Abstract
Background
Parathyroid carcinoma is a rare disease. Conflicting results on prognostic factors and extent of surgical resection for patients with parathyroid carcinoma have been made based on small sample sizes. A large, robust dataset is needed to help address some of the controversies.
Methods
A retrospective review of patients with parathyroid carcinoma in the National Cancer Data Base from 1985 to 2006 was performed. Characteristics of the cohort and type of treatment were evaluated. Prognostic factors were assessed with Cox proportional hazards regression models and 5- and 10-year OS rates were determined.
Results
There were 733 evaluable patients with a mean age of 56.1 ± 15.3 years (median 57, range 15–89) and mean tumor size of 29.6 ± 18.4 mm (median 25.0 mm, range 10.0–150.0). Tumor size, age at diagnosis, male sex, positive nodal status, and complete tumor resection had hazard ratios for death of 1.02 (1.01–1.02, p < 0.0001), 1.06 (1.05–1.07, p < 0.0001), 1.67 (1.24–2.25, p = 0.0008), 1.25 (0.57–2.76, p = 0.6), and 0.42 (0.22–0.81, p = 0.01), respectively, on multivariable analysis. Patients who had removal of the parathyroid tumor with concomitant resection of adjacent organs had HR for death of 0.70 (0.35–1.41, p = 0.3). The 5- and 10-year OS rates were 82.3 and 66 % respectively.
Conclusions
Patient age, tumor size, and sex have modest effects on survival in patients with parathyroid carcinoma. A staging system with prognostic value for parathyroid carcinoma should include at least these pertinent prognostic factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
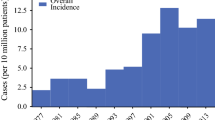
Parathyroid carcinoma is a rare disease, responsible for <1 % of cases of primary hyperparathyroidism.1,2 The diagnosis often is difficult to make but should be considered in patients with marked hypercalcemia (>14 mg/dL) or evidence of local invasion at the time of parathyroidectomy.3 If parathyroid carcinoma is suspected, en bloc resection of the parathyroid tumor is recommended.3,4 There is no consensus for the role of ipsilateral thyroid lobectomy and central compartment lymph node dissection, because the extent of surgical resection has not been found to correlate with improved survival.1,5 Histologic confirmation of parathyroid carcinoma can be challenging but is suggested by the presence of mitotic figures, capsular or vascular invasion, or thick fibrous bands.3,4,6 Estimated 5- and 10-year overall survival (OS) rates are 78–85 and 49–70 % respectively.2,4,5,7,8
The majority of studies on parathyroid carcinoma have been single-institution, small, retrospective reviews, which have reported conflicting outcomes. Two studies utilizing data from large national databases [National Cancer Data Base (NCDB) and Surveillance, Epidemiology and End Results (SEER)] have provided important insights to the incidence and treatment patterns of parathyroid carcinoma2,7 Limitations of these studies have been the substantial number of patients with missing data and lack of multivariable assessment of factors prognostic for survival. There is currently no formal American Joint Committee on Cancer (AJCC) TNM staging for parathyroid carcinoma. The prognostic value of size and nodal status for patients with parathyroid carcinoma remain controversial.4,7,9,10
A sample size with adequate power is needed to address prevailing controversies about prognostic factors and treatment outcomes for patients with parathyroid carcinoma2,5,8,11 Therefore, the purpose of this study was to utilize the NCDB to: (1) determine prognostic factors; (2) evaluate the types and frequency of surgical intervention; and (3) determine overall survival in patients with parathyroid carcinoma.
Methods
A retrospective analysis was performed of a cohort of patients with parathyroid carcinoma in the NCDB from 1985 to 2006. The NCDB is jointly supported by the Commission on Cancer of the American College of Surgeons and the American Cancer Society; information on demographic, tumor, treatment factors, and outcomes for patients diagnosed with cancer across the United States is collected by certified cancer registrars, who undergo routine audits. Approximately 70 % of all newly diagnosed cancers from approximately 1500 hospitals are captured.
Patients with the primary site code C75.0 were selected. Only patients with International Classification of Diseases for Oncology (ICD, 2nd and 3rd editions) histology codes 8000, 8010, 8140, and 8290 were included. Variables of interest were sex, age at diagnosis, tumor size, nodal status, extent of surgical resection, use of radiation therapy, and vital status. In the NCDB, extent of initial surgical resection for parathyroid carcinoma is coded as: (1) local tumor destruction/excision; (2) simple/partial surgical removal; (3) total/complete surgical removal (“complete excision of the parathyroid mass”); (4) debulking; (5) radical surgery (removal of the parathyroid mass with a resection in continuity (partial or total removal) with other organs (usually ipsilateral thyroid lobe); and (6) surgery, not otherwise specified (NOS). For purposes of analysis and meaningful clinical interpretation, extent of surgery was recombined as follows: (1) no surgery; (2) incomplete surgical removal, including local tumor destruction/excision, simple/partial surgical removal, and debulking; (3) complete surgical removal; and (4) radical surgery. Patients with missing tumor size or with reported tumor sizes of <1 or >15 cm were considered outliers and excluded from the analysis.
Statistical Analysis
Statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC). Statistical significance was assumed for p values <0.05. Data for continuous variables were reported as mean ± standard deviation (SD). Discrete values were reported as number with corresponding percentage. Hazard ratios (HR) were presented as point estimates with 95 % confidence intervals (CI). The primary outcome was assessment of the factors prognostic for survival while OS was the secondary outcome of interest. A univariable Cox proportional hazards regression model was used to predict mortality based on extent of surgery, receipt of radiation treatment, nodal status, and tumor size. A multivariable Cox proportional hazards regression model to predict mortality was built using tumor size, age, sex, nodal status, and extent of surgery. The variables included in the multivariable Cox model were based on availability, sample size, and clinical validity from previous studies.2,4,5,8 The 5- and 10-year OS estimates for the evaluable cohort were calculated using the Kaplan–Meier method; OS was calculated from date of diagnosis to the date of death. Patients who were alive at last follow-up were censored.
Sensitivity analysis of tumor size on survival was performed with size as a continuous variable, dichotomized into ≤4 or >4 cm and finally into thresholds of 1–1.99, 2–3.99, and >4 cm, based on previous literature.2,10
Results
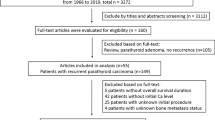
The initial cohort included 1526 patients; patients with missing tumor size (n = 659), tumor size <1 cm (n = 103), or >15 cm (n = 5) and patients with parathyroid carcinoma diagnosed at the time of autopsy (n = 26) were excluded. The final cohort included 733 patients, of which 180 (24.6 %) had all variables present (Table 1). The mean age was 56.1 ± 15.3 years (median 57 years; range 15–89); 406 (55.4 %) were females. The mean tumor size was 29.6 ± 18.4 mm (median 25.0 mm, range 10.0–150.0).
The 5- and 10-year OS rates were 82.3 and 66 %, respectively (Fig. 1). Median survival was 14.3 years with median follow-up of 65.1 months (range <1 month to 26 years).
Assessment of Prognostic Factors
Univariable Analyses
Patients who had complete or incomplete removal of their tumor experienced improved survival compared with those who had no surgical therapy (Table 2). Patients who underwent “incomplete” tumor removal had a 47 % decrease in the risk of death (HR 0.47, 95 % CI 0.26–0.83; p = 0.01), whereas complete tumor removal decreased the risk of death by 39 % (HR 0.39, 95 % CI 0.20–0.75; p = 0.005). Radical surgery was not associated with improved survival in this cohort (HR 0.54, 95 % CI 0.27–1.06; p = 0.07).
Of the 51 (7.0 %) patients who received radiation treatment, there was no improvement in rates of survival compared with the 674 (92 %) patients who did not receive radiation treatment (HR 1.24, 95 % CI 0.75–2.05; p = 0.4; Table 2).
There were 553 (75.4 %) patients whose nodal status was unknown; 157 (21.4 %) and 23 (3.1 %) patients had N0 and N1 status, respectively. Compared with N0 status, N1 status was not associated with an increased risk of death (HR 1.62, 95 % CI 0.75–3.54; p = 0.2), although an unknown nodal status was associated with an increased risk of death (HR 1.52, 95 % CI 1.04–2.22; p = 0.03; Table 2).
Patients with tumor size >4 cm had an increased risk of death (HR 1.91, 95 % CI 1.35–2.69; p = 0.0002; Table 2).
Multivariable Analysis
On multivariable analysis, positive nodal status (N1) was still not associated with an increased risk of death (HR 1.25, 95 % CI 0.57–2.76; p = 0.6; Table 3). When adjusted for nodal status, sex, age at diagnosis, and extent of surgical resection, each centimeter increase in tumor size was associated with increased risk of death by 2 % (HR 1.02, 95 % CI 1.01–1.02; p < 0.0001; Table 3). For each year increase in age, there was an associated 6 % increase in the risk of death when nodal status, sex, tumor size, and extent of resection were adjusted for (HR 1.06, 95 % CI 1.05–1.07; p < 0.0001; Table 3). Compared with females, males had a 67 % increase in the risk of death (HR 1.67; 95 % CI 1.24–2.25; p = 0.0008; Table 3).
Discussion
Parathyroid carcinoma is a rare cause of primary hyperparathyroidism. This study represents one of the largest reported cohorts of patients and demonstrates that on multivariable analysis, negative prognostic factors for patients with parathyroid carcinoma include older age at the time of diagnosis, increasing tumor size, and male sex. Complete or partial tumor removal was associated with improved survival but radical surgery did not decrease the risk of death. Neither positive nodal status nor receipt of radiation treatment was associated with improved survival.
Older age has previously been shown to predict poorer survival in patients with parathyroid carcinoma.2,8 Although a small study of 37 patients did not find age to be prognostic for survival, using SEER data, Lee et al. found increasing age to be associated with decreased survival (HR 2.23; p < 0.0001) on univariable analysis2,5 In the current study, after multivariable analysis, age also was prognostic for survival, with older patients having an increased risk of death.
There are conflicting data in previously published studies on the effect of nodal status on the risk of death. Utilizing the SEER database, Lee et al. reported no increased risk of death (HR of 2.84; p = 0.227) in patients with N1 disease.2 Similarly, among a cohort of 286 patients in the NCDB from 1985 to 1995, only 8 had positive lymph nodes and 5-year OS rates were 82.6 and 83.3 % for patients with N1 and N0 disease, respectively.7 In contrast to the aforementioned, other studies have shown N1 disease to be a risk factor for decreased survival, with reported relative risks of 6.16 (95 % CI 0.88–42.85; p < 0.01) and 4.27 (95 % CI 1.19–15.30; p < 0.05).5,10 The findings of our study suggest that positive lymph node status is not associated with increased mortality when age, tumor size, and extent of resection are adjusted for. This finding, however, should be interpreted with caution given the large number of patients with unknown nodal status (75 %). The variable impact of nodal status on survival between our study and others may be due to the large sample size and use of multivariable analysis.
In contrast to other studies, tumor size, assessed as a continuous variable in the multivariable Cox model, was found to predict survival2,10 Two previous studies had analyzed tumor size as categorical variables, using thresholds of 0–1.9, 2–3.9, and ≥4 cm and <4 or >4 cm, respectively, neither finding tumor size to be associated with an increased risk of death.2,10 In the current cohort, tumor size >4 cm was associated with increased risk of death; however, size categorized into 0–1.99, 2–3.99, and ≥4 cm did not predict increased risk of death.2,10 Similar to our results, Hsu et al. found tumor size ≥3 cm to be associated with an increased risk of death.12
Most experts agree that in the patient with a known or suspected diagnosis of parathyroid carcinoma, an ipsilateral thyroid lobectomy with en bloc resection of the parathyroid gland should be performed4 In this NCDB data, “complete” and “incomplete” tumor resection were both associated with improved survival compared with patients in whom no surgical treatment was offered. The resolution of hyperparathyroidism decreases the effects of chronic intractable hypercalcemia, which is the usual cause of death among patients with parathyroid carcinoma. Aggressive surgical resection did not improve survival and may be due to associated comorbidities and unique biology of the tumor in this cohort. Although not assessed in this study, the cohort who had resection of adjacent structures or organs may have had a variant of disease that was more locally aggressive. In a large national database, it is not possible to capture the phenotypic characteristics of parathyroid carcinoma; for example, hard, fixed, firm, and locally adherent to surroundings (i.e., recurrent laryngeal nerve, ipsilateral thyroid lobe, esophageal outer wall) versus large glands that are not locally fixed but penetrate or have local satellite tumor burden. Both phenotypes are likely affected by quantity of disease burden and other adverse prognostic factors that may not be captured by the NCDB; hence the lack of association with improved survival.
There have been calls for a unified staging system for parathyroid carcinoma to facilitate standardized data collection, to develop standard treatment guidelines, and to enable comparison of treatment groups. Shaha and Shah proposed a TNM staging system for parathyroid carcinoma wherein T1: tumor <3 cm, T2: tumor >3 cm, T3: tumor of any size with invasion of the surrounding soft tissues, T4: massive central compartment disease invading the trachea and esophagus or recurrent disease were combined with nodal status and presence or absence of metastasis to define stage groups.9 A validation study by Talat and Schulte using 330 patients with parathyroid carcinoma did not find the proposed TNM staging system by Shaha and Shah to show significant differences in survival between stage groups.10 Talat and Schulte proposed an anatomic staging system for parathyroid carcinoma in which the tumor categories are defined by capsular invasion (T1), surrounding soft tissue invasion excluding trachea, esophagus, and larynx (T2), vascular invasion (T3), and invasion of vital organs, such as hypopharynx, trachea, esophagus, larynx, recurrent laryngeal nerve, or carotid artery (T4)10 This staging system has been validated with a cohort of 82 patients.11 Although the NCDB data cannot validate this proposed anatomic staging system due to the lack of specific variables on microscopic and macroscopic invasion, this study did not find nodal status to be prognostic. Therefore, in the absence of an adequately powered sample size to validate the proposed staging system, the utility of an anatomic staging system that includes nodal status in patients with parathyroid carcinoma is not clear.
Limitations of this study include those inherent to a retrospective review of a large national database, including missing tumor size, nodal status, calcium and parathyroid hormone levels, and potentially discrepant coding for the extent of surgery. However, the characteristics of patients excluded due to lack of information regarding tumor size and nodal status did not differ from those included in the final analysis. Disease-specific mortality is not available in the NCDB; therefore, OS was chosen as the main endpoint. Furthermore, the diagnosis of parathyroid carcinoma can be challenging and it is possible that some recorded cases may not be carcinomas. However, only histologic codes that are consistent with carcinoma were selected and our results of 5- and 10-year OS rates are similar to single institution studies in which histologic confirmation of diagnosis were performed5,8 Finally, while surgeon’s experience may be an important factor in the adequacy of treatment and hence survival, data on surgeon’s operative experience are not available in the NCDB at this time.
Despite these limitations, this study represents one of the largest reported cohorts of patients with parathyroid carcinoma to allow multivariable assessment of prognostic factors. Age at diagnosis, tumor size, and sex are important factors that should be considered when evaluating prognosis. While positive nodal status did not predict increased risk of death on multivariable analysis in this study, the large number of patients with missing data on nodal status calls for cautious interpretation of the prognostic value of lymph node status for this rare disease. This work also highlights the gaps that exist in the quality of data for rare diseases in large national registries and the need for all stakeholders to engage. Future work should seek to develop a prognostic stratification system that incorporates clinical factors, evidence of microscopic and macroscopic invasion, and other anatomic factors; creation of such a system could allow for improved assessment of an individual’s risk of recurrence and rate of survival and lay the foundation for creation of treatment guidelines for patients suspected to have parathyroid carcinoma.
References
Busaidy NL, Jimenez C, Habra MA, et al. Parathyroid carcinoma: a 22-year experience. Head Neck. 2004;26:716–26.
Lee PK, Jarosek SL, Virnig BA, et al. Trends in the incidence and treatment of parathyroid cancer in the United States. Cancer. 2007;109:1736–41.
Al-Kurd A, Mekel M, Mazeh H. Parathyroid carcinoma. Surg Oncol. 2014;23:107–14.
Kebebew E. Parathyroid carcinoma. Curr Treat Options Oncol. 2001;2:347–54.
Harari A, Waring A, Fernandez-Ranvier G, et al. Parathyroid carcinoma: a 43-year outcome and survival analysis. J Clin Endocrinol Metab. 2011;96:3679–86.
Wei CH, Harari A. Parathyroid carcinoma: update and guidelines for management. Curr Treat Options Oncol. 2012;13:11–23.
Hundahl SA, Fleming ID, Fremgen AM, et al. Two hundred eighty-six cases of parathyroid carcinoma treated in the U.S. between 1985-1995: a National Cancer Data Base Report. The American College of Surgeons Commission on Cancer and the American Cancer Society. Cancer. 1999;86:538–44.
Sandelin K, Auer G, Bondeson L, et al. Prognostic factors in parathyroid cancer: a review of 95 cases. World J Surg. 1992;16:724–31.
Shaha AR, Shah JP. Parathyroid carcinoma: a diagnostic and therapeutic challenge. Cancer. 1999;86:378–80.
Talat N, Schulte KM. Clinical presentation, staging and long-term evolution of parathyroid cancer. Ann Surg Oncol. 2010;17:2156–74.
Schulte KM, Gill AJ, Barczynski M, et al. Classification of parathyroid cancer. Ann Surg Oncol. 2012;19:2620–8.
Hsu KT, Sippel RS, Chen H, et al. Is central lymph node dissection necessary for parathyroid carcinoma? Surgery. 2014;156:1336–41; discussion 1341.
Acknowledgments
Elliot A. Asare, MD, is supported by the American College of Surgeons Clinical Scholars in Residence Program.
Disclosures
All authors have no financial disclosures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Asare, E.A., Sturgeon, C., Winchester, D.J. et al. Parathyroid Carcinoma: An Update on Treatment Outcomes and Prognostic Factors from the National Cancer Data Base (NCDB). Ann Surg Oncol 22, 3990–3995 (2015). https://doi.org/10.1245/s10434-015-4672-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4672-3