Abstract
Background
Parathyroid carcinoma is a rare cause of hyperparathyroidism. Surgery is the only effective therapy, and en bloc resection has previously been recommended.
Methods
A retrospective cohort study of patients with parathyroid carcinoma in the California Cancer Registry and California Office of Statewide Health Planning and Development database from 1999 to 2012 was performed. Patients were stratified by surgical procedure: parathyroidectomy alone, thyroid resection with en bloc parathyroidectomy, and parathyroidectomy with delayed thyroid resection within 6 months. The primary outcome was overall survival stratified by surgical procedure. Secondary outcomes included perioperative complications within 30 days of initial surgery and disease-related complications.
Results
Among our study cohort (n = 136), 60 patients underwent parathyroidectomy alone, 58 patients had en bloc resection, and 18 patients had parathyroidectomy followed by delayed thyroid resection. For the entire cohort, the 5-year and 10-year overall survival rates were 86.9 and 72.0 %. The overall survival rates did not differ between the surgical procedures. Factors that were independently associated with decreased survival included age (hazard ratio 1.05, P = 0.017) and distant metastases (hazard ratio 4.73, P = 0.017), while en bloc resection and delayed thyroid resection were not associated with improved survival over parathyroidectomy alone. There were no differences in perioperative or disease-related complications across procedures.
Conclusions
The addition of thyroid resection to parathyroidectomy may not improve survival for patients with parathyroid carcinoma over complete parathyroid resection alone. A larger prospective study is necessary to determine the optimal treatment to achieve long-term survival with minimal complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
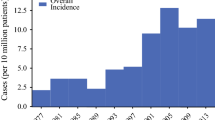
Parathyroid carcinoma is a rare disease, comprising less than 1 % of all cases of hyperparathyroidism.1 Surgical resection is the only effective treatment and can palliate symptoms related to hypercalcemia.2 Ipsilateral thyroid lobectomy with en bloc parathyroid resection has been recommended to decrease disease recurrence and can potentially cure patients with localized parathyroid carcinoma.1–7 Despite that, initial en bloc resection is performed in only 12 % of cases, which may reflect that the diagnosis is often established on final histopathology.8,9 In such cases, the surgeon may be faced with the dilemma whether to reoperate to remove adjacent thyroid tissue. More recent studies have not demonstrated a clear survival benefit with en bloc resection over parathyroidectomy alone, and the optimal extent of surgery for parathyroid carcinoma is currently unclear.9–11
In addition, the impact of surgical treatment on perioperative and disease-related complications is not well characterized, as previous studies have focused predominantly on survival.4,8–10 Perioperative complications include hypoparathyroidism and recurrent laryngeal nerve palsy.5,11,12 Disease-related complications such as renal failure and bone fractures occur due to uncontrollable hypercalcemia.2,13 Data is lacking to show whether more extensive surgery impacts the risk of perioperative complications or long-term rate of disease-related complications.
Using a population-based database with longitudinal follow-up, we aimed to assess the impact of extent of surgery on overall survival as well as perioperative and disease-related complications in patients with parathyroid carcinoma. We hypothesized that the addition of thyroid resection would be associated with improved overall survival and fewer disease-related complications over parathyroidectomy alone.
Methods
Sample
Given the rarity of parathyroid carcinoma, we used the California Cancer Registry linked to California Office of Statewide Health Planning Database to allow for longitudinal tracking of patients with unique record identifiers after surgery. Using the California Cancer Registry (CCR), patients with parathyroid cancer were identified using the ICD-O-2 code C750 for 1999–2000 and ICD-O-3 code C750 for 2001–2012. Patient records were linked by unique identifiers to inpatient and ambulatory hospital records maintained by the California Office of Statewide Health Planning and Development (OSHPD) to allow for longitudinal follow-up.
Patients were stratified by surgical procedure: parathyroidectomy alone, thyroid resection with en bloc parathyroidectomy, and parathyroidectomy with delayed thyroid resection. Parathyroidectomy was coded using ICD-9-CM codes 0681 and 0689 and CPT codes 60500 and 60502. En bloc resection was coded if the patient had a thyroidectomy procedure (Appendix A) in addition to a parathyroidectomy on the same day. A delayed thyroid resection was coded if a patient had a thyroidectomy procedure within a 6-month window after parathyroidectomy. Patients who had no surgery information in OSHPD were excluded from the study.
Perioperative complications were defined as complications occurring within 30 days of surgery. Disease-related complications were defined as one of the following complications occurring beyond 30 days of surgery: pancreatitis (ICD-9-CM codes 577.0 and 577.1), fractures (ICD-9-CM codes 733.10–733.16, 733.19, 733.93–733.98, and 805–829), renal failure requiring dialysis, and tracheostomy. Dialysis and tracheostomy cases were identified by keyword search of code descriptors. Patients who had end-stage renal disease requiring dialysis before surgery were not considered as having a disease-related complication.
Stage at diagnosis was categorized into localized, regional (by direct extension and/or to lymph nodes), and remote disease using the CCR variable for summary stage at time of diagnosis. We also abstracted the date of most recent follow-up, vital status, and cause of death from the CCR-OSHPD files linked to the California Department of Public Health Vital Statistics data files. Hospital volume, used as a surrogate for individual surgeon-specific data as that is unavailable in this registry, was determined by the average number of parathyroidectomies performed at that institution annually during the study period.
Statistical Analysis
Patient demographics, clinical factors, and perioperative and disease-related complications were reported as means ± standard deviations for continuous variables and frequencies and percentages for categorical variables. Logistic regression models were used to predict perioperative and disease-related complications. Multivariable regression analyses included adjustments for age, sex, race, socioeconomic status, hospital volume, and type of surgical procedure.
The 5-year and 10-year overall survival rates were estimated using the Kaplan–Meier method. The log-rank test was used to compare outcomes among the different surgical procedures. We performed subgroup analyses examining the association between type of surgical procedure and overall survival for patients with localized, regional, and remote disease. Patients in the en bloc resection and delayed thyroid resection groups were analyzed individually and together due to the small number of patients in the latter group. The Kaplan–Meier graphs were truncated at five years due to small sample size beyond this timeframe. The survival curves were also examined in a subset of patients with at least 5 years of follow-up. The small number of perioperative complications did not permit individual statistical analysis between surgical groups, so they were combined into a single group for comparison. All analyses were conducted by SAS 9.3 (SAS Institute, Cary, NC).
Results
Between 1999 and 2012, 136 patients underwent surgery for parathyroid carcinoma in California. Median follow-up time was 5.3 years (interquartile range [IQR] 2.5–8.7). The average age at diagnosis was 57.2 years, and the cohort comprised evenly of men (52.2 %) and women (Table 1). The median tumor size was 25 mm (IQR 17–35 mm). The majority of patients had localized disease at the time of diagnosis (59.6 %). Sixty patients (44.1 %) underwent parathyroidectomy alone, 58 patients (42.7 %) had initial en bloc resection, and 18 patients (13.2 %) had a parathyroidectomy with delayed thyroid resection. Patients who underwent parathyroidectomy alone were on average slightly older (59.0 years) compared to patients who underwent en bloc resection (57.5 years) or delayed thyroid resection (50.1 years) (P = 0.037). None of the patients who underwent delayed thyroid resection had distant metastases, while 2 patients who underwent parathyroidectomy only and 5 patients who underwent en bloc resection were classified as having remote disease in CCR (P = 0.037). There were no other differences in baseline patient characteristics between the surgical procedure groups (Table 1). Of the 18 patients who underwent a staged operation, only two patients (11.1 %) underwent the delayed thyroid resection at a different hospital.
The 5- and 10-year overall survival rates were 86.9 % and 72.0 %, respectively. The 5-year overall survival rate was 85.7 % for patients who underwent parathyroidectomy alone, 84.0 % for patients who underwent initial en bloc resection, and 100 % for patients who underwent parathyroidectomy followed by delayed thyroid resection (P = 0.26). The Kaplan–Meier survival curves showed no difference in overall survival between the three surgical groups (P = 0.26, Fig. 1). There was still no significant survival difference when the initial en bloc and delayed thyroid resection patients were combined into a single group and compared against the patients who underwent parathyroidectomy only (P = 0.63). In multivariable analysis, predictors of decreased overall survival included age at diagnosis (hazard ratio 1.05, P = 0.017) and remote disease (hazard ratio 4.73, P = 0.017). In the multivariable model, en bloc resection (P = 0.15) and delayed thyroid resection (P = 0.36) were not significantly associated with survival as compared with parathyroidectomy alone. Hospital volume was also not a significant predictor of survival (P = 0.75).
When stratified by disease stage, there was still no difference in survival between the surgical groups for localized disease (P = 0.48, Fig. 2a), regional disease (P = 0.70, Fig. 2b), and metastatic disease (P = 0.35, data not shown due to small sample size). Based on our sample size, we had 80 % power to detect a between-group difference in survival of 11 % at a 0.05 significance level. In a subgroup analysis of patients with at least 5 years follow-up (n = 73), there was still no significant difference in overall survival based on the type of surgical procedure (P = 0.28).
a Kaplan–Meier analysis of overall survival compared across type of surgical procedure for patients with localized disease (n = 81). Delayed thyroid resection group was combined with initial en bloc resection group because there were no deaths in the former group. b Kaplan–Meier analysis of overall survival compared across type of surgical procedure for patients with regional disease only (n = 48). Delayed thyroid resection group was combined with initial en bloc resection group
Perioperative complications were rare, and included 3 patients (2.2 %) who required a temporary tracheostomy, 3 patients (2.2 %) who had unilateral vocal cord paralysis, 1 patient (0.7 %) who had bilateral vocal cord paralysis, 3 patients (2.2 %) who developed acute kidney failure, and 3 patients (2.2 %) who experienced a urinary tract infection. The rate of any perioperative complication was similar among the surgical procedures (6.7, 12.1, and 0 % in the parathyroidectomy only, initial en bloc resection, and delayed thyroid resection groups, respectively; P = 0.28).
Disease-related complications were also rare (Table 2). The most common complication was fracture, occurring in 8 patients (5.9 %) after surgery. The median time between surgery and fracture was 29.4 months. Six patients (4.4 %) developed renal failure requiring dialysis, with 4 patients progressing to end-stage renal disease requiring chronic dialysis and 2 patients receiving dialysis only once after surgery. The median time between surgery and dialysis was 16.6 months. There were no significant differences in the rate of disease-related complications based on type of surgical procedure (16.7, 6.9, and 22.2 % in the parathyroidectomy only, initial en bloc resection, and delayed thyroid resection groups, respectively; P = 0.12). In the logistic regression analyses, none of the model predictors (including hospital volume and type of surgery) were significant for disease-related complications.
Discussion
This study of 136 parathyroid carcinoma patients found similar overall survival regardless of extent of surgical resection. The CCR linked to OSHPD database gave us the unique opportunity to identify patients who underwent reoperation with subsequent thyroid resection after initial parathyroidectomy, and permitted more detailed longitudinal follow-up than previous studies.8,9 We found no difference in survival, perioperative and disease-related complications between patients who underwent parathyroidectomy alone versus en bloc or delayed thyroid resection.
The 5-year overall survival rate for patients with parathyroid carcinoma has been reported to be 82–90 %, which is consistent with our results.8–10,12,14 Among our study cohort, 42.7 % underwent initial en bloc resection and 13.2 % underwent delayed thyroid resection. This is higher than the previously reported 12–39 % of patients who underwent en bloc resection for parathyroid carcinoma.8,12 The increased rate of initial en bloc resection in our contemporary study may reflect prior studies suggesting decreased recurrence with this approach.1,3–5
The optimal surgical treatment for parathyroid carcinoma is not clear. Although thyroid lobectomy with en bloc resection of the parathyroid gland has previously been recommended, a growing number of studies have not shown a benefit of this approach over parathyroidectomy alone.4,8–12,15,16 In a recent study of 733 patients using the National Cancer Data Base, patients who had any surgical resection (incomplete or complete) had improved overall survival compared to patients who had no surgery.14 Complete resection (defined as complete excision of the entire parathyroid mass) was not associated with a survival benefit over incomplete resection (defined as simple or local tumor excision). We specifically analyzed en bloc resection (defined as thyroid resection at the time of parathyroidectomy) and also found no significant survival benefit over parathyroidectomy alone. To our knowledge this is the first population-based study to identify patients who underwent delayed thyroid resection after parathyroidectomy. Although this was a small number of patients, they had similar overall survival compared to patients in the other surgical procedure groups.
We hypothesized that more extensive surgery may increase the rate of perioperative complications but decrease disease-related complications by decreasing recurrence. We found similarly low rates of perioperative complications across surgical procedures. The rate of perioperative complications has large institution-dependent variability and ranges from 9 to 45 %.5,11,12,17 Factors associated with decreased perioperative complication rates in previous studies include initial operation performed at a dedicated endocrine surgery center.11 Reoperation for recurrent or persistent disease has high complication rates, although delayed thyroid resection within 6 months of initial surgery was not associated with increased perioperative complications in our study.5,11 We also did not detect a difference in disease-related complications between the surgical groups. Although our analysis is likely limited by undercoding of complications in a statewide registry, this may be due to similar rates of disease recurrence, which likely parallel the overall survival rates.
One of the main limitations of this study was the relatively small sample size despite the use of a state-wide database, highlighting the rare incidence of parathyroid carcinoma. Parathyroid carcinoma can be difficult to diagnose and some cases may have been misclassified, as we were unable to personally review the pathology. We only included cases with the appropriate histology codes for carcinoma, and our survival curves are similar to the recent National Cancer Data Base and other studies. Although all survival analyses were adjusted for hospital volume, the latter cannot fully function as a surrogate for reliability of pathologic diagnosis. Another significant limitation is that the initial disease severity likely influenced the type of surgery the patient received. Patients with invasive disease, where the tumor was adherent to the thyroid or other local structures, would be more likely to undergo en bloc resection. We were unable to control for differences in disease severity aside from stage at diagnosis. While CCR includes stage at diagnosis, it lacks biochemical data and gross intraoperative findings. Thus, patient survival in our analysis may have been impacted by extent of operation as well as initial disease severity. A multicenter prospective study is necessary to confirm the optimal surgical treatment for parathyroid carcinoma. Other limitations include inability to track calcium and parathyroid hormone levels and likely underreporting of complications. Finally, similar to other state-wide and national cancer registries, information on disease recurrence was not available and our analysis was limited to overall survival.
Parathyroid carcinoma is a rare endocrine disease that is optimally treated with surgical resection. We found an increased rate of en bloc resection compared to earlier studies, but no difference in overall survival compared to parathyroidectomy alone. The addition of thyroid resection to parathyroidectomy may not improve survival or disease-related complications in parathyroid carcinoma over complete parathyroid resection alone. A larger prospective study with longer follow-up is necessary to determine the optimal treatment to achieve long-term survival with minimal complications.
References
Koea JB, Shaw JH. Parathyroid cancer: biology and management. Surg Oncol. 1999;8:155–65.
Owen RP, Silver CE, Pellitteri PK, et al. Parathyroid carcinoma: a review. Head Neck. 2011;33:429–36.
Obara T, Fujimoto Y. Diagnosis and treatment of patients with parathyroid carcinoma: an update and review. World J Surg. 1991;15:738–44.
Sandelin K, Auer G, Bondeson L, Grimelius L, Farnebo LO. Prognostic factors in parathyroid cancer: a review of 95 cases. World J Surg. 1992;16:724–31.
Kebebew E, Arici C, Duh QY, Clark OH. Localization and reoperation results for persistent and recurrent parathyroid carcinoma. Arch Surg. 2001;136:878–85.
Shane E. Clinical review 122: parathyroid carcinoma. J Clin Endocrinol Metab. 2001;86:485–93.
Wei CH, Harari A. Parathyroid carcinoma: update and guidelines for management. Curr Treat Options Oncol. 2012;13:11–23.
Hundahl SA, Fleming ID, Fremgen AM, Menck HR. Two hundred eighty-six cases of parathyroid carcinoma treated in the U.S. between 1985 and 1995: a National Cancer Data Base Report. The American College of Surgeons Commission on Cancer and the American Cancer Society. Cancer. 1999;86:538–44.
Lee PK, Jarosek SL, Virnig BA, Evasovich M, Tuttle TM. Trends in the incidence and treatment of parathyroid cancer in the United States. Cancer. 2007;109:1736–41.
Busaidy NL, Jimenez C, Habra MA, et al. Parathyroid carcinoma: a 22-year experience. Head Neck. 2004;26:716–26.
Harari A, Waring A, Fernandez-Ranvier G, et al. Parathyroid carcinoma: a 43-year outcome and survival analysis. J Clin Endocrinol Metab. 2011;96:3679–86.
Kleinpeter KP, Lovato JF, Clark PB, et al. Is parathyroid carcinoma indeed a lethal disease? Ann Surg Oncol. 2005;12:260–6.
Givi B, Shah JP. Parathyroid carcinoma. Clin Oncol. 2010;22:498–507.
Asare EA, Sturgeon C, Winchester DJ, et al. Parathyroid carcinoma: an update on treatment outcomes and prognostic factors from the National Cancer Data Base (NCDB). Ann Surg Oncol. 2015;22:3990–5.
Iacobone M, Lumachi F, Favia G. Up-to-date on parathyroid carcinoma: analysis of an experience of 19 cases. J Surg Oncol. 2004;88:223–8.
Wiseman SM, Rigual NR, Hicks WL Jr, Popat SR. Parathyroid carcinoma: a multicenter review of clinicopathologic features and treatment outcomes. Ear Nose Throat J. 2004;83:491–4.
Villar-del-Moral J, Jimenez-Garcia A, Salvador-Egea P, et al. Prognostic factors and staging systems in parathyroid cancer: a multicenter cohort study. Surgery. 2014;156:1132–44.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Appendix
Rights and permissions
About this article
Cite this article
Young, S., Wu, J.X., Li, N. et al. More Extensive Surgery May Not Improve Survival Over Parathyroidectomy Alone in Parathyroid Carcinoma. Ann Surg Oncol 23, 2898–2904 (2016). https://doi.org/10.1245/s10434-016-5256-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-016-5256-6