Abstract
Background
Disseminated tumor cells (DTC) in the bone marrow (BM) of primary breast cancer (BC) patients are a promising surrogate marker of micrometastatic spread and an independent predictor of poor prognosis for disease-free survival (DFS) and overall survival (OS). The present study aims to analyze DTCs as an independent prognostic factor for DFS/OS in tumor biology and bisphosphonate treatment.
Methods
A total of 504 patients with operable primary BC and a median observation time of 72.3 months [lower quartile (LQ) 58.1; upper quartile (UQ) 82.8] have been included. DTCs were detected via immunohistochemistry as MUC-1 positive cells in the BM of 59.13 % (298 of 504) of the patients. The immunophenotyping of cancer cells was achieved immunohistochemically as well.
Results
For luminal A/B carcinoma patients, we observed a significant benefit of BM DTC negativity with respect to DFS (luminal A, P = 0.0498; luminal B, P = 0.0224). In triple-negative patients, DTC-negative BM was associated with a longer OS (P = 0.0326). In a multivariate Cox survival analysis relating to DFS and OS, the DTC status was identified as an independent prognostic factor for DFS in luminal A/B BC (P = 0.0071). A multivariate Cox survival analysis among DTC-positive patients with luminal immunophenotype showed bisphosphonate application (P = 0.0326) to be an independent prognostic factor for DFS.
Conclusions
The findings of our multivariate analyses reveal BM DTC positivity as an independent risk factor for DFS particularly in luminal A/B BC patients. This might be a novel criterion for the identification of candidates most likely to benefit from additional adjuvant therapy possibly including bisphosphonates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Survival of primary breast cancer (BC) patients has continuously improved over the last decades, foremost as a result of earlier diagnosis. In the long term, however, despite surgical treatment and further adjuvant therapy a significant number of patients will still suffer from distant metastasis, since current systemic therapy strategies are able to prevent only a minority of BC recurrences.1–5 Consequently, it is of crucial importance to determine which BC patients will benefit from which therapeutic approach.
This firstly requires the identification of patients who are at high risk for the development of distant metastases. The conventional clinical and tumor-biologic characteristics do not sufficiently take into account the variety of immunological features of the primary tumor or the potency of single BC cells to survive, thus leading to minimal residual disease.2 Therefore, the differentiation of tumor subtypes according to their immunophenotype as well as further characterization of single cells from the micrometastatic spread may be instrumental in better identifying high-risk patients.
Intrinsic BC molecular subtypes can be defined surrogately by a 6-biomarker (ER, PR, Ki-67, HER2, EGFR, and CK 5/6) immunohistologic panel as luminal A, luminal B, luminal HER2, HER2-enriched, basal-like, or triple-negative phenotype-non-basal. In this context, luminal A tumors (ER or PR positive, HER2 negative, Ki-67 < 1 %) have the best clinical prognosis.6
On the other hand, disseminated tumor cells (DTCs) can be detected in the bone marrow (BM) of a major proportion of primary BC patients at the time of first diagnosis, while detection of those cells is not observed in healthy donors.2,7–13 DTCs as a promising surrogate marker of micrometastatic spread (i.e., minimal residual disease) turned out to be an independent predictor of poor prognosis in regard to disease-free and overall survival (OS).2,8,11,14
One promising issue in BC treatment now is the prognostic and clinical relevance of DTCs for risk stratification in BC molecular subtypes. Hartkopf et al. recently published data on the prevalence of DTCs in different intrinsic subclasses of BC, showing a higher incidence especially in more aggressive (ER/PR/HER2-negative) tumors.15 Furthermore, a clinical benefit in DTC-positive patients after bisphosphonate treatment has been detected in general.15 This is in accordance with the data published by Diel et al. in 1998 showing a protective effect of bisphosphonates not only in regard to osseous, but also relating to visceral metastases.16
In the present study, we are building upon a recently published, large monocentric cohort of 1378 primary BC patients with one of the longest follow-ups.2 In this latter publication, a significantly higher incidence of distant metastases, a reduced disease-free survival (DFS), and a diminished OS in DTC-positive patients were observed. From this population we could define a subgroup of 504 patients in whom a tumor-biologic assessment by immunohistochemistry (IHC) had been performed and who were included in the present study. The central question of the present article is now the impact of DTCs within the different intrinsic, tumor-biologic subclasses in regard to overall and DFS as well as the clinical impact of bisphosphonate treatment in those specific subgroups. We, hereby, aim to define novel criteria for the identification of DTC-positive candidates most likely to benefit from additional adjuvant therapy possibly including bisphosphonates.
Methods
Patient Cohort
In a recent study, BM samples were acquired from 1378 primary BC patients in a monocenter observation trial at the Breast Unit of Heidelberg University Hospital, Germany.2 In a subgroup of 504 patients, a tumor-biologic assessment by IHC had been performed. Those patients were included in the present study. The study protocol had been approved by the ethics committee of the University of Heidelberg, Germany. Informed consent was obtained from all participating patients.
From 1987 to 1998, primary BC patients underwent surgery of the breast with BM aspiration for analysis of DTCs. Exclusion criteria were regional or distant metastasis within 3 months after surgery, breast biopsy and/or lumpectomy before definitive surgery, and a history of other malignant disease or simultaneous second primary tumor as well as incomplete follow-up data. Furthermore, neoadjuvantly pretreated patients and patients with recurrent BC have been excluded. If patients received clodronate, the daily dose administered was 1600 mg orally for 2 years.16 Follow-up was performed between March and September 2005 by assessing patients’ records or, if the last visit was more than 6 months before, by contacting the patients or their physicians by mail and/or phone.
Bone Marrow Aspiration, Immunocytology, and Immunohistochemistry
BM samples were acquired under standardized conditions during primary surgery.17 The immunocytochemical staining method was presented in detail in our previous study.8 In short, the aspirate was separated by density centrifugation (Ficoll) and the cell suspension (4–5 × 106 cells) was smeared onto slides. Immunocytochemical staining with the avidin–biotin complex technique was performed using murine monoclonal antibody 2E11 directed against the MUC-1 molecule, which is very common on BC cells while it is absent or poorly expressed in normal mammary gland.18 Thus, the MUC-1-specific antibody 2E11 does positively react with more than 96 % of primary BCs. This method is sensitive enough to recognize 1 positive cell in 106 normal BM cells. Both positive and negative controls were analyzed against 4 smears per patient. The membrane and cytoplasm of tumor cells stained bright red. Smears were defined as positive if containing 1 or more than 1 stained cell. Furthermore, immunopositive cells were only classified as tumor cells if nuclei were clearly enlarged or atypical and clusters of 2 or more positive cells were present (in case of multiple cells). This procedure follows the morphological criteria as proposed by a European Working Group (with coauthor I.D. serving as member).19 All slides were assessed by 2 independent investigators with an interobserver agreement of more than 99 %. In discordant findings, patients were considered to be tumor cell negative. Analyses were done without knowledge of patients’ clinical or histopathological results.
All immunohistochemical stainings regarding the level of HER2/neu and Ki-67 expression as well as the estrogen and progesterone hormone receptor (ERα and PR) status were performed according to protocols of the Department of Pathology, Heidelberg University Hospital. Intrinsic subtypes were defined by IHC measurements of ER, PR, Ki-67, and HER2/neu as surrogate markers. Patients were regarded as HER2/neu-positive only in case of a 3+ score in IHC or amplification in fluorescence in situ hybridization (FISH). Relating to the proliferation index, a threshold of ≥14 % was interpreted as “high” Ki-67 status and discriminated between luminal A and B patients.20,21
Statistics
Correlations of DTCs with established prognostic markers were analyzed by χ 2 test or t test according to the distribution of the data. Distant DFS was defined as survival without the development of distant metastases, while OS means the entire length of time that patients diagnosed with BC are still alive. Survival curves were calculated by means of the Kaplan–Meier estimate, and the comparison of 2 survival curves was based on the log-rank test according to Peto and Peto. A multivariate Cox regression analysis was performed to assess the independent prognostic value of DTCs adjusted for intrinsic phenotype prognosis. The impact of each variable in the Cox regression model was tested by the Wald χ2 test and described by the risk ratio (i.e., the hazard ratio). All reported probabilities are 2-sided, and P values of <0.05 were regarded as statistically significant.
Results
Patient Characteristics
A total of 504 patients with operable primary BC were included in the study cohort.
DTCs as MUC-1 positive cells were detected in the BM of 59.13 % (298 of 504) of those patients. Patient and tumor characteristics, immunophenotypes, and bisphosphonate treatment in relation to the detection rate of BM DTCs are presented in Table 1. Interestingly, the prevalence of DTCs in the patient cohort does not significantly correlate with any of the patients’ clinicopathological characteristics. In particular, no significant difference between the DTC-positive and DTC-negative groups was found with respect to tumor size, histological type, staging, grading, or nodal status. Nor were hormonal receptor (ER/PR), HER2 and proliferation marker Ki-67 statuses statistically varying (Table 1). Of note, surgical approach and adjuvant therapeutic regimens in regard to chemotherapy, endocrine therapy, bisphosphonate treatment, and radiation did not differ either between DTC-positive and DTC-negative groups (Table 1).
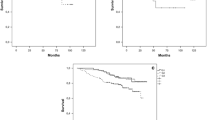
DFS and OS Relating to Immunophenotypes
Next, patient groups arranged according to their immunophenotype were analyzed in a long-term follow-up with a median observation time of 72.3 months [lower quartile (LQ) 58.1; upper quartile (UQ) 82.8]. In this context, luminal HER2 and HER2-enriched groups were merged into a surrogate HER2-positive subtype, which did not imply any changes in the statistical significance compared with the single groups before merging. Figure 1 shows Kaplan–Meier analyses of DFS (Fig. 1a) and OS (Fig. 1b) with respect to the immunophenotype while disregarding the DTC status. As expected, luminal A patients showed the longest survival time relating to both DFS and OS. Interestingly, HER2-positive patients had a poor clinical outcome comparable with that of triple-negative patients, as trastuzumab was not administered in the time when patients underwent surgery. DFS in the luminal A group was significantly longer than that in HER2-positive (P < 0.0001), luminal B (P = 0.0006), and triple-negative (P < 0.0001) groups, respectively. Concordantly, patients with luminal A immunophenotypic BC had also a benefit regarding OS compared with HER2-positive (P < 0.0001), luminal B (P = 0.0066), and triple-negative (P < 0.0001) groups, respectively. These findings are compatible with a representative character of our study cohort.
a Kaplan–Meier analysis of patients’ disease-free survival with respect to the BC immunophenotype while disregarding the BM DTC status. b Kaplan–Meier analysis of patients’ overall survival relating to the BC immunophenotype while disregarding the BM DTC status. HER2 human epidermal growth factor receptor 2
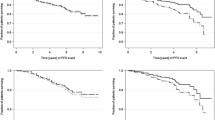
DFS and OS in BM DTCs and Immunophenotypes
Subsequently, the clinical prognosis of all molecular subtypes depending on the presence of DTCs in patients’ BM was analyzed. Table 2 highlights the univariate comparison of disease-free and OS curves in BM DTC+ and BM DTC− patients with regard to the particular immunophenotype. For luminal A and luminal B groups, we observed a significant benefit of BM DTC-negative patients with respect to DFS (luminal A, P = 0.0498; luminal B, P = 0.0224), while the OS of patients with DTC-negative luminal immunophenotypes was not significantly extended. In the subgroup of HER2-positive patients, no influence of DTCs was detected on both overall and DFS. In triple-negative patients, however, DTC-negative BM was associated with a longer OS compared with DTC-positive BM (P = 0.0326).
As patients with luminal immunophenotypic BC and no detectable BM DTCs had turned out to have survival advantages, we consequently performed a multivariate Cox survival analysis relating to DFS and OS with BM DTC status and luminal immunophenotypes as adjusted covariates (Table 3). In this multivariate analysis, DTC status was identified as an independent prognostic factor for DFS in the cohort of luminal BC patients with luminal A and luminal B phenotypes as adjusted prognostic parameters (P = 0.0071). With respect to the OS, DTC status turned out to be only close to statistical significance (P = 0.0786). In the next step, we included all patients into the multivariate analysis and adjusted for HER2 and triple-negative phenotype in addition to luminal A and B as prognostic parameters. In this context, the triple-negative phenotype has been set as reference parameter. In this analysis we did not observe a significant prognostic impact of DTC on DFS (P = 0.1655) or OS (P = 0.1605).
Subgroup Analysis of Bisphosphonate Treatment
Notably, an equivalent number of patients among the DTC-positive and DTC-negative groups have received clodronate-based bisphosphonate therapy (36.9 vs 35.9 %) (Table 1). This raises the question whether bisphosphonate administration might be of prognostic benefit for the treated patient. Interestingly, bisphosphonate therapy turned out to have a significantly positive impact on the DFS only of BM DTC-positive luminal A/B patients (P = 0.0299), while DTC-negative patients’ prognosis was not significantly influenced by bisphosphonate treatment (P = 0.5385). Accordingly, our adjacent multivariate Cox survival analysis relating to DFS and OS of exclusively DTC-positive patients, with luminal immunophenotypes and bisphosphonate therapy as adjusted covariates, is shown in Table 4. This multivariate analysis demonstrates bisphosphonate treatment to be an independent prognostic factor for DFS (P = 0.0326) in the cohort of luminal BC patients, whereas OS does not appear to correlate statistically.
Discussion
In BC most prognostic factors refer to the immunophenotype of the cancer tissue and to common clinical characteristics as tumor size and lymph node status. Meanwhile, the immunocytochemical detection of DTCs in BM of BC patients has also proved to be an independent prognostic factor in that the detection of epithelial cells inside the BM is significantly linked to a poor clinical prognosis.2,8,10,22–28 Nevertheless, the prognostic and clinical relevance of DTCs for risk stratification in BC molecular subtypes remains largely unclear to date.
A pilot trial based on gene expression analysis utilizing cDNA microarrays as well as the TP53 mutation status and HER2 amplification revealed a particularly poor outcome in luminal A subtype patients with DTC-positive BM.29 In the present study, we suggest BM DTC positivity as an independent risk factor for DFS predominantly in luminal A/B BC patients but also for OS in triple-negative patients. Additionally, however, we can show bisphosphonate treatment to be a favorable, independent prognostic factor in luminal A/B BC patients with BM DTCs.
With respect to the role of DTCs as a prognostic factor for OS in triple-negative breast cancer (TNBC) patients, our data obviously concurs with recent findings. Synnestvedt et al. detected a distinct cell subset in the BM of BC patients that correlated with an unfavorable outcome in triple-negative patients relating to overall and DFS.30 Those cells comprised characteristics of DTCs.30 Additionally, Hall et al. reported on the absence of DTCs in TNBC patients who achieved a pathologic complete remission (pCR) after neoadjuvant chemotherapy.31 Patients who achieve a pCR have significantly better outcomes, irrespective of their intrinsic subtype.32,33 TNBC patients with residual disease of the primary tumor following neoadjuvant chemotherapy experienced significantly shorter disease-free and OS.33 The latter finding might suggest a clinical impact of persisting DTCs in triple-negative BC after (neo)-adjuvant chemotherapy. This hypothesis, however, needs proving in further studies using another BM aspiration after adjuvant chemotherapy.
Also relating to BM DTC positivity as an independent risk factor for DFS particularly in luminal A/B BC patients, our results agree with previous findings. In a preliminary study, for instance, Synnestvedt et al. showed a poor prognosis for patients with luminal A phenotype and BM tumor cells.30 Likewise, in further studies of luminal A patients with specific molecular signature, the presence of BM DTCs was associated with significantly reduced survival rates.29,34
Consequently, in search of options to eradicate DTCs, 2 nitrogen-containing bisphosphonates—zoledronate and ibandronate—have been identified as potential agents capable of exerting cytotoxic effects on DTCs.35–38 Zoledronic acid (ZOL) in particular is a well-known inhibitor of tumor angiogenesis, adhesion, invasion, and proliferation steps in the metastatic cascade.39,40 In our subgroup analysis of BC patients with luminal A/B immunophenotype and positive BM DTC status, we were able to show bisphosphonate treatment to be an independent prognostic factor for DFS.
Several trials examining the impact of zoledronate (ZOL) treatment in high-risk early-stage BC were all capable of demonstrating reduced DTC numbers in patients’ BM. These studies suggested that ZOL might deliver its antitumor effect via directly eradicating DTCs with a positive impact on patients’ survival.35–37,41 Large clinical studies, named ABCSG-12 and ZO-FAST, respectively, likewise reported significant benefit in terms of prolonged DFS in premenopausal women if conventional adjuvant BC therapy was combined with ZOL treatment.42–44 The final results of the ABCSG-12 study after 94-month follow-up suggest that twice-yearly ZOL enhances the efficacy of adjuvant endocrine treatment, and this benefit is maintained long-term.43 In the ZO-FAST trial, postmenopausal BC women received adjuvantly the aromatase inhibitor letrozole combined with ZOL.44 At 36-month follow-up, the ZOL group showed a significantly improved DFS.
Those two studies, therefore, are in accordance with our findings showing a clinical benefit of bisphosphonate treatment especially in BC patients with luminal A/B immunophenotype and positive BM DTC status.
In contrast, however, to the aforementioned findings, data from the phase III AZURE study did not suggest a substantial benefit in terms of DFS for ZOL added to standard adjuvant chemotherapy or endocrine therapy in the overall early BC patient group.45,46 This might be inconsistent with our findings. However, zoledronic acid did significantly reduce the development of bone metastases and, for women with established menopause, improved disease outcomes.46 Furthermore, patients from the AZURE trial might be different from those of the present trial, as in the AZURE study 96 % of the patients received adjuvant chemotherapy and all of them showed lymph node involvement. Therefore, a comparison with the present data has to be drawn with caution.
In the adjuvant therapy of operable primary BC patients, inconsistent findings in the literature underscore the importance of defining additional criteria as prerequisite for the identification of candidates most likely to benefit from bisphosphonate treatment. The results of our multivariate analysis suggest BM DTC positivity as an independent risk factor for DFS particularly in luminal A and B BC patients and demonstrate survival advantages for DTC-positive luminal patients receiving bisphosphonates. This data implies potential consequences for reshaping adjuvant therapy strategies including bisphosphonates.
Admittedly, a limitation of our study is the high detection rate of MUC-1 positive cells inside the BM compared with other studies using cytokeratin (CK), epithelial membrane antigen (EMA), or epithelial cell adhesion molecule (EpCam) antibodies. On the other hand, the overall observed impact of immunopositive BM cells on disease-free as well as OS is comparable in all studies regardless of the technique of cell detection used. Clearly, as to date no final consensus has been established to standardize the laboratory protocols for micrometastasis detection, a comparative evaluation of the various DTC immunostaining techniques is highly desirable with respect to sensitivity and specificity rates of the different antibodies available presently.
Our findings are also limited by the retrospective nature of the study. Subgroup analyses should therefore be interpreted with caution. Significant and also nonsignificant findings might be due to a small sample size. Of course, to confirm the clinical benefit of bisphosphonate treatment further prospective trials are needed. In this context, at our institution a nonrandomized, prospective phase II study is currently being performed to analyze the impact of the monoclonal antibody denosumab on DTCs in patients with early-stage breast cancer (NCT01545648).
Last but not least, in future studies, especially gene signature analyses of the primary tumor tissue should be taken into account to further individualize potential adjuvant therapy options.
References
Molloy TJ, Bosma AJ, Baumbusch LO, et al. The prognostic significance of tumour cell detection in the peripheral blood versus the bone marrow in 733 early-stage breast cancer patients. Breast Cancer Res. 2011;13:R61.
Domschke C, Diel IJ, Englert S, et al. Prognostic value of disseminated tumor cells in the bone marrow of patients with operable primary breast cancer: a long-term follow-up study. Ann Surg Oncol. 2013;20:1865–71.
O’Shaughnessy J. Extending survival with chemotherapy in metastatic breast cancer. Oncologist. 2005;10 Suppl 3:20–9.
Cianfrocca M. Prognostic and predictive factors in early-stage breast cancer. Oncologist. 2004;9:606–16.
Cossetti RJD, Tyldesley SK, Speers CH, Zheng Y, Gelmon KA. Comparison of breast cancer recurrence and outcome patterns between patients treated from 1986 to 1992 and from 2004 to 2008. J Clin Oncol. 2014;33:65–73.
Voduc KD, Cheang MCU, Tyldesley S, Gelmon K, Nielsen TO, Kennecke H. Breast cancer subtypes and the risk of local and regional relapse. J Clin Oncol. 2010;28:1684–91.
Mansi JL, Gogas H, Bliss JM, Gazet JC, Berger U, Coombes RC. Outcome of primary-breast-cancer patients with micrometastases: a long-term follow-up study. Lancet. 1999;354:197–202.
Diel IJ, Kaufmann M, Costa SD, Holle R, von Minckwitz G, Solomayer EF, et al. Micrometastatic breast cancer cells in bone marrow at primary surgery: prognostic value in comparison with nodal status. J Natl Cancer Inst. 1996;88:1652–8.
Solomayer E, Diel IJ, Salanti G, Hahn M, Gollan C, Bastert G. Time independence of the prognostic impact of tumor cell detection in the bone marrow of primary breast cancer patients. Clin Cancer Res. 2001;7:4102–8.
Braun S, Pantel K, Müller P, Janni W, Hepp F, Kentenich CR, et al. Cytokeratin-positive cells in the bone marrow and survival of patients with stage I, II, or III breast cancer. N Engl J Med. 2000;342:525–33.
Braun S, Vogl FD, Naume B, Janni W, Osborne MP, Coombes RC, et al. A pooled analysis of bone marrow micrometastasis in breast cancer. N Engl J Med. 2005;353:793–802.
Fehm T, Krawczyk N, Solomayer EF, Becker-Pergola G, Dürr-Störzer S, Neubauer H, et al. ERalpha-status of disseminated tumour cells in bone marrow of primary breast cancer patients. Breast Cancer Res. 2008;10:R76.
Meads MB, Hazlehurst LA, Dalton WS. The bone marrow microenvironment as a tumor sanctuary and contributor to drug resistance. Clin Cancer Res. 2008;14:2519–26.
Wiedswang G, Borgen E, Kåresen R, Kvalheim G, Nesland JM, Qvist H, et al. Detection of isolated tumor cells in bone marrow is an independent prognostic factor in breast cancer. J Clin Oncol. 2003;21:3469–78.
Hartkopf AD, Taran F-A, Wallwiener M, Hahn M, Becker S, Solomayer EF, et al. Prognostic relevance of disseminated tumour cells from the bone marrow of early stage breast cancer patients—results from a large single-centre analysis. Eur J Cancer. 2014;50:2550–9.
Diel IJ, Solomayer EF, Costa SD, Gollan C, Goerner R, Wallwiener D, et al. Reduction in new metastases in breast cancer with adjuvant clodronate treatment. N Engl J Med. 1998;339:357–63.
Domschke C, Neubrech F, Dick M, Rom J, Beckhove P, Sohn C, et al. Intraoperative bone marrow puncture in breast cancer patients: prospective assessment of adverse side-effects. Breast. 2011;20:62–5.
McGuckin MA, Walsh MD, Hohn BG, Ward BG, Wright RG. Prognostic significance of MUC1 epithelial mucin expression in breast cancer. Hum Pathol. 1995;26:432–9.
Borgen E, Naume B, Nesland JM, Kvalheim G, Beiske K, Fodstad Ø, et al. Standardization of the immunocytochemical detection of cancer cells in BM and blood: I. Establishment of objective criteria for the evaluation of immunostained cells. Cytotherapy. 1999;1:377–88.
Cheang MCU, Chia SK, Voduc D, Gao D, Leung S, Snider J, et al. Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst. 2009;101:736–50.
Goldhirsch A, Winer EP, Coates AS, Gelber RD, Piccart-Gebhart M, Thürlimann B, et al. Personalizing the treatment of women with early breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2013. Ann Oncol. 2013;24:2206–23.
Mansi JL, Easton D, Berger U, Gazet JC, Ford HT, Dearnaley D, Coombes RC. Bone marrow micrometastases in primary breast cancer: prognostic significance after 6 years’ follow-up. Eur J Cancer. 1991;27:1552–5.
Cote RJ, Rosen PP, Lesser ML, Old LJ, Osborne MP. Prediction of early relapse in patients with operable breast cancer by detection of occult bone marrow micrometastases. J Clin Oncol. 1991;9:1749–56.
Harbeck N, Untch M, Pache L, Eiermann W. Tumour cell detection in the bone marrow of breast cancer patients at primary therapy: results of a 3-year median follow-up. Br J Cancer. 1994;69:566–71.
Gerber B, Krause A, Müller H, Richter D, Reimer T, Makovitzky J, et al. Simultaneous immunohistochemical detection of tumor cells in lymph nodes and bone marrow aspirates in breast cancer and its correlation with other prognostic factors. J Clin Oncol. 2001;19:960–71.
Gebauer G, Fehm T, Merkle E, Beck EP, Lang N, Jäger W. Epithelial cells in bone marrow of breast cancer patients at time of primary surgery: clinical outcome during long-term follow-up. J Clin Oncol. 2001;19:3669–74.
Diel IJ, Kaufmann M, Goerner R, Costa SD, Kaul S, Bastert G. Detection of tumor cells in bone marrow of patients with primary breast cancer: a prognostic factor for distant metastasis. J Clin Oncol. 1992;10:1534–9.
Naume B, Borgen E, Kvalheim G, Kåresen R, Qvist H, Sauer T, et al. Detection of isolated tumor cells in bone marrow in early-stage breast carcinoma patients: comparison with preoperative clinical parameters and primary tumor characteristics. Clin Cancer Res. 2001;7:4122–9.
Naume B, Zhao X, Synnestvedt M, Borgen E, Russnes HG, Lingjærde OC, et al. Presence of bone marrow micrometastasis is associated with different recurrence risk within molecular subtypes of breast cancer. Mol Oncol. 2007;1:160–71.
Synnestvedt M, Borgen E, Schlichting E, Schirmer CB, Renolen A, Giercksky KE, et al. Disseminated tumour cells in the bone marrow in early breast cancer: morphological categories of immunocytochemically positive cells have different impact on clinical outcome. Breast Cancer Res Treat. 2013;138:485–97.
Hall C, Krishnamurthy S, Lodhi A, Mosalpuria K, Kuerer HM, Meric-Bernstam F, et al. Disseminated tumor cells in biologic subtypes of stage I-III breast cancer patients. Ann Surg Oncol. 2010;17:3252–8.
Bonnefoi H, Litière S, Piccart M, MacGrogan G, Fumoleau P, Brain E, et al. Pathological complete response after neoadjuvant chemotherapy is an independent predictive factor irrespective of simplified breast cancer intrinsic subtypes: a landmark and two-step approach analyses from the EORTC 10994/BIG 1-00 phase III trial. Ann Oncol. 2014;25:1128–36.
Liedtke C, Mazouni C, Hess KR, André F, Tordai A, Mejia JA, et al. Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J Clin Oncol. 2008;26:1275–81.
Woelfle U, Cloos J, Sauter G, Riethdorf L, Jänicke F, van Diest P, et al. Molecular signature associated with bone marrow micrometastasis in human breast cancer. Cancer Res. 2003;63:5679–84.
Aft R, Naughton M, Trinkaus K, Watson M, Ylagan L, Chavez-MacGregor M, et al. Effect of zoledronic acid on disseminated tumour cells in women with locally advanced breast cancer: an open label, randomised, phase 2 trial. Lancet Oncol. 2010;11:421–8.
Rack B, Jückstock J, Genss E-M, Schoberth A, Schindlbeck C, Strobl B, et al. Effect of zoledronate on persisting isolated tumour cells in patients with early breast cancer. Anticancer Res. 2010;30:1807–13.
Solomayer E-F, Gebauer G, Hirnle P, Janni W, Lück HJ, Becker S, et al. Influence of zoledronic acid on disseminated tumor cells in primary breast cancer patients. Ann Oncol. 2012;23:2271–7.
Hoffmann O, Aktas B, Goldnau C, Heubner M, Oberhoff C, Kimmig R, Kasimir-Bauer S. Effect of ibandronate on disseminated tumor cells in the bone marrow of patients with primary breast cancer: a pilot study. Anticancer Res. 2011;31:3623–8.
Stefanovic S, Schuetz F, Sohn C, Beckhove P, Domschke C. Bone marrow microenvironment in cancer patients: immunological aspects and clinical implications. Cancer Metastasis Rev. 2013;32:163–78.
Gnant M. Zoledronic acid in breast cancer: latest findings and interpretations. Ther Adv Med Oncol. 2011;3:293–301.
Banys M, Solomayer E-F, Gebauer G, Janni W, Krawczyk N, Lueck HJ, et al. Influence of zoledronic acid on disseminated tumor cells in bone marrow and survival: results of a prospective clinical trial. BMC Cancer. 2013;13:480.
Gnant M, Mlineritsch B, Stoeger H, Luschin-Ebengreuth G, Heck D, Menzel C, et al. Adjuvant endocrine therapy plus zoledronic acid in premenopausal women with early-stage breast cancer: 62-month follow-up from the ABCSG-12 randomised trial. Lancet Oncol. 2011;12:631–41.
Gnant M, Mlineritsch B, Stoeger H, Luschin-Ebengreuth G, Knauer M, Moik M, et al. Zoledronic acid combined with adjuvant endocrine therapy of tamoxifen versus anastrozol plus ovarian function suppression in premenopausal early breast cancer: final analysis of the Austrian Breast and Colorectal Cancer Study Group Trial 12. Ann Oncol. 2015;26:313–20.
Eidtmann H, de Boer R, Bundred N, Llombart-Cussac A, Davidson N, NevenP, et al. Efficacy of zoledronic acid in postmenopausal women with early breast cancer receiving adjuvant letrozole: 36-month results of the ZO-FAST Study. Ann Oncol. 2010;21:2188–94.
Coleman RE, Marshall H, Cameron D, Dodwell D, Burkinshaw R, Keane M, et al. Breast-cancer adjuvant therapy with zoledronic acid. N Engl J Med. 2011;365:1396–405.
Coleman R, Cameron D, Dodwell D, Bell R, Wilson C, Rathbone E, et al. Adjuvant zoledronic acid in patients with early breast cancer: final efficacy analysis of the AZURE (BIG 01/04) randomised open-label phase 3 trial. Lancet Oncol. 2014;15:997–1006.
Disclosure
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stefanovic, S., Diel, I., Sinn, P. et al. Disseminated Tumor Cells in the Bone Marrow of Patients with Operable Primary Breast Cancer: Prognostic Impact in Immunophenotypic Subgroups and Clinical Implication for Bisphosphonate Treatment. Ann Surg Oncol 23, 757–766 (2016). https://doi.org/10.1245/s10434-015-4895-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4895-3