Abstract
Background
To investigate the prognostic significance of altered breast cancer susceptibility gene 1 (BRCA1) and p53 expression in triple-negative breast cancer (TNBC).
Methods
Immunohistochemical expression of BRCA1 and p53 was examined in the tumor tissues of 465 TNBC cases and relations were sought with clinicopathological features and patient survival.
Results
Loss of BRCA1 expression was found in 29.5% (137/465) of TNBCs. Positive expression of p53 was observed in 49.9% (232/465). Patients with loss of BRCA1 expression had a tendency to have higher rate of lymph node metastasis (p = 0.075). An association between p53 expression and high histological grade was observed (p = 0.039). TNBC patients with loss of BRCA1 expression had a tendency to have poorer overall survival (OS) than those positive for BRCA1 (p = 0.09). TNBC patients with positive p53 expression showed better OS than those with p53 negativity (p = 0.001). In terms of combined expression patterns, significantly poorer overall survival (OS) was observed for BRCA1-negative/p53-negative TNBCs and best OS for BRCA1-positive/p53-positive TNBCs (p = 0.005).
Conclusions
Combined expression patterns of BRCA1 and p53 could serve as useful prognostic markers in TNBC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2) are important biomarkers for the prediction of prognosis and for determining treatment options, such as hormone therapy for ER- and/or PR-positive tumors or targeted therapy with trastuzumab for HER2-positive tumors. Triple-negative breast cancer (TNBC) does not express ER, PR, and HER2, and its prognosis is generally poorer than that of ER/PR-positive breast cancers, particularly within the first 3–5 years after diagnosis.1–3 However, the outcomes of patients with TNBC are not uniformly poor, and the highly variable clinical behavior of TNBC suggests further subclassification of these tumors could benefit clinical management. We previously reported that it might be possible to classify TNBC into different prognostic groups using the immunohistochemical expression patterns of biomarkers in tumor tissues.4,5
Breast cancer susceptibility gene 1 (BRCA1) and tumor protein P53 (TP53) are tumor suppressor genes that participate the DNA damage signaling pathway. Furthermore, these two genes have been reported to be physically and functionally associated. BRCA1 is located on chromosome 17q21 and is involved in DNA repair, apoptosis, chromosomal remodeling, and cell cycle checkpoint control.6 In addition, BRCA1 plays important roles in growth inhibition and DNA repair by potentiating p53-activated transcriptions of p21 and bax.7,8 A germline mutation of BRCA1 has been shown to be responsible for hereditary breast and ovarian cancer syndrome.9 Although no somatic mutation has been detected, BRCA1 promoter hypermethylation and loss of BRCA1 protein and of heterozygosity in the BRCA1 locus have been reported in sporadic breast cancer.10–16 However, the role played by BRCA1 and the significance of changes in BRCA1 protein expression have not been determined and remain controversial in sporadic breast cancer.
TP53 is located on chromosome 17p13 and encodes p53 transcription factor, which plays a key role in the determination of cell fate after challenge by various stressors, such as radiation, ultraviolet, carcinogen, or cytotoxic drug-induced DNA damage.17 TP53 is the most frequently mutated gene in human cancers, and ~30% of breast cancers display TP53 mutation.18,19 The frequency of this mutation is dependent on breast cancer molecular subtype, for example, lowest mutation frequency is observed in the luminal subtype and highest in the basal subtype.20,21 Although the presence of TP53 mutation was found to be correlated with shorter survival in a large series of breast cancer cases, the prognostic significance of p53 expression as assessed by immunohistochemistry (IHC) is contested.18,22–26
In this study, we examined the immunohistochemical expressions of BRCA1 and p53 proteins in tumor tissues obtained from 492 TNBC cases and evaluated: (1) the relationship between the expressions of BRCA1 and p53, which are functionally closely related proteins, in TNBC, and (2) the prognostic role of these proteins in TNBC.
Materials and Methods
Case Selection and Construction of Tissue Microarray
The study was performed using 465 consecutive TNBC cases, which were obtained from surgical resection at Yeungnam University Hospital, Daegu, South Korea, between January 1995 and December 2009. All tissues were fixed in 10% buffered formalin and embedded in paraffin. To focus on sporadic genetic alterations of BRCA1 and TP53, we excluded patients who had a family history of breast cancer in first-degree relatives or who presented bilateral breast cancer synchronously or metachronously. None of the patients had a family history of breast cancer in first-degree relatives or received neoadjuvant chemotherapy. Tissue microarrays (TMAs) were constructed using two 2-mm cores from a representative tumor block per case as described previously.5
Pathology reports, medical records, and hematoxylin and eosin-stained slides were reviewed to obtain clinicopathological information, including age at time of diagnosis, tumor size, lymph node status, histological grade, lymphovascular invasion (LVI), treatment type, overall survival (OS), and disease-free survival (DFS). The study was approved by the Institutional Review Board of Yeungnam University Hospital (YUH-14-0392-O38), which waived the requirement for informed consent.
Immunohistochemical Evaluation
TMA sections (4 μm) were deparaffinized and immunostained for BRCA1 (MS110, Biocare Medical, Concord, CA) and p53 (DO-7, predilution, Ventana Medical Systems, Tucson, AZ) using the automated BenchMark® platform (Ventana Medical Systems). We regarded the summed tumor area of two consecutive tumor cores as the total tumor area (100%). Regarding the interpretation of BRCA1 and p53 staining, cases exhibiting nuclear staining ≥10% of tumor cells were considered positive.11,24
Statistical Analysis
Statistical analysis was performed using SPSS version 23.0 for Windows (IBM Co., Armonk, NY). The chi-squared test was used to evaluate the significance of correlations between BRCA1 or p53 expression and patient characteristics. Univariate and multivariate analyses were performed to determine the effects of BRCA1 or p53 expression on survival (OS and DFS). Survival curves were plotted using the Kaplan-Meier method and the log-rank test was used to test the significance of survival differences. Significant variables identified by univariate analyses were further analyzed using a Cox regression proportional hazard model. Adjusted hazard ratios and associated 95% confidence intervals (CIs) were estimated for each variable. P values < 0.05 were considered statistically significant.
Results
Patient Demographics
Of the 465 cases, median age at diagnosis was 47 years (range, 25–83 years; mean, 48 years). Invasive tumor sizes ranged from 0.3 to 10.5 (mean, 2.5) cm. Two hundred six (44.3%) patients had an invasive tumor ≤ 2 cm (pT1), and the other 259 patients had an invasive tumor > 2 cm (pT2 in 238; pT3 in 20; pT4 in 1). Axillary lymph node metastasis (LNM) was found in 165 (35.5%) patients and LVI in 186 (40%). Histological grades were 1 in 4 (0.9%), 2 in 32 (6.9%), and 3 in 429 (92.3%). Of the 465 patients, 233 (50.1%) underwent mastectomy and 232 (49.9%) underwent breast-conserving surgery.
For adjuvant chemotherapy, 355 (76.3%) patients received anthracycline-based chemotherapy, and another 90 (19.4%) patients received nonanthracycline chemotherapeutic regimens. The remaining 20 (4.3%) patients did not receive chemotherapy. During a median follow-up of 72 (range 1–202) months, there were recurrences in 70 (15.1%) patients (locoregional recurrence in 27 [5.8%] and distant metastasis in 43 [9.3%] patients). At last follow-up, 76 (16.3%) deaths had occurred.
Immunohistochemical Results
BRCA1 nuclear staining of tumor cells was compared with that of nonneoplastic luminal or ductal cells, because BRCA1 also is expressed in the nuclei of normal epithelial cells and stromal lymphocytes (Fig. 1a). In total, 137 (29.5%) cases were negative for BRCA1 staining in nearly all tumor cells, whereas in the other cases variable proportions of tumor cells showed less intense staining than normal cells (160 cases, 34.4%) or strong immunoreactivity in almost all tumor cells (168 cases, 36.1%; Fig. 1b). On the other hand, p53 expression was observed exclusively in tumor cell nuclei, and 232 (49.9%) cases were positive (Fig. 2).
Representative immunohistochemical results for BRCA1 expression in triple-negative breast cancer. a This case shows loss of BRCA1 expression in tumor cell nuclei. Nonneoplastic luminal epithelial cells and stromal lymphocytes show positive expression for BRCA1 in the nuclei. b In other case, BRCA1 is strongly expressed in most tumor cells
Relationships between the Expressions of BRCA1 and p53 and Clinicopathological Variables
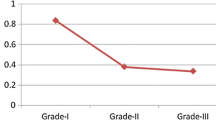
A summary of relationships between BRCA1 or p53 expression and clinicopathological variables is provided in Table 1. Patients with loss of BRCA1 expression had a tendency to have higher rate of LNM (p = 0.075), but no significant correlation was observed between BRCA1 expression and other clinicopathological variables, including tumor size, LVI, and histologic grade. There was a positive association between p53 expression and histological grade (p = 0.039), and p53 expression showed no significant correlation with other clinicopathologic variables. No significant correlation was found between BRCA1 expression and p53 expression (p = 0.495).
Prognostic Significances of the Expressions of BRCA1 and p53
TNBC patients with loss of BRCA1 expression had poorer OS than those positive for BRCA1 (p = 0.09; Fig. 3a). Although BRCA1 expression did not have a significant influence on DFS, BRCA1-negative patients tended to have poorer outcomes than BRCA1-positive patients (p = 0.314). TNBC patients with p53 positivity achieved better outcomes (OS, p = 0.001; DFS, p = 0.125; Fig. 3b). We also evaluated survival differences with respect to the combined expression of BRCA1 and p53. As shown in Fig. 3c, BRCA1+/p53+ patients had better OS than BRCA1–/p53– patients (p = 0.005). Multivariate analysis, including tumor size, lymph node status, and a BRCA1/p53 status, showed that all three variables independently predicted OS in TNBC (Table 2). More specifically, BRCA1–/p53– was found to be associated with lower OS with a threefold higher risk of death (95% CI 1.679–6.411; p = 0.001) than BRCA1+/p53+.
Discussion
Breast cancer is a heterogeneous disease, and the abilities of some biomarkers to predict prognosis might depend on hormone receptor status (ER-positive vs. ER-negative or TNBC), when their expressions are associated with hormone receptor status. Although androgen receptor and Bcl-2 expression are considered good prognostic markers in ER-positive breast cancer in previous studies, we found they were correlated with poor prognosis in some patients with TNBC.4,5 BRCA1 and TP53 are functionally related tumor suppressor genes, and absent or diminished BRCA1 expression and positive p53 expression were found to be associated with an ER–/PR– status.13,17 Considering the strong correlations that exist between the expressions of these proteins and hormone receptor status, we investigated the prognostic impacts of expressions of BRCA1 and/or p53 in TNBC to exclude the effects of hormone receptor expressions on patient survival.
In the present study, loss of BRCA1 expression was observed in 29.5% of TNBCs and was significantly correlated with a non-basal phenotype. In another study performed in an invasive breast cancer series, absent or reduced BRCA1 expression was associated with larger tumor size, advanced lymph node stage, high histological grade, LVI, negative hormone receptor status, p53 positivity, and basal phenotype of breast cancer.13 Yang et al. also reported associations between BRCA1 expression and LNM and histological grade but not with other conventional prognostic markers, such as tumor size, histologic type, hormone receptor status, expression of p53 or c-erbB-2, and MIB-1 labeling index.11 Considering that TNBC usually involves grade 3 and p53-positive tumors, LNM was the only parameter associated with BRCA1 expression regardless of hormone receptor status.3,27 In our study, patients with loss of BRCA1 expression had a higher rate of LNM than those with BRCA1 expression, but the association was not statistically significant. Studies, including the present study, consistently have shown that loss of BRCA1 expression is associated with poor survival in breast cancer. Because BRCA1 facilitates stress-induced apoptosis, loss of BRCA1 protein may result in tumor cell resistance to chemotherapy-induced apoptosis, which would explain why negative BRCA1 expression is associated with poorer prognosis.11,28 Promoter hypermethylation and posttranscriptional modifications resulting in reduced BRCA1 protein stability are considered to underlie the absence of or reduced BRCA1 protein expression in sporadic breast cancer.29
To investigate the value of TP53 status for predicting treatment response and clinical outcomes, different clinical and methodological settings have been used, but results are contradictory.30 IHC has been widely used to assess p53 alterations, but it is a poor surrogate of gene mutation status. Missense mutation of TP53 yields a highly stable mutant p53 protein that can be detected by IHC, whereas p53 proteins resulting from truncating TP53 mutations are unstable and cannot be detected by IHC. In addition wild-type p53 may show strong immunoreactivity, because it commonly accumulates in tumors as a result of DNA damage or of binding to other cellular proteins.17,21,23,31
We evaluated p53 expression in TNBC by IHC and observed it was expressed in 49.9% of cases. Reported positivity rates of p53 expression range from 56 to 71% in TNBC, and its correlations with clinicopathological features vary in studies. In the present study, histological grade was the only parameter associated with p53 expression, whereas significant correlations have been reported with LNM and histological grade.26,32 Furthermore, we observed p53 positivity was associated with better prognosis in TNBC, whereas previous studies have reported TP53 mutation has negative prognostic significance.18,22 Studies on the prognostic significance of p53 expression as assessed by IHC arrived at contrary conclusions.23–26,31,33 Two recent studies reported results very similar to ours regarding the relationship between p53 expression and clinical outcome.24,26 Coates et al. reported that p53 expression was associated with better DFS and OS in patients with ER-negative breast cancer, but with poorer DFS and OS in patients with ER-positive breast cancer.24 These authors suggested that interpretation of the prognostic significance of p53 expression requires knowledge of the concurrent expressional status of ER but added that the reason for the prognostic interaction between p53 and ER is unknown. Jin et al. reported p53 negativity was an independent risk factor for LNM and that p53 positivity predicted better survival in TNBC.26 It also was suggested the immunohistochemical expression of p53 might reflect the accumulation of wild-type p53 rather than mutant p53 protein in TNBC.
Although the immunohistochemical detection of TP53 mutation depends on mutation type (a high positive rate for missense mutations and a high negative rate for truncating mutations), the different prevalence of TP53 mutation types among different breast cancer subgroups must also be considered. Dumay et al. reported a high prevalence of missense mutations in luminal tumors and of truncating mutations in basal tumors.20 In addition, the prognostic significances of TP53 mutation differ between mutation types. Non–missense mutations (mostly truncating mutations) were most strongly associated with poor survival, and these mutations are not likely to be detected by IHC.34 A positive association between p53 expression and good prognosis in TNBC could be explained by p53-induced enhancement of response to chemotherapy. Bertheau et al. suggested that an accumulation of genetic abnormalities leads to mitotic catastrophe and better response to anthracycline-cyclophosphamide-based chemotherapy in patients with ER-negative/TP53-mutated breast cancer, whereas in patients with ER-positive/TP53-wild-type breast cancer, ER-induced inhibition of p53 apoptotic response would lead to tumor cell senescence and subsequent resistant to treatment.21 Therefore, a link between TP53 status and response to chemotherapy affected patient’ survival, because more than 90% of our patients received adjuvant chemotherapy based on anthracyclines and alkylating agents.
We also found that combined BRCA1 and p53 expression status intensifies classification of TNBC cases into different prognostic subgroups. Notably, BRCA1–/p53– cases had the poorest prognosis, which could be explained by resistance to chemotherapy in TNBC patients with inactivated BRCA1/intact p53 functions.
In conclusion, immunohistochemical assessments of the expressions of BRCA1 and p53 proteins might provide information that could be used to stratify TNBCs into subgroups with different aggressiveness and prognoses, regardless of the underlying mechanisms driving protein expression alterations in cancer cells.
References
Dent R, Trudeau M, Pritchard KI, et al. Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res. 2007;13:4429-34.
Tischkowitz M, Brunet JS, Begin LR, et al. Use of immunohistochemical markers can refine prognosis in triple negative breast cancer. BMC Cancer. 2007;7:134.
Kim J, Hwang T, Kang S, Lee S, Bae Y. Prognostic Significance of Basal Markers in Triple-negative Breast Cancers. J Breast Cancer. 2009;12:4-13.
Choi JE, Kang SH, Lee SJ, Bae YK. Prognostic significance of Bcl-2 expression in non-basal triple-negative breast cancer patients treated with anthracycline-based chemotherapy. Tumour Biol. 2014;35:12255-63.
Choi JE, Kang SH, Lee SJ, Bae YK. Androgen receptor expression predicts decreased survival in early stage triple-negative breast cancer. Ann Surg Oncol. 2015;22:82-9.
Somasundaram K. Breast cancer gene 1 (BRCA1): role in cell cycle regulation and DNA repair–perhaps through transcription. J Cell Biochem. 2003;88:1084-91.
Ouchi T, Monteiro AN, August A, Aaronson SA, Hanafusa H. BRCA1 regulates p53-dependent gene expression. Proc Natl Acad Sci U S A. 1998;95:2302-6.
Zhang H, Somasundaram K, Peng Y, et al. BRCA1 physically associates with p53 and stimulates its transcriptional activity. Oncogene. 1998;16:1713-21.
Miki Y, Swensen J, Shattuck-Eidens D, et al. A strong candidate for the breast and ovarian cancer susceptibility gene BRCA1. Science. 1994;266:66-71.
Yoshikawa K, Honda K, Inamoto T, et al. Reduction of BRCA1 protein expression in Japanese sporadic breast carcinomas and its frequent loss in BRCA1-associated cases. Clin Cancer Res. 1999;5:1249-61.
Yang Q, Sakurai T, Mori I, et al. Prognostic significance of BRCA1 expression in Japanese sporadic breast carcinomas. Cancer. 2001;92:54-60.
Kurebayashi J, Yamamoto Y, Kurosumi M, Okubo S, Nomura T, Tanaka K, Sonoo H. Loss of BRCA1 expression may predict shorter time-to-progression in metastatic breast cancer patients treated with taxanes. Anticancer Res. 2006;26:695-701.
Rakha EA, El-Sheikh SE, Kandil MA, El-Sayed ME, Green AR, Ellis IO. Expression of BRCA1 protein in breast cancer and its prognostic significance. Hum Pathol. 2008;39:857-65.
Zhu X, Shan L, Wang F, et al. Hypermethylation of BRCA1 gene: implication for prognostic biomarker and therapeutic target in sporadic primary triple-negative breast cancer. Breast Cancer Res Treat. 2015;150:479-86.
Yamashita N, Tokunaga E, Kitao H, et al. Epigenetic Inactivation of BRCA1 Through Promoter Hypermethylation and Its Clinical Importance in Triple-Negative Breast Cancer. Clin Breast Cancer. 2015;15:498-504.
Okada S, Tokunaga E, Kitao H, et al. Loss of heterozygosity at BRCA1 locus is significantly associated with aggressiveness and poor prognosis in breast cancer. Ann Surg Oncol. 2012;19:1499-507.
Lacroix M, Toillon RA, Leclercq G. P53 and Breast Cancer, an Update. Endocr Relat Cancer. 2006;13:293-325.
Borresen-Dale AL. TP53 and breast cancer. Hum Mutat. 2003;21:292-300.
Petitjean A, Mathe E, Kato S, Ishioka C, Tavtigian SV, Hainaut P, Olivier M. Impact of mutant p53 functional properties on TP53 mutation patterns and tumor phenotype: lessons from recent developments in the IARC TP53 database. Hum Mutat. 2007;28:622-9.
Dumay A, Feugeas JP, Wittmer E, et al. Distinct tumor protein p53 mutants in breast cancer subgroups. Int J Cancer. 2013;132:1227-31.
Bertheau P, Lehmann-Che J, Varna M, et al. P53 in Breast Cancer Subtypes and New Insights into Response to Chemotherapy. Breast. 2013;22 Suppl 2:S27-9.
Pharoah PD, Day NE, Caldas C. Somatic mutations in the p53 gene and prognosis in breast cancer: a meta-analysis. Br J Cancer. 1999;80:1968-73.
Biganzoli E, Coradini D, Ambrogi F, et al. P53 Status Identifies Two Subgroups of Triple-Negative Breast Cancers with Distinct Biological Features. Jpn J Clin Oncol. 2011;41:172-9.
Coates AS, Millar EK, O’Toole SA, et al. Prognostic interaction between expression of p53 and estrogen receptor in patients with node-negative breast cancer: results from IBCSG Trials VIII and IX. Breast Cancer Res. 2012;14:R143.
Maeda T, Nakanishi Y, Hirotani Y, et al. Immunohistochemical co-expression status of cytokeratin 5/6, androgen receptor, and p53 as prognostic factors of adjuvant chemotherapy for triple negative breast cancer. Med Mol Morphol. 2016;49:11-21.
Jin MS, Park IA, Kim JY, et al. New insight on the biological role of p53 protein as a tumor suppressor: re-evaluation of its clinical significance in triple-negative breast cancer. Tumour Biol. 2016. doi:10.1007/s13277-016-4990-5.
Thike AA, Cheok PY, Jara-Lazaro AR, Tan B, Tan P, Tan PH. Triple-negative breast cancer: clinicopathological characteristics and relationship with basal-like breast cancer. Mod Pathol. 2010;23:123-33.
Thangaraju M, Kaufmann SH, Couch FJ. BRCA1 facilitates stress-induced apoptosis in breast and ovarian cancer cell lines. J Biol Chem. 2000;275:33487-96.
Miyamoto K, Fukutomi T, Asada K, et al. Promoter hypermethylation and post-transcriptional mechanisms for reduced BRCA1 immunoreactivity in sporadic human breast cancers. Jpn J Clin Oncol. 2002;32:79-84.
Petitjean A, Achatz MI, Borresen-Dale AL, Hainaut P, Olivier M. TP53 mutations in human cancers: functional selection and impact on cancer prognosis and outcomes. Oncogene. 2007;26:2157-65.
Kim JY, Park K, Jung HH, et al. Association between mutation and expression of TP53 as a potential prognostic marker of triple-negative breast cancer. Cancer Res Treat. 2016. doi:10.4143/crt.2015.430.
Thike AA, Tan PH, Ikeda M, Iqbal J. Increased ID4 expression, accompanied by mutant p53 accumulation and loss of BRCA1/2 proteins in triple-negative breast cancer, adversely affects survival. Histopathology. 2016;68:702-12.
Rakha EA, El-Sayed ME, Green AR, Lee AH, Robertson JF, Ellis IO. Prognostic markers in triple-negative breast cancer. Cancer. 2007;109:25-32.
Olivier M, Langerod A, Carrieri P, et al. The clinical value of somatic TP53 gene mutations in 1,794 patients with breast cancer. Clin Cancer Res. 2006;12:1157-67.
Acknowledgment
This study was supported by Medical Research Center Program (2015R1A5A2009124) through the National Research Foundation of Korea (NRF), Ministry of Science, ICT and Future Planning.
Conflict of Interest
The authors declared no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, M.C., Choi, J.E., Lee, S.J. et al. Coexistent Loss of the Expressions of BRCA1 and p53 Predicts Poor Prognosis in Triple-Negative Breast Cancer. Ann Surg Oncol 23, 3524–3530 (2016). https://doi.org/10.1245/s10434-016-5307-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5307-z