Abstract
Introduction The Preoperative Chemotherapy in Primary Operable Breast Cancer (POCOB) study was designed to compare preoperative with postoperative chemotherapy in patients with early breast cancer concerning breast conserving therapy (BCT) procedures, disease free survival (DFS) and overall survival (OS). Methods Patients (n = 698) with early breast cancer were enrolled between 1991 and 1999 and randomized between preoperative versus postoperative chemotherapy (four cycles of fluorouracil, epirubicin, and cyclophosphamide). Endpoints were BCT procedures, DFS, OS, and tumor response to preoperative chemotherapy. In addition, tumor tissue was collected for translational research and the following markers were examined: ER, PgR, HER2, p21, p53, and bcl-2 expression. Results With a median follow-up of 10 years, there was no statistically significant difference between the two treatment arms for OS (HR = 1.09; 95%CI 0.83–1.42; P = 0.54), DFS (HR = 1.12; 95%CI 0.90–1.39; P = 0.30), or locoregional recurrences (LRR, HR = 1.16; 95%CI 0.77–1.74). Preoperative chemotherapy was associated with an increase in BCT rates. BCT in part feasible due to tumor downsizing after preoperative chemotherapy was not correlated with higher LRR or worse OS compared to BCT which was feasible without downsizing of the tumor. Using available tumor material, only tumor stage, nodal stage, and grade were independent prognostic factors for overall survival. Conclusions Preoperative chemotherapy does not result in a difference in OS or DFS compared to postoperative chemotherapy in patients with early breast cancer. Moreover, it increases BCT rates with no significant increase of LRR. This implies that preoperative chemotherapy is a safe procedure for patients with early breast cancer, even after a follow-up period of 10 years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Preoperative, primary, or neoadjuvant systemic therapy is systemic therapy before local treatment. This form of initial treatment is widely used and has become increasingly common in the management of patients with (large) early breast cancer. Preoperative chemotherapy was introduced in the 1980s and was based on several translational hypotheses. First, the Goldie–Coldman hypothesis, which implies that out of an increasing tumor cell population an ever expanding number of drug-resistant phenotypic variants arise due to spontaneous somatic mutations [1]. This occurrence of resistant cells can be minimized by initiating chemotherapy as soon as possible. Secondly, surgical removal of tumor in animal models led to an increase in labeling index of metastasis and in circulating growth-stimulating factors [2–4]. Chemotherapy administrated before surgery could prevent these kinetic changes [5]. These hypotheses were the basis for several randomized studies, initiated in the end of the last century, comparing preoperative chemotherapy with the same regimen of chemotherapy administered postoperative [6–12].
None of these trials showed differences in disease free survival (DFS) and overall survival (OS) between patients in the preoperative and postoperative groups. In addition, provided that patients undergo surgical excision of the tumor, locoregional recurrence (LRR) rates are not increased. This was also the case when all trials were analyzed in a Cochrane analysis [13]. Although these randomized trials have not shown a survival advantage, use of preoperative chemotherapy has several advantages over postoperative chemotherapy. First, tumor response can be monitored in vivo and appropriate changes can be made in case of drug resistance. Second, it allows downsizing of tumors, making previously ineligible patients eligible for breast conserving therapy (BCT). Third, preoperative treatment is the keystone for translational research.
In 1991, the European Organization for Research and Treatment of Cancer (EORTC) initiated a randomized trial (EORTC trial 10902, or the Preoperative Chemotherapy in Operable Breast Cancer, POCOB trial) to compare preoperative to postoperative chemotherapy in patients with early breast cancer. Objectives of this trial were: (1) to determine whether preoperative chemotherapy would permit more BCT by reducing the size of the primary tumor, (2) to determine DFS and OS in both groups, and (3) to evaluate the tumor response to preoperative chemotherapy and correlate this to DFS and OS.
Findings with respect to the 5 year outcome, BCT rates, response rates, and toxicity have been published previously [9]. Although there were no significant differences in OS and DFS between both groups, preoperative chemotherapy did allow more BCT. Additionally, translational research suggested that p53 expression is correlated with tumor response to preoperative chemotherapy [14]. This report updates the clinical and translational outcome results throughout 10 years of follow-up.
Patients and methods
Patients and treatment assignment
Women were enrolled in 17 institutions in 14 countries between April 1991 and May 1999. Eligibility criteria and treatment have been described previously [9]. In summary, eligible patients had primary early breast cancer (T1c, T2, T3, T4b, N0-1, and M0), preferable diagnosed by core needle biopsy or by fine needle aspiration cytology as part of triple diagnosis. All patients gave informed consent before entering into the trial and ethics authorities approved the protocol before enrolment of patients began. Randomization was performed centrally by the EORTC Data Center. Stratification factors were: institution, age, clinical tumor size, clinical nodal status, and planned indicated type of surgery. Patients were randomly assigned to receive surgery in combination with either preoperative or postoperative chemotherapy. Surgery consisted out of modified radical mastectomy or BCT (lumpectomy plus axillary dissection and irradiation of the whole breast). Additionally, radiotherapy was indicated in all cases where surgery was not considered to be radical. Chemotherapy consisted of four cycles of preoperative fluorouracil 600 mg/m2, epirubicin 60 mg/m2, and cyclophosphamide 600 mg/m2 (FEC) administered intravenous, at 3 week intervals. Patients who were ≥50 years of age were considered to be postmenopausal and received tamoxifen 20 mg daily for at least 2 years, regardless of the estrogen receptor (ER). All patients were followed up until death.
Tumor response
The primary tumor and the axillary lymph nodes were clinically estimated (palpation and mammography) before randomization and at time of surgery. The product of the two greatest perpendicular diameters was used to compare tumor size before and after chemotherapy, as defined by the International Union Against Cancer criteria [15]. The absence of clinical detectable malignant disease determined by palpation as well as mammography was categorized as clinical complete response (cCR). The absence of microscopic residual tumor cells at the primary site and axillary lymph nodes was categorized as pathological complete response (pCR). A partial response (PR) was defined as a decrease of tumor size by 50% or more. Progressive disease (PD) was defined as an increase of 25% in tumor size after a minimum of two courses of preoperative chemotherapy. In patients with clinically negative nodes at randomization, development of palpable nodes during the administration of preoperative chemotherapy was considered evidence of PD. Patients whose tumor did not meet the criteria for cCR, PR, or PD were considered as having stable disease (SD).
Outcome measures
OS was defined as the time between randomization and death from any cause. DFS was defined as the time between randomization to disease relapse (including LRR, distant metastases, secondary primary tumors, and contralateral breast cancers) or death, depending which came first. LRR was defined as a recurrence in the ipsilateral breast or in the ipsilateral regional lymph nodes, including supraclavicular nodes.
Immunohistochemical analysis of collected material
Blocks were collected from resection specimens and core needle biopsies in case of preoperative treatment taken before the start of chemotherapy in order to avoid interference of the chemotherapeutic regime with expression levels of oncogenic markers. All immunohistochemical analyses were performed in one reference laboratory and results were assessed two pathologists who were unaware of clinical outcome of patients. Invasive carcinomas were histologically graded according to the method of Bloom and Richardson, adapted by Elston and Ellis. ER, progesterone receptor (PgR), humane epidermal growth factor receptor 2 (HER2) expression, p53 accumulation, p21, and bcl2 expression were assessed as described previously [14].
Statistics
Patients were analyzed according to their assigned treatment regardless of compliance or cross-over. Survival curves were estimated using the Kaplan–Meier method. The two treatment arms were compared using log-rank test for the time-to-event endpoints. Cox proportional hazards model was used to compute relative risks and 95% confidence intervals (CI). All data were analyzed using the statistical package SPSS for Windows 15.0 (SPSS Inc, Chicago, IL, USA). Descriptive data are given as mean (SD) or median (Range). Pearson’s chi-square or Fisher’s exact test was used to compare frequencies among groups. LRR are reported as cumulative incidence functions, after accounting for death as competing risk [16]. All testing was two-tailed with 0.05 as level of significance [17]. The trial was designed to detect a 10% survival difference at 5 years (from 75% to 85%) with 80% power, for which 102 events were needed.
For DFS and OS, variables were examined using univariate Cox regression to determine univariate associations. Multivariate analyses were performed using Cox proportional hazards model entering significant variables (defined as those with P < 0.1) of univariate analysis.
Results
Patients
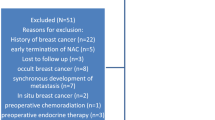
Of the 698 patients, 350 patients were randomized to receive preoperative chemotherapy, and 348 patients were randomized to receive postoperative chemotherapy. Tumor and patients characteristics were well distributed between the two groups (Table 1). Twenty-one patents were ineligible. Median follow-up was 10 years (0–14 years).
Overall survival
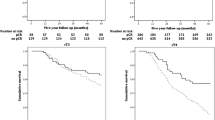
The 10 year OS was 66% in the postoperative group (104 deaths) and 64% in the preoperative group (111 deaths). Similar to the previous publication, no significant differences in survival between the two treatment arms were observed (hazard ratio (HR) = 1.09; 95%CI 0.83–1.42, P = 0.54; Fig. 1a).
Relapses
To date, 332 patients (48%) have experienced relapse of disease, new primary, and/or death. DFS rates after 10 years: 50% in the postoperative group 48% and in the preoperative group (HR = 1.12; 95%CI 0.90–1.39, P = 0.30; Fig. 1b): There have been 44 LRR in the postoperative group and 49 in the preoperative group; this difference is not statically significant (HR = 1.16; 95%CI 0.77–1.74, P = 0.48; Fig. 2). There have been 122 distant recurrences in the postoperative group and 141 in the preoperative group; again, this is not a statistically significant difference (HR = 1.18; 95%CI 0.92–1.50, P = 0.19). To date, 63 patients (9%) have experienced new primary disease; 34 in the postoperative versus 29 in the preoperative group. Likewise there was no difference between the two arms in new primaries (HR = 0.86; 95%CI 0.52–1.41, P = 0.55).
Breast conserving therapy and locoregional recurrences
As previously published, the BCT rate was higher in the preoperative group than in the postoperative group (35% vs. 22% respectively) [9]. However, in the same publication it was stated that patients planned for mastectomy but undergoing BCT after tumor downsizing did worse in terms of OS compared to patients who were initially allotted to receive BCT and treated according to plan. This difference cannot be observed after a follow-up of 10 years. We compared three groups: the first group consisting of patients in the postoperative group who were treated with BCT (n = 64); the second group containing patients in the preoperative group who were initially eligible for BCT (n = 63); and the third group composed of patients in the preoperative group who became eligible for BCT due to tumor downsizing (n = 58). There were no statistically significant differences in LRR (group 1 vs. 2 and 3; HR = 1.00; 95%CI 0.46–2.15 and HR = 1.10; 95%CI 0.50–2.39; overall P = 0.97) or in OS (group 1 vs. 2 and 3; HR = 1.03; 95%CI 0.51–2.09 and HR = 1.33; 95%CI 0.66–2.66; overall P = 0.67) (Fig. 3). BCT after tumor downsizing is not associated with an increased incidence of LRR.
Comparison of (a) locoregional recurrence and (b) overall survival of patients treated with breast conservation surgery. Group I: patients in the postoperative group who were treated with breast conserving surgery. Group II: patients in the preoperative group who were initially eligible for breast conserving surgery. Group III: patients in the preoperative group who became eligible for breast conserving surgery due to tumor downsizing. No statistically significant differences between these groups concerning locoregional recurrence and overall survival are observed
Association between pathological tumor response and outcome
pCR was compared to no pCR with respect to LRR and OS. No statistically significant differences were seen in our population (resp. HR = 0.91; 95%CI 0.22–3.75, P = 0.89 and HR = 4.77; 95%CI 0.67–34.15, P = 0.12).
Translational research
Paraffin material was available from 117 patients from the preoperative group and 32 patients from the postoperative group. Results concerning correlation between cCR, pCR, and patient and tumor characteristics have been published before [14]. With a follow-up of almost 10 years, independent prognostic factors for DFS were age, pathological tumor and nodal stage, performed surgery, use of tamoxifen, and p21 expression (Table 2). In multivariate analysis, younger age, positive nodal stage, and omission of tamoxifen were correlated with a shorter DFS (Table 3). Independent prognostic factors for OS were pathological tumor and nodal stage, use of tamoxifen, multifocal disease and tumor grade (Table 2). In multivariate analysis, higher tumor stage, positive nodal stage and higher grade were correlated with a shorter OS (Table 3).
Discussion
This long term follow-up analysis shows that preoperative chemotherapy increase BCT rates without increasing LRR rates. Preoperative chemotherapy is a commonly used treatment option for locally advanced breast cancer and is used increasingly in early breast cancer. However, some physicians, especially surgeons, still have a threshold using preoperative chemotherapy in early breast cancer patients. The main issues are: (1) Does preoperative chemotherapy have a negative effect on LRR? (2) Which patients treated with BCT after preoperative chemotherapy have a higher change of LRR? (3) How can the tumor be localized after preoperative chemotherapy, especially after cCR? (4) What is optimal treatment of the axilla, especially after the introduction of the sentinel lymph node procedure (SLNP)? (5) Which patients should be selected? (6) What is the change on PD, is fear for PD justified?
Does preoperative chemotherapy has a negative effect on LRR?
Preoperative chemotherapy allows tumor downsizing in approximately 26% of patients and therefore less extensive surgery is needed [6–10]. In studies comparing preoperative to postoperative chemotherapy, more LRR were seen in patients receiving preoperative chemotherapy. However, this difference was largely influenced by three studies in which some patients did not receive surgery but only radiotherapy after cCR. In one of these trials, LRR percentage was 34% after a follow-up of 10 years [8]. When these three studies are excluded from further analysis, no statistically significant differences were seen in LRR between patients treated with preoperative or postoperative chemotherapy [13]. Therefore, it can be concluded that it is not permitted to omit surgery after preoperative chemotherapy.
Additionally, there has been concern regarding employment of BCT after downsizing due to preoperative chemotherapy. When comparing tumors initially feasible for BCT to tumors having become BCT-feasible after downsizing, we found no differences in LRR or OS. This in contrast to our previous publication where it was stated that downsized BCT was correlated with worse survival (HR = 2.53; 95%CI 1.02–6.25) [9]. After the first year, patients treated with BCT feasible after downsizing of the tumor have a slightly worse survival than patients with initially feasible BCT. However, both survival curves congregate after 8 years and after this period no difference can be seen between both groups. It was not possible to observe this in the previous publication due to the short follow-up. The current analyses include more patients with a longer follow-up and indicate that BCT after downsizing of the tumor is comparable to initial BCT without preoperative treatment and is not associated with an increased LRR rate or decreased OS. BCT safety after tumor downsizing or with a cCR is also observed in other studies. In the M.D. Anderson Cancer Center, LRR rate was studied in patients with breast cancer who underwent segmental mastectomy after a cCR on preoperative chemotherapy [18]. An excellent locoregional control was observed in these patients: just 3 of 109 patients developed a LRR after a median follow-up of almost 7 years.
Which patients treated with BCT after preoperative chemotherapy have a higher change of LRR?
In the same center, an index was developed on a scale of 0–4 which identified subgroups of patients with significantly different rates of LRR after chemotherapy followed by BCT [19, 20]. Patients with a score of 4 had a higher chance of LRR than patients with a lower score. Factors included in this index were clinical N2–N3 disease, lymphovascular invasion, residual pathological tumor size >2 cm, and pathologically multifocal residual disease. This index was validated in a relatively large cohort of patients (n = 815), including patients treated with mastectomy [21]. Only patients treated with BCT and a score of 3–4 had a significantly shorter LRR free period than patients treated with mastectomy. Patients treated with BCT with a score of 0–2 had comparable LRR rates with patients treated with mastectomy with the same score. After validating this index in randomized trials, it can be useful in helping to select optimal surgical treatment after preoperative chemotherapy.
How can the tumor be localized after preoperative chemotherapy, especially after cCR?
In case of a cCR, it is impossible to localize the original tumor. In our study, 22 patients (6%) had a cCR. The regime used in our study is probably considered substandard today and it is likely that cCR rates will increase due to better chemotherapy and better selection of patients. Therefore, it will be necessary to localize the tumor bed with a marker before administrating preoperative chemotherapy. This can be performed by the radiologist making use of clips or in vivo detection markers [22].
What is optimal treatment of the axilla, especially after the introduction of the SLNP?
In the last century, all patients received an axillary lymph node dissection (ALND). In the last decade, the SLNP was successfully introduced to decrease morbidity of local treatment. Normally, SLNP is performed during the operation to identify tumor spread to the lymph node most at risk. It is hypothesized that the axillary drainage can change due to preoperative chemotherapy and therefore influence accuracy of the SLNP. Therefore, an advantage of performing the SLNP before administrating preoperative chemotherapy is an accurate assessment of lymph node involvement. One study showed that sentinel node identification rates were better in patients when the SLNP was performed before, compared to after administrating chemotherapy [23]. However, performing SLNP before chemotherapy does not allow nodal downstaging. In our study, positive clinical node status was 50% in both arms, positive pathological nodal status was 63% in patients receiving postoperative, and 55% in patients receiving preoperative chemotherapy. This can be based on downstaging of the axilla. A recently published prospective study evaluated 54 consecutive breast cancer patients with biopsy-proven axillary nodal metastases at the time of diagnosis [24]. After preoperative chemotherapy, all patients received a SLNP with a complete ALND. The sentinel lymph node identification rate was 98% and 17 patients had no residual axillary disease. This means that, due to downstaging, in 32% of patients morbidity of ALND could be spared. In a meta-analysis of early breast cancer patients (n = 1,273) treated with SLNP and subsequent ALND after preoperative chemotherapy, identification rate of sentinel lymph node ranged from 72% to 100% (pooled estimate of 90%) and sensitivity ranged from 67% to 100% (pooled estimate 88%, 95%CI 85–90) [25]. These data were compared to a large meta-analysis that examined results of SLNP in breast cancer patients (n = 8,059) who did not receive preoperative chemotherapy [26]. Identification rate in this meta-analysis was 90% and the authors concluded that SLNP performed after chemotherapy is reliable. In conclusion, identification rates are almost equal but performing SLNP after preoperative chemotherapy allows downstaging of the axilla and therefore decreased morbidity seen after ALND. Besides this, there is no delay of administration of chemotherapy and there is no need of two surgical procedures [27].
Which patients should be selected?
It likewise remains an issue which patients should be selected for preoperative chemotherapy. While local treatment become less and less extensive, indications for receiving chemotherapy still are increasing. Which patients should receive systemic before local treatment? First of all, preoperative chemotherapy decisions require a multidisciplinary approach where surgeons, oncologists, radiologists, radiation oncologists and pathologists discuss every patient. Without a multidisciplinary team, preoperative systemic therapy should not be offered because of the complexity of approach, monitoring, and evaluation on these patients. If a multidisciplinary team is available then, strictly speaking, any early breast cancer patient who is eligible and has an indication for chemotherapy, can receive this chemotherapy before surgery. If it is not sure if the patient will receive systemic treatment (clinical nodal negative with a very small tumor) then surgery should be advised as primary treatment.
New techniques and development will help with better patient selection. For instance, microarray studies may introduce more tailored treatment schedules based on gene expression risk profiles [28, 29]. However, these profiles are not validated for clinical practice. In our study, none of the studied pathological markers was prognostic or predictive. One of the oldest (validated) prognostic and predictive factor is the ER. It was demonstrated that pCR is more likely to occur in patients with ER negative than ER positive disease [30–33]. Therefore, preoperative chemotherapy may not be the most appropriate preoperative approach for patients with ER positive disease. These patients may benefit more from preoperative hormonal therapy. In a study of 239 postmenopausal breast cancer patients with hormonal positive disease, preoperative chemotherapy (doxorubicin with paclitaxel) was compared with preoperative hormonal therapy (anastrozole or exemestane), both for 3 months [34]. Clinical objective response, time to clinical response, rates of pCR and PD were similar between both treatment groups. Preoperative hormonal and chemotherapy were equal in this patients population. More and more studies are examining the optimal use of preoperative hormonal therapy like the Tamoxifen Exemestane Adjuvant Multicentre Trial II (3 vs. 6 months preoperative therapy with exemestane) and the American College of Surgeons Oncology Group Z1031 study (anastrozole versus exemestane versus letrozole for 4 months preoperative).
What is the change on PD, is fear for PD justified?
One fear to maintain the threshold for preoperative therapy is the chance of PD; there is a possibility that patients initially eligible for surgery can become ineligible for surgery because of tumor growth during chemotherapy. Is this realistic? In our study, 3% of tumors (n = 10) had PD. This is in line with older preoperative chemotherapy studies: PD percentage ranging between 1% and 4% [10, 11, 35, 36]. In one study, reported PD percentage was 12%, however, patients with SD were included [10]. With more recent, more effective chemotherapy regimens it is likely that PD rates decrease. In the German Preoperative Adriamycin and Docetaxel II (GEPARDUO) study, all patients (n = 913) were treated with preoperative chemotherapy. Patients were randomized between doxorubicin combined with docetaxel or with cyclophosphamide followed by docetaxel [37]. PD percentages were 1% and 2% respectively. Forty percent of patients with PD could still be treated with BCT [38]. In the Trial of Preoperative Infusional Chemotherapy (TOPIC), patients (n = 426) were randomized between doxorubicin and cyclophosphamide or epirubicin, cisplatin and fluorouracil; PD rates were 2% and 1% respectively [39]. In conclusion, PD percentages are very low and acceptable. Moreover, in case of PD, it is possible to switch to another chemotherapy regimen or start with local therapy. Therefore, patients can be saved from unnecessary toxic side effects from a therapy which is not effective. It is impossible to determine tumor’s sensitivity to chemotherapy when this is given after local treatment. In case of postoperative chemotherapy and a resistant tumor, patients will only experience toxic side effects and no benefit of chemotherapy.
In summary, long term data showed that preoperative chemotherapy for early breast cancer patients is equal to postoperative chemotherapy concerning DFS and OS. Moreover, BCT rates are increased with no additional increase of LRR. Therefore, BCT after preoperative chemotherapy is not associated with an significant increase in LRR and is a safe procedure.
References
Goldie JH, Coldman AJ (1979) A mathematic model for relating the drug sensitivity of tumors to their spontaneous mutation rate. Cancer Treat Rep 63:1727–1733
Fisher B, Gunduz N, Saffer EA (1983) Influence of the interval between primary tumor removal and chemotherapy on kinetics and growth of metastases. Cancer Res 43:1488–1492
Gunduz N, Fisher B, Saffer EA (1979) Effect of surgical removal on the growth and kinetics of residual tumor. Cancer Res 39:3861–3865
Fisher B, Gunduz N, Coyle J et al (1989) Presence of a growth-stimulating factor in serum following primary tumor removal in mice. Cancer Res 49:1996–2001
Fisher B, Saffer E, Rudock C et al (1989) Effect of local or systemic treatment prior to primary tumor removal on the production and response to a serum growth-stimulating factor in mice. Cancer Res 49:2002–2004
Broet P, Scholl SM, de la Rochefordière A et al (1999) Short and long-term effects on survival in breast cancer patients treated by primary chemotherapy: an updated analysis of a randomized trial. Breast Cancer Res Treat 58:151–156
Cleator SJ, Makris A, Ashley SE et al (2005) Good clinical response of breast cancers to neoadjuvant chemoendocrine therapy is associated with improved overall survival. Ann Oncol 16:267–272
Mauriac L, MacGrogan G, Avril A et al (1999) Neoadjuvant chemotherapy for operable breast carcinoma larger than 3 cm: a unicentre randomized trial with a 124-month median follow-up. Institut Bergonie Bordeaux Groupe Sein (IBBGS). Ann Oncol 10:47–52
van der Hage JA, van de Velde CJH, Julien JP et al (2001) Preoperative chemotherapy in primary operable breast cancer: results from the European Organization for Research and Treatment of Cancer trial 10902. J Clin Oncol 19:4224–4237
Wolmark N, Wang J, Mamounas E et al (2001) Preoperative chemotherapy in patients with operable breast cancer: nine-year results from National Surgical Adjuvant Breast and Bowel Project B-18. J Natl Cancer Inst Monogr 30:96–102
Bear HD, Anderson S, Brown A et al (2003) The effect on tumor response of adding sequential preoperative docetaxel to preoperative doxorubicin and cyclophosphamide: preliminary results from National Surgical Adjuvant Breast and Bowel Project Protocol B-27. J Clin Oncol 21:4165–4174
Rastogi P, Anderson SJ, Bear HD et al (2008) Preoperative chemotherapy: updates of National Surgical Adjuvant Breast and Bowel Project Protocols B-18 and B-27. J Clin Oncol 26:778–785
Mieog JS, van der Hage JA, van de Velde CJ (2007) Preoperative chemotherapy for women with operable breast cancer. Cochrane Database Syst Rev:CD005002
Mieog JSD, van der Hage JA, van de Vijver MJ, van de Velde CJH (2006) Tumour response to preoperative anthracycline-based chemotherapy in operable breast cancer: the predictive role of p53 expression. Eur J Cancer 42:1369–1379
Hayward JL, Carbone PP, Heusen JC et al (1977) Assessment of response to therapy in advanced breast cancer. Br J Cancer 35:292–298
Putter H, Fiocco M, Geskus RB (2007) Tutorial in biostatistics: competing risks and multi-state models. Stat Med 26:2389–2430
Altman DG, Machin D, Bryant TN, Gardner MJ (2000) Statistics with confidence. British Medical Journal Books, Bristol
Peintinger F, Symmans WF, Gonzalez-Angulo AM et al (2006) The safety of breast-conserving surgery in patients who achieve a complete pathologic response after neoadjuvant chemotherapy. Cancer 107:1248–1254
Chen AM, Meric-Bernstam F, Hunt KK et al (2005) Breast conservation after neoadjuvant chemotherapy. Cancer 103:689–695
Chen AM, Meric-Bernstam F, Hunt KK et al (2004) Breast conservation after neoadjuvant chemotherapy: the MD Anderson cancer center experience. J Clin Oncol 22:2303–2312
Huang EH, Strom EA, Perkins GH et al (2006) Comparison of risk of local-regional recurrence after mastectomy or breast conservation therapy for patients treated with neoadjuvant chemotherapy and radiation stratified according to a prognostic index score. Int J Radiat Oncol Biol Phys 66:352–357
Gray RJ, Salud C, Nguyen K et al (2001) Randomized prospective evaluation of a novel technique for biopsy or lumpectomy of nonpalpable breast lesions: radioactive seed versus wire localization. Ann Surg Oncol 8:711–715
Jones JL, Zabicki K, Christian RL et al (2005) A comparison of sentinel node biopsy before and after neoadjuvant chemotherapy: timing is important. Am J Surg 190:517–520
Newman EA, Sabel MS, Nees AV et al (2007) Sentinel lymph node biopsy performed after neoadjuvant chemotherapy is accurate in patients with documented node-positive breast cancer at presentation. Ann Surg Oncol 14:2946–2952
Xing Y, Foy M, Cox DD et al (2006) Meta-analysis of sentinel lymph node biopsy after preoperative chemotherapy in patients with breast cancer. Br J Surg 93:539–546
Kim T, Giuliano AE, Lyman GH (2006) Lymphatic mapping and sentinel lymph node biopsy in early-stage breast carcinoma: a metaanalysis. Cancer 106:4–16
Buchholz TA, Lehman CD, Harris JR et al (2008) Statement of the science concerning locoregional treatments after preoperative chemotherapy for breast cancer: a National Cancer Institute conference. J Clin Oncol 26:791–797
Gianni L, Zambetti M, Clark K et al (2005) Gene expression profiles in paraffin-embedded core biopsy tissue predict response to chemotherapy in women with locally advanced breast cancer. J Clin Oncol 23:7265–7277
Hannemann J, Oosterkamp HM, Bosch CA et al (2005) Changes in gene expression associated with response to neoadjuvant chemotherapy in breast cancer. J Clin Oncol 23:3331–3342
Colleoni M, Viale G, Zahrieh D et al (2004) Chemotherapy is more effective in patients with breast cancer not expressing steroid hormone receptors: a study of preoperative treatment. Clin Cancer Res 10:6622–6628
Tubiana-Hulin M, Stevens D, Lasry S et al (2006) Response to neoadjuvant chemotherapy in lobular and ductal breast carcinomas: a retrospective study on 860 patients from one institution. Ann Oncol 17:1228–1233
Ring AE, Smith IE, Ashley S et al (2004) Oestrogen receptor status, pathological complete response and prognosis in patients receiving neoadjuvant chemotherapy for early breast cancer. Br J Cancer 91:2012–2017
Guarneri V, Broglio K, Kau SW et al (2006) Prognostic value of pathologic complete response after primary chemotherapy in relation to hormone receptor status and other factors. J Clin Oncol 24:1037–1044
Semiglazov VF, Semiglazov VV, Dashyan GA et al (2007) Phase 2 randomized trial of primary endocrine therapy versus chemotherapy in postmenopausal patients with estrogen receptor-positive breast cancer. Cancer 110:244–254
Chua S, Smith IE, A’Hern RP et al (2005) Neoadjuvant vinorelbine/epirubicin (VE) versus standard adriamycin/cyclophosphamide (AC) in operable breast cancer: analysis of response and tolerability in a randomised phase III trial (TOPIC 2). Ann Oncol 16:1435–1441
Therasse P, Mauriac L, Welnicka-Jaskiewicz M et al (2003) Final results of a randomized phase III trial comparing cyclophosphamide, epirubicin, and fluorouracil with a dose-intensified epirubicin and cyclophosphamide + filgrastim as neoadjuvant treatment in locally advanced breast cancer: an EORTC-NCIC-SAKK multicenter study. J Clin Oncol 21:843–850
von Minckwitz G, Raab G, Caputo A et al (2005) Doxorubicin with cyclophosphamide followed by docetaxel every 21 days compared with doxorubicin and docetaxel every 14 days as preoperative treatment in operable breast cancer: the GEPARDUO study of the German Breast Group. J Clin Oncol 23:2676–2685
Loibl S, von Minckwitz G, Raab G et al (2006) Surgical procedures after neoadjuvant chemotherapy in operable breast cancer: results of the GEPARDUO trial. Ann Surg Oncol 13:1434–1442
Smith IE, A’Hern RP, Coombes GA et al (2004) A novel continuous infusional 5-fluorouracil-based chemotherapy regimen compared with conventional chemotherapy in the neo-adjuvant treatment of early breast cancer: 5 year results of the TOPIC trial. Ann Oncol: 15:751–758
Acknowledgements
We thank the patients participating in the trial, the trial committee, the trial investigators, monitors, nurses, data managers, and other support staff. We thank the European Organization of Research and Treatment of Cancer for their continued support. We thank Jos van de Hage and Sven Mieog, Leiden University Medical Center, for their help with the tissue database. This publication was supported by grants 5U10 CA11488-21 through 5U10 CA11488-37 from the National Cancer Institute (Bethesda, Maryland, USA) and by FOCA (Fonds Cancer), Belgium. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Cancer Institute.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
This article is presented in part as poster and oral presentation at the 5th European Breast Cancer Conference, 21–24 March 2006, Nice, France and 13th Congress of the European Society of Surgical Oncology, 30 November–2 December 2006, Venice, Italy.
See appendix for participating institutions and cooperating investigators.
Appendix
Appendix
Cooperating investigators and participating institution:
-
J.-P. Julien, Centre Henri Becquerel, France.
-
M. Tubiana-Hulin, F. Bachelot, Centre René Huguenin, St Cloud, France.
-
T. Delozier, Centre Regional François Baclesse, Caen, France.
-
C.J.H. van de Velde, M.A. Nooy, Leiden University Medical Center, Leiden, the Netherlands.
-
H. Bonnefoi, Hopital Cantonal Universitaire de Geneve, Geneva, Switzerland.
-
J.A. van Zyl, A.G. Muller, University of Stellenbosch, Tygerberg Hospital, Tygerberg, Republic of South Africa.
-
S. Omar, National Cancer Institute, Cairo, Egypt.
-
J. Jassem, J. Jaskiewicz, Medical University of Gdansk, Gdansk, Poland.
-
J.J. Grau, Hospital Clinico y Provencial de Barcelona, Barcelona, Spain.
-
D. Vukotic, Institute of Oncology and Radiology, Belgrade, Federal Republic of Yugoslavia.
-
T. Cufer, M. Snoj, The Institute of Oncology, Ljubljana, Slovenia.
-
O. Ivanova, V.F. Semiglazov, Petrov Research Institute of Oncology, St. Petersburg, Russia.
-
I. Varthalitis, Evangelismos Hospital, Athens, Greece.
-
A. Ezzat, King Faisal Spec. Hospital and Research Center, Riyadh, Saudi Arabia.
Rights and permissions
About this article
Cite this article
van Nes, J.G.H., Putter, H., Julien, JP. et al. Preoperative chemotherapy is safe in early breast cancer, even after 10 years of follow-up; clinical and translational results from the EORTC trial 10902. Breast Cancer Res Treat 115, 101–113 (2009). https://doi.org/10.1007/s10549-008-0050-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-008-0050-1