to demonstrate any benefit of perioperative systemic chemotherapy,25,26 while other studies suggest systemic chemotherapy prior to CRS and HIPEC may be associated with worse outcomes, possibly due to tumor progressing through ineffective systemic therapy, closing the window for potentially curative cytoreduction and debilitating patients so they are no longer candidates for cytoreduction.1,27,28 Similar to others, we did not find an improvement in outcomes for all patients treated with neoadjuvant chemotherapy; however, patients who received systemic chemotherapy also had disproportion of the poor prognostic variables, reflecting selection bias that is difficult to account for in a retrospective analysis. Only a prospective, randomized trial will be able to definitively answer this question. A prospective phase II trial evaluating the use of postoperative 5-fluorouracil-based chemotherapy with bevacizumab is currently accruing patients and we look forward to the reporting of this trial (NCT02420509). In the absence of clinical trial results, our data demonstrate a significant radiographic response to neoadjuvant systemic chemotherapy, with stable or responsive disease in nearly 90% of patients. Furthermore, the radiographic response or stable disease was associated with improved outcomes compared with those who progressed on therapy, suggesting that response to neoadjuvant chemotherapy can be an important selection criterion for CRS and HIPEC in high-grade tumors.
Other important prognostic criteria are the presence of mucinous histology, the presence of signet ring cells, positive peritoneal cytology, and the PCI, with previous reports of exclusively high-grade appendiceal adenocarcinoma reporting the significance of lymph node status, PCI, and CC.9,10,13,21,27,29 The use of peritoneal cytology is a unique and important finding. As more and more patients with high-grade histology should be undergoing DL to evaluate suitability for CRS and HIPEC, the addition of peritoneal cytology may offer further prognostic information. The presence of these cells in the setting of peritoneal carcinomatosis from colon cancer has been demonstrated, in a recent French study, to be prognostic. The authors reviewed 162 patients with peritoneal disease from colon cancer who had a complete cytoreduction, and found positive cytology in 23.5% of patients was associated with a poor median OS of 19 months, compared with 44 months with negative cytology. This effect was independent of other prognostic variables.30 Similarly, Yonemura et al. found peritoneal cytology to be an independent predictor of reduced PFS in 205 patients with peritoneal metastasis from colorectal cancer treated with CRS and perioperative chemotherapy.31 As we found no long-term survivors in the patients with positive cytology, this may serve as an important selection criterion but warrants further clinical investigation.
Conclusions
Our data support the role of DL in the evaluation of these patients, both to exclude residual disease and to evaluate the likelihood of complete cytoreduction. In regard to patient selection, we demonstrated that a PCI < 20, and response or stable disease after neoadjuvant systemic chemotherapy, are important predictors of outcome and should be incorporated in treatment algorithms. Lastly, patients with nonmucinous and signet ring cell histology have high aggressive biology and should be carefully selected for CRS and HIPEC.
References
Chua TC, et al. Early- and long-term outcome data of patients with pseudomyxoma peritonei from appendiceal origin treated by a strategy of cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. J Clin Oncol. 2012;30(20):2449–56.
Votanopoulos KI, et al. Peritoneal surface disease (PSD) from appendiceal cancer treated with cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC): overview of 481 cases. Ann Surg Oncol. 2015;22(4):1274–9.
Stewart JH, et al. Appendiceal neoplasms with peritoneal dissemination: outcomes after cytoreductive surgery and intraperitoneal hyperthermic chemotherapy. Ann Surg Oncol. 2006;13(5):624–34.
Sugarbaker PH, Chang D. Results of treatment of 385 patients with peritoneal surface spread of appendiceal malignancy. Ann Surg Oncol. 1999;6(8):727–31.
Austin F, et al. Aggressive management of peritoneal carcinomatosis from mucinous appendiceal neoplasms. Ann Surg Oncol. 2012;19(5):1386–93.
Davison JM, et al. Clinicopathologic and molecular analysis of disseminated appendiceal mucinous neoplasms: identification of factors predicting survival and proposed criteria for a three-tiered assessment of tumor grade. Mod Pathol. 2014;27(11):1521–39.
Shetty S, et al. Proposed classification of pseudomyxoma peritonei: influence of signet ring cells on survival. Am Surg. 2013;79(11):1171–6.
Overman MJ, et al. Improving the AJCC/TNM staging for adenocarcinomas of the appendix: the prognostic impact of histological grade. Ann Surg. 2013;257(6):1072–8.
Lieu CH, et al. Systemic chemotherapy and surgical cytoreduction for poorly differentiated and signet ring cell adenocarcinomas of the appendix. Ann Oncol. 2012; 23(3):652–8.
Polanco PM, et al. Outcomes of cytoreductive surgery and hyperthermic intraperitoneal chemoperfusion in patients with high-grade, high-volume disseminated mucinous appendiceal neoplasms. Ann Surg Oncol. 2016;23(2):382–90.
Asare EA, et al. The impact of stage, grade, and mucinous histology on the efficacy of systemic chemotherapy in adenocarcinomas of the appendix: analysis of the National Cancer Data Base. Cancer. 2016;122(2):213–21.
Choe JH, et al. Improved survival with anti-VEGF therapy in the treatment of unresectable appendiceal epithelial neoplasms. Ann Surg Oncol. 2015;22(8):2578–84.
Van Sweringen HL, et al. Predictors of survival in patients with high-grade peritoneal metastases undergoing cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Surgery. 2012;152(4):617–24 (discussion 624–5).
Grotz TE, et al. Intrathoracic chemoperfusion decreases recurrences in patients with full-thickness diaphragm involvement with mucinous appendiceal adenocarcinoma. Ann Surg Oncol. 2016;23(9):2914–9.
Jacquet P, Sugarbaker PH. Clinical research methodologies in diagnosis and staging of patients with peritoneal carcinomatosis. Cancer Treat Res. 1996;82:359–74.
Jayakrishnan TT, et al. Role of laparoscopy in patients with peritoneal metastases considered for cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (HIPEC). World J Surg Oncol. 2014;12:270.
Tabrizian P, et al. Incorporation of diagnostic laparoscopy in the management algorithm for patients with peritoneal metastases: a multi-institutional analysis. J Surg Oncol. 2015; 111(8):1035–40.
Iversen LH, Rasmussen PC, Laurberg S. Value of laparoscopy before cytoreductive surgery and hyperthermic intraperitoneal chemotherapy for peritoneal carcinomatosis. Br J Surg. 2013;100(2):285–92.
Dineen SP, et al. A simplified preoperative assessment predicts complete cytoreduction and outcomes in patients with low-grade mucinous adenocarcinoma of the appendix. Ann Surg Oncol. 2015;22(11):3640–6.
Flicek K, et al. Correlation of radiologic with surgical Peritoneal Cancer Index scores in patients with pseudomyxoma peritonei and peritoneal carcinomatosis: how well can we predict resectability? J Gastrointest Surg. 2016;20(2):307–12.
El Halabi H, et al. The role of cytoreductive surgery and heated intraperitoneal chemotherapy (CRS/HIPEC) in patients with high-grade appendiceal carcinoma and extensive peritoneal carcinomatosis. Ann Surg Oncol. 2012;19(1):110–4.
Omohwo C, et al. Complete cytoreduction offers longterm survival in patients with peritoneal carcinomatosis from appendiceal tumors of unfavorable histology. J Am Coll Surg. 2009;209(3):308–12.
Sugarbaker PH. Epithelial appendiceal neoplasms. Cancer J. 2009;15(3):225–35.
Shapiro JF, et al. Modern systemic chemotherapy in surgically unresectable neoplasms of appendiceal origin: a single-institution experience. Cancer. 2010;116(2):316–22.
Gough DB, et al. Pseudomyxoma peritonei. Long-term patient survival with an aggressive regional approach. Ann Surg. 1994;219(2):112–9.
Smith JW, et al. Pseudomyxoma peritonei of appendiceal origin. The Memorial Sloan-Kettering Cancer Center experience. Cancer. 1992;70(2):396–401.
Baumgartner JM, et al. Predictors of progression in high-grade appendiceal or colorectal peritoneal carcinomatosis after cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Ann Surg Oncol. 2015;22(5):1716–21.
Baratti D, et al. Pseudomyxoma peritonei: clinical pathological and biological prognostic factors in patients treated with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (HIPEC). Ann Surg Oncol. 2008;15(2):526–34.
Halabi HE, et al. Prognostic significance of lymph node metastases in patients with high-grade appendiceal cancer. Ann Surg Oncol. 2012;19(1):122–5.
Trilling B, et al. Intraperitoneal-free cancer cells represent a major prognostic factor in colorectal peritoneal carcinomatosis. Dis Colon Rectum. 2016;59(7):615–22.
Yonemura Y, et al. Treatment failure following complete cytoreductive surgery for peritoneal metastasis from colorectal cancer. Gan To Kagaku Ryoho. 2016;43(12):1435–9.
Acknowledgment
The authors would like to acknowledge Harold Allen, Sun and Do Lee, and Andrew Shroeder for their contribution to gastrointestinal cancer research at MD Anderson Cancer Center.
Disclosures
Travis E. Grotz, Michael J. Overman, Cathy Eng, Kanwal P. Raghav, Richard E. Royal, Paul F. Mansfield, Gary N. Mann, Kristen A. Robinson, Karen A. Beaty, Safia Rafeeq, Aurelio Matamoros, Melissa W. Taggart, and Keith F. Fournier have no disclosures to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Grotz, T.E., Overman, M.J., Eng, C. et al. Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy for Moderately and Poorly Differentiated Appendiceal Adenocarcinoma: Survival Outcomes and Patient Selection. Ann Surg Oncol 24, 2646–2654 (2017). https://doi.org/10.1245/s10434-017-5938-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-5938-8